SYSTEMATIC REVIEW article
Interventions to reduce the incidence of medical error and its financial burden in health care systems: a systematic review of systematic reviews.

- 1 Department of Health Policy and Management, Tabriz Health Services Management Research Center, Iranian Center of Excellence in Health Management, School of Management and Medical Informatics, Tabriz University of Medical Sciences, Tabriz, Iran
- 2 Wolfson Institute of Population Health, Queen Mary University of London, London, United Kingdom
- 3 Department of Infectious Disease Epidemiology, London School of Hygiene and Tropical Medicine, London, United Kingdom
- 4 Social Determinants of Health Research Center, Tabriz University of Medical Sciences, Tabriz, Iran
Background and aim: Improving health care quality and ensuring patient safety is impossible without addressing medical errors that adversely affect patient outcomes. Therefore, it is essential to correctly estimate the incidence rates and implement the most appropriate solutions to control and reduce medical errors. We identified such interventions.
Methods: We conducted a systematic review of systematic reviews by searching four databases (PubMed, Scopus, Ovid Medline, and Embase) until January 2021 to elicit interventions that have the potential to decrease medical errors. Two reviewers independently conducted data extraction and analyses.
Results: Seventysix systematic review papers were included in the study. We identified eight types of interventions based on medical error type classification: overall medical error, medication error, diagnostic error, patients fall, healthcare-associated infections, transfusion and testing errors, surgical error, and patient suicide. Most studies focused on medication error (66%) and were conducted in hospital settings (74%).
Conclusions: Despite a plethora of suggested interventions, patient safety has not significantly improved. Therefore, policymakers need to focus more on the implementation considerations of selected interventions.

Introduction
A medical error is a preventable adverse effect of medical care (“iatrogenesis”). It can be defined as the “failure of a planned action to be completed as intended or the use of a wrong plan to achieve an aim” ( 1 ). As the associated burden is evident, medical errors have drawn considerable attention from academics, hospital managers, and major health stakeholders. Medical errors have a significant adverse impact on patients' outcomes and workers' mental health. They are associated with a considerable financial burden and undermine public trust in the health system ( 2 – 4 ). Medical errors, including healthcare-related adverse events, occur in 8–12% of hospitalisations in Europe ( 5 ). At least 50% of hospitalized patients' harm could be preventable ( 6 ). Overall, healthcare-associated infections incidence is estimated at 4.1 million patients a year in Europe, with the four main types of error being urinary tract infections (27%), lower respiratory tract infections (24%), surgical site infections (17%), and bloodstream infections (10.5%) ( 5 ). In the US (2007), 1.7 million healthcare-associated infections occur annually. They result in excess healthcare costs of $35.7–$45 billion for inpatient hospital services ( 7 , 8 ).
The medical errors can be classified based on their content or “what went wrong” (e.g., medication, surgical, transfusion, healthcare-associated infection) ( 9 – 15 ); location or “where did it happen” (e.g., intensive care unit, operation theater, emergency department, children's ward) ( 15 – 18 ); staff or “who made an error” (e.g., doctor, pharmacists, nurse) ( 10 , 19 , 20 ); error's severity or “how harmful was it” (e.g., error, no harm, near miss) ( 21 – 25 ); and “who was affected” (e.g., patient, family, medical staff) ( 26 , 27 ). Depending on the type of medical errors, studies suggest various solutions, from simple activities (e.g., hand hygiene to prevent healthcare-associated infection) to more complex ones such as using technological instruments or methods to prevent retained surgical instruments errors ( 7 , 15 ).
Despite the ongoing efforts to reduce and prevent the burden of medical errors and related patient harm, global efforts have not yet achieved substantial change over the past 15 years due to various reasons ( 6 ). Unclear policies, insufficient or unreliable data to drive patient safety improvements, unskilled health care professionals, lack of organizational leadership capacity, and non-participation of patients and families in the care process led to unsustainable and insignificant improvements in health care safety ( 2 ). Hence the primary goal of this article was to conduct a systematic review of systematic reviews to elicit interventions that can reduce medical errors or medical error costs in hospitals and analyse interventions implementation results where available. Specifically, we focused on interventions that can reduce health care costs, patient's harm and death, improve health services quality, patient's satisfaction, and safety.
Literature search and study selection
Inclusion criteria for articles considered in this review were as follows: (a) systematic reviews; (b) studies published in English language; (c) studies on solutions regarding medical error reduction or medical error costs; (d) studies on interventions in hospitals or the whole of the healthcare sector, which entered the study regardless of whether these reviews were based on reported errors, an examination of medical profiles, observational studies or other methods. We excluded studies (a) published in languages other than English; (b) studies conducted in settings other than the hospital; (c) studies focused only on a specific type of medical error/activity/patient subgroup, or a sporadic type of medical error (e.g., wrong-site surgery in neurosurgery); (d) studies focusing on a particular group of employees where generalisability to other groups would not be feasible (i.e., only nurses, physicians, pharmacists); (e) conference abstracts, narrative reviews, editorial and other types of studies but systematic reviews; (f) studies related to adverse events only; and (g) studies with no effect on medical errors.
Search strategy
To identify relevant interventions, we searched the four databases (PubMed, Scopus, Ovid Medline and Embase) from Oct 1977 until January 2021 and selected English-only publications. Multiple keywords related to medical errors were researched and customized for each database. We used the filters for searching papers on interventions to reduce medical error to maximize the sensitivity of our literature search. We did not make any limitations on the outcomes. Additionally, references from the included systematic reviews were checked and added to selected studies. Our search strategy was adjusted for each database accordingly. For example, following combination was used for Pubmed database: ((((((((((((((((medical errors[MeSH Terms] OR “recording error”[Title/Abstract]) OR “no harm”[Title/Abstract] OR “patient fall * ”[Title/Abstract]) OR “hospital infection”[Title/Abstract]) OR “transfusion error”[Title/Abstract]) OR “prescription error”[Title/Abstract]) OR “prescribing error”[Title/Abstract]) OR “CPR error”[Title/Abstract]))) OR “medication error”[Title/Abstract]) OR “near miss”[Title/Abstract]) OR “suicide”[Title/Abstract]) OR “sentinel event”[Title/Abstract]) OR “never event”[Title/Abstract]) AND systematic[sb]). An overview of the full search strategy can be found in Appendix 1 .
Data extraction
Two researchers independently extracted data from selected reviews. A third reviewer resolved any disagreements between the two reviewers. The following data were extracted: author, year, aim of the study, setting, medical error type, interventions, and the overall results if reported. Only reviews that met our selection criteria were extracted and analyzed.
Data analysis
The interventions of reviews were classified based on the medical error types. We additionally checked for the overlap between primary studies included in systematic reviews. Since there was no complete overlap between the reviews, none of the studies were excluded.
Search results
The initial search provided 2108 records (Figure 1 ). After eliminating duplicate papers, titles and abstract screening, 181 reviews underwent the full-text assessment. In total 76 reviews met the inclusion criteria, 105 were excluded for various reasons ( Figure 1 ).
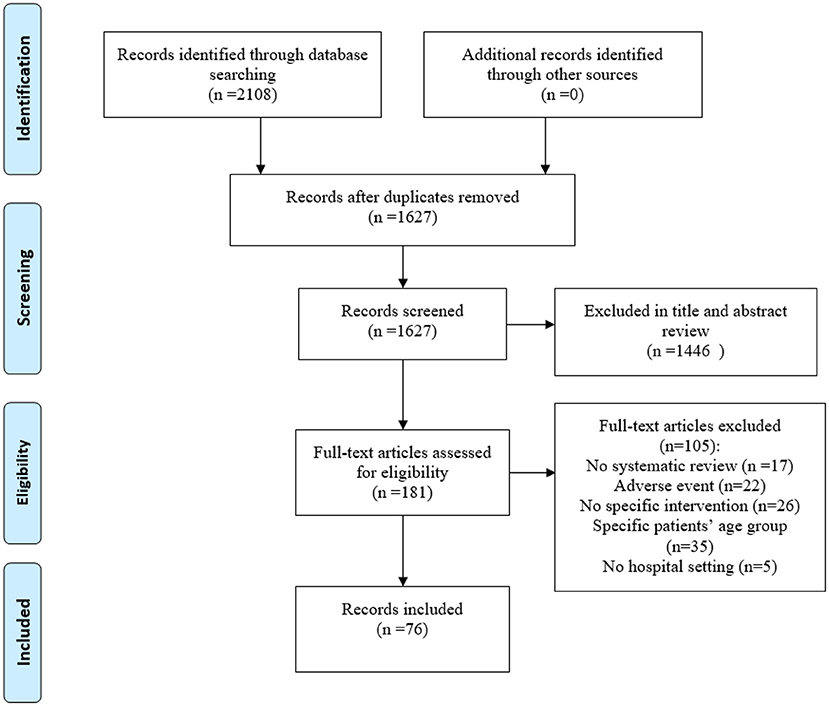
Figure 1 . PRISMA flow diagram for the review process.
Characteristics of the included systematic reviews
More than half of systematic reviews (67%) were published between 2013 and 2020 ( n = 51). 66% of reviews were about medication error ( n = 49), and 74% were related to all hospital settings ( n = 56). The included studies reported on interventions for eight types of medical errors: overall medical error (13 interventions), medication error (37 interventions), patients' fall (11 interventions), healthcare-associated infections (21 interventions), diagnostic errors (7 interventions), transfusion and testing errors (8 interventions), surgical errors (3 interventions), and patients' suicide (13 interventions) ( Table 1 ). Table 2 provides an overview of the impact of interventions on medical error reduction by intervention group. A more detailed overview of the impact of studies, including their aim, setting, and overall results can be found in Supplementary Table 1 .
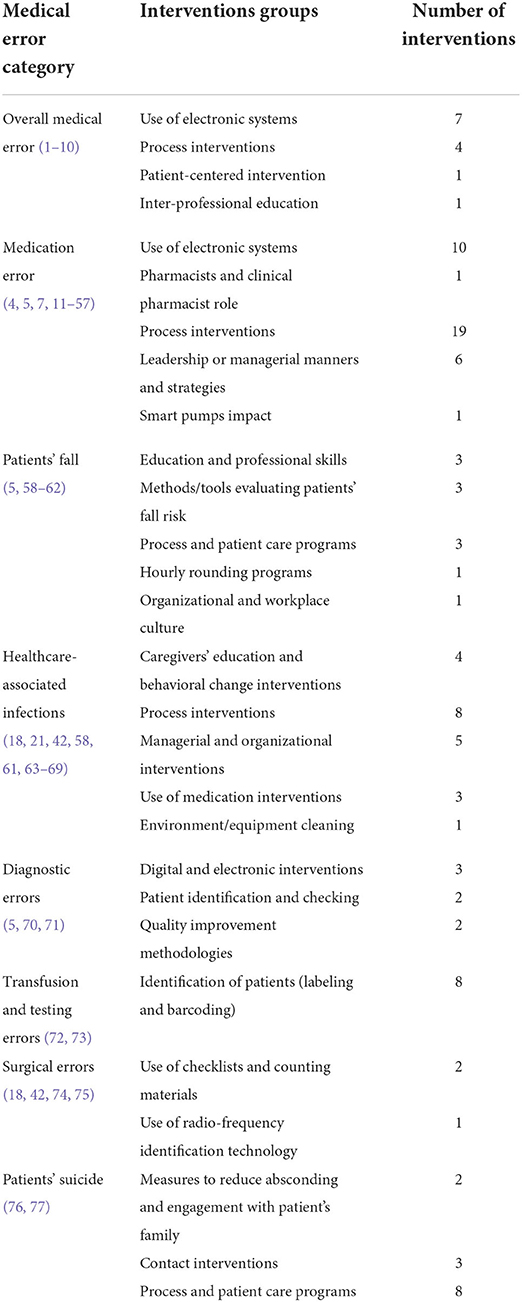
Table 1 . Interventions to reduce medical error by medical error category.
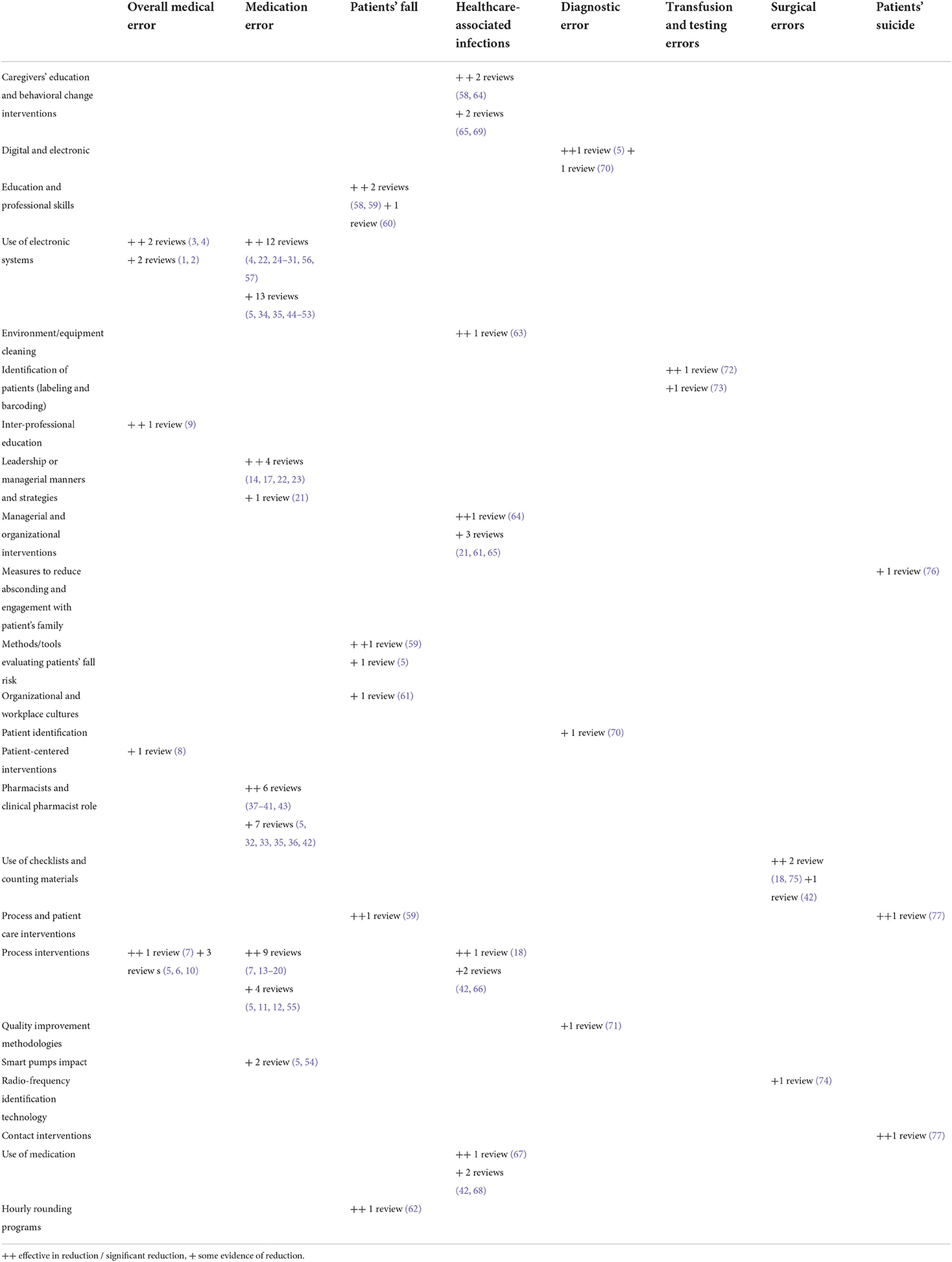
Table 2 . Impact of interventions on medical error reduction by intervention group.
Interventions based on medical error types
Overall medical error.
This group of interventions was not restricted to a specific medical error type. It included four interventions groups (i.e., use of electronic systems, patient-centered intervention, process interventions, and inter-professional education). In total, ten reviews focused on overall medical errors ( 28 – 37 ) and included 257 primary studies ( Table 1 ). Five reviews focused on the use of electronic systems to reduce overall medical error levels using health information systems, computerized provider order entry systems combined with clinical decision support systems, diagnostic and clinical decision-making aids, error-resistant systems, computer-enabled discharge communication, personal digital assistants, human simulation training) ( 28 – 32 ). Four reviews presented the process interventions such as failure mode and effects analysis, proactive technique, systematic safety processes, teamwork and communication training interventions, and reactive systematic safety processes in reducing risks, medical errors and adverse events ( 32 – 34 , 37 ). One study referred to a patient-centered intervention, i.e., documentation through patient involvement and feedback on the medical file ( 35 ). Reeves et al. focused on interprofessional education ( 36 ) ( Supplementary Table 1 ).
Reviews confirmed that using electronic systems could reduce ( 28 , 29 ) or effectively and significantly ( 30 , 31 ) reduce medical errors. For example, Charles et al. ( 29 ) stated that computerized provider order entry reduces medical error and adverse drug events. The effect would be more when combined with clinical decision support systems to alert healthcare providers of medical errors ( 29 ). Studies that focused on other intervention groups [i.e., process interventions ( 32 – 34 , 37 ), patient-centered intervention ( 35 ), and inter-professional education ( 36 )] presented some evidence of their potential to reduce medical errors ( Table 2 ). For example, using process interventions minimizes risks and improves service quality ( 33 ). In contrast, interprofessional education could reduce medical errors and enhance behavior culture in the emergency department ( 36 ).
Medication error
This intervention group related to medication errors and specific subcategories (prescribing, dispensing, administering, transcription and dose errors). These interventions fell into five groups: use of electronic systems, pharmacists and clinical pharmacist involvement in the treatment process, process interventions, leadership or managerial manners, and strategies and smart pumps impact. Overall, 49 reviews focused on interventions to reduce medication errors. This was the most prominent intervention category, including 1,380 primary studies ( Table 1 ). Twentyfive reviews focused on using electronic systems ( 14 , 16 , 31 , 32 , 38 – 58 ). Twelve reviews focused on pharmacists and clinical pharmacist involvement in the treatment process ( 13 , 17 , 32 , 41 , 59 – 66 ). Five reviews presented leadership or managerial manners interventions ( 12 , 56 , 67 – 69 ). The remaining 12 reviews stated process interventions ( 9 , 12 , 32 , 34 , 67 , 70 – 76 ), and two reviews focused on smart pumps impact ( 32 , 77 ) ( Table 2 ).
Similarly to overall medical error interventions, reviews focusing on electronic systems provided evidence that they could reduce ( 14 , 16 , 32 , 38 – 48 ) or effectively and significantly ( 31 , 49 – 58 ) reduce medication errors. For example, the most significant results were noted for computerized provider order entry in 96% error interception and 90% reduction of medication errors ( 41 , 44 ). There was evidence that leadership or managerial manners intervention could effectively and significantly reduce medication errors ( 12 , 56 , 67 – 69 ). For example, redesign of diabetes prescribing charts incorporating prescribing guidelines, diabetes prescription error management pathway, and mandatory e-learning reduced insulin prescription errors from 65 to 2% ( 67 ) ( Table 2 , Supplementary Table 1 ). Reviews on pharmacists and clinical pharmacist involvement in the treatment process presented evidence of some to a very effective and significant reduction on medical errors. For example, pharmacists' participation in medical treatment leads to a 43% reduction in prescribing errors and a 27% reduction in overall medication errors ( 63 , 64 ). Most reviews on process interventions had also shown that such intervention could effectively and significantly reduce medication errors ( 9 , 12 , 34 , 67 , 70 – 74 ), with only a few ( 32 , 75 , 76 , 78 ) presenting only some evidence of medication error reduction. For example, double-checking reduce medication error from 2.98 to 2.12 per 1,000 medication administered and dispensing error from 9.8 to 6 ( 73 ).
Patients' fall
This group of interventions focused on interventions that could reduce patients' falls by using four different categories of interventions (professional skills and education, methods/tools evaluating patients' fall risk, process and patient care programs, organizational and workplace culture). In total, six reviews ( 10 , 26 , 27 , 32 , 79 , 80 ) focused on fall prevention and included 14 primary studies. Three reviews focused on using education and professional skills interventions ( 10 , 27 , 79 ). Two reviews presented using methods and tools evaluating patients' fall risk ( 27 , 32 ). Cumbler et al. reported process and patient care programs as beneficial interventions ( 27 ). One study focused on hourly rounding programs ( 80 ), and Braithwaite et al. presented organizational and workplace culture interventions ( 26 ) ( Table 2 ).
Based on the results of reviews, education and professional skills interventions effectively reduced or led to a significant reduction in patients' falls ( 10 , 27 , 80 ), while another review showed some evidence of a reduction in patients' falls ( 79 ). For example, there were patients' fall differences in intervention groups vs. control groups through patient-centered interventions (180 in intervention group vs. 319 in control group) ( 79 ). There was evidence that methods/tools evaluating patients' fall risk intervention could effectively and significantly reduce medical errors ( 27 ), and other reviews showed that could reduce patients' falls ( 32 ). For example, using the Morse fall scale decreased falls ( 27 ). Two remaining studies focused on effectively and significantly reducing patients' falls ( 27 , 80 ), and the other had some evidence of reduction ( 26 ). For example, staff education, care planning, patient training in rehabilitation and nutritionist support lead to a reduction in falls from 16.28 to 6.29 per 1,000 patient days ( 27 ) ( Table 2 , Supplementary Table 1 ).
Healthcare-associated infections
Twelve reviews and 382 primary studies focused on five groups of interventions that could reduce healthcare-associated infections (caregivers' educational and behavioral change interventions, process interventions, managerial and organizational interventions, using medication interventions and environment/equipment cleaning) ( Table 1 ). Four reviews focused on the caregivers' education and behavioral changes ( 10 , 81 – 83 ). Three reviews focused on process interventions ( 65 , 72 , 84 ). Four reviews presented the managerial and organizational interventions ( 26 , 69 , 81 , 83 ). Three reviews reported medication interventions ( 65 , 85 , 86 ). Schabrun et al. focused on equipment cleaning ( 87 ) ( Table 2 ).
Caregivers' education and behavioral change effectively reduced healthcare-associated infections ( 10 , 81 ), and the other two reviews showed some evidence of a reduction in healthcare-associated infections ( 82 , 83 ). For example, hand-hygiene campaigns reduced nosocomial infection rates (median effect 49%) ( 81 ). Boyd et al. presented an effective or significant reduction in healthcare-associated infections ( 72 ), and two reviews showed that these interventions could reduce healthcare-associated infections ( 65 , 84 ). For example, the Keystone intensive care unit intervention for central line-associated bloodstream infections and chlorhexidine for vascular catheter site care economically reduced healthcare-associated infections ( 65 ). One review stated that managerial and organizational interventions are significant or effective in reducing healthcare-associated infections ( 81 ), while three studies have some evidence on reducing healthcare-associated infections ( 26 , 69 , 83 ). For example, antibiotic stewardship, antibiotic restriction, guidelines, education, and performance feedback showed a significant decrease ranging from 13 to 82% ( 81 ). One review of medication interventions reported a significant decline (28%) in surgical site infection using a chlorhexidine impregnated dressing that applied to the surgical site ( 86 ). Another review demonstrated an effective reduction (82.1%) in colony-forming units after cleaning pieces of equipment with alcohol ( 87 ).
Diagnostic error
Three studies that included 68 primary studies focused on three intervention categories (digital and electronic interventions, patient identification and checking and quality improvement methodologies) that affect diagnostic errors ( 2 , 32 , 88 ) ( Table 1 ). Two studies presented the use of digital and electronic interventions ( 2 , 32 ). One study focused on the use of patient identification ( 2 ). Amaratunga et al. focused on quality improvement methodologies ( 88 ). One review focused on digital and electronic interventions showed a significant effect of interventions to reduce diagnostic error. The other one presented some evidence of diagnostic error reduction ( 2 , 32 ). For example, clinical decision support systems and a web-based diagnostic reminder system significantly reduced diagnostic errors ( 32 ). Zhou et al. ( 2 ) presented some evidence of a reduction in diagnostic error using patient identification. For example, the patient identification check, obtaining informed consent, verifying the correct side and site, and a final check by the radiologist decreased the incidence rate of diagnostic error from 0.03% (9 of 32,982) to 0.005% ( 2 ). Another review reported some evidence of a reduction in diagnostic error within radiology by lean and Six Sigma approaches as quality improvement methodologies ( 88 ).
Transfusion and testing errors
Two reviews included 26 primary studies focused on the identification of patients (labeling and barcoding) intervention ( 11 , 89 ) ( Table 1 ). The results of Snyder et al.'s review was effective in reducing transfusion and testing errors ( 89 ), and another review showed some evidence on reducing transfusion and testing errors ( 11 ) ( Table 2 ). For example, labeling significantly reduces testing errors, so the most effective intervention in reducing transfusion and testing errors was barcoding systems, which reduced 2.26 errors to 0.17 errors per 10,000 specimens ( 89 ).
Surgical errors
Four reviews included 38 primary studies focused on two intervention groups to reduce surgical errors (use of checklists and counting instruments and material and use of radio-frequency identification technology) ( 15 , 65 , 72 , 90 ) ( Table 1 ). Three reviews reported using checklists and counting materials interventions ( 65 , 72 , 90 ). Another review focused on radio-frequency identification technology ( 15 ) ( Table 2 ). Two reviews showed an effective reduction in surgical errors ( 72 , 90 ) while, Etchells et al.'s review had some evidence related to reducing surgical errors ( 65 ). For example, using checklists (or similar interventions) could reduce equipment errors in the operating room by 48.6% ( 90 ). One review showed some evidence to reduce retained surgical instrument errors, reduce the risk of counting errors, and improve workflow using radio-frequency identification technology ( 15 ) ( Table 2 ).
Patients' suicide
Two reviews included 112 primary studies focused on reducing patients' suicide ( 91 , 92 ) ( Table 1 ). One review focused on reducing absconding and engagement with patient's family intervention ( 91 ). Doupnik et al., focused on process and patient care interventions and contact interventions ( 92 ) ( Table 2 ). Bowers et al. reported measures to reduce absconding and engagement with patient's family intervention, showed some evidence to reduce absconding without locking the door and engage with patients' family problems to reduce patients' suicide ( 91 ). Another review focused on process, and patient care interventions and contact interventions showed significant reduction (pooled odds ratio, 0.69) in patients' suicide by using 11 interventions (i.e., telephone, postcard, letters, coordination between the mental health care team, and follow up mental health care team) ( 92 ) ( Supplementary Table 1 , Table 2 ).
We systematically reviewed systematic reviews for interventions to reduce medical errors in hospitals. Studies related to preventing medication errors included approximately 35 interventions. We identified 21 groups of interventions falling into seven broader categories of medical errors. The least studied category of medical errors was related to patients' suicide and surgical errors. Our findings showed that among 101 presented interventions, the use of electronic systems intervention group, was included in most of the reviews (27 reviews). This group included interventions that reduce medication and overall medical errors. Most interventions were related to the processing group (30 interventions). Also, this group had three types of errors (overall medical error, medication error, and healthcare-associated infections). The most effective interventions were related to medication errors among medical error types (27 reviews) and electronic systems among intervention groups (12 reviews).
Patient safety has several requirements such as safe infrastructure, technologies and medical devices, patient and staff education, information, professional participation in patient safety programs, and ensuring that all individuals receive secure health services, regardless of where they are delivered. This was reiterated in the resolution on “Global action on patient safety” in May 2019 (WHA72.6) ( 93 ). In particular, the resolution requests the World Health Organization's Director-General to formulate a global patient safety action plan in consultation with the Member States, regional economic integration organizations and all relevant stakeholders, including in the private sector. As stated in the resolution, to achieve the highest level of patient safety and to be able to reduce medical error and adverse events, one needs to recognize patient safety as a health priority in health sector policies and programs, collaborate with other member states along with the improvement of national policies, programs, guidelines, strategies and tools.
There are several ways, policies and procedures to identify medical errors. Differences in error identification methods affect the incidence of errors and error reduction interventions. These methods include voluntary reporting, direct observation, patient and family reporting, and retrospective and prospective methods (cohort and cross sectional studies) and related techniques (e.g., failure mode, effects analysis, and root cause analysis) ( 94 – 99 ).
The most effective interventions related to patient satisfaction referred to managerial and process interventions that show patients do not have enough knowledge about medical issues. Process and administrative interventions increase their satisfaction as a perceived issue ( 70 , 80 ). Effective interventions to reduce costs and increase efficiency were related to using electronic systems and processes and managerial or leadership strategies ( 9 , 12 , 54 , 70 ). For example, electronic distribution drug systems decreased by €44,295 in a month ( 9 ). Effective interventions related to reducing death referred to the use of electronic systems and process interventions ( 16 , 70 ). For example, commercial computerized provider order entry led to a 12% reduction in intensive care units mortality rates ( 16 ). Effective interventions for increasing health care quality were referred to as checklists and counting materials, environment/equipment cleaning, use of electronic systems, and process interventions ( 9 , 54 , 87 , 90 ). Effective interventions related to patient safety were associated with the use of electronic systems, process, education and professional skills, methods/tools evaluating patients' fall risk, and process and patient care interventions groups ( 9 , 27 , 34 , 51 , 53 , 58 ).
As we highlighted in our study findings, use of electronic systems has a wide effect on reduction of medical errors and related deaths, efficiency and effectiveness of services, and improvement of patient safety. Of course, when using electronic systems, like any other method, one must pay attention to its specific limitations and considerations. For example, implementation of computerized prescription order entry can lead to wrong drug selection from drop-down menus ( 49 ). Nonetheless, computerized prescription order entry systems are more effective to detect medical errors when they are bundled with clinical decision support systems, which has the potential to prevent errors of medication forms nearly completely ( 29 , 100 ). Simulation systems prevent iatrogenic risk related to medication errors, if the program is well designed ( 14 ).
Our review has several limitations. One is that medical errors cover a very wide range of topics that cannot be addressed in one review article. For example, topics that were left outside the scope of this paper include error identification policies, procedures and methods, disclosure approaches, and incidence of medical errors. Another limitation is that we focused on the interventions in the hospital settings. Due to the high number of papers related to the effect of interventions on medical error, we restricted our analysis to documents that reported the positive impact of the intervention on medical error reduction. Also, our study was limited to systematic reviews that had different focus; hence, meta-analyses were not possible.
Prevention of medical errors is vital in reducing patient's harm and improving overall patient outcomes. A review of the combined evidence of 73 systematic reviews found that a wide range of interventions could be used to prevent and decrease of incidence of medical errors. Process and managerial interventions, and use of electronic systems had a critical role in medical error reduction.
Data availability statement
The original contributions presented in the study are included in the article/ Supplementary material , further inquiries can be directed to the corresponding author/s.
Author contributions
EA-E and LD conceived the basic and original idea, outlined the study, literature review, data acquisition, data analysis, interpretation of data, and drafted the article. VS contributed to data acquisition, data analysis, interpretation of data, and drafting and revising of manuscript. All authors participated in the final design, revision of the manuscript, and have read and approved the manuscript.
Acknowledgments
This study forms Ph.D. research project of the primary author supported by the Tabriz University of Medical Sciences, Tabriz, Iran.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2022.875426/full#supplementary-material
1. Donaldson MS, Corrigan JM, Kohn LT. To Err is Human: Building a Safer Health System . Vol. 6. Washington, DC: National Academies Press (2000).
2. Zhou Y, Boyd L, Lawson C. Errors in medical imaging and radiography practice: a systematic review. J Med Imag Radiat Sci. (2015) 46:435–41. doi: 10.1016/j.jmir.2015.09.002
PubMed Abstract | CrossRef Full Text | Google Scholar
3. Heideveld-Chevalking A, Calsbeek H, Griffioen I, Damen J, Meijerink W, Wolff A. Development and validation of a Self-assessment Instrument for Perioperative Patient Safety (SIPPS). BJS open. (2018) 2:381–91. doi: 10.1002/bjs5.82
4. Andel C, Davidow SL, Hollander M, Moreno DA. The economics of health care quality and medical errors. J Health Care Finance. (2012) 39:39.
PubMed Abstract | Google Scholar
5. Patient safety, Data and statisics: WHO Regional office for Europe. (2021). Available online at: https://www.euro.who.int/en/health-topics/Health-systems/patient-safety/data-and-statistics (accessed January 29, 2021).
6. Patient safety, Overview (2021). Available online at: https://www.who.int/health-topics/patient-safety#tab=tab_1 (accessed January 29, 2021).
7. Sreeramoju P. Preventing healthcare-associated infections: Beyond best practice. Am J Med Sci. (2013) 345:239–44. doi: 10.1097/MAJ.0b013e31824435e6
8. Scott RD. The direct medical costs of healthcare-associated infections in US hospitals and the benefits of prevention. (2009).
9. Ahtiainen HK, Kallio MM, Airaksinen M, Holmström AR. Safety, time and cost evaluation of automated and semi-automated drug distribution systems in hospitals: a systematic review. Eur J Hospital Pharmacy. (2019). doi: 10.1136/ejhpharm-2018-001791
10. Coelho P. Relationship between nurse certification and clinical patient outcomes: a systematic literature review. J Nurs Care Qual. (2019). doi: 10.1097/NCQ.0000000000000397
11. Cottrell S, Watson D, Eyre TA, Brunskill SJ, Dorée C, Murphy MF. Interventions to reduce wrong blood in tube errors in transfusion: A systematic review. Transfus Med Rev. (2013) 27:197–205. doi: 10.1016/j.tmrv.2013.08.003
12. Mikrani R, Naveed M, Mikrani A, Yasmeen S, Akabar M, Xiaohui Z. The impact of clinical pharmacy services in Nepal in the context of current health policy: a systematic review. J Public Health. (2019). doi: 10.1007/s10389-019-01042-y
CrossRef Full Text | Google Scholar
13. Noormandi A, Karimzadeh I, Mirjalili M, Khalili H. Clinical and economic impacts of clinical pharmacists' interventions in Iran: a systematic review. DARU, J Pharmaceutical Sci. (2019) 27:361–78. doi: 10.1007/s40199-019-00245-8
14. Sarfati L, Ranchon F, Vantard N, Schwiertz V, Larbre V, Parat S, et al. Human-simulation-based learning to prevent medication error: A systematic review. J Eval Clin Pract. (2019) 25:11–20. doi: 10.1111/jep.12883
15. Schnock KO, Biggs B, Fladger A, Bates DW, Rozenblum R. Evaluating the impact of radio frequency identification retained surgical instruments tracking on patient safety: literature review. J Patient Saf. (2017). doi: 10.1097/PTS.0000000000000365
16. Prgomet M, Li L, Niazkhani Z, Georgiou A, Westbrook JI. Impact of commercial computerized provider order entry (CPOE) and clinical decision support systems (CDSSs) on medication errors, length of stay, and mortality in intensive care units: A systematic review and meta-analysis. J Am Med Inform Assoc. (2017) 24:413–22. doi: 10.1093/jamia/ocw145
17. Cohen V, Jellinek SP, Hatch A, Motov S. Effect of clinical pharmacists on care in the emergency department: A systematic review. Am J Health-Syst Pharmacy. (2009) 66:1353–61. doi: 10.2146/ajhp080304
18. Lucas AJ. Improving medication safety in a neonatal intensive care unit. Am J Health-Syst Pharm. (2004) 61:33–7. doi: 10.1093/ajhp/61.1.33
19. Lee SE, Quinn BL. Incorporating medication administration safety in undergraduate nursing education: a literature review. Nurse Educ Today. (2019) 72:77–83. doi: 10.1016/j.nedt.2018.11.004
20. Owoc J, Manczak M, Tombarkiewicz M, Robert Olszewski R. Association between physician burnout and self-perceived error: Meta-analysis. Eur J Prev Cardiol. (2019) 26:S57. doi: 10.1177/2047487319860048
21. Mehtsun WT, Ibrahim AM, Diener-West M, Pronovost PJ, Makary MA. Surgical never events in the United States. Surgery. (2013) 153:465–72. doi: 10.1016/j.surg.2012.10.005
22. Omar I, Graham Y, Singhal R, Wilson M, Madhok B, Mahawar KK. Identification of common themes from never events data published by NHS England. World J Surg. (2021) 45:697–704. doi: 10.1007/s00268-020-05867-7
23. Kim CW, Myung SJ, Eo EK, Chang Y. Improving disclosure of medical error through educational program as a first step toward patient safety. BMC Med Educ. (2017) 17:1–6. doi: 10.1186/s12909-017-0880-9
24. Wallis J, Fletcher D, Bentley A, Ludders J. Medical errors cause harm in veterinary hospitals. Front Veter Sci. (2019) 6:12. doi: 10.3389/fvets.2019.00012
25. Benimana C, Small M, Rulisa S. Preventability of maternal near miss and mortality in Rwanda: a case series from the University Teaching Hospital of Kigali (CHUK). PLoS ONE. (2018) 13:e0195711. doi: 10.1371/journal.pone.0195711
26. Braithwaite J, Herkes J, Ludlow K, Testa L, Lamprell G. Association between organisational and workplace cultures, and patient outcomes: Systematic review. BMJ Open . (2017) 7:e017708. doi: 10.1136/bmjopen-2017-017708
27. Cumbler EU, Simpson JR, Rosenthal LD, Likosky DJ. Inpatient falls: defining the problem and identifying possible solutions. Part I: An Evidence-Based Review. The Neurohospitalist. (2013) 3:135–43. doi: 10.1177/1941874412470665
28. Ahmadian L, Salehi Nejad S, Khajouei R. Evaluation methods used on health information systems (HISs) in Iran and the effects of HISs on Iranian healthcare: A systematic review. Int J Med Inform. (2015) 84:444–53. doi: 10.1016/j.ijmedinf.2015.02.002
29. Charles K, Cannon M, Hall R, Coustasse A. Can utilizing a computerized provider order entry (CPOE) system prevent hospital medical errors and adverse drug events? Perspect Health Inf Manag e. (2014) 11:1b.
30. Motamedi SM, Posadas-Calleja J, Straus S, Bates DW, Lorenzetti DL, Baylis B, et al. The efficacy of computer-enabled discharge communication interventions: A systematic review. BMJ Quality and Safety. (2011) 20:403–15. doi: 10.1136/bmjqs.2009.034587
31. Prgomet M, Georgiou A, Westbrook JI. The Impact of Mobile Handheld Technology on Hospital Physicians' Work Practices and Patient Care: A Systematic Review. J Am Med Inform Assoc. (2009) 16:792–801. doi: 10.1197/jamia.M3215
32. Dückers M, Faber M, Cruijsberg J, Grol R, Schoonhoven L, Wensing M. Safety and risk management interventions in hospitals: A systematic review of the literature. Medical Care Research and Review. (2009) 66:90S–119S. doi: 10.1177/1077558709345870
33. Asgari Dastjerdi H, Khorasani E, Yarmohammadian MH, Ahmadzade MS. Evaluating the application of failure mode and effects analysis technique in hospital wards: a systematic review. J Injury Violence Res . (2017) 9:51. doi: 10.5249/jivr.v9i1.794
34. Damiani G, Pinnarelli L, Scopelliti L, Sommella L, Ricciardi W. A review on the impact of systematic safety processes for the control of error in medicine. Med Sci Monitor. (2009) 15:RA157–RA66.
35. Vermeir P, Degroote S, Vandijck D, Van Tiggelen H, Peleman R, Verhaeghe R, et al. The patient perspective on the effects of medical record accessibility: a systematic review. Acta Clinica Belgica: Int J Clin Laboratory Med. (2017) 72:186–94. doi: 10.1080/17843286.2016.1275375
36. Reeves S, Perrier L, Goldman J, Freeth D, Zwarenstein M. Interprofessional education: Effects on professional practice and healthcare outcomes (update). Cochrane Datab System Rev. (2013) 2013:CD002213. doi: 10.1002/14651858.CD002213.pub3
37. Alsabri M, Boudi Z, Lauque D, Roger DD, Whelan JS, Östlundh L, et al. Impact of teamwork and communication training interventions on safety culture and patient safety in emergency departments: a systematic review. J Patient Saf. (2020). doi: 10.1097/PTS.0000000000000782
38. Eslami S, de Keizer NF, Abu-Hanna A. The impact of computerized physician medication order entry in hospitalized patients–a systematic review. Int J Med Inform. (2008) 77:365–76. doi: 10.1016/j.ijmedinf.2007.10.001
39. Khajouei R, JasperS MWM. The impact of CPOE medication systems' design aspects on usability, workflow and medication orders a systematic review. Methods Inf Med. (2010) 49:3–19. doi: 10.3414/ME0630
40. Ammenwerth E, Schnell-Inderst P, Machan C, Siebert U. The effect of electronic prescribing on medication errors and adverse drug events: a systematic review. J Am Med Inform Assoc. (2008) 15:585–600. doi: 10.1197/jamia.M2667
41. Acheampong F, Anto BP, Koffuor GA. Medication safety strategies in hospitals - A systematic review. Int J Risk Safety Med. (2014) 26:117–31. doi: 10.3233/JRS-140623
42. Kaushal R, Shojania KG, Bates DW. Effects of computerized physician order entry and clinical decision support systems on medication safety: A systematic review. Arch Intern Med. (2003) 163:1409–16. doi: 10.1001/archinte.163.12.1409
43. Manias E, Kusljic S, Wu A. Interventions to reduce medication errors in adult medical and surgical settings: a systematic review. Ther Adv Drug Saf. (2020) 11:2042098620968309. doi: 10.1177/2042098620968309
44. Shitu Z, Aung MMT, Kamauzaman THT, Bhagat V, Rahman AFA. Medication error in hospitals and effective intervention strategies: A systematic review. Res J Pharm Technol. (2019) 12:4669–77. doi: 10.5958/0974-360X.2019.00804.7
45. Keers RN, Williams SD, Cooke J, Walsh T, Ashcroft DM. Impact of interventions designed to reduce medication administration errors in hospitals: A systematic review. Drug Safety. (2014) 37:317–32. doi: 10.1007/s40264-014-0152-0
46. Jia P, Zhang L, Chen J, Zhao P, Zhang M. The effects of clinical decision support systems on medication safety: An overview. PLoS ONE . (2016) 11:e0167683. doi: 10.1371/journal.pone.0167683
47. Pawloski PA, Brooks GA, Nielsen ME, Olson-Bullis BA. A systematic review of clinical decision support systems for clinical oncology practice. JNCCN J National Comprehensive Cancer Network. (2019) 17:331–8. doi: 10.6004/jnccn.2018.7104
48. Bouaud J, Lamy JB, Section Editors for the IYSoDS. A medical informatics perspective on clinical decision support systems. Findings from the yearbook 2013 section on decision support. Yearbook of Med Inform . (2013) 8:128–31. doi: 10.1055/s-0038-1638844
49. Velez-Diaz-Pallares M, Perez-Menendez-Conde C, Bermejo-Vicedo T. Systematic review of computerized prescriber order entry and clinical decision support. Am J Health Syst Pharm. (2018) 75:1909–21. doi: 10.2146/ajhp170870
50. Nuckols TK, Smith-Spangler C, Morton SC, Asch SM, Patel VM, Anderson LJ, et al. The effectiveness of computerized order entry at reducing preventable adverse drug events and medication errors in hospital settings: A systematic review and meta-analysis. System Rev. (2014) 3:56. doi: 10.1186/2046-4053-3-56
51. Ahmed Z, Garfield S, Jani Y, Jheeta S, Franklin BD. Impact of electronic prescribing on patient safety in hospitals: Implications for the UK. Clin Pharmacist . (2016) 8:1–11. doi: 10.1211/CP.2016.20201013
52. Roumeliotis N, Sniderman J, Adams-Webber T, Addo N, Anand V, Rochon P, et al. Effect of Electronic Prescribing Strategies on Medication Error and Harm in Hospital: a Systematic Review and Meta-analysis. J Gen Intern Med. (2019) 34:2210–23. doi: 10.1007/s11606-019-05236-8
53. Ojeleye O, Avery A, Gupta V, Boyd M. The evidence for the effectiveness of safety alerts in electronic patient medication record systems at the point of pharmacy order entry: A systematic review. BMC Med Inform Decis Making. (2013) 13:1–10. doi: 10.1186/1472-6947-13-69
54. Chaudhry B, Wang J, Wu S, Maglione M, Mojica W, Roth E, et al. Systematic review: Impact of health information technology on quality, efficiency, and costs of medical care. Ann Intern Med. (2006) 144:742–52. doi: 10.7326/0003-4819-144-10-200605160-00125
55. Devin J, Cleary BJ, Cullinan S. The impact of health information technology on prescribing errors in hospitals: a systematic review and behaviour change technique analysis. Syst Rev. (2020) 9:275. doi: 10.1186/s13643-020-01510-7
56. Yang C, Yang L, Xiang X, Tang Y, Wang H, Bobai N, et al. Interventions assessment of prescription automatic screening system in chinese hospitals: a systematic review. Drug Inf J. (2012) 46:669–76. doi: 10.1177/0092861512454417
57. Schedlbauer A, Prasad V, Mulvaney C, Phansalkar S, Stanton W, Bates DW, et al. What evidence supports the use of computerized alerts and prompts to improve clinicians' prescribing behavior? J Am Med Inform Assoc. (2009) 16:531–8. doi: 10.1197/jamia.M2910
58. Alanazi A, Alomar M, Aldosari H, Shahrani A, Aldosari B. The effect of electronic medication administration records on the culture of patient safety: a literature review. Studies Health Technol Inform. (2018) 251:223–6. doi: 10.3233/978-1-61499-880-8-223
59. Poh EW, McArthur A, Stephenson M, Roughead EE. Effects of pharmacist prescribing on patient outcomes in the hospital setting: A systematic review. JBI Datab System Rev Implement Reports. (2018) 16:1823–73. doi: 10.11124/JBISRIR-2017-003697
60. Bethishou L, Herzik K, Fang N, Abdo C, Tomaszewski DM. The impact of the pharmacist on continuity of care during transitions of care: A systematic review. J Am Pharm Assoc. (2020) 60:163–77.e2. doi: 10.1016/j.japh.2019.06.020
61. Mekonnen AB, McLachlan AJ, Brien JAE. Pharmacy-led medication reconciliation programmes at hospital transitions: A systematic review and meta-analysis. J Clin Pharm Ther. (2016) 41:128–44. doi: 10.1111/jcpt.12364
62. Chiewchantanakit D, Meakchai A, Pituchaturont N, Dilokthornsakul P, Dhippayom T. The effectiveness of medication reconciliation to prevent medication error: A systematic review and meta-analysis. Res Social Adm Pharm. (2020) 16:886–94. doi: 10.1016/j.sapharm.2019.10.004
63. Wang T, Benedict N, Olsen KM, Luan R, Zhu X, Zhou N, et al. Effect of critical care pharmacist's intervention on medication errors: a systematic review and meta-analysis of observational studies. J Crit Care. (2015) 30:1101–6. doi: 10.1016/j.jcrc.2015.06.018
64. Naseralallah LM, Hussain TA, Jaam M, Pawluk SA. Impact of pharmacist interventions on medication errors in hospitalized pediatric patients: a systematic review and meta-analysis. Int J Clin Pharm. (2020) 42:979–94. doi: 10.1007/s11096-020-01034-z
65. Etchells E, Koo M, Daneman N, McDonald A, Baker M, Matlow A, et al. Comparative economic analyses of patient safety improvement strategies in acute care: a systematic review. BMJ Quality Safety. (2012) 21:448–56. doi: 10.1136/bmjqs-2011-000585
66. Gillani SW, Gulam SM, Thomas D, Gebreigziabher FB, Al-Salloum J, Assadi RA, et al. Role and services of pharmacist in the prevention of medication errors: a systematic review. Curr Drug Saf. (2020). doi: 10.2174/1574886315666201002124713
67. Bain A, Hasan SS, Babar ZUD. Interventions to improve insulin prescribing practice for people with diabetes in hospital: a systematic review. Diabetic Med. (2019) 36:948–60. doi: 10.1111/dme.13982
68. Schroers G. Characteristics of interruptions during medication administration: An integrative review of direct observational studies. J Clin Nurs. (2018) 27:3462–71. doi: 10.1111/jocn.14587
69. Wong CA, Cummings GG, Ducharme L. The relationship between nursing leadership and patient outcomes: A systematic review update. J Nurs Manag. (2013) 21:709–24. doi: 10.1111/jonm.12116
70. Ashcraft S, Bordelon C, Fells S, George V, Thombley K, Shirey MR. Interprofessional Clinical Rounding: Effects on Processes and Outcomes of Care. J Healthcare Quality. (2017) 39:85–94. doi: 10.1097/JHQ.0000000000000039
71. Wimpenny P, Kirkpatrick P. Roles and systems for routine medication administration to prevent medication errors in hospital-based, acute care settings: a systematic review. JBI Libr Syst Rev. (2010) 8:405–46. doi: 10.11124/jbisrir-2010-123
72. Boyd JM, Wu G, Stelfox HT. The impact of checklists on inpatient safety outcomes: A systematic review of randomized controlled trials. J Hospital Med. (2017) 12:675–82. doi: 10.12788/jhm.2788
73. Alsulami Z, Conroy S, Choonara I. Double checking the administration of medicines: What is the evidence? A systematic review. Arch Dis Childhood. (2012) 97:833–7. doi: 10.1136/archdischild-2011-301093
74. McDowell SE, Mt-Isa S, Ashby D, Ferner RE. Where errors occur in the preparation and administration of intravenous medicines: A systematic review and Bayesian analysis. Quality Safety Health Care. (2010) 19:341–5. doi: 10.1136/qshc.2008.029785
75. Jensen LS, Merry AF, Webster CS, Weller CS, Larsson L. Evidence-based strategies for preventing drug administration errors during anaesthesia. Anaesthesia. (2004) 59:493–504. doi: 10.1111/j.1365-2044.2004.03670.x
76. Ostini R, Roughead EE, Kirkpatrick CMJ, Monteith GR, Tett SE. Quality Use of Medicines - Medication safety issues in naming; Look-alike, sound-alike medicine names. Int J Pharm Pract. (2012) 20:349–57. doi: 10.1111/j.2042-7174.2012.00210.x
77. Ohashi K, Dalleur O, Dykes PC, Bates DW. Benefits and risks of using smart pumps to reduce medication error rates: a systematic review. Drug Safety. (2014) 37:1011–20. doi: 10.1007/s40264-014-0232-1
78. Lehnbom EC, Stewart MJ, Manias E, Westbrook JI. Impact of medication reconciliation and review on clinical outcomes. Ann Pharmacotherapy. (2014) 48:1298–312. doi: 10.1177/1060028014543485
79. Avanecean D, Calliste D, Contreras T, Lim Y, Fitzpatrick A. Effectiveness of patient-centered interventions on falls in the acute care setting compared to usual care: a systematic review. JBI Datab System Rev Implement Reports. (2017) 15:3006–48. doi: 10.11124/JBISRIR-2016-003331
80. Mitchell MD, Lavenberg JG, Trotta RL, Umscheid CA. Hourly rounding to improve nursing responsiveness: a systematic review. J Nursing Administration. (2014) 44:462–72. doi: 10.1097/NNA.0000000000000101
81. Murni I, Duke T, Triasih R, Kinney S, Daley AJ, Soenarto Y. Prevention of nosocomial infections in developing countries, a systematic review. Paediatr Int Child Health. (2013) 33:61–78. doi: 10.1179/2046905513Y.0000000054
82. Safdar N, Abad C. Educational interventions for prevention of healthcare-associated infection: A systematic review. Crit Care Med. (2008) 36:933–40. doi: 10.1097/CCM.0B013E318165FAF3
83. Aboelela SW, Stone PW, Larson EL. Effectiveness of bundled behavioural interventions to control healthcare-associated infections: a systematic review of the literature. J Hospital Infection. (2007) 66:101–8. doi: 10.1016/j.jhin.2006.10.019
84. Vonberg RP, Gastmeier P. Hospital-acquired infections related to contaminated substances. J Hospital Infection. (2007) 65:15–23. doi: 10.1016/j.jhin.2006.09.018
85. Flanders SA, Collard HR, Saint S. Nosocomial pneumonia: State of the science. Am J Infect Control. (2006) 34:84–93. doi: 10.1016/j.ajic.2005.07.003
86. Savage JW, Anderson PA. An update on modifiable factors to reduce the risk of surgical site infections. Spine J. (2013) 13:1017–29. doi: 10.1016/j.spinee.2013.03.051
87. Schabrun S, Chipchase L. Healthcare equipment as a source of nosocomial infection: a systematic review. J Hospital Infection. (2006) 63:239–45. doi: 10.1016/j.jhin.2005.10.013
88. Amaratunga T, Dobranowski J. Systematic review of the application of lean and six sigma quality improvement methodologies in radiology. J Am College Radiol . (2016) 13:1088–95.e7. doi: 10.1016/j.jacr.2016.02.033
89. Snyder SR, Favoretto AM, Derzon JH, Christenson RH, Kahn SE, Shaw CS, et al. Effectiveness of barcoding for reducing patient specimen and laboratory testing identification errors: A Laboratory Medicine Best Practices systematic review and meta-analysis. Clin Biochem. (2012) 45:988–98. doi: 10.1016/j.clinbiochem.2012.06.019
90. Weerakkody RA, Cheshire NJ, Riga C, Lear R, Hamady MS, Moorthy K, et al. Surgical technology and operatingroom safety failures: A systematic review of quantitative studies. BMJ Quality and Safety. (2013) 22:710–8. doi: 10.1136/bmjqs-2012-001778
91. Bowers L, Banda T, Nijman H. Suicide inside: A systematic review of inpatient suicides. J Nervous Mental Disease. (2010) 198:315–28. doi: 10.1097/NMD.0b013e3181da47e2
92. Doupnik SK, Rudd B, Schmutte T, Worsley D, Bowden CF, McCarthy E, et al. Association of suicide prevention interventions with subsequent suicide attempts, linkage to follow-up care, and depression symptoms for acute care settings: a systematic review and meta-analysis. JAMA Psychiatry. (2020) 77:1021–30. doi: 10.1001/jamapsychiatry.2020.1586
93. Kim JM, Suarez-Cuervo C, Berger Z, Lee J, Gayleard J, Rosenberg C, et al. Evaluation of patient and family engagement strategies to improve medication safety. Patient. (2018) 11:193–206. doi: 10.1007/s40271-017-0270-8
94. Garrouste-Orgeas M, Philippart F, Bruel C, Max A, Lau N, Misset B. Overview of medical errors and adverse events. Ann Intensive Care. (2012) 2:2. doi: 10.1186/2110-5820-2-2
95. Khammarnia M, Ravangard R, Barfar E, Setoodehzadeh F. Medical Errors and Barriers to Reporting in Ten Hospitals in Southern Iran. Malays J Med Sci. (2015) 22:57–63. doi: 10.1155/2015/357140
96. Poorolajal J, Rezaie S, Aghighi N. Barriers to medical error reporting. Int J Preventive Med . (2015) 6:97. doi: 10.4103/2008-7802.166680
97. Morrison M, Cope V, Murray M. The underreporting of medication errors: A retrospective and comparative root cause analysis in an acute mental health unit over a 3-year period. Int J Ment Health Nurs. (2018) 27:1719–28. doi: 10.1111/inm.12475
98. Senders J. FMEA and RCA: the mantras; of modern risk management. BMJ Qual Saf. (2004) 13:249–50. doi: 10.1136/qshc.2004.010868
99. Tanaka M, Tanaka K, Takano T, Kato N, Watanabe M, Miyaoka H. Analysis of risk of medical errors using structural-equation modelling: a 6-month prospective cohort study. BMJ Quality Safety . (2012) 21:784–90. doi: 10.1136/bmjqs-2010-048330
100. Vardi A, Efrati O, Levin I, Matok I, Rubinstein M, Paret G, et al. Prevention of potential errors in resuscitation medications orders by means of a computerised physician order entry in paediatric critical care. Resuscitation. (2007) 73:400–6. doi: 10.1016/j.resuscitation.2006.10.016
Keywords: medical error, financial burden, hospital, intervention, quality of care, public health
Citation: Ahsani-Estahbanati E, Sergeevich Gordeev V and Doshmangir L (2022) Interventions to reduce the incidence of medical error and its financial burden in health care systems: A systematic review of systematic reviews. Front. Med. 9:875426. doi: 10.3389/fmed.2022.875426
Received: 22 April 2022; Accepted: 11 July 2022; Published: 27 July 2022.
Reviewed by:
Copyright © 2022 Ahsani-Estahbanati, Sergeevich Gordeev and Doshmangir. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Leila Doshmangir, doshmangirl@tbzmed.ac.ir
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
- Search Menu
- Sign in through your institution
- Author Guidelines
- Submission Site
- Why publish with JPHSR?
- Open Access Options
- Self-Archiving Policy
- Call for Papers
- About Journal of Pharmaceutical Health Services Research
- About the Royal Pharmaceutical Society
- Editorial Board
- Advertising & Corporate Services
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
Introduction, concept and incidence of medication errors, classification of medication errors, other classifications and types of medication errors, causes of medication errors, medication errors and nursing, results of medication errors, reporting medication errors of nurses, strategies for preventing medication errors, conclusion and recommendations, author contributions, conflict of interest.
- < Previous
Medication errors: a focus on nursing practice
- Article contents
- Figures & tables
- Supplementary Data
Nasr Alrabadi, Shaima Shawagfeh, Razan Haddad, Tareq Mukattash, Sawsan Abuhammad, Daher Al-rabadi, Rana Abu Farha, Suzan AlRabadi, Ibrahim Al-Faouri, Medication errors: a focus on nursing practice, Journal of Pharmaceutical Health Services Research , Volume 12, Issue 1, March 2021, Pages 78–86, https://doi.org/10.1093/jphsr/rmaa025
- Permissions Icon Permissions
Health departments endeavor to give care to individuals to remain in healthy conditions. Medications errors (MEs), one of the most types of medical errors, could be venomous in clinical settings. Patients will be harmed physically and psychologically, in addition to adverse economic consequences. Reviewing and understanding the topic of medication error especially by nurses can help in advancing the medical services to patients.
A search using search engines such as PubMed and Google scholar were used in finding articles related to the review topic.
This review highlighted the classifications of MEs, their types, outcomes, reporting process, and the strategies of error avoidance. This summary can bridge and open gates of awareness on how to deal with and prevent error occurrences. It highlights the importance of reporting strategies as mainstay prevention methods for medication errors.
Medication errors are classified based on multifaceted criteria and there is a need to standardize the recommendations and make them a central goal all over the globe for the best practice. Nurses are the frontlines of clinical settings, encouraged to be one integrated body to prevent the occurrence of medication errors. Thus, systemizing the guidelines are required such as education and training, independent double checks, standardized procedures, follow the five rights, documentation, keep lines of communication open, inform patients of drug they receive, follow strict guidelines, improve labeling and package format, focus on the work environment, reduce workload, ways to avoid distraction, fix the faulty system, enhancing job security for nurses, create a cultural blame-free workspace, as well as hospital administration, should support and revise processes of error reporting, and spread the awareness of the importance of reporting.
Health administrations, all over the world, endeavor to give proper care to individuals when they are ill or to remain healthy. Primary care services are increasingly concentrated at the heart of integrated people-centered health care systems in many countries. [ 1 ] They provide a passage point with a useful framework focused on progressing health planning to ensure safety for individuals and their families. Availability and safe application are basics to accomplish all-inclusive wellbeing criteria and to support the United Nations sustainable development goals, that organize solid lives and advance prosperity for all. [ 2 ]
The therapeutic services’ framework is very unpredictable. It includes basic circumstances of hazard, a collaboration between different experts and institutions, and relies upon huge help from innovations. The attributes of the therapeutic framework may increase the danger of slip-ups and compound the results of these mix-ups. [ 1 , 3 ] In this sense, it is vital to evaluate hazards and harm to patients in the scan for extreme patient wellbeing. The World Health Organization’s meaning of patient wellbeing builds up of which pointless damage or potential harm related to therapeutic services ought to be decreased to a worthy least. [ 4 ]
Healthcare providers consider patient safety one of the paramount priorities in clinical settings. One of the major threats to the well being of patients is medical errors. [ 5 ] One of the main branches of medical errors is medication errors which were demonstrated to be the source of morbidity and mortality in addition to the resulted adverse economic consequences. [ 6–8 ] Patient safety is esteemed as a critical issue for our social insurance framework and human services providers, [ 9 ] and in such manner, medication errors are utilized as a list to survey quiet wellbeing in clinics. In the next sections, we will go through the concept, classification, types, causes, consequences, reporting, and those strategic plans to prevent the occurrence of medication errors.
A medication error is characterized by ignoring the condition of shaping harm, hazard, or any evadable frequency to happen amid the procedure from medicine ordering to patient consumption. [ 10 , 11 ] It might be characterized by National Coordinating Council for Medication Error Reporting and Prevention (NCCMERP) as any preventable occasion that may cause, or prompt improper medicine use or patient harm while the medicine is in the control of the healthcare worker, patient, or buyer. [ 12 , 13 ] The measurement of medication errors may vary widely in clinical settings due to the different ways of recognizing and defining the status of medication errors, how to calculate error rates, variation in numerator/dominator, and the process, documentation, and culture of settings technologies. [ 14–16 ]
Medication errors are a global issue where 5.0% is deadly, and almost 50.0% of those are preventable. [ 17 ] The in-hospital incidence for adverse drug events was reported to be high which ranged from 2 to 6 events per 100 admissions. [ 18 , 19 ] Moreover, around 7000–9000 patients’ deaths in the USA each year can be attributed to medication errors. [ 11 , 20 ] However, the rate of patient serious injuries as a result of medication errors among different studies varies, 1–2%, [ 21 ] 9–13%, [ 22 ] 29.0% [ 23 ] and 51.8% [ 24 ] and almost 30.5% death rate per year in the United States because of medication errors. [ 25 ] As indicated by the Institute of Medicine (IOM) of the National Academies in 2006, 400 000 instances of avoidable patient damage because of medication errors happen every year in emergency clinics in the USA. It is noticed that 19% of medication errors in the Intensive Care Units (ICUs) are life-threatening and 42% are considered to be paramount for further maintaining treatment. [ 26 , 27 ] Somewhere in the range of 44 000 and 98 000 emergency clinic patients have been evaluated to kick the bucket every year because of drug errors. [ 28 ] For instance, in the USA hospitals in 1995, the annual spending on medication errors for each hospital was around 2.9 million dollars and a 17% reduction in the error incidence led to 480 000 dollars saving per hospital as in the case of transcription errors. [ 29 ] For example; a patient in an Iranian hospital had given 80 units of insulin instead of eight units which led to the patient’s death, therefore, the government gave 140 million dollars to the patient’s family. [ 14 , 30 ] Add up, the overall cost of adverse outcomes that are associated with medication errors could surpass 40$ billion each year. [ 11 ] Bates et al . stated that medication errors increase the costs for each patient by 2000–2500$ and extend their hospitalization period by at least two days. [ 18 ] The total cost of these errors, including expenses of error, disability, and lost income and productivity, is expected to be between $17 billion and $29 billion per year. [ 31 , 32 ]
Grouping of medication errors occurrence into contextual, modular, or mental (psychological) is considered an ideal protocol to assess how errors happen. Contextual order assesses the specific time, place, medications, and individuals who are included. Modular characterization analyses the manners in how errors occur (i.e, by omission, repetition, or substitution). Mental order is preferred, as it clarifies occasions as opposed to just prescribing them. Its burden is that it focuses on humans as opposed to frameworks wellsprings of errors. The accompanying mental grouping depends on crafted by Reason on errors and there are four distinct types of medication errors. [ 33 , 34 ]
The first type is ‘Knowledge-based errors’ (Learning absence). As it may seem, administering penicillin to the patient without any concise information whether the patient is unfavorably susceptible. Knowledge-based errors that are connected to any kind of knowledge which could be related to expert, specific, or general. As a general knowledge, health care providers should understand that allergic reactions, for instance, could be associated with penicillins, however, realizing that the patient is allergic to penicillin can be considered specific knowledge. On the other hand, experts are those who may know that co-fluampicil has penicillin. As a result, Knowledge-based errors might be provoked when ignoring any of that information. In an Australian examination, correspondence issues with trouble in getting to suitable medication dosing data added to knowledge-based errors. [ 35–39 ] When being educated about medication is being given dispensed to patients could reduce the incidence of medication errors. [ 40 ] Errors can be blocked from occurrence through computerized prescribing entry orders, bar-coded medicine frameworks, and cross-checking by others (for instance, medicine specialists and nurses). [ 41 , 42 ] A study showed that before implantation of electronic Bar-Coded Medication Administration (BCMA-e MAR), wrong time (33.9%), omission (27.7%), wrong technique (18.0%), wrong dose (13.3%), and unauthorized drug (2.9%) were happening frequently. However, after the implementation of BCMA- e MAR, errors have been declined. [ 43 ] In another study, error rates were reduced more than a half after applying BCMA- e MAR. [ 44 ]
The second type is ‘Rule-based errors’ (utilizing a terrible standard or twisting a decent principle). For instance, infusing diclofenac into the sidelong (lateral) thigh instead of being injected into the butt cheek. Appropriate standards and instruction help to keep away from these kinds of errors, as do computerized prescribing frameworks. [ 38 , 39 , 45–47 ]
The third type is ‘Activity-based errors’ (known as slips). For example, when confusion happens between two drugs like diazepam and diltiazem from a medicine store rack. [ 38 , 46 , 47 ] In the Australian examination, most errors were because of slips in consideration that happened amid routine prescribing, dispensing, and administering organization. Slips errors could be minimized through keeping away from distraction, by cross-checking, by naming prescriptions plainly, and by utilizing identifiers, for example, standardized identifications or barcoded); alleged ‘Tall Man’ lettering (when blending lower- and upper-case letters in the same word) which showed to be a good protocol in the prevention of misreading of names, yet tall-man lettering has not been assessed in genuine conditions. [ 48 ] A branch of specialized technical errors of activity-based errors, for instance, as seen in measuring the incorrect amount of potassium chloride into an infusion bottle. Using agendas, safeguard frameworks, and computerized updates could prevent this type of error from occurring. [ 49 , 50 ]
The fourth type is ‘Memory-based errors’ (so-called lapses). For instance, giving penicillin to a patient, with a known history of allergy, but forgetting that the patient is allergic. These are difficult to keep away from; however, computerized prescribing frameworks and cross-checking can reduce the error incidence. [ 50 , 51 ]
Errors might provoke in any stage. [ 52–54 ] Prescribing errors (during drug prescription), transcription errors (wrong/incomplete transfer information from a prescription), dispensing errors (disagreement between medicine dispensed and prescription), administration errors (during drug administration), discharge summaries errors (due to discrepancy between discharged summaries and medical records), and monitoring errors (while taking the medicine of renal and liver). [ 30 ] Karthikeyan et al . reviewed the occurrence of errors among healthcare providers. [ 55 ] (a) Prescribing errors; were presented as follow; drug-drug interaction (68.2%), incomplete prescription (25.0%), monitoring (12.6%), incorrect drug (13.0%), underdose (12.6%), incorrect interval (12.0%), and overdose (7.0%). (b) Nursing errors; as in wrong rate (34.0%), wrong time administration (28.6%), wrong dose (25.3%), medication omitted (24.0%), wrong fluid (22.4%), wrong drug (21.1%), wrong route (19.9%), and wrong patient (19.7%). (c) Pharmacist errors; as in wrong medication (25.0%), excessive dose (23.0%), poor labeling (23%), wrong dosage errors (21.8%), wrong strength (10.8%), wrong quantity (6.9%), and wrong direction dispensing (2.3%). [ 55 ] Prescription and administration types of medication errors are considered common and can contribute up to 65.0%–87.0% of medication errors. [ 56 ] According to the National Patient Safety Agency (2009) in the United Kingdom, it was observed the most prominent kinds of medication errors were 16.0% in prescribing, 18.0% in dispensing, and 50.0% in the drug administration. [ 57 ] Furthermore, medication errors accounted to be 37.6% of administration errors, 21.1% of prescription errors, and 10.0% of transcription errors in Iran. [ 58 ] On the other hand, previous studies showed that in prescription errors mainly occurred at outpatient ward accounted as (39.0–44.0%) and in emergency wards were (60.0–73.5%), however, transcription errors were accounted 16.9% and 13.8% for inpatient and discharged patients, respectively, while discharge summaries errors accounted 16.0–36.0% of (omission, drug name, administration route, drug dose, and drug regimen). [ 59 , 60 ] There were 192 477 medication errors reported by staff from 482 hospitals through voluntary reporting that could occur at any stage. Errors during administration were accounted to be (33.0%), documentation (23.0%), dispensing (22.0%), prescribing (21.0%), and monitoring (1.0%). Also, errors were related to omission (25.0%), dosage (30.0%), unauthorized drugs, and the wrong time, patient, and administration technique. [ 61 ]
Moreover, 0.078 errors per patient, and 0.029 errors per medication mainly because of dosing errors, drug omission, and wrong frequency errors. [ 62 ] A previous study showed that (94.0%) out of 430 errors were omissions and only 6.0% of errors caused a major impact on patients’ life but was not considered as a life–alarming errors. [ 63 ] Medication errors are also related to the problem of wrong phenomena. These incorporate errors of course of medication, doses, timing, patient, and inability to follow up the patient. [ 53 , 64 ]
Prescription errors are a standout amongst the most widely recognized therapeutic errors and their occurrence rate in adult ward accounted to be 5.6 cases per 1000 patients and 14.8 cases per 1000 patients in the pediatrics ward. [ 65 ] As seen, a sample of 57 nurses in pediatric settings, medication errors were 67.0% compared to 56.0% of a sample of 227 nurses working with adults. [ 64 , 65 ] The occurrence of prescription errors in pediatrics is three-times higher than adults. An examination in Canada showed that the number of children who admitted to the emergency clinic accounted to be 5000 because of medication errors and of these, 2500 experienced moderate to serious side effects. [ 66 ] Prescription errors can happen because of human errors just as from fundamental errors and thus is needed for a cautiously monitoring through medication organization. [ 10 ] It is suggested that at whatever point when medication error has occurred it should be reported to the significant manager, and such notice is essential for understanding the reasons for the errors and to enable strides to be taken to lessen such errors later on. [ 67 ] The most frequent types of prescribing errors might be related to the inability to manage the medication and mistaken medication writing. [ 68 ] On the other hand, certain variables add to the high rates of prescription errors in pediatric patients. These incorporate inability to peruse the remedy, distraction, high patient/nurture proportion, and hard to get the accessibility of the right medications as endorsed. [ 65 ] Few investigations have tended to show the rates and reasons for medication errors in grown-up patients, and these examinations have regularly been founded on reports from nursing staff. [ 69 , 70 ] Moreover, few investigations have inspected medication errors from the viewpoint of pediatric nurses. [ 65 ]
The error might be identified with expert practice, which is related to human services items, to systems, or to correspondence issues including prescribing, ordering, item naming, labeling/packaging, preparation, compounding, dispensing, administration, education, and the best possible utilization of medicines. [ 2 , 11 , 71 ]
Patients are sometimes being harmed by incidents despite the safe and effective health services that are provided to them. Medication errors have been considered a global issue and it is essential to focus on the causes, results, and solutions. [ 11 , 72 ] The proportion of medication errors among nurses varies in different studies, it was 57.4% in Ethiopia, [ 16 ] 42.1% in Jordan, [ 15 ] 41.9% in Australia, [ 73 ] and 28.9% in the USA. [ 38 ] Thus, differences in rate are due to differences in organizational reporting systems, and the time frame of studies that have been conducted. Medication errors incorporate not just undesirable impacts from prescriptions, yet additionally incorporate ordering, transcription, dispensing, administration and organization mistakes. [ 11 , 74 ] Medication errors are more barely characterized than unfavorable medication occasions and incorporate mistakes of commission and omission. Errors of commission happen while abusing one of the five privileges of organization: right medication, patient, portion, course, time, and documentation. An error of omission is a mistake that consists of not doing something you should have done, or not including something such as an amount of fact that should be included, or when the patient does not get a drug that was arranged. [ 75 ] In a survey conducted on 1384 nurses in 24 ICUs in the United States hospitals regarding nurses’ perception of medication errors, [ 76 ] the main causes contributing to medication errors are illegible handwriting, mental and physical health, interruption and distraction from patient and co-workers, lack of pharmacological knowledge with problems in calculations, performance deficit, sometimes lab tests are not considered, overtime of working hours, absence of self-awareness, organizational factors (training) and failure to follow protocols. [ 15 , 46 , 53 , 77–88 ] Furthermore, it could be related to execution deficit (36.7%) and impairment of strategies realization, but knowledge, communication, drug distribution, and entry system were accounted for lesser percentages. [ 78 , 89 ] However, interruptions play a big impact on causing medication errors especially during administration. [ 46 ] As it may seem, 1354 errors occurred in 136 hours, which means 10 interruptions per hour. [ 90 ] Besides, registered nurses were interrupted (36.0–57.0%), which accounted from the patients (28.0%), other nurses (25.0%), assistive personnel (10.0%), and physician (9.0%), that led to 7.0% of medication errors from interruptions. [ 65 , 79 ] Moreover, around 20% of hospital registered nurses experienced frequent medication errors because of factors as overload, extra hours, unsatisfactory staffing with low support, and shift length. [ 91 ]
Lack of knowledge and miscalculation of doses are the factors contributing to medication errors. [ 36 , 37 , 39 ] It is noticed that competence skills in drug calculation are prerequisites to nursing registration and examining their learning abilities rather than follow strict protocol which imped nurses thinking skills. [ 11 , 92 ] Moreover, focusing on continuing education with clinical and theoretical support will help in the prevention of medication error occurrence. [ 15 , 93–95 ]
Medication errors are normally characterized as deviations from a doctor’s structure. Sources of errors could be from ordering, prescribing, transcription, dispensing, and administration errors (i.e. when the patient is administered a wrong medicine). Healthcare providers as doctors, medical specialists, pharmacists, unit assistants, and nurses could be related to the incidence of medication errors. [ 96 ] A patient can get up to 18 portions of prescription for each day, and a healthcare provider can regulate upwards of 50 medications for each move. [ 50 , 97 ] This places the healthcare provider at the forefront of administration accountability. [ 98 ]
Nurses are considered critical agents among the medical staff of clinics. One of the real undertakings of nurses is administering medicines to patients. They should be mindful of recognition significance of organized prescription to dodge potential dangers and conceivable complexities coming about because of medicine errors. [ 99 ]
Medication errors in clinics, for the most part, include 3.0–6.9% of hospitalized patients. [ 100 ] Customarily, to maintain a strategic distance from medicine errors, nurses utilized five privileges of the prescription organization; the correct patient, the correct medicine, the correct portion, the correct course, and the ideal time. Following this rule before giving any prescription, can help nurses keep away from the vast majority of medication errors. [ 30 , 52 ]
Most medicine executives are nurses and, in this manner, when errors happen, nurses are frequently considered responsible. [ 101 ] Medicine supervisors can give defend against errors made at any of the past stages, notwithstanding, and are thought to block around 86.0% of errors made by prescribers or medicine specialists. [ 102 , 103 ] Along these lines, nurses give a security guard against medication errors at the same time, can put patients in danger. [ 104 ]
Nurses have a central role in their activities to advance safety and anticipate damage to patients. [ 103 , 105 ] While this of great practice, nurses ought to assess how they work in groups to guarantee that the aggregate frameworks and procedures of training are sheltered and to help and instruct unpracticed partners. [ 46 ]
Even though that the way toward conveying medication to patients requires a joint effort between medical experts, registered nurses, and pharmacists, it is the essential obligation of healthcare providers to protect prescription administration. As indicated by Anderson and Webster administering prescription is the most noteworthy hazard undertaking a nurse can perform and can prompt destroying ramifications for the patient and the nurses’ vocation. [ 106 ] Besides, the mental injury brought about by submitting a medication error can be overpowering to the nurses, they may feel agitated, blameworthy, and panicked. [ 46 ] Therefore, medication errors might not only intend harm to patients, they additionally deface the notoriety of all medical experts in whom patients place their trust. [ 107 , 108 ]
On the off chance that nurses don’t have the fundamental capability on providing important data and capacity for the protection of human wellbeing and life, thus therapeutic errors wind up unavoidable. Notwithstanding these, reasons, for example, numerical deficiency of nurses in the workplace, persistent conditions, restlessness, tiredness, absence of consideration, unsure employment definition, insecure working hours, improper physical conditions, having an extraordinary number of patients, could trigger medication errors. [ 38 , 46 , 53 ]
Execution of medical requests is a critical piece of recovery procedure and patient consideration. Nursing execution is considered a prominent role that impacts patients’ safety. [ 109 ] Certain consequences as an impact on patient safety and treatment expenses will have resulted from medication errorss. [ 110 ] Administration of drugs is likely a standout amongst the most basic missions of nurses since the subsequent errors may have unintended, genuine complication for the patient. [ 111 ] Medication errors can prompt unfriendly results, for example, increased mortality, increased length of hospital stay, and expanded restorative expenses. [ 112 ] Although medication errors can be brought about by all individuals from healthcare providers. Most medical and therapeutic executions are done with the nurses, therefore, nursing medication errors are the most common. Besides, nurses execute most of the therapeutic requests and invest about 40.0% of their energy in the emergency clinic to manage medicines. [ 113 ] In developing and developed countries, the nursing medication error rate is observed to be high. [ 114 ]
Medical nurses are a fundamental piece of the human services group and are in charge of the wellbeing of patients yet sadly, the expansion in complaining from medical nurses and doctors in the previous years is proof of expanded frequency of errors. [ 53 ] On the other hand, no examinations have exhibited solid connections between nurse’s qualities (i.e. age, long stretches of training, and education) and the number of medication errors. [ 115 ] This would appear to show that nurses are conceivably in danger of making a medication error.
It is critical to identify medication error, regardless of whether vital or not, because of identification the error will uncover a disappointment in the treatment procedure which causes another event of hurt. There is additional proof that the demise rate from medication errors is expanding. These increments are not amazing as of late emergency clinics have seen an expanded rate of patients, new medications have developed that are progressively hard to utilize securely and viably, factors that will in general lead to increment the danger of medicine error. [ 116 , 117 ]
At the point when errors are distinguished, they can cause many disappointments because of the inability of how to deal with the resulting error, and they might cause potential harm to patients with disabilities. The backhanded results incorporate harm to the medical nurses as far as an expert and individual circumstances, decreased self-assurance, expanded pressure and clashes at work, lack of quality of the patient’s family to nurse. [ 118 , 119 ] Hence, the need to bring issues to interpret and manipulate the nature and reasons of errors is fundamental and can help nursing chiefs to recognize plans for improving the nature of medication administration, expanding the patient wellbeing, and lessening the extra cost. [ 120 ]
Handling medication is a high-recurrence movement in nursing; the potential for error increments when the normal number of prescriptions builds. Besides, prescription administration is an intricate procedure that is frequently performed under not exactly perfect conditions. Thus, the continuous flow of multifaceted prescriptions could prompt the occurrence of the hazard. [ 11 , 74 ] There is likewise a propensity to accuse people instead of the faulty system. Be that as it may, most medication errors emerge from the requests of doctors, trailed by medical organizations. [ 11 , 121 ]
A previous study about the report referring to the United Kingdom (UK) restorative safeguard associations, showed that 25.0% of all cases were because of prescription errors that included the following accompanying errors: [ 122 ] prescribing and administration errors (miscalculation, contraindicated or unlicensed medication, a wrong dose, or wrong patient), repeat dispensing without legitimate checks, failure to monitor the case, and failure to caution about antagonistic impacts (which may be that as it may, not be viewed as a medicine error).
Reporting the medication errors is critical in improving the medication management process, therefore, it is considered a legal and ethical commitment in each health care settings. Reporting medication errors could provide an effective resource of important information, therefore underreporting errors is observed as a crucial threat. [ 81 , 123 , 124 ] Regardless of whether the nurse is the wellspring of a mistake, a benefactor, or a spectator, associations depend on medical nurses as bleeding-edge staff to perceive and report medication errors. [ 15 ] A previous examination has exhibited underreporting among nurses. Adding to the weight of announcing, over 90.0% are oneself reports. [ 125 ] Moreover, in Israel, 26.0% of medication errors were reported, and 46% were self-reported. [ 126 ] In Taiwan, almost 6000 to 20000 deaths from medication errors, and 10.0% of medical lawsuits were mainly of underreporting. [ 127 ] In Turkey, 66.7% of involved nurses who caused medication errors did not report it. [ 128 ]
Medication administration is a high-risk area of nursing practice. Thus, reporting a medication error is an important step based on awareness and willingness to report it. [ 127 , 129 ] This barrier might be provoked, yet focus on the person rather than a system with fear from adverse outcomes lead to underreporting data. [ 11 , 38 , 52 , 61 , 65 , 77 , 130 ]
Precise detailing of medication errors could result in the avoidance of medication errors. Revealing prescription mistakes is reliant on the nurse’s decision making. Underreporting or not announcing medicine mistakes covers defective frameworks. [ 124 ] Besides, developing structured protocols on drug administration with an un-punitive approach could encourage reporting and improve patient safety. [ 131 ]
At present, self-revealed medication errors give negligible data to associations since disparities, as far as answered to-actual rates, are across the board. Medication errors are normally reported through institutional reporting frameworks, for example, incident reports to give information about the medication errors. [ 132 ]
Reports are created by the medical nurse who distinguishes the error and afterward is sent to the executives, quality divisions, or board offices of hazard. Detailing and reporting the issue is subject to the medical nurse in many ways: [ 117 ] capacity to perceive a mistake has happened, the conviction that the mistake warrants reporting, the conviction that she/he has submitted the error, and eagerness to beat the humiliation and dread of striking back for having submitted a medication error.
Nurses specifically are imperative in evaluating such errors since they are, for the most part, in a situation to see medication errors directly and find a way to lessen the danger of medication errors. [ 133 ] Their uncommon position is regularly fortified by their continuous learning concerning the medications in addition to their strategies regarding planning and controlling the medicines and for checking the impacts of the treatment. [ 11 ] All nurses must get comfortable with different methodologies to forestall or diminish the probability of medication errors. Here are certain techniques to follow:
1. Guarantee the five privileges of the prescription organization
Nurses must guarantee that institutional approaches identified with prescription interpretation are pursued. It isn’t adequate to translate the medicine as prescribed, however, to guarantee the right medicine is recommended for the right patient, right time, the right measurements, through the right course, and planned effectively (otherwise called the five rights). [ 88 , 134 ]
2. Pursue legitimate medication reconciliation techniques
Foundations must have instruments set up for medicine reconciliation while exchanging a patient starting with one establishment then onto the next or starting with one unit then onto the next in a similar organization. Audit and check every prescription for the right patient, right medicine, right measurements, right course, and right time against the exchange (transfer) requests, or medications recorded on the exchange archives. Nurses must contrast this with the Medication Administration Record (MAR). Frequently not all components of a medicine record are accessible for simple confirmation, yet it is of central significance to check with each conceivable source including the releasing or exchanging establishment/unit, the patient or patient’s family, and doctor, to forestall potential mistakes identified with inappropriate reconciliation. [ 135 ]
3. Have the doctor (or other nurses) read it back
This is a procedure whereby a nurse peruses back a request to the recommending doctor to guarantee the arranged medicine is deciphered accurately. This procedure can likewise be completed starting with one medical nurse then onto the next whereby a medical nurse peruses back a request deciphered to the doctor’s structure to another medical nurse as the MAR is checked on to guarantee precision. [ 136 ]
4. Document everything
This incorporates legitimate medicine naming, clear documentation, or appropriate recording of administered medicine. An absence of appropriate documentation for any prescription can result in an error. For instance, a nurse neglecting to report an as required prescription can result in another administration being directed by another healthcare provider since no documentation signifying past administration exists. Perusing the medicine name/label and expiration date of the medicine is additionally another best practice. A right prescription can have a wrong mark or the other way around, and this can likewise prompt a medicine error. [ 11 , 137 ]
5. Guarantee appropriate storage of medications for legitimate adequacy
Health care providers should avoid the medication storage with close or identical names or package on them at the same medication stock rack. Alphabetized drug storage could lead to unintentional confusion. Besides, it is essential to separate ‘high alert’ medications from other medications to avoid ambiguity. Medications that ought to be refrigerated must be kept refrigerated to look after adequacy, and medications that ought to be kept at room temperature ought to be put away in like manner. Most biologicals items require refrigeration, and if a multi-dose vial is utilized, it must be named to guarantee it isn’t utilized past its lapse/expiration date from the date it was opened. Thus, it is recommended to keep it organized and control access to it. [ 138 , 139 ]
6. Consider having a drug guide accessible consistently
Regardless of whether it’s print or electronic is a matter of personal (or institutional) inclination, however, both are similarly significant in giving imperative data on most classifications of prescription, including trade/generic names, therapeutic class, dosing, nursing consideration, side effect, drug-drug interaction and medication cautionary, for example, ‘don’t crush, or give with the meal’. [ 140 ]
7. Know institution policies, regulations, and guidelines
Nurses should be familiar with the policies and guidelines and how to apply them. Since these regulations and policies could provide necessary information regarding drug ordering, transcription, administration, and documentation. Besides, it could provide information for the nurses about black box warnings, look alike, sound alike, and warning labels. [ 138 , 141 ]
As penultimate, medication errors are multifaceted criteria. It is motivated to standardize the recommendation and make it a central goal all over the globe for the best practice. Thus, it is suggested to; (a) get a deeper meaning of the medication errors concept, (b) focus on broader causes outside of the taken picture, (c) converge on clinical settings variations and patient illness severity, (d) include questions related to nurse’s psychology, (c) create a group of expert to publish new guidelines internationally adapted to any changes according to hospital needs. Nurses are the heart of clinical settings, encouraged to be one integrated body to prevent the occurrence of medication errors. Thus, systemizing the guidelines are required such as education and training, independent double checks, standardized procedures, follow the five rights, documentation, keep lines of communication open, inform patients of drug they receive, follow strict guidelines, improve labeling and package format, focus on the work environment, reduce workload, ways to avoid distraction, fix the faulty system, enhancing job security for nurses, create a cultural blame-free workspace, as well as hospital administration, should support and revise processes of error reporting, and spread the awareness of the importance of reporting.
Initiating the idea of the manuscript: Nasr Alrabadi and Razan Haddad. Writing the first draft: Shaima Shawagfah, Nasr Alrabadi, Suzan AlRabadi, Razan Haddad, Daher Al-rabadi, and Tareq Mukattash. Reviewing and approving the final draft: Nasr Alrabadi, Sawsan Abuhammad, Rana Abu Farha, and Ibrahim Al-Faouri.
Not applicable.
The authors declared no conflict of interest.
Simsekler MCE , Ward JR , Clarkson PJ . Design for patient safety: a systems-based risk identification framework . Ergonomics 2018 ; 61 : 1046 – 64 .
Google Scholar
World Health Organization (WHO) . Medication Errors . 2016 . https://apps.who.int/iris/handle/10665/252274
Google Preview
Rosa MB , Perini E . Erros de medicação: quem foi . Rev Assoc Med Bras 2003 ; 49 : 335 – 41 .
Safety WP , Organization WH . Conceptual framework for the international classification for patient safety version 1.1: final technical report January 2009 . Geneva : World Health Organization , 2010 . Report No.: 606940937X.
Prot S , Fontan JE , Alberti C et al. . Drug administration errors and their determinants in pediatric in-patients . Int J Qual Health Care 2005 ; 17 : 381 – 9 .
Kohn LT , Corrigan J , Donaldson MS. To Err is Human: Building a Safer Health System . Washington, DC : National Academy Press , 2000 .
Alrabadi N , Haddad R , Haddad R et al. . Medication errors among registered nurses in Jordan . J Pharm Health Serv Res 2019 ; 11 : 237 – 43 .
Pham JC , Story JL , Hicks RW et al. . National study on the frequency, types, causes, and consequences of voluntarily reported emergency department medication errors . J Emerg Med 2011 ; 40 : 485 – 92 .
Alsulami Z , Choonara I , Conroy S . Paediatric nurses’ adherence to the double-checking process during medication administration in a children’s hospital: an observational study . J Adv Nurs 2014 ; 70 : 1404 – 13 .
Berlin J , McCarver D , Notterman D et al. . Prevention of medication errors in the pediatric inpatient setting . Pediatrics 1998 ; 102 : 428 – 30 .
Tariq RA , Scherbak Y. Medication Errors . StatPearls [Internet] : StatPearls Publishing , 2019 .
Reporting NCCfME, Prevention . NCC MERP Taxonomy of Medication Errors . Rockville : Ncc MERP , 1998 .
Fahmy S , Garfield S , Furniss D et al. . A comparison of two methods of assessing the potential clinical importance of medication errors . Safety in Health 2018 ; 4 : 1 – 4 .
Moyen E , Camiré E , Stelfox HT . Clinical review: medication errors in critical care . Crit Care 2008 ; 12 : 208 .
Mrayyan MT , Shishani K , Al-Faouri I et al. . Nurses’ perceptions of medication errors in Jordan . Jordan Med J 2008 ; 42 : 92 – 105 .
Jember A , Hailu M , Messele A et al. . Proportion of medication error reporting and associated factors among nurses: a cross sectional study . BMC Nurs 2018 ; 17 : 9 .
Nuckols TK , Bell DS , Liu H et al. . Rates and types of events reported to established incident reporting systems in two US hospitals . Qual Saf Health Care 2007 ; 16 : 164 – 8 .
Bates DW , Boyle DL , Vander Vliet MB et al. . Relationship between medication errors and adverse drug events . J Gen Intern Med 1995 ; 10 : 199 – 205 .
Alsulami Z , Conroy S , Choonara I . Medication errors in the Middle East countries: a systematic review of the literature . Eur J Clin Pharmacol 2013 ; 69 : 995 – 1008 .
Starfield B . Is US health really the best in the world? JAMA 2000 ; 284 : 483 – 5 .
Nebeker JR , Barach P , Samore MH . Clarifying adverse drug events: a clinician’s guide to terminology, documentation, and reporting . Ann Intern Med 2004 ; 140 : 795 – 801 .
Anselmi ML , Peduzzi M , Dos Santos CB . Errors in the administration of intravenous medication in Brazilian hospitals . J Clin Nurs 2007 ; 16 : 1839 – 47 .
Donchin Y , Gopher D , Olin M et al. . A look into the nature and causes of human errors in the intensive care unit . BMJ Qual Saf 2003 ; 12 : 143 – 7 .
Agalu A , Ayele Y , Bedada W et al. . Medication administration errors in an intensive care unit in Ethiopia . Int Arch Med 2012 ; 5 : 15 .
Haw C , Stubbs J , Dickens GL . Barriers to the reporting of medication administration errors and near misses: an interview study of nurses at a psychiatric hospital . J Psychiatr Ment Health Nurs 2014 ; 21 : 797 – 805 .
Tissot E , Cornette C , Demoly P et al. . Medication errors at the administration stage in an intensive care unit . Intensive Care Med 1999 ; 25 : 353 – 9 .
Wilmer A , Louie K , Dodek P et al. . Incidence of medication errors and adverse drug events in the ICU: a systematic review . Qual Saf Health Care 2010 ; 19 : e7 .
Errors PM . Quality Chasm Series. In: Aspden P , Wolcott J , Bootman JL , Cronenwett LR , (eds.), Committee on Identifying and Preventing Medication Errors. Institute of Medicine , 2006 .
Bates DW , Leape LL , Cullen DJ et al. . Effect of computerized physician order entry and a team intervention on prevention of serious medication errors . JAMA 1998 ; 280 : 1311 – 6 .
Riaz MK , Riaz M , Latif A . Review - medication errors and strategies for their prevention . Pak J Pharm Sci 2017 ; 30 : 921 – 8 .
Institute of Medicine (US) Committee on Quality of Health Care in America In: Kohn LT, Corrigan JM, Donaldson MS (eds.), To Err is Human: Building a Safer Health System . Washington, DC: National Academies Press , 2000 .
Cheragi MA , Manoocheri H , Mohammadnejad E et al. . Types and causes of medication errors from nurse’s viewpoint . Iran J Nurs Midwifery Res 2013 ; 18 : 228 – 31 .
Reason J. Human Error . Cambridge: Cambridge University Press , 1990 .
Aronson JK . Medication errors: definitions and classification . Br J Clin Pharmacol 2009 ; 67 : 599 – 604 .
Nichols P , Copeland TS , Craib IA et al. . Learning from error: identifying contributory causes of medication errors in an Australian hospital . Med J Aust 2008 ; 188 : 276 – 9 .
Polifroni EC , McNulty J , Allchin L . Medication errors: more basic than a system issue . J Nurs Educ 2003 ; 42 : 455 – 8 .
Wilson A . Nurses’ maths: researching a practical approach . Nurs Stand 2003 ; 17 : 33 – 6 .
Ulanimo VM , O’Leary-Kelley C , Connolly PM . Nurses’ perceptions of causes of medication errors and barriers to reporting . J Nurs Care Qual 2007 ; 22 : 28 – 33 .
Carlton G , Blegen MA . Medication-related errors: a literature review of incidence and antecedents . Annu Rev Nurs Res 2006 ; 24 : 19 – 38 .
Likic R , Maxwell SR . Prevention of medication errors: teaching and training . Br J Clin Pharmacol 2009 ; 67 : 656 – 61 .
Agrawal A , Wu W , Khachewatsky I , (eds.). Evaluation of an electronic medication reconciliation system in inpatient setting in an acute care hospital. In: Medinfo 2007: Proceedings of the 12th World Congress on Health (Medical) Informatics, Building Sustainable Health Systems, IOS Press , 2007 .
Poon EG , Keohane CA , Yoon CS et al. . Effect of bar-code technology on the safety of medication administration . N Engl J Med 2010 ; 362 : 1698 – 707 .
Seibert HH , Maddox RR , Flynn EA et al. . Effect of barcode technology with electronic medication administration record on medication accuracy rates . Am J Health Syst Pharm 2014 ; 71 : 209 – 18 .
Naidu MaA , Y . Impact of bar-code medication administration and electronic medication administration record system in clinical practice for an effective medication administration process . Health 2019 ; 11 : 511 – 26 .
Frush K , Hohenhaus S , Luo X et al. . Evaluation of a Web-based education program on reducing medication dosing error: a multicenter, randomized controlled trial . Pediatr Emerg Care 2006 ; 22 : 62 – 70 .
Mayo AM , Duncan D . Nurse perceptions of medication errors: what we need to know for patient safety . J Nurs Care Qual 2004 ; 19 : 209 – 17 .
Keers RN , Williams SD , Cooke J et al. . Understanding the causes of intravenous medication administration errors in hospitals: a qualitative critical incident study . BMJ Open 2015 ; 5 : e005948 .
David U , Cohen MR . A tall man lettering project to enhance medication safety . Farm Hosp 2011 ; 35 : 223 – 4 .
Filik R , Purdy K , Gale A et al. . Labeling of medicines and patient safety: evaluating methods of reducing drug name confusion . Hum Factors 2006 ; 48 : 39 – 47 .
Radley DC , Wasserman MR , Olsho LE et al. . Reduction in medication errors in hospitals due to adoption of computerized provider order entry systems . J Am Med Inform Assoc 2013 ; 20 : 470 – 6 .
Aronson JK . Medication errors resulting from the confusion of drug names . Expert Opin Drug Saf 2004 ; 3 : 167 – 72 .
Stetina P , Groves M , Pafford L . Managing medication errors–a qualitative study . Medsurg Nurs 2005 ; 14 : 174 – 8 .
Tang FI , Sheu SJ , Yu S et al. . Nurses relate the contributing factors involved in medication errors . J Clin Nurs 2007 ; 16 : 447 – 57 .
Abukhader I , Abukhader K . Effect of medication safety education program on intensive care nurses’ knowledge regarding medication errors . J Biosci Med 2020 ; 8 : 135 – 47 .
Karthikeyan M , Balasubramanian T , Khaleel MI et al. . A systematic review on medication errors . Int J Drug Dev Res 2015 ; 7 : 9 – 11 .
Al-Shara M . Factors contributing to medication errors in Jordan: a nursing perspective . Iran J Nurs Midwifery Res 2011 ; 16 : 158 – 61 .
Al-Faouri IG , Hayajneh WA , Habboush DM . A five years retrospective study of reported medication incidents at a Jordanian teaching hospital: patterns and trends . Int J Humanit Soc Sci 2014 ; 4 : 280 – 7 .
Vazin A , Zamani Z , Hatam N . Frequency of medication errors in an emergency department of a large teaching hospital in southern Iran . Drug Healthc Patient Saf 2014 ; 6 : 179 – 84 .
Ghaleb MA , Barber N , Franklin BD et al. . Systematic review of medication errors in pediatric patients . Ann Pharmacother 2006 ; 40 : 1766 – 76 .
Hicks RW , Cousins DD , Williams RL . Selected medication-error data from USP’s MEDMARX program for 2002 . Am J Health Syst Pharm 2004 ; 61 : 993 – 1000 .
Rothschild JM , Churchill W , Erickson A et al. . Medication errors recovered by emergency department pharmacists . Ann Emerg Med 2010 ; 55 : 513 – 21 .
Berdot S , Sabatier B , Gillaizeau F et al. . Evaluation of drug administration errors in a teaching hospital . BMC Health Serv Res 2012 ; 12 : 60 .
Thomas B , Paudyal V , MacLure K et al. . Medication errors in hospitals in the Middle East: a systematic review of prevalence, nature, severity and contributory factors . Eur J Clin Pharmacol 2019 ; 75 : 1269 – 82 .
Stratton KM , Blegen MA , Pepper G et al. . Reporting of medication errors by pediatric nurses . J Pediatr Nurs 2004 ; 19 : 385 – 92 .
Kozer E , Scolnik D , Macpherson A et al. . Variables associated with medication errors in pediatric emergency medicine . Pediatrics 2002 ; 110 : 737 – 42 .
Fernald DH , Pace WD , Harris DM et al. . Event reporting to a primary care patient safety reporting system: a report from the ASIPS collaborative . Ann Fam Med 2004 ; 2 : 327 – 32 .
Otero P , Leyton A , Mariani G et al. . ; Patient Safety Committee . Medication errors in pediatric inpatients: prevalence and results of a prevention program . Pediatrics 2008 ; 122 : e737 – 43 .
Wakefield BJ , Blegen MA , Uden-Holman T et al. . Organizational culture, continuous quality improvement, and medication administration error reporting . Am J Med Qual 2001 ; 16 : 128 – 34 .
Rai DR , Devi NS. The knowledge regarding pediatric drug calculation among the staff nurses . Pharma Innovation , 2019 ; 8 : 444 – 9 .
Cousins DD , Heath WM . The National Coordinating Council for Medication Error Reporting and Prevention: promoting patient safety and quality through innovation and leadership . Jt Comm J Qual Patient Saf 2008 ; 34 : 700 – 2 .
Frankel A , Gandhi TK , Bates DW . Improving patient safety across a large integrated health care delivery system . Int J Qual Health Care 2003 ; 15 Suppl 1 : i31 – 40 .
Evans SM , Berry JG , Smith BJ et al. . Attitudes and barriers to incident reporting: a collaborative hospital study . Qual Saf Health Care 2006 ; 15 : 39 – 43 .
Wakefield DS , Wakefield BJ , Uden-Holman T et al. . Understanding why medication administration errors may not be reported . Am J Med Qual 1999 ; 14 : 81 – 8 .
Grober ED , Bohnen JM . Defining medical error . Can J Surg 2005 ; 48 : 39 – 44 .
Wakefield BJ , Wakefield DS , Uden-Holman T et al. . Nurses’ perceptions of why medication administration errors occur . Medsurg Nurs 1998 ; 7 : 39 – 44 .
Rogers AE , Hwang WT , Scott LD et al. . The working hours of hospital staff nurses and patient safety . Health Aff 2004 ; 23 : 202 – 12 .
Winterstein AG , Johns TE , Rosenberg EI et al. . Nature and causes of clinically significant medication errors in a tertiary care hospital . Am J Health Syst Pharm 2004 ; 61 : 1908 – 16 .
Pape TM . The effect of a five-part intervention to decrease omitted medications . Nurs Forum 2013 ; 48 : 211 – 22 .
Walters JA . Nurses’ perceptions of reportable medication errors and factors that contribute to their occurrence . Appl Nurs Res 1992 ; 5 : 86 – 8 .
Osborne J , Blais K , Hayes JS . Nurses’ perceptions: when is it a medication error? J Nurs Adm 1999 ; 29 : 33 – 8 .
O’Shea E . Factors contributing to medication errors: a literature review . J Clin Nurs 1999 ; 8 : 496 – 504 .
Hand K , Barber N . Nurses’ attitudes and beliefs about medication errors in a UK hospital . Int J Pharm Pract 2000 ; 8 : 128 – 34 .
Mansouri A , Ahmadvand A , Hadjibabaie M et al. . A review of medication errors in iran: sources, underreporting reasons and preventive measures . Iran J Pharm Res 2014 ; 13 : 3 – 17 .
Deans C . Medication errors and professional practice of registered nurses . Collegian 2005 ; 12 : 29 – 33 .
Reason J . Human error: models and management . BMJ 2000 ; 320 : 768 – 70 .
Asensi-Vicente J, Jiménez-Ruiz I, Vizcaya-Moreno MF. Medication Errors Involving Nursing Students: A Systematic Review . Nurse Educ , 2018 ; 43 : E1 – 5 .
Hewitt P . Nurses’ perceptions of the causes of medication errors: an integrative literature review . Medsurg Nurs 2010 ; 19 : 159 – 67 .
Frith KH , Anderson EF , Tseng F et al. . Nurse staffing is an important strategy to prevent medication errors in community hospitals . Nurs Econ 2012 ; 30 : 288 .
Kalisch BJ , Aebersold M . Interruptions and multitasking in nursing care . Jt Comm J Qual Patient Saf 2010 ; 36 : 126 – 32 .
Wilkins K , Shields M . Correlates of medication error in hospitals . Health Rep 2008 ; 19 : 7 – 18 .
Sabin M. Competence in Practice Based Calculation: Issues for Nurse Education . Edinburgh : Napier University , 2001 .
Wolf ZR , Haakenson DA , Jablonski RA et al. . Nurses’ perceptions of harmful outcomes from medication errors . Medsurg Nurs 1995 ; 4 : 460 – 7, 471 .
Manias E , Bullock S . The educational preparation of undergraduate nursing students in pharmacology: clinical nurses’ perceptions and experiences of graduate nurses’ medication knowledge . Int J Nurs Stud 2002 ; 39 : 773 – 84 .
Gorgich EA , Barfroshan S , Ghoreishi G et al. . Investigating the causes of medication errors and strategies to prevention of them from nurses and nursing student viewpoint . Glob J Health Sci 2016 ; 8 : 54448 .
Fontan JE , Maneglier V , Nguyen VX et al. . Medication errors in hospital: computerized unit dose drug dispensing system versus ward stock distribution system . Pharm World Sci 2003 ; 25 : 112 – 7 .
Morris S . Who’s to blame? Nursing 1991 ; 4 : 8 .
Benner P , Sheets V , Uris P et al. . Individual, practice, and system causes of errors in nursing: a taxonomy . J Nurs Adm 2002 ; 32 : 509 – 23 .
Morales-González M , Galiano MG . Predesigned labels to prevent medication errors in hospitalized patients: a quasi-experimental design study . Medwave 2017 ; 17 : e7038 .
SHoHani M , Tavan H . Factors affecting medication errors from the perspective of nursing staff . J Clin Diagn Res 2018 ; 12 : IC01 – 4 .
Burke KG . Executive summary: the state of the science on safe medication administration symposium . J Infus Nurs 2005 ; 28 : 87 – 92 .
Leape LL , Bates DW , Cullen DJ et al. . Systems analysis of adverse drug events. ADE Prevention Study Group . JAMA 1995 ; 274 : 35 – 43 .
Soori S , Rostami Z , Aghilidehkordi G . Occurrence and reporting of nurses’ medication errors in a teaching hospital in Isfahan . J Health Admin 2019 ; 21 : 75 – 86 .
Pape TM , Guerra DM , Muzquiz M et al. . Innovative approaches to reducing nurses’ distractions during medication administration . J Contin Educ Nurs 2005 ; 36 : 108 – 16; quiz 141–2 .
Valentin A , Capuzzo M , Guidet B et al. . ; Research Group on Quality Improvement of the European Society of Intensive Care Medicine (ESICM); Sentinel Events Evaluation (SEE) Study Investigators . Errors in administration of parenteral drugs in intensive care units: multinational prospective study . BMJ 2009 ; 338 : b814 .
Anderson DJ , Webster CS . A systems approach to the reduction of medication error on the hospital ward . J Adv Nurs 2001 ; 35 : 34 – 41 .
Carothers NB . Medication errors: the problem and its scope . Int J Trauma Nurs 1998 ; 4 : 104 – 8 .
Härkänen M , Turunen H , Vehviläinen-Julkunen K . Differences between methods of detecting medication errors: a secondary analysis of medication administration errors using incident reports, the global trigger tool method, and observations . J Patient Saf 2020 ; 16 : 168 – 76 .
Cheraghi MA , Nasabadi N , Reza A et al. . Medication errors among nurses in intensive care units (ICU) . Journal of Mazandaran University of Medical Sciences 2012 ; 21 : 115 – 9 .
Hashemi F . Response ethics to nursing errors . J Med Ethics Hist Med 2007 ; 4 : 31 – 46 .
Johnstone MJ , Kanitsaki O . The ethics and practical importance of defining, distinguishing and disclosing nursing errors: a discussion paper . Int J Nurs Stud 2006 ; 43 : 367 – 76 .
Fathi A , Hajizadeh M , Moradi K et al. . Medication errors among nurses in teaching hospitals in the west of Iran: what we need to know about prevalence, types, and barriers to reporting . Epidemiol Health 2017 ; 39 : e2017022 .
Armitage G , Knapman H . Adverse events in drug administration: a literature review . J Nurs Manag 2003 ; 11 : 130 – 40 .
Ismail M , Hamid H , Hamid S et al. . Check the amount and type of medication errors in nursing students at four teaching hospitals of Tehran . Iran J Med Ethics Hist 2009 ; 3 : 60 – 9 .
Blegen MA , Vaughn TE , Goode CJ . Nurse experience and education: effect on quality of care . J Nurs Adm 2001 ; 31 : 33 – 9 .
Maxwell S , Walley T , Ferner RE. Using drugs safely: Undergraduates Must be Proficient in Basic Prescribing . BMJ 2002 ; 324 : 930 – 1 .
Härkänen M , Vehviläinen-Julkunen K , Murrells T et al. . Medication administration errors and mortality: incidents reported in England and Wales between 2007–2016 . Res Social Adm Pharm 2019 ; 15 : 858 – 63 .
Tabatabaee SS , Kohpeima Jahromi V , Asadi M et al. . Ranking factors contributing to medication error incidents in private hospital: a nurse’s perspective . Int J Hosp Res 2013 ; 2 : 187 – 94 .
Burke KG . Executive summary: the State of the Science on Safe Medication Administration symposium . Am J Nurs 2005 ; 105 : 4 – 9; discussion 42–7 .
Abusaad EFES , Etawy EA . Medication administration errors at Children’s University hospitals: nurses point of view . J Nur Health Sci 2015 ; 4 : 51 – 60 .
Sutker WL . The physician’s role in patient safety: what’s in it for me? Proc (Bayl Univ Med Cent) 2008 ; 21 : 9 – 14 .
Donaldson L . An Organisation With a Memory: Report of an Expert Group on Learning from Adverse Events in the NHS chaired by the Chief Medical Officer . London, UK: The Stationery Office , 2000 .
Leape LL , Berwick DM , Bates DW . What practices will most improve safety? Evidence-based medicine meets patient safety . JAMA 2002 ; 288 : 501 – 7 .
Dirik HF , Samur M , Seren Intepeler S et al. . Nurses’ identification and reporting of medication errors . J Clin Nurs 2019 ; 28 : 931 – 8 .
Spurlock B , Nelson M , Paterno J et al. . Legislating Medication Safety: The California Experience . Oakland, CA : California HealthCare Foundation , 2003 .
Kagan I , Barnoy S . Factors associated with reporting of medication errors by Israeli nurses . J Nurs Care Qual 2008 ; 23 : 353 – 61 .
Chiang HY , Pepper GA . Barriers to nurses’ reporting of medication administration errors in Taiwan . J Nurs Scholarsh 2006 ; 38 : 392 – 9 .
Güneş ÜY , Gürlek Ö , Sönmez M . Factors contributing to medication errors in Turkey: nurses’ perspectives . J Nurs Manag 2014 ; 22 : 295 – 303 .
Gaal S , Verstappen W , Wensing M . Patient safety in primary care: a survey of general practitioners in The Netherlands . BMC Health Serv Res 2010 ; 10 : 21 .
Madegowda B , Hill PD , Anderson MA . Medication errors in a rural hospital . Medsurg Nurs 2007 ; 16 : 175 – 80 .
Petrova E . Nurses’ perceptions of medication errors in Malta . Nurs Stand 2010 ; 24 : 41 – 8 .
Shiima Y , Wong ZS . Classification scheme for incident reports of medication errors . Stud Health Technol Inform 2019 ; 265 : 113 – 8 .
Kahriman İ , Öztürk H . Evaluating medical errors made by nurses during their diagnosis, treatment and care practices . J Clin Nurs 2016 ; 25 : 2884 – 94 .
Lengacher CA , Mabe PR , Bowling CD et al. . Redesigning nursing practice. The partners in patient care model . J Nurs Adm 1993 ; 23 : 31 – 7 .
Barnsteiner JH . Medication reconciliation: transfer of medication information across settings-keeping it free from error . Am J Nurs 2005 ; 105 : 31 – 6; quiz 48–51 .
Hewitt T , Chreim S , Forster A . Double checking: a second look . J Eval Clin Pract 2016 ; 22 : 267 – 74 .
Edwards M , Moczygemba J . Reducing medical errors through better documentation . Health Care Manag 2004 ; 23 : 329 – 33 .
Jenkins RH , Vaida AJ . Simple strategies to avoid medication errors . Fam Pract Manag 2007 ; 14 : 41 – 7 .
Sarfati L , Ranchon F , Vantard N et al. . Human-simulation-based learning to prevent medication error: a systematic review . J Eval Clin Pract 2019 ; 25 : 11 – 20 .
Greengold NL , Shane R , Schneider P et al. . The impact of dedicated medication nurses on the medication administration error rate: a randomized controlled trial . Arch Intern Med 2003 ; 163 : 2359 – 67 .
Carver N , Gupta V , Hipskind JE. Medical Error. In: StatPearls [Internet]. Treasure Island, FL: StatPearls Publishing , 2020 .
| Month: | Total Views: |
|---|---|
| January 2021 | 115 |
| February 2021 | 202 |
| March 2021 | 574 |
| April 2021 | 281 |
| May 2021 | 76 |
| June 2021 | 27 |
| July 2021 | 12 |
| August 2021 | 13 |
| September 2021 | 37 |
| October 2021 | 55 |
| November 2021 | 16 |
| December 2021 | 24 |
| January 2022 | 17 |
| February 2022 | 97 |
| March 2022 | 1,133 |
| April 2022 | 1,078 |
| May 2022 | 1,269 |
| June 2022 | 1,040 |
| July 2022 | 1,150 |
| August 2022 | 1,389 |
| September 2022 | 1,939 |
| October 2022 | 2,183 |
| November 2022 | 1,630 |
| December 2022 | 1,036 |
| January 2023 | 1,742 |
| February 2023 | 2,435 |
| March 2023 | 3,169 |
| April 2023 | 3,268 |
| May 2023 | 3,049 |
| June 2023 | 2,180 |
| July 2023 | 2,375 |
| August 2023 | 2,207 |
| September 2023 | 2,638 |
| October 2023 | 2,837 |
| November 2023 | 2,324 |
| December 2023 | 1,546 |
| January 2024 | 2,212 |
| February 2024 | 2,656 |
| March 2024 | 3,257 |
| April 2024 | 3,341 |
| May 2024 | 2,466 |
| June 2024 | 2,035 |
| July 2024 | 2,178 |
| August 2024 | 1,626 |
Email alerts
Citing articles via.
- Recommend to Your Librarian
- Advertising and Corporate Service
- Journals Career Network
Affiliations
- Online ISSN 1759-8893
- Copyright © 2024 Royal Pharmaceutical Society
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
To read this content please select one of the options below:
Please note you do not have access to teaching notes, leadership for reducing medical errors via organizational culture: a literature review.
Measuring Business Excellence
ISSN : 1368-3047
Article publication date: 13 May 2022
Issue publication date: 14 July 2022
Medical errors have become the third leading cause of death in the USA. Two million deaths from preventable medical errors will occur annually worldwide each year. The purpose of this paper is to find themes from the literature relating leadership styles – leadership approaches in practice – with success in reducing medical errors and patient safety.
Design/methodology/approach
This review analyzed primary and secondary sources based on a search for the terms leadership OR leadership style AND medical errors OR patient safety using five high-quality health-care-specific databases: Healthcare Administration Database from Proquest, LLC, Emerald Insight from Emerald Publishing Limited, ScienceDirect from Elsevier, Ovid from Ovid Technologies and MEDLINE with Full-Text from Elton B. Stevens Company. After narrowing, the review considered 21 sources that met the criteria.
The review found three leadership approaches and four leadership actions connected to successfully reducing medical errors and improving patient safety. Transformational, authentic and shared leadership produced successful outcomes. The review also found four leadership actions – regular checks on the front line and promoting teamwork, psychological safety and open communication – associated with successful outcomes. The review concluded that leadership appeared to be the preeminent factor in reducing medical errors and improving patient safety. It also found that positive leadership approaches, regardless of the safety intervention, led to improving results and outcomes.
Research limitations/implications
This review was limited in three ways. First, the review only included sources from the USA, the UK, Canada and Australia. While those countries have similar public-private health-care systems and similar socioeconomics, the problem of medical errors is global (Rodziewicz and Hipskind, 2019). Other leadership approaches or actions may have correlated to reducing medical errors by broadening the geographic selection parameters. Future research could remove geographic restrictions for selection. Second, the author has a bias toward leadership as distinctive from management. There may be additional insights gleaned from expanding the search terms to include management concepts. Third, the author is a management consultant to organizations seeking to improve health-care safety. The author’s bias against limited action as opposed to strategic leadership interventions is profound and significant. This bias may generalize the problem more than necessary.
Practical implications
There are three direct practical implications from this review. The limitations of this review bound these implications. First, organizations might assess strategic and operational leaders to determine their competencies for positive leadership. Second, organizations just beginning to frame or reframe a safety strategy can perhaps combine safety and leadership interventions for better outcomes. Third, organizations could screen applicants to assess team membership and team leadership orientation and competencies.
Originality/value
This review is valuable to practitioners who are interested in conceptual relationships between leadership approaches, safety culture and reducing medical errors. The originality of this research is limited to that of any literature review. It summarizes the main themes in the selected literature. The review provides a basis for future considerations centered on dual organizational interventions for leadership and safety.
- Strategic leadership
- Patient safety
- Positive leadership
- Medical errors
- Leadership approaches
- Safety culture
Adams, D.E. (2022), "Leadership for reducing medical errors via organizational culture: a literature review", Measuring Business Excellence , Vol. 26 No. 2, pp. 143-162. https://doi.org/10.1108/MBE-06-2021-0079
Emerald Publishing Limited
Copyright © 2022, Emerald Publishing Limited
Related articles
All feedback is valuable.
Please share your general feedback
Report an issue or find answers to frequently asked questions
Contact Customer Support
- Article Information
See More About
Select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Others Also Liked
- Download PDF
- X Facebook More LinkedIn
Mazor KM , Simon SR , Gurwitz JH. Communicating With Patients About Medical Errors : A Review of the Literature . Arch Intern Med. 2004;164(15):1690–1697. doi:10.1001/archinte.164.15.1690
Manage citations:
© 2024
- Permissions
Communicating With Patients About Medical Errors : A Review of the Literature
From the Meyers Primary Care Institute, University of Massachusetts Medical School, and Fallon Foundation, Worcester (Drs Mazor and Gurwitz); and Department of Ambulatory Care and Prevention, Harvard Medical School, and Harvard Pilgrim Health Care, Boston, Mass (Dr Simon). The authors have no relevant financial interest in this article.
Background Ethical and professional guidelines recommend disclosure of medical errors to patients. The objective of this study was to review the empirical literature on disclosure of medical errors with respect to (1) the decision to disclose, (2) the process of informing the patient and family, and (3) the consequences of disclosure or nondisclosure.
Methods We searched 4 electronic databases (MEDLINE, CINAHL, PsycINFO, and Social Sciences Citations Index) and the reference lists of relevant articles for English-language studies on disclosure of medical errors. From more than 800 titles reviewed, we identified 17 articles reporting original empirical data on disclosure of medical errors to patients and families. We examined methods and results of the articles and extracted study designs, data collection procedures, populations sampled, response rates, and definitions of error.
Results Available research findings suggest that patients and the public support disclosure. Physicians also indicate support for disclosure, but often do not disclose. We found insufficient empirical evidence to support conclusions about the disclosure process or its consequences.
Conclusions Empirical research on disclosure of medical errors to patients and families has been limited, and studies have focused primarily on the decision stage of disclosure. Fewer have considered the disclosure process, the consequences of disclosure, or the relationship between the two. Additional research is needed to understand how disclosure decisions are made, to provide guidance to physicians on the process, and to help all involved anticipate the consequences of disclosure.
When medical errors occur, effective physician-patient communication is critical. Ethical and professional guidelines make clear that physicians have a responsibility to disclose medical errors, 1 - 3 and recent standards link disclosure of unexpected outcomes to hospital accreditation. 4 The National Patient Safety Foundation's statement of principle on disclosure of health care injuries urges health care professionals and institutions to be forthcoming about health care injuries and errors and to provide truthful and compassionate explanations to patients and families when errors occur. 5 The literature is replete with discussions, commentaries, letters, and editorials on disclosure of medical errors to patients, many of which argue for disclosure on ethical and pragmatic grounds.
The objective of this study was to review the empirical literature on disclosure of medical errors to patients. We also examined the evidence regarding the decision to disclose, the process of disclosing the error to the patient and family, and the consequences of disclosure or nondisclosure.
We conducted searches of 4 electronic databases (MEDLINE, CINAHL, PsycINFO, and Social Sciences Citations Index) through March 31, 2003, for English-language articles with empirical data related to disclosure of medical errors. For the MEDLINE search, we used the subject headings truth disclosure or disclosure in combination with medical errors , medication errors , diagnostic errors , or iatrogenic disease ; we also combined the disclosure terms with risk management and with malpractice in combination with physician-patient relations or hospital-patient relations. We modified terms as needed for the remaining 3 databases, selecting parallel terms where possible. As primary articles were identified, we reviewed the reference lists for additional articles. We also reviewed the reference lists of published reviews and commentaries on disclosure of medical errors. 6 - 19
Articles reporting original empirical results of systematic research relating to disclosure of medical errors to patients and families were selected. We used 3 selection criteria. First, we required content on disclosure of medical error to patients or families, using the Institute of Medicine's definition of medical error. 20 If it was not clear whether the event or item considered in the study met this definition (eg, if it was not explicitly stated that the event was preventable), we included the study if the researchers or participants referred to the event as an error, mistake, accident, or negligence. We excluded studies of disclosure if the focus was nonpreventable adverse events, as well as studies of disclosure of other sorts of information, such as human immunodeficiency virus status or genetic testing results. This criterion (disclosure to patients and families) also excluded studies of internal reporting, public reporting, or reporting to professional or regulatory organizations. Our second criterion was that the study report original empirical data; this excluded personal accounts, reviews, letters, editorials, opinion pieces, and commentaries. Finally, we excluded articles in veterinary, dentistry, trade, or medical technicians' journals; unpublished manuscripts; legal decisions; and popular press articles.
Included studies were abstracted for study design, data collection procedures, study population, and response rate, where applicable. Evaluations of interventions were classified using the rubric described by Campbell and Stanley. 21 We also abstracted whether medical error was defined and, if so, how.
Our initial review of the studies led us to conceptualize disclosure as consisting of 3 stages: (1) the decision to disclose that an error occurred, (2) the process of disclosing the error to the patient and family (given the decision to disclose), and (3) the consequences of disclosure or nondisclosure. We therefore categorized each study as providing evidence on 1 or more of these stages.
Of the 825 articles identified through searches of the electronic databases, 9 met our inclusion criteria. 22 - 30 Eight additional articles were identified through hand searching. 31 - 38 Key characteristics of the 17 articles reviewed are summarized in Table 1 . All studies were primarily descriptive. With one exception, 25 the studies used cross-sectional designs. One study 32 also incorporated an experimental component: 2 versions of a vignette were developed and randomly assigned to respondents. Only one study 25 considered the effect of an intervention (a change in organizational policy on disclosure). This study involved a static group comparison and was classified as preexperimental.
Definitions of medical error varied across studies. Seven of the studies incorporated 1 or more vignettes describing a medical error and associated outcome. 23 , 26 , 29 , 32 , 34 , 35 , 37 In these studies, the medical error was defined by the vignette. Alternatively (or, in some cases, additionally), researchers provided explicit definitions of medical error or adverse event 22 , 23 , 30 , 32 , 35 or used terms such as mistake or error in the questionnaire item or stem. 24 , 28 One study 36 defined medical error in the article, but did not provide the definition of medical error used with participants. Studies 27 , 31 , 33 , 34 , 38 of patients and relatives seeking advice or legal action presume that the respondent believes that a negligent event occurred, and negligent events are considered a subset of preventable adverse events. 20 Finally, for the intervention study, 25 the policy under study explicitly referred to medical error.
Several of the studies have significant methodological weaknesses related to response rates and sampling. Of the 13 studies reporting response rates, 6 reported rates less than 50%. 22 , 28 - 30 , 33 , 38 In addition, most studies drew samples from highly constrained populations; only 3 studies randomly sampled from state 37 or national 32 , 35 lists. The findings from the reviewed studies are summarized herein, organized by stage of disclosure.
Studies using retrospective self-report by physicians and trainees suggest that disclosure often does not occur. During interviews about how mistakes were handled, trainees mentioned the patient or family in only 6% of the cases. 36 When queried about their most significant medical mistake in the last year, 24% of trainees had discussed the error with the patient or family, 30 and a similar rate (21%) was found in a later study 22 of physicians. A survey of hospital risk managers in the United States found that disclosure of adverse events (preventable and nonpreventable) occurred a mean of 7.4 times per 10 000 admissions; 65% of managers indicated that hospital practice was always to disclose death or serious injury, and 37% indicated that their practice was always to disclose serious short-term harm. 35
Reports of patients and relatives also suggest low rates of disclosure. A recent national survey found that, of those who believed that they had experienced an error in their care or in the care of a family member, approximately 30% had been told by the health professional involved that an error had been made. 32
When asked to predict whether they would disclose under different circumstances, physicians' responses are variable. Physician focus group participants described specific situations in which they would not disclose; some indicated that there was no need to disclose if the harm was trivial or if the patient was unaware of the error. 23 A study 28 that queried European physicians on whether they would disclose an "iatrogenic incident (avoidable mistake)" found that 32% would disclose what happened, while 63% would minimize the incident. In response to vignettes describing medical errors, 95% of physicians and physician trainees predicted that they would disclose a medication error that resulted in injury, while 84% would disclose the same error if it resulted in death. 26 In a separate study 37 using a different medication error vignette also resulting in death, approximately 50% of physicians indicated that they would admit the error. Hospital risk managers reported that disclosure would be more likely to occur for a medical error leading to a serious adverse event than for an error resulting in a minor adverse event (90% vs 80%). 35 In addition, 53% of risk managers reported a lower likelihood of disclosing preventable harm than nonpreventable harm.
Physicians agree that patients should be informed about medical errors. With respect to the iatrogenic incident (avoidable mistake) noted in the previous paragraph, 70% of responding European physicians believed that they should provide details of such an event. 28 In a survey of US physicians, 77% responded that physicians should be required to tell patients when errors are made in their care. 32 The same survey presented respondents with 1 of 2 vignettes. One vignette described a prescribing error resulting in death. In this instance, 90% of physicians believed that the prescribing physician should disclose the error; fewer thought that the nurse involved (70%) or the hospital (71%) should disclose. In response to the same error resulting in a rash but with full recovery, 85% believed that the physician should disclose, while 75% thought that the nurse should disclose and 60% believed that the hospital should disclose.
Studies of patient and family preferences for disclosure have found strong support for disclosure. In focus group discussions, patients were unanimous in their desire to be told about any error that caused harm, although not all would want to know about errors that did not cause harm. 23 A national survey found that 89% of the public believed that physicians should be required to tell patients when errors are made in their care. 32 A smaller study 24 of emergency department patients found that 76% would want to be informed immediately if "something did go wrong in the administration of [their] health care" and 88% favored full disclosure of the error's extent.
Similar results have been reported with respect to patients' responses to vignettes. When presented with a vignette describing an adverse event (complications during eye surgery), 92% of patient respondents favored disclosure, and 81% favored receiving detailed information on adverse consequences. 34 Another vignette-based study 29 found that 98% of patients wanted some acknowledgment that an error had been made, even when no harm to the patient occurred. Similar rates were found in another vignette-based study, 32 in which respondents were presented with 1 of 2 different medication error vignettes. For the error resulting in death, 95% of the public believed that the prescribing physician should disclose the error; 84% thought that the hospital should disclose, and 57% believed that the nurse should disclose. For the same error resulting in a minor event (rash) with full recovery, 95% favored disclosure by the physician, while fewer believed that the hospital (78%) or the nurse (67%) should disclose.
In response to a national survey, hospital risk managers reported that the most common elements of the disclosure process were explanations (92%), an undertaking to investigate the incident (87%), an apology (68%), and an acknowledgment of harm (66%). 35 Less frequently reported were offering to share the results of the investigation (41%) and assuming responsibility for harm (33%). Eighty-two percent of risk managers reported that hospitals offered to pay the costs of associated care.
In a national survey of physicians and the public, approximately one third (34% of physicians and 33% of the public) of all respondents who had experienced an error in their care or in the care of a family member reported receiving an apology from the health care professional involved. 32 Of patients who believed that they had been injured as a result of their medical treatment, 21% reported that staff accepted responsibility for what had happened, and 27% reported that they had been offered an apology. 27 Somewhat lower rates were reported in a subsequent study 38 of patients and relatives pursuing medical negligence claims, in which 13% reported that the responsibility for the incident was fully or partly accepted and 15% reported a full or partial apology. A review of depositions of malpractice plaintiffs found that failure to provide an explanation was cited as a reason for pursuing legal action in 10% of the depositions. 31
Explanations did not necessarily result in patient satisfaction. Among patients who believed that they had been injured and were seeking advice, 82% were dissatisfied with the amount of information they received, 67% were dissatisfied with the clarity, and 63% were dissatisfied with the accuracy. 27 In addition, 63% believed that the explanation had been given unsympathetically, and 44% indicated that they had had no opportunity to ask questions. Similar rates were found among patients and family members pursuing medical negligence claims: 61% of those who had received an explanation of the incident reported that the explanation had been given unsympathetically, 11% were satisfied with the amount of information provided, 20% were satisfied with the accuracy, and 24% were satisfied with the clarity of the information. 38 Timing also appears to be of concern to patients. Of patients who believed that they had been injured as a result of medical treatment, 20% reported that they had waited longer than 6 months for an explanation. 27 Of those pursuing medical negligence claims, only 21% reported that they had received explanations within a few days of the incident, and 37% never received an explanation. 38
There are few data from physicians on the disclosure process. Physician focus group participants reported that they would be likely to choose their words carefully and to avoid explicitly stating that an error had taken place. 23 Most indicated that they would want to apologize, but would worry that an expression of regret might be construed as admission of legal liability. In contrast, patients in focus groups expressed a desire to be told what had happened and why, the implications of the error for their health, how the problem would be corrected, and how future errors would be prevented. Furthermore, they would want the physician to be forthcoming about the error, rather than have to ask a lot of questions to get the information. Patients also wanted assurances that they would not incur financial liabilities because of error. Vignette-based surveys have also assessed patient preferences. When presented with vignettes of error resulting in no harm or moderate harm, more than 70% of patients indicated that they would want to discuss the error with the physician involved; for the serious error vignette, 80% would want to discuss it with another physician. 29 Fourteen percent indicated that they would want a referral to another physician if the error did not result in injury; this percentage increased as the injury became more serious, to approximately 40% for a moderate error and approximately 65% for a severe error. Fewer than 10% reported that they would want financial compensation following an error without harm; this increased to approximately 20% following a moderate error and to nearly 60% following a severe error.
None of the studies examined herein provided evidence of a causal relationship between the occurrence (or nonoccurrence) of disclosure and litigation, or between specific elements of the disclosure process and litigation. Given that caveat, studies of those taking or considering legal action provide some insight. Of family members involved in malpractice claims alleging perinatal injury, 20% indicated that they were seeking information, and 24% indicated that they sought legal action when they perceived that there had been a cover-up or that the physician had failed to be completely honest, had allowed them to believe things that were not true, or had intentionally misled them; 32% had believed that the physician involved would not talk to them or answer their questions. 33 A study 31 of malpractice plaintiffs' depositions identified physician-patient relationship issues in 71% of the depositions. Although it is not clear whether issues with the physicians existed before the adverse outcomes, 32% of depositions referred to physician desertion or failure to be available, 26% referred to dysfunctional delivery of information, and 13% referred to failure to solicit or hear patients' requests for information, opinions, or expressions of discomfort. Of those pursuing medical negligence claims, 91% of respondents reported that desire for an explanation was a reason for their pursuing legal action. 38 When asked whether anything could have been done once the incident occurred that would have prevented the need for legal action, 41% responded affirmatively; many suggested explanation and apology (39%). Of patients who believed that they had been injured through medical treatment, lower frequencies of explanations were associated with greater distress and greater difficulty with adjustment. 27 These relationships were not attributable to an overall negative attitude toward physicians or pain levels. In addition, although all of the patients in the study had considered litigation, those who had decided to go forward with litigation were more dissatisfied with the explanations that they had received than those who had chosen not to proceed.
Patients' predictions about their behavior in response to vignettes suggest that disclosure by the physician may result in more positive consequences than learning of the error from another source; patients indicated that they would be more likely to continue to see the physician, less likely to report the physician, and less likely to file a lawsuit if the physician informed them of the error. 29 In focus group discussions, patients predicted that disclosure would be reassuring and would enhance their trust in the physician's honesty. 23
In the study 25 that examined the effects of an intervention (implementation of a policy of "extreme honesty"), the claims experience of the facility implementing the new policy, a Veterans Affairs (VA) medical center in Lexington, Ky, was compared with 35 other VA facilities without such a policy. The findings suggest that, although the number of claims against the Lexington facility was high (only 5 facilities had more claims), the total amount of payments was low (only 7 facilities reported lower payments).
Ethical and professional guidelines, 1 - 3 credentialing organizations, 4 patient safety organizations, 5 and experts on medical errors advocate disclosure of medical errors to patients and families, 6 - 19 but there is little empirical evidence to guide practitioners. We found empirical support for concluding that disclosure often does not occur, 22 , 28 , 30 , 32 , 36 that patients and the public favor disclosure, 23 , 24 , 29 , 32 , 34 and that physicians support disclosure, 23 , 28 , 32 but we found no empirical results to guide practitioners with respect to the practical questions of who, what, when, and how to disclose. Because best process is defined by best outcomes, answers to these questions await an understanding of the relationship between the process and consequences of disclosure. Insufficient empirical data exist to evaluate whether full disclosure results in benefits for patients, providers, and organizations or whether expectations of negative consequences are unfounded. Medical malpractice litigation provides an example of a potential negative consequence. Fear of litigation has been cited as a significant obstacle to disclosure. 31 In focus group discussions, physicians noted that fear of litigation might limit their statements to patients and inhibit the offer of an apology. 23 Fear of malpractice litigation was reported by risk managers to be a barrier to disclosure more frequently than any other barrier studied. 35 The findings of Witman and colleagues 29 have often been cited to support the assertion that disclosure may reduce litigation risk. However, this assumes a link between patients' responses to hypothetical scenarios and their responses to actual errors, and such a link has not yet been established. The results of the implementation of the extreme honesty policy at the Lexington VA facility 25 are encouraging, but the unique characteristics of the VA system, the patients served, and the legal status of providers within that system make it questionable whether similar results would be obtained in other settings. Studies 27 , 31 , 33 , 38 of patients and families considering or involved in litigation suggest the importance of explanation and apology, but findings from such studies are suggestive rather than conclusive, and correlation and causation are not yet established. Other research findings suggest that the characteristics of the injury, the physician-patient relationship before the adverse event, the physicians' communication skills, and the patients' financial status are influential in litigation decisions. 39 - 43 Evaluation of the relative importance of each of these factors and the specific components of disclosure should be a goal for future research. Fear of malpractice litigation is not the only barrier to disclosure; physicians may also anticipate patient distress, patient attrition, damage to their reputation, license revocation, loss of privileges, and other consequences. 6 - 8 , 11 , 16 , 19 , 22 , 44 Future research should seek to determine the extent to which such concerns are in fact barriers and then evaluate methods for minimizing the likelihood of anticipated negative consequences.
Accompanying the need for research on the relationship between decision, process, and consequences is the necessity to investigate the circumstantial variables that affect all 3 stages of disclosure. Vincent et al 45 have proposed a framework for understanding and responding to adverse events, suggesting the headings of institutional , organization and management , work environment , team , individual staff member , task , and patient. Other researchers have stressed the importance of the national, regional, and professional culture. 46 We believe that variables in all of these categories are important to disclosure and that further work is needed to develop a coherent framework for investigating the influence of these types of variables on disclosure. Such a framework will facilitate systematic examination of the interrelationships between variables and will help in the development of guidelines for practitioners.
The Institute of Medicine's report defines an adverse event as "an injury caused by medical management rather than the underlying condition of the patients." 20 (p28) Adverse events attributable to error are considered preventable (although by definition not all medical errors result in adverse events), and negligent adverse events are a subset of preventable adverse events. 20 In practice, there is likely to be considerable uncertainty as to causality and preventability. Trained physicians reviewing medical records have displayed poor to moderate agreement on whether an adverse event occurred and whether that occurrence was preventable. 47 , 48 Although a treating physician may have greater knowledge of the patient's condition than a reviewer working from the medical record, determination of causality and preventability may be as difficult or more so. In practice, such uncertainty complicates the disclosure decision. Premature disclosure may cause unnecessary distress, but waiting for an investigation to be completed may increase patient anger and frustration, especially when causality is obscure to the patient and family.
Difficulties in defining and identifying medical errors in practice are paralleled by the different definitions of medical errors used in the studies reviewed herein. Each definition or lack of definition of medical error in a questionnaire or interview study must be considered in interpreting results. If the term medical error is not defined, inferences about group differences may not be valid. For instance, some patients include rudeness or poor service quality as medical errors, 23 events that most physicians would not include. The use of clear, explicit definitions should increase the likelihood that all respondents are referring to the same class of events. Case vignettes ensure that all respondents are referring to the same event and eliminate the need for the respondent to decide whether an error has occurred. However, the case details will influence responses, so that conclusions based on a specific vignette are not necessarily generalizable, and inferences about attitudes or behaviors regarding disclosure in general may not be justified. Future research should attempt to identify which components of case vignettes influence responses, not only to facilitate cross-study comparisons but also to better understand and predict responses to disclosure of actual errors.
One important limitation to the research considered herein is that most of the studies reported participants' recollections of behaviors or events or predictions about future behaviors. The conclusions of such studies are predicated on the assumption that reports or predictions are related to participants' behavior in circumstances of actual errors, but we found no tests of this assumption. Researchers should examine the extent to which errors in recall or prediction occur, as well as whether the study setting introduces a bias. Patients and physicians are likely to have strong emotions and beliefs about disclosure of medical errors and are likely to be sensitive to the explicit or implicit social context of data collection. Respondents are likely to filter their responses to meet social norms, especially in the context of focus groups or nonanonymous interviews or questionnaires. For physicians, knowledge of ethical standards may result in reporting more "correct" behavior; for patients, especially those involved in legal action, expectations and beliefs about the legal process may influence reporting. Future research should examine the accuracy of self-reports and predictions in this area.
Many of the studies reviewed herein drew from small, circumscribed populations, and many reported poor response rates; both issues need to be addressed in future research. When the study population is limited (eg, drawn from a single medical center, geographic region, medical specialty, or organization), results may not be generalizable to other populations. Similarly, self-selection and nonresponse biases limit generalizability; these effects are likely to be most problematic when response rates are low.
Although traditional randomized controlled trials are not feasible or ethically appropriate for studying disclosure of medical error, this review found an overreliance on cross-sectional designs and direct self-report measures. We suggest 2 avenues for future research. First, the use of vignette-based studies in experimental designs provides a means of efficiently and systematically examining multiple variables and allows manipulation of these variables in ways that would be unethical in the clinical setting. This approach will be especially useful for identifying a smaller set of variables for further study. Greater realism can be introduced through videotaped simulations (rather than written vignettes), although the link between behavior in the hypothetical situation and real life must be addressed, as noted herein. The second avenue that researchers should be alert to is the potential for capitalizing on naturally occurring changes in health care organizations. As organizations institute new policies on disclosure of error, opportunities for conducting "natural experiments" may occur. The report on the experience of the Lexington VA facility describes one such effort, 25 but there is a need for additional rigorous evaluations in different settings. Studies conducted at the organizational level, with organizations rather than individual patients assigned to intervention conditions, may also avoid some of the ethical and practical difficulties inherent in research in this area.
The prevalence of discussion papers, commentaries, and editorials on disclosure of errors to patients is evidence of the importance of the topic of disclosure for clinicians; the dearth of empirical research is a barrier to improvements in practice. Without empirical data to provide guidance on how to disclose well and without a better understanding of the relationship between the disclosure process and the consequences of disclosure, clinicians can only guess at what is most effective in this difficult situation. This lack of knowledge may lead to suboptimal outcomes for the patient and the physician and thereby discourage disclosure in future cases. With respect to the decision stage of disclosure, future research should examine what influences this decision, focusing on barriers and how these might be reduced. With respect to process, researchers should seek to develop answers to the many practical questions faced by practitioners, such as who should disclose, what information should be provided, and when disclosure should occur. Answers to these questions will require a greater knowledge of the consequences of disclosure and how specific process components affect the consequences. Finally, future research must consider the many levels of variables that may influence all stages of disclosure, from the cultural context at the national level to the characteristics of the individual patient and physician.
Correspondence: Kathleen M. Mazor, EdD, Meyers Primary Care Institute, University of Massachusetts Medical School, and Fallon Foundation, 630 Plantation St, Worcester, MA 01605 ( [email protected] ).
Accepted for publication November 28, 2003.
This study was supported by grants from the Agency for Healthcare Research and Quality, Rockville, Md, to the HMO Research Network Center for Education and Research on Therapeutics (CERTs) (U18HS10391-01) and to the HMO Research Network CERTs Prescribing Safety Program (U18HS11843-01) and by a grant from the National Patient Safety Foundation and The Commonwealth Fund (20030288). Dr Simon is the recipient of a Morgan-Zinsser Fellowship from the Academy at Harvard Medical School.
We thank Dawn Peterson, BS, and Ryan Tappin, BS, for providing technical assistance.
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- BMJ Journals
You are here
- Online First
- Diagnostic error in mental health: a review
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0002-8390-8844 Andrea Bradford 1 , 2 ,
- http://orcid.org/0000-0001-7993-8584 Ashley N D Meyer 1 , 2 ,
- Sundas Khan 2 ,
- http://orcid.org/0000-0002-9184-6524 Traber D Giardina 1 , 2 ,
- http://orcid.org/0000-0002-4419-8974 Hardeep Singh 1 , 2
- 1 Department of Medicine , Baylor College of Medicine , Houston , TX , USA
- 2 Center for Innovations in Quality, Effectiveness and Safety , Michael E. DeBakey VA Medical Center and Baylor College of Medicine , Houston , Texas , USA
- Correspondence to Dr Andrea Bradford, Baylor College of Medicine, Houston, Texas, USA; Andrea.Bradford{at}bcm.edu
Diagnostic errors are associated with patient harm and suboptimal outcomes. Despite national scientific efforts to advance definition, measurement and interventions for diagnostic error, diagnosis in mental health is not well represented in this ongoing work. We aimed to summarise the current state of research on diagnostic errors in mental health and identify opportunities to align future research with the emerging science of diagnostic safety. We review conceptual considerations for defining and measuring diagnostic error, the application of these concepts to mental health settings, and the methods and subject matter focus of recent studies of diagnostic error in mental health. We found that diagnostic error is well understood to be a problem in mental healthcare. Although few studies used clear definitions or frameworks for understanding diagnostic error in mental health, several studies of missed, wrong, delayed and disparate diagnosis of common mental disorders have identified various avenues for future research and development. Nevertheless, a lack of clear consensus on how to conceptualise, define and measure errors in diagnosis will pose a barrier to advancement. Further research should focus on identifying preventable missed opportunities in the diagnosis of mental disorders, which may uncover generalisable opportunities for improvement.
- Diagnostic errors
- Mental health
- Medical error, measurement/epidemiology
This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
https://doi.org/10.1136/bmjqs-2023-016996
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Introduction
Timely and appropriate diagnosis in mental health is an essential first step towards effective treatment. Missed, delayed or wrong diagnosis of mental disorders can lead to poorer patient outcomes and can waste time and resources. For example, delayed diagnosis of bipolar disorder has been linked to more frequent relapse and hospitalisations. 1 2 In a large registry study of over 1000 patients with narcolepsy, over one-quarter of the sample reported having consulted five or more clinicians before receiving the diagnosis. 3 Missed and delayed diagnosis can also result in a lack of functional improvement, delayed remission, and delayed or unnecessary treatments. 4
Mental disorders are largely clinical diagnoses that seldom have specific objective findings that can be detected through laboratory testing, physical examination or imaging. As such, history taking, behavioural observation and data gathering from collateral sources (eg, family members, teachers) are essential to the diagnosis. Despite the importance of effective data gathering and synthesis, time pressures, competing priorities and various cognitive biases can interfere with this process. 4–6 Validated psychological tests and symptom reporting scales can help with the data gathering process, but these can lead to inaccurate diagnostic impressions if they are interpreted without sufficient context or not followed with an appropriate diagnostic interview. 7 8 Finally, evolving (and in some cases, expanding) diagnostic criteria for mental disorders have prompted concerns that clinicians could inadvertently pathologise normal experiences. 9 10
Despite these and other concerns about the quality of psychiatric diagnosis, most discussion of diagnostic error in mental health has been disconnected from the broader national conversation on diagnostic error and diagnostic excellence. As a stark example, while the National Academies of Science, Engineering, and Medicine’s (NASEM) landmark report Improving Diagnosis in Health Care 4 describes mental health diagnosis as ‘particularly challenging’ (p. 52), there is otherwise little explicit mention of mental health in this 472-page report. In turn, the NASEM report is only sparsely cited in the mental health literature. 11 12 The NASEM report and contemporary research on diagnostic errors has stimulated major private (eg, Moore Foundation) and public (eg, Agency for Healthcare Research and Quality) funding initiatives to study and improve diagnostic safety. Again, however, mental health has been scarcely represented in the various projects funded under these initiatives. This is a significant gap given the high prevalence of mental disorders in the USA and worldwide.
As definitions and methods for studying diagnostic safety advance, it is important that these concepts can be applied to mental health. In this narrative review, we aim to summarise the current state of research on diagnostic error in mental health and identify opportunities to align future research with the emerging science of diagnostic safety. Specifically, we review (1) how diagnostic error in mental health has been conceptualised and measured; (2) evidence for diagnosis-specific pitfalls in common mental disorders; and (3) evidence to inform interventions to reduce diagnostic errors. Although diagnostic overshadowing (the attribution of symptoms to an existing diagnosis rather than a potential comorbid condition 13 ) in people with mental disorders is an important problem, 13–16 this is reviewed elsewhere 17 18 and is outside the scope of this review. We also do not cover the topic of overdiagnosis (when a condition is diagnosed that would not otherwise be consequential to the patient’s health or well-being 4 19 ), as the term is used inconsistently in this literature and is usually conflated with related concepts such as false positives, overtreatment and misdiagnosis. 20
Conceptualising and measuring diagnostic errors
Explicit definitions of diagnostic error seldom appear in the mental health literature, making it difficult to compare findings across studies. A definition in a major psychiatry textbook, acknowledging the work of Cullen et al , 21 focuses on diagnostic accuracy: ‘Diagnostic errors are not only inappropriate psychiatric diagnosis, but also mistaking a physical illness for a psychiatric condition or vice versa.’ 22 Similarly, studies of diagnostic error in mental health have implicitly or explicitly conceptualised diagnostic error as a discrepancy between a previously assigned clinical diagnosis (or lack thereof) and subsequent reappraisal. For example, in a youth community mental health sample, Jensen-Doss and colleagues compared clinician-generated diagnoses with the diagnoses generated by team consensus based on a structured diagnostic interview, medical record review and diagnostic impressions from team members. In this study, most discrepancies between clinician and team consensus diagnoses were attributable to missed diagnoses (ie, diagnoses not noted by the original clinician but subsequently assigned by team consensus). 23
Studies use similar approaches to reappraising prior mental disorder diagnoses with the aid of structured diagnostic interviews such as the Composite International Diagnostic Interview (CIDI), 24–26 Mini Neuropsychiatric Inventory (MINI), 2 , 7–32 Structured Clinical Interview for DSM Disorders (SCID), 33–36 or population-specific 37 or disorder-specific 38 interviews. Others report re-review of medical records to confirm diagnostic criteria. 39–41 However, there are several potential pitfalls of using diagnostic reappraisal to identify errors, including hindsight bias, failure to consider the disorder’s timing of onset, natural history or circumstances that might have complicated a previous diagnostic evaluation. 42 Moreover, methodological inconsistencies prevent comparisons across studies. For instance, whereas some studies of diagnostic discrepancies use structured interviews and other standardised methods for diagnostic assessment, others have inferred a previously ‘missed’ diagnosis solely based on a positive screening test without a more thorough assessment of diagnostic criteria. 43–47 Table 1 summarises recent approaches to identifying diagnostic error and recommendations for future studies.
- View inline
Empirical approaches for studying diagnostic error in mental health
More detailed conceptual and operational definitions for diagnostic errors are needed to measure and learn from these events. The NASEM report defines diagnostic error in terms of not only accuracy but also timeliness and communication: ‘the failure to (a) establish an accurate and timely explanation of the patient’s health problem(s) or (b) communicate that explanation to the patient.’ 4 Other recent definitions emphasise similar concepts and also introduce a component of preventability (‘missed opportunities’). 48 49 An acceptable or normative diagnostic interval is difficult to specify and must be balanced against unrealistic expectations that could invite hasty or overaggressive pursuit of diagnosis. 42 However, factors that are systematically associated with diagnostic accuracy or delays may point to missed opportunities. Such variation can also be examined in the context of health disparities ( table 1 ).
Importantly, conceptual models for understanding diagnostic error emphasise diagnosis as a process that unfolds within a complex system, sometimes across providers and locations. For example, the diagnostic process model in the NASEM report 4 ( figure 1 ), as well as the related Safer Dx framework, 50 describe five data gathering and interpretation processes: clinical history and interview, physical examination (including observation of appearance and behaviour), referral and consultation, diagnostic testing, and (in the latter) patient-related factors. Identifying process failures 51 (eg, did the clinician gather sufficient information to rule out an alternative diagnosis?), rather than focusing solely on the end result (eg, was the clinician’s original diagnosis correct?) enables more precise measurement of errors even when the ‘correct’ or final diagnosis cannot be confirmed, and allows for targeted improvements in the diagnostic process. Clinic-based studies are needed to better understand clinical reasoning and other diagnostic processes in practice. However, complementary evidence about clinical reasoning comes from vignette-based studies that experimentally manipulate patient characteristics, symptom presentation and specific instructions for diagnostic reasoning. 52–58 In a separate section below, we discuss further details of potential interventions to enhance the diagnostic process.
- Download figure
- Open in new tab
- Download powerpoint
The diagnostic process model from the National Academies of Science, Medicine and Engineering report Improving Diagnosis in Health Care 4 (reprinted with permission) emphasises data gathering and synthesis, as depicted in the circular portion of the diagram. To better describe the context of missed and delayed diagnosis in mental health, we suggest an elaboration of this model (depicted in the upper portion) that describes the steps and potential delays involved in seeking and accessing mental health services (adapted from Andersen et al 64 ).
Applying diagnostic process models to mental health
While formal concepts and definitions have potential to advance understanding of diagnostic error, it is important to ensure that they reflect the context of mental disorder diagnosis. For instance, while the NASEM model includes the initial steps of experiencing a health problem and engaging with the healthcare system, the model places less emphasis on these initial steps as compared with data gathering. This is an important limitation because patient knowledge and attitudes, stigma and structural barriers play a considerable role in mental healthcare delays. 59–61 A few studies of delayed diagnosis in mental health have defined the diagnostic process in terms of key clinical milestones (eg, first symptoms, first time seeking professional help and time of final, accurate diagnosis), altogether constituting the duration of untreated illness. For example, two studies depicted the evolution of a bipolar disorder diagnosis 62 63 in the form of a graph showing the total diagnostic timeline and the time elapsed between milestones. Other process-oriented models cited in this literature emphasise potential barriers and facilitators to care seeking (eg, Andersen’s behavioural model of health services 64 65 and the cascade of care model 66 ). To better account for the total delay in diagnosing mental disorders, elaboration of the NASEM model may be appropriate. The extension of the NASEM model shown in figure 1 is similar to depictions of the diagnostic pathway for other diseases such as cancer. 67 68
Evidence of diagnosis-specific pitfalls and process breakdowns
Studies have brought to light several pitfalls in the diagnosis of common mental disorders, which may inform further studies to identify and mitigate diagnostic errors. While not an exhaustive list, below is a summary of the some of the most frequently studied conditions in this literature. The degrees of both prevalence and interest in these conditions make them strong candidates for further research and development of improvement strategies:
Anxiety disorders. Despite the high prevalence of anxiety disorders (eg, generalised anxiety disorder, panic disorder, phobias), few studies focus on this category of disorders. The available data point to underdetection and misdiagnosis as common problems. In a study of children and adolescents, 18% of anxiety disorder diagnoses were missed by clinicians compared with 1% that were false positives. 23 A clinic-based study of adults found that 29% of major depressive disorder (MDD) diagnoses were not supported by findings on structured interview, and in about half of these cases, an anxiety disorder was a more appropriate diagnosis. 28 In a sample of 61 US veterans with a diagnosis of ‘anxiety disorder not otherwise specified,’ a more specific diagnosis was justified in 77% of cases, a meaningful finding given that patients with non-specific diagnoses were less likely to receive treatment. 35
Attention deficit hyperactivity disorder (ADHD). A systematic literature review on diagnostic error in children and adolescents did not identify a clear pattern or underdetection versus overdetection of ADHD. 69 However, US-based research has identified evidence of racial and ethnic disparities in ADHD diagnosis. For instance, even after adjusting for demographic and behavioural risk factors, white children are consistently more likely to be diagnosed with ADHD than their Black, Hispanic/Latino and Asian peers. 70–73 There is some evidence that diagnostic disparities between white and Black children has narrowed over time, but disparities in treatment have not narrowed in turn. 74 Additionally, a study of 685 children found evidence that ADHD was underdetected in children with neurological disorders, suggestive of diagnostic overshadowing. 75
Autism spectrum disorder (ASD). Older age at diagnosis is considered a marker of delayed identification, which may indicate missed opportunities in diagnosis. Children who are higher functioning and have less severe or atypical symptoms are at risk for later diagnosis. 65 76 77 Later diagnosis of ASD has also been associated with female gender, 78 79 lower family education and socioeconomic status, 76 77 79 80 less reliable access to healthcare, 65 66 history of adverse childhood experiences 81 and prior diagnosis of ADHD. 82 Racial and ethnic disparities in the diagnosis of ASD have been documented, 83 84 although findings are inconsistent across studies. 85 86
Mood disorders. Research suggests a variety of potential problems in the diagnosis of MDD. A self-reported clinical diagnosis of ‘depression’ had a 62% false-positive rate in a study of over 5000 US adults. 24 In a UK study of 441 people with a recent (past 5 years) diagnosis of MDD, 15% did not meet criteria for MDD or any mood disorder and 30% had undetected bipolar disorder (type I or II). 25 Studies performed outside of the USA and UK document care delays in MDD, 87 88 and a study from Israel found that underdetection occurred more frequently than false-positive diagnosis. 89 Missed and delayed diagnoses are consistently documented in bipolar disorder. 90 Patients with bipolar disorder often experience depressive episodes before (hypo)manic mood symptoms emerge, and thus a diagnostic journey from MDD to bipolar disorder can be expected in many cases. However, failure to assess previous episodes of elevated mood in a depressed patient is a source of diagnostic error. For example, in the aforementioned UK study, among patients with bipolar disorder who were first diagnosed with MDD, about half reported elevated mood symptoms even before their first MDD diagnosis. 25 Additional studies suggest possible missed opportunities to assess manic symptoms at the time of a mood disorder diagnosis, with a significant proportion of major depressive disorder diagnoses converted to bipolar disorder on re-evaluation. 29 91–94 Other studies suggest that bipolar disorder is often misdiagnosed initially as a psychotic disorder. 95 96
Schizophrenia is a challenging diagnosis, especially in the early stage of the disorder. Several studies suggest that an initial diagnosis of schizophrenia changes after further assessment within a short-term interval in 36–51% of patients. 40 97 98 However, it is unclear to what extent these initial incorrect diagnoses reflect ‘missed opportunities’ versus other diagnostic challenges. Another concerning signal for missed opportunities comes from studies of racial disparities, which show that Black patients are more likely than white patients to be diagnosed with schizophrenia even when adjusting for clinical and demographic risk factors. 99–101
To better understand these diagnostic pitfalls and translate them into preventive strategies, it will be important to clarify common diagnostic process breakdowns. Research on diagnostic error in other fields of medicine has identified both general and disease-specific pitfalls that can inform improvements to clinical training and practice. 102 Adaptation of existing frameworks to classify diagnostic process breakdown frameworks 51 103 for use in mental health settings may help facilitate future efforts. For instance, Fletcher et al ’s adaptation of a checklist to assess missed opportunities in diagnosis yielded good reviewer agreement on presence/absence of diagnostic errors in a review of 103 records of US veterans with anxiety disorder diagnoses. 11
Potential interventions to reduce diagnostic error in mental health
Although existing studies of diagnostic error have highlighted potential intervention targets, few studies have tested specific strategies to improve diagnostic decision-making and reduce error in psychiatric diagnosis. We are aware of only two publications that evaluated individual-level interventions to facilitate clinician cognition in ‘real time.’ In a randomised study of 475 clinicians who assigned diagnoses based on vignettes, use of checklists to facilitate assessment (vs no checklists) resulted in fewer false-positive diagnoses of MDD, generalised anxiety disorder and borderline personality disorder. However, checklist use also led to underdetection of MDD. 57 Another study randomised 137 mental health professionals to receive brief education about paediatric bipolar disorder, versus education about cognitive biases and corrective strategies, prior to evaluating four vignettes. Participants in the ‘de-biasing’ condition gave more accurate diagnostic impressions and made fewer errors. 54 Although both studies were conducted within low-fidelity simulations, they join a larger body of work suggesting that cognitive interventions may improve clinicians’ diagnostic performance. 104
Distributing the work of diagnosis among team members is another potential avenue for intervention that emerges from the literature. In a randomised trial, 296 new psychiatric outpatients were randomised to receive usual care vs the addition of a structured clinical interview (SCID) conducted by a psychiatric nurse within 2 weeks of the patient’s intake visit. Results of the interview were provided to the psychiatrist. Within 90 days, the diagnosis changed in 73% of the interview group vs 16% of patients assigned to usual care. 105 In primary care settings, where a large proportion of mental disorder diagnoses are identified, the integration of behavioural health professionals as team members may facilitate screening and diagnosis of mental disorders. 106 107 Integration of mental health services is supported by position statements from the American College of Physicians 108 and the American Academy of Family Physicians. 109 Further studies should evaluate how error in the diagnosis of mental disorders is conceptualised in primary care versus specialty mental health settings.
Interventions to reduce diagnostic errors in mental health need further development. Batstra et al advocated for a conservative ‘stepped diagnosis’ approach that allows for diagnostic evolution within an episode of care without delaying treatment. 110 Suggested interventions that have appeared in the diagnostic error literature, including second opinions, decision support tools and patient engagement strategies, are promising avenues for further investigation in mental health settings. 111 112
We aimed to summarise the state of current research on diagnostic error in mental disorders. The volume of literature on this topic indicates that diagnostic error is well understood to be a problem. However, an obstacle to progress is a lack of clear consensus on how to conceptualise, define and measure errors in mental health diagnosis. Formal definitions for diagnostic errors, if they are cited at all, are used inconsistently in the mental health literature and are not always consistent with definitions used elsewhere in the literature on diagnostic quality and safety. Without a useful way to conceptualise diagnostic errors, it will be difficult to gain insight into how best to prevent them.
Another limitation of much of the literature is that it is difficult to distinguish preventable diagnostic error from other possible causes of diagnostic delays or discrepancies. Very few studies use methods to assess whether sufficient information was available to make an earlier, correct diagnosis. Because variation in diagnosis is subject to many influences, some outside of the clinician’s control, future research should focus on identifying preventable missed opportunities. Fortunately, recent evidence suggests that strategies to identify missed diagnostic opportunities in record review can be adapted to mental health settings. 11 Framing diagnostic errors as learning opportunities is consistent with a culture of safety and improvement and can help break down barriers to open acknowledgement and discussion of this important issue. 113–115
Advancing concepts and measurement strategies will yield better estimates of diagnostic errors and help identify ways to prevent them. However, it is not necessary to quantify these with precision before working towards tools and interventions to reduce errors. Development of measurement methods and interventions can and should occur in parallel. Bridging the gap between the mental health field and the emerging field of diagnostic safety promises to enhance both fields and advance the science of improving patient care. Given the increasingly large share of the population who seek care for mental health problems, 116 117 even modest improvements in diagnostic quality have potential to translate to meaningful gains in patients’ health and quality of life.
Ethics statements
Patient consent for publication.
Not applicable.
Ethics approval
- Xing MJ , et al
- Primavera D ,
- Oliva M , et al
- Ohayon MM ,
- Thorpy MJ ,
- Carls G , et al
- Miller BT ,
- Mallaris Y , et al
- Traut-Mattausch E ,
- Jonas E , et al
- Aragonès E ,
- Zimmerman M ,
- Cacciatore J ,
- Wakefield JC
- Fletcher TL ,
- Vaghani V , et al
- Schildkrout B
- The Joint Commission
- Thornicroft G
- Graber MA ,
- Dawson JD , et al
- Yamauchi Y ,
- Shikino K , et al
- Hallyburton A ,
- Allison-Jones L
- Munro I , et al
- Korenstein D
- Turner KA ,
- Cullen SW ,
- Oberfield NC ,
- Jensen-Doss A ,
- Youngstrom EA ,
- Youngstrom JK , et al
- Martin-Key NA ,
- Barton-Owen G , et al
- Kessler RC ,
- Saunders EFH ,
- Mukherjee D ,
- Waschbusch DA , et al
- Mosolov S ,
- Ushkalova A ,
- Kostukova E , et al
- Kostaras P ,
- Bergiannaki J-D ,
- Psarros C , et al
- Sheehan DV ,
- Lecrubier Y ,
- Sheehan KH , et al
- Sheehan KH ,
- Shytle RD , et al
- Ramirez Basco M ,
- Bostic JQ ,
- Davies D , et al
- Leontieva L ,
- Kunik ME , et al
- Columbia University Department of Psychiatry
- Peña-Salazar C ,
- Arrufat F ,
- Santos JM , et al
- Samardžić RM ,
- Krstić D , et al
- Hilton NZ ,
- Ham E , et al
- Than W , et al
- Kim SJ , et al
- Ghesquiere AR ,
- Kinsey J , et al
- Faisal-Cury A ,
- Rodrigues DMO ,
- Matijasevich A
- Grady A , et al
- Pickett KE ,
- Petherick ES , et al
- Browder SE , et al
- ↵ Agency for Healthcare Research and Quality. User’s guide and glossary. AHRQ Common Formats for Event Reporting - Diagnostic Safety Version 1.0 , January . 2023 Available : https://www.psoppc.org/psoppc_web/publicpages/commonFormatsDSV1.0 [Accessed 21 Aug 2023 ].
- Schiff GD ,
- Kim S , et al
- Candelari AE , et al
- Kunst MJJ ,
- Van de Wiel M
- Jenkins MM ,
- Youngstrom EA
- Glazier K ,
- Calixte RM ,
- Rothschild R , et al
- Lemke JE , et al
- Andrade LH ,
- Mneimneh Z , et al
- Benjet C , et al
- Reardon T ,
- Creswell C , et al
- Drancourt N ,
- Lajnef M , et al
- Keramatian K ,
- Schaffer A , et al
- Andersen R ,
- Martinez M ,
- Thomas KC ,
- Williams CS , et al
- Nguyen H-AT ,
- Rosenberg J ,
- Kistin CJ , et al
- Webster A ,
- Scott S , et al
- Vedsted P ,
- Rubin G , et al
- Merten EC ,
- Margraf J , et al
- Hunter Guevara LR ,
- Dykhoff HJ , et al
- Morgan PL ,
- Hillemeier MM ,
- Farkas G , et al
- Hillemeier MM , et al
- Elliott MN ,
- Toomey SL , et al
- Glasofer A ,
- Hendriksen JGM ,
- Peijnenborgh J ,
- Aldenkamp AP , et al
- Mazurek MO ,
- Handen BL ,
- Wodka EL , et al
- Daniels AM ,
- Migliarese G ,
- Torriero S , et al
- Kurzius-Spencer M ,
- Mastergeorge AM , et al
- Chiang T-L ,
- Lin S-J , et al
- Acharya K ,
- Shiu C-S , et al
- Kentrou V ,
- de Veld DM ,
- Mataw KJ , et al
- Barnard-Brak L ,
- Morales-Alemán MM ,
- Tomeny K , et al
- McArthur D ,
- Hughes MM , et al
- Wallis KE ,
- Adebajo T ,
- Bennett AE , et al
- Anthony BJ , et al
- Huerta-Ramírez R ,
- Bertsch J ,
- Cabello M , et al
- Stagnaro JC ,
- Vommaro H , et al
- Kanat-Maymon Y
- J. Rakofsky J ,
- W. Dunlop B
- Bongards EN ,
- Daveney J ,
- Panagioti M ,
- Waheed W , et al
- Russell AMT ,
- Allwang C , et al
- Lu Z , et al
- Altamura AC ,
- Cesana BM , et al
- Knežević V ,
- Coulter C ,
- Margolis RL
- Lopez-Castroman J ,
- Leiva-Murillo JM ,
- Cegla-Schvartzman F , et al
- Olbert CM ,
- Nagendra A ,
- Strakowski SM ,
- Arnold LM , et al
- Volodarskaya M ,
- Ruan E , et al
- Spitzmueller C , et al
- O’Reilly G ,
- Kelly BD , et al
- Kashner TM ,
- Surís A , et al
- Bohnert KM ,
- Sripada RK ,
- Mach J , et al
- Walter HJ ,
- Vernacchio L ,
- Correa ET , et al
- Crowley RA ,
- Kirschner N , for the Health and Public Policy Committee of the American College of Physicians*
- American Academy of Family Physicians
- Batstra L ,
- Nieweg EH ,
- Pijl S , et al
- Morgan C , et al
- Meyer AND , et al
- Edmondson A
- Carmeli A ,
- Meyer AND ,
- Upadhyay DK ,
- Collins CA , et al
- Terlizzi EP ,
- Schiller JS
- American Psychiatric Association Presidential Report on the Assessment of Psychiatric Bed Needs in the United States
X @abradfordphd, @TDGiardina, @HardeepSinghMD
Correction notice This aritcle has been corrected since it was first published online. The funding statement has been updated. In addition, the author Ashley N D Meyer was incorrectly listed as Ashley Mayer. This has now been updated.
Contributors AB and HS contributed to the conception and design of the study. AB, AM, SK and TDG participated in data collection, data analysis and data interpretation. AB wrote the initial draft of the manuscript and revised the manuscript after peer review. AM, SK, TDG and HS critically reviewed the manuscript. All authors have read and approved the final version.
Funding This project was funded under contract number HHSP233201500022I/75P00119F37006 from the Agency for Healthcare Research and Quality (AHRQ), U.S. Department of Health and Human Services. Drs. Bradford, Giardina, Meyer, and Singh are partially supported by the Houston VA Health Services Research and Development (HSR&D) Center for Innovations in Quality, Effectiveness, and Safety (CIN13-413). Dr. Meyer is additionally supported by a U.S. Veterans Administration (VA) HSR&D Career Development Award (CDA-17-167); Dr. Giardina is additionally supported by AHRQ (K01-HS025474); and Dr. Singh is additionally supported by AHRQ (R01HS028595 and R18HS029347).
Competing interests None declared.
Provenance and peer review Not commissioned; externally peer reviewed.
Read the full text or download the PDF:
This paper is in the following e-collection/theme issue:
Published on 27.8.2024 in Vol 26 (2024)
Barriers and Facilitators to the Implementation of Digital Health Services for People With Musculoskeletal Conditions in the Primary Health Care Setting: Systematic Review
Authors of this article:

- Mark Leendert van Tilburg 1 , MSc ;
- Ivar Spin 1 , MSc ;
- Martijn F Pisters 2, 3, 4 , PhD ;
- J Bart Staal 5, 6 , PhD ;
- Raymond WJG Ostelo 7, 8 , PhD ;
- Miriam van der Velde 1, 2 , MSc ;
- Cindy Veenhof 1, 2, 3 , PhD ;
- Corelien JJ Kloek 1, 3 , PhD
1 Innovation of Movement Care Research Group, Research Centre for Healthy and Sustainable Living, HU University of Applied Sciences Utrecht, Utrecht, Netherlands
2 Department of Rehabilitation, Physiotherapy Science and Sports, UMC Utrecht Brain Center, University Medical Center Utrecht, Utrecht University, Utrecht, Netherlands
3 Center for Physical Therapy Research and Innovation in Primary Care, Julius Health Care Centers, Utrecht, Netherlands
4 Research Group Empowering Healthy Behaviour, Department of Health Innovations and Technology, Fontys University of Applied Sciences, Eindhoven, Netherlands
5 Musculoskeletal Rehabilitation Research Group, HAN University of Applied Sciences, Radboud University Medical Centre, Nijmegen, Netherlands
6 Radboud Institute for Health Sciences, IQ Healthcare, Radboud University Medical Center, Nijmegen, Netherlands
7 Department of Health Sciences, Faculty of Science, VU University, Amsterdam Movement Sciences Research Institute, Amsterdam, Netherlands
8 Department of Epidemiology and Data Science, Amsterdam University Medical Center, Location Vrije Universiteit, Amsterdam Movement Sciences Research Institute, Amsterdam, Netherlands
Corresponding Author:
Mark Leendert van Tilburg, MSc
Innovation of Movement Care Research Group
Research Centre for Healthy and Sustainable Living
HU University of Applied Sciences Utrecht
Heidelberglaan 7
Utrecht, 3584 CS
Netherlands
Phone: 31 618302750
Email: [email protected]
Background: In recent years, the effectiveness and cost-effectiveness of digital health services for people with musculoskeletal conditions have increasingly been studied and show potential. Despite the potential of digital health services, their use in primary care is lagging. A thorough implementation is needed, including the development of implementation strategies that potentially improve the use of digital health services in primary care. The first step in designing implementation strategies that fit the local context is to gain insight into determinants that influence implementation for patients and health care professionals. Until now, no systematic overview has existed of barriers and facilitators influencing the implementation of digital health services for people with musculoskeletal conditions in the primary health care setting.
Objective: This systematic literature review aims to identify barriers and facilitators to the implementation of digital health services for people with musculoskeletal conditions in the primary health care setting.
Methods: PubMed, Embase, and CINAHL were searched for eligible qualitative and mixed methods studies up to March 2024. Methodological quality of the qualitative component of the included studies was assessed with the Mixed Methods Appraisal Tool. A framework synthesis of barriers and facilitators to implementation was conducted using the Consolidated Framework for Implementation Research (CFIR). All identified CFIR constructs were given a reliability rating (high, medium, or low) to assess the consistency of reporting across each construct.
Results: Overall, 35 studies were included in the qualitative synthesis. Methodological quality was high in 34 studies and medium in 1 study. Barriers (–) of and facilitators (+) to implementation were identified in all 5 CFIR domains: “digital health characteristics” (ie, commercial neutral [+], privacy and safety [–], specificity [+], and good usability [+]), “outer setting” (ie, acceptance by stakeholders [+], lack of health care guidelines [–], and external financial incentives [–]), “inner setting” (ie, change of treatment routines [+ and –], information incongruence (–), and support from colleagues [+]), “characteristics of the healthcare professionals” (ie, health care professionals’ acceptance [+ and –] and job satisfaction [+ and –]), and the “implementation process” (involvement [+] and justification and delegation [–]). All identified constructs and subconstructs of the CFIR had a high reliability rating. Some identified determinants that influence implementation may be facilitators in certain cases, whereas in others, they may be barriers.
Conclusions: Barriers and facilitators were identified across all 5 CFIR domains, suggesting that the implementation process can be complex and requires implementation strategies across all CFIR domains. Stakeholders, including digital health intervention developers, health care professionals, health care organizations, health policy makers, health care funders, and researchers, can consider the identified barriers and facilitators to design tailored implementation strategies after prioritization has been carried out in their local context.
Introduction
Approximately 1.71 billion people experience musculoskeletal conditions, which are a major contributor to health care problems worldwide [ 1 ]. Worldwide population growth and aging will increase the burden of musculoskeletal conditions on health care in the upcoming decades [ 2 , 3 ]. Therefore, prevention, early detection, and optimal treatment of musculoskeletal conditions, which comprise one of the largest patient groups in primary care, become increasingly important [ 4 - 6 ]. However, patients experience barriers that decrease access to primary care services, such as geographic and transport-related barriers, lack of health insurance, no after-hours access, and a shortage of primary health care professionals [ 7 , 8 ]. A potential solution to optimize prevention and treatment of musculoskeletal conditions, reduce the burden of musculoskeletal conditions on health care, and improve accessibility in primary care is the use of digital health services.
Digital health is an umbrella term encompassing eHealth and mobile health, which are defined as the use of information and communications technology in support of health and health-related fields and the use of mobile wireless technologies for health [ 9 ]. Examples are video consultations between a health care professional and patient and the integration of apps within primary care treatment. There are several potential benefits to digital health services, such as improved cost-effectiveness, more information about the health status of the patient, better communication between patients and health care professionals, and more accessibility for patients [ 10 , 11 ]. Previous research supports the effectiveness of digital health services in reducing pain and improving functional disability, catastrophizing, coping ability, and self-efficacy [ 12 , 13 ].
Despite the benefits of digital health services, their use for musculoskeletal conditions in primary care is lagging. Therefore, a thorough implementation is needed, including the development of implementation strategies that potentially improve the use of digital health services for patients with musculoskeletal conditions in primary care. Important stakeholders for designing these implementation strategies are eHealth developers, health care professionals, health care organizations, health policy makers, health care funders, and researchers. The first step to design implementation strategies for local contexts is to perform a determinant analysis in a more specific context to gain insight into determinants that influence implementation from the perspective of patients and health care professionals. Several studies have identified barriers and facilitators to the implementation of digital health services in other settings and populations [ 14 - 17 ]. Some of these barriers for patients or health care professionals in these settings are workflow, resistance to change, costs, reimbursement, intervention design, and digital literacy. However, it remains unclear which barriers and facilitators are applicable for patients with musculoskeletal conditions in the primary health care setting and what the overarching narrative is for this patient population and setting. A generic overview of barriers and facilitators within this more specific context, which is the aim of this systematic review, is useful as a first step for a thorough implementation. A prioritization of these barriers and facilitators for various local contexts, that is, a specific primary care physiotherapy practice, would be the next step to design fitting implementation strategies for the local context [ 18 ].
A practical theory-based framework to guide for systematical assessment of barriers and facilitators that influence implementation is the Consolidated Framework for Implementation Research (CFIR) [ 18 ]. The CFIR consolidates implementation determinants from a broad array of implementation theories and is composed of 5 domains (intervention [digital health service] characteristics, outer setting, inner setting, characteristics of individuals [health care professionals], and the implementation process), and it provides a systematic way of identifying constructs that have been associated with effective implementation. The use of a framework such as CFIR to structure the overview of barriers and facilitators allows stakeholders undertaking implementation activities to focus on barriers and facilitators that are of most interest to them more easily and design implementation strategies that are specific to their local context [ 19 ].
No systematic overview of barriers and facilitators influencing the implementation of digital health services for people with musculoskeletal conditions in the primary health care setting exists to support these stakeholders in designing fitting implementation strategies. Therefore, the aim of this systematic literature review was to identify barriers and facilitators to the implementation of digital health for people with musculoskeletal conditions in the primary health care setting.
This systematic literature review of qualitative data from qualitative and mixed methods articles is reported following the enhancing transparency in reporting the synthesis of qualitative research statement [ 20 ]. Exclusively incorporating qualitative evidence in this systematic review enables a nuanced exploration of the multifaceted factors influencing implementation, providing diverse perspectives and in-depth insights from both patients and health care providers.
Search Strategy
The electronic databases PubMed, Embase, and CINAHL were searched to seek all available studies up to March 2024. The complete search strategy can be found in Multimedia Appendix 1 . Inclusion and exclusion criteria are presented in Textbox 1 .
Inclusion criteria
- Domain: adults (aged ≥18 years); musculoskeletal conditions (eg, low back pain, osteoarthritis, and total knee replacement); primary health care setting (eg, general practice and physiotherapy practice)
- Determinant: the health care professional (eg, general practitioners, physiotherapists, and occupational therapists) has provided digital health (eg, synchronous patient-therapist interactions through telephone or video consultations and asynchronous physical exercise training, coaching, and monitoring using web applications, wearables, and platforms) more than once during an intervention
- Outcome: data on barriers or facilitators to the implementation of digital health services that fit into one of the Consolidated Framework for Implementation Research domains; data of patients or health care professionals
- Article type: qualitative and mixed methods designs; full text in English is available
Exclusion criteria
- Determinant: web-based training programs for health care professionals
- Article type: articles with no qualitative component, such as a quantitative survey only
Selection of Studies
The web-based screening tool Rayyan was used for the selection of studies [ 21 ]. A total of 3 reviewers (MLvT, IS, and MvdV) conducted the inclusion of eligible articles. Articles were screened independently by 2 reviewers for eligibility based on title and abstract. When an article was potentially eligible for inclusion, a full paper copy of the report was obtained and screened independently by 2 reviewers. Disagreements between the reviewers regarding an article’s eligibility were resolved by discussion until consensus was reached. In case of disagreement, a fourth reviewer (CJJK) was consulted. In addition, reference tracking was performed in all included articles. The reasons for exclusion were recorded ( Figure 1 ) [ 22 ].

Data Extraction and Management
The reviewers extracted the following data using a standardized extraction form: first author, country, year of publication, aim, design and method of data collection and methods of analysis, sample, description of digital health service, and data on barriers or facilitators to the implementation of digital health services reported in the Results section.
Assessment of Methodological Quality
In total, 3 reviewers (MLvT, IS, and MvdV) independently assessed the methodological quality of the qualitative component of the included articles. The Mixed Methods Appraisal Tool (MMAT) was used to appraise studies for this review [ 23 ]. It is a 5-item tool designed to appraise the methodological quality of 5 categories of studies, including qualitative and mixed methods studies. The MMAT has established content validity and has been piloted across the mentioned methodologies [ 24 ]. The MMAT encompasses 2 initial screening questions: “Are there clear research questions?” and “Do the collected data allow to address the research questions?” Methodological quality assessment was only performed if “yes” could be answered for both screening questions. A detailed presentation of the individual ratings of each MMAT criterion was provided to inform the quality of the included studies. Overall sum scores were calculated based on the quality of the qualitative component only and presented as number of stars (*), with 0 and 1 star indicating low quality, 2 and 3 stars indicating medium quality, and 4 and 5 stars indicating high quality [ 25 ]. These cutoff values were determined by 2 reviewers (MLvT and IS), as the MMAT subscribes, and are arbitrary but useful for transparent data syntheses. Disagreements were resolved in a consensus meeting between the raters. When there was any disagreement, a fourth reviewer (CJJK) could be consulted but was not necessary. As the aim was to describe and synthesize a body of qualitative literature and not determine an effect size, the quality assessment was only included to inform the overall quality of the included articles and to determine the reliability rating.
Data Synthesis
A framework synthesis was performed, with secondary thematic analysis of the results section of the included articles. To synthesize the findings, the CFIR was used, using the 2009 version because the analysis began before the 2022 update [ 18 ]. Initially, MLvT and IS used an open coding process to identify barriers and facilitators to implementation and allocated them to the most fitting CFIR construct or subconstruct using a coding manual from the CFIR [ 26 ]. During the axial coding process, these open codes were organized into thematic categories representing barriers and facilitators to implementation. MLvT conducted the axial coding, which was reviewed by IS and CJJK on an iterative basis. As the thematic analysis progressed, recurring themes identified across the included studies informed the development of a comprehensive narrative for the generic overview of barriers and facilitators to implementation.
Next, all identified CFIR constructs or subconstructs were given (MLvT, IS, and MvdV) a reliability rating to review the consistency of reporting across each construct and the quality of the studies that identified them, which was also reported in another systematic review on barriers and facilitators in another context and aims to indicate confidence in the findings [ 27 ]. All disagreements were resolved through discussion until consensus was reached. Three levels of reliability were distinguished: (1) high reliability (the construct is consistently supported by >1 study of medium quality and 1 study of high quality or the construct is supported by at least 2 studies of high quality based on the MMAT); (2) medium reliability (the construct is supported by >1 study of medium quality or the construct is identified on the basis of at least 1 high-quality study based on the MMAT); and (3) low reliability (the construct is supported only by studies of low quality or single studies of medium quality based on the MMAT).
Study Selection
The literature search resulted in a total of 1516 articles found in the Embase, PubMed, and CINAHL databases. After removing duplicates, 1425 articles were screened based on title and abstract. This resulted in 95 studies that were screened full text, after which studies were excluded on outcome (n=27, 28%), article type (n=21, 22%), determinant (n=7, 7%), and domain (n=5, 5%). In 2 cases of initial disagreement between reviewers, a fourth reviewer (CJJK) was consulted. Finally, 35 studies were included in the qualitative synthesis [ 28 - 62 ]. No additional studies were found through reference checking. The study selection procedure is presented in Figure 1 .
Study Characteristics
Characteristics of the included studies are presented in Table 1 . Individual articles are ordered alphabetically within all presented tables. All included articles were published between 2011 and 2024. A total of 10 articles originated from Australia [ 31 , 38 , 40 , 44 , 47 , 48 , 52 , 54 , 57 , 60 ]; 9 articles originated from the Netherlands [ 28 - 30 , 35 , 39 , 43 , 45 , 46 , 62 ]; 4 articles originated from Canada [ 34 , 37 , 41 , 50 ]; 3 articles originated from the United Kingdom [ 51 , 53 , 59 ]; 2 articles originated from Brazil [ 36 , 58 ], Sweden [ 32 , 55 ], and France [ 42 , 61 ]; and 1 article originated from Denmark [ 56 ]. The digital health services mentioned in the included articles aimed to facilitate synchronous patient-therapist interactions through telephone or video consultations and to support asynchronous physical exercise training, coaching, and monitoring using web applications and platforms. The participants in the included articles primarily consisted of patients, physiotherapists, and general practitioners but also encompassed occupational therapists, dietitians, psychologists, and a pharmacist. Patients presented with a variety of musculoskeletal conditions, including knee and hip osteoarthritis, knee conditions, chronic nonspecific low back pain, Achilles tendinopathy, traumatic hand injury, anterior cruciate ligament reconstruction, shoulder joint replacement, and total knee replacement.
Information about methodological quality of the studies is presented in Table 2 . Almost all qualitative components of the included studies, assessed with the MMAT, were of high methodological quality. In total, 31 articles scored 5 stars, and 3 articles scored 4 stars. Qualitative component of 1 article was of medium methodological quality and scored 3 stars.
| Author, year, country | Aims of the study | Methods | Participants | Digital health service |
| Aily et al [ ], 2020; Brazil | In-person exercise therapy instructions along with a booklet and DVD to take home. Participants also received 6 motivational phone calls throughout the 12-week treatment | |||
| Arensman et al [ ], 2022; the Netherlands | The Physitrack app that allows physiotherapists to create and share personalized exercise programs with patients. The app allows patients to set reminders to perform their exercises, track their adherence, rate pain scores during the exercises, and send direct messages to their physiotherapists | |||
| Barton et al [ ], 2022; Australia | Telehealth care from physiotherapists throughout Australia | |||
| Bossen et al [ ], 2016; the Netherlands | E-Exercise is a 12-week intervention, which combines visits with a physiotherapist and a web-based physical activity intervention. Patients receive 4 face-to-face sessions and are supposed to complete 12 web-based assignments. The website has a portal for both patients and physiotherapists and contains text- and video-based information | |||
| Button et al [ ], 2018; the United Kingdom | TRAK is a web-based intervention for supporting rehabilitation of knee conditions, with a potential to enhance the quality of treatment components, such as health information provision, rehabilitation monitoring, remote support, and personalized exercise progression | |||
| Martínez de la Cal et al [ ], 2021; Spain | McKenzie Exercise Therapy and electroanalgesia based on telerehabilitation with the help of 10.1 “Quad Core” tablets | |||
| Cottrell et al [ ], 2017; Australia | Telerehabilitation: delivery of rehabilitation service at a distance using telecommunications technology | |||
| Dehainault et al [ ], 2024; France | Participants were presented with screenshots from the “Mon Coach Dos” and “Activ’Dos” mobile apps, with a standardized explanatory presentation framework. An information sheet about the apps was integrated into the slideshow presenting their description, creator, funding, and data use | |||
| Dunphy et al [ ], 2017; the United Kingdom | TRAK is a digital intervention developed to support self-management of knee conditions. TRAK provides a platform for individually tailored exercise programs with videos, detailed instructions and progress logs for individual exercises, a health information section, and a contact option that allows a patient to email a physiotherapist for additional support | |||
| Egerton et al [ ], 2017; Australia | The new model for primary care management of knee osteoarthritis includes a multidisciplinary team of health professionals using remote delivery options (primarily telephone) to provide ongoing “care support.” The GP refers the patient to the “care support team” following a brief initial consultation. The “care support team” staff will have skills in health behavior change plus expertise in current best practice for knee osteoarthritis management | |||
| Eriksson et al [ ], 2011; Sweden | A 2-month home-based video physiotherapy program, supervised by an experienced physiotherapist specializing in shoulder problems. | |||
| Ezzat et al [ ], 2022; Australia | GLA:D is a physiotherapist-led 8-week program, which includes 2 group education sessions, followed by 12 supervised, neuromuscular exercise therapy sessions. The program is delivered via telehealth or in person | |||
| Ezzat et al [ ], 2023; Australia | GLA:D is a physiotherapist-led 6- to 8-week program, which includes 2 to 3 group education sessions, followed by 12 supervised, neuromuscular exercise therapy sessions. The program is delivered via telehealth or in person | |||
| Farzad et al [ ], 2023; Canada | Web-based hand therapy interventions | |||
| Geraghty et al [ ], 2020; the United Kingdom | SupportBack is a web-based platform to support patients through a self-tailored, 6-week self-management program. Contents include exercises or a walking program with weekly goals, feedback, and advice. Patients also received 3 telephone calls from an musculoskeletal physiotherapist to provide reassurance, address concerns, problem-solve, and encourage continued engagement with the intervention and physical activity goals | |||
| Hasani et al [ ], 2021; Australia | Gym-based exercise program where the participants performed 4 sets of unilateral isotonic standing and seated calf raise exercises in a Smith machine (both sides, one leg at a time) 3 times per week, over 12 weeks Physiotherapists supervised 1 session per week via videoconference software (Zoom) that was downloaded to the participants’ smartphone | |||
| Hinman et al [ ], 2017; Australia | Participants were provided 7 internet-based Skype-delivered physical therapy sessions for 3 months, with the main purpose being to prescribe an individualized home-based strengthening program to be undertaken 3 times per week | |||
| Hjelmager et al [ ], 2019; Denmark | Distribution of health-related information via the internet | |||
| Kairy et al [ ], 2013; Canada | An in-home telerehabilitation program consisting of twice-a-week physiotherapy sessions for 8 weeks (total 16 sessions) by a videoconferencing system located in the participant’s home | |||
| Kelly et al [ ], 2022; Ireland | The use of technological platforms (eg, mobile, computer and tablet) in physiotherapy | |||
| Kingston et al [ ], 2015; Australia | The use of technology, namely, telehealth and the use of the internet | |||
| Kloek et al [ ], 2020; the Netherlands | The intervention consists of about 5 physiotherapy sessions in combination with a web-based application (E-Exercise). The web-based application contains a tailored 12-week behavioral graded activity program, videos with strength and mobility exercises, and videos and texts with information about osteoarthritis-related topics. | |||
| Lamper et al [ ], 2021; the Netherlands | The eCoach Pain is an electronic coach to facilitate pain rehabilitation. It supports the provision of integrated rehabilitation care with a shared biopsychosocial vision on health. Both patients and primary health care professionals use the eCoach Pain. It comprises a measurement tool for assessing complexity of the pain problem, diaries, pain education sessions, monitoring options, and a chat function | |||
| Lawford et al [ ], 2019; Australia | The patients received 5 to 10 telephone consultations over a 6-month period. Physiotherapists devised goals and an action plan for each patient that involved both a structured home exercise program and a physical activity plan. Patients also had access to a study website containing video demonstrations of each exercise | |||
| Van der Meer et al [ ], 2022; the Netherlands | eHealth included in the health care process of people with TMD | |||
| Östlind et al [ ], 2022; Sweden | A wearable activity tracker (Fitbit Flex 2) in combination with the Fitbit app for 12 weeks. The participants were asked to monitor their activity daily, and they received automatic feedback from the app | |||
| Palazzo et al [ ], 2016; France | The use of new technologies to decrease the burden of home-based exercise programs in chronic LBP | |||
| Passalent et al [ ], 2022; Canada | Technology for encouraging physical activity | |||
| Pereira et al [ ], 2023; Brazil | Physical therapy by telerehabilitation | |||
| Petrozzi et al [ ], 2021; Australia | Physical treatments combined with an internet-delivered psychosocial program called MoodGYM | |||
| Poolman et al [ ], 2024; the Netherlands | Back2Action is a newly developed biopsychosocial-blended intervention consisting of in-person physiotherapy sessions blended with psychologically informed digital health. The digital part of the intervention incorporates pain education and behavioral activation | |||
| Renard et al [ ], 2022; Canada | Teleconsultation follow‐ups | |||
| Van Tilburg et al [ ], 2022; the Netherlands | The patients received a stratified blended intervention, whereby a prognostic stratification tool, a web-based application (e-Exercise), and face-to-face physiotherapy sessions are integrated within physiotherapy treatment to create an optimal combination | |||
| Van Tilburg et al [ ], 2023; the Netherlands | A blended physiotherapy treatment (e-Exercise) for people with neck and shoulder conditions in which a smartphone app with personalized information, exercises, and physical activity modules was an integral part of physiotherapy treatment | |||
| De Vries et al [ ], 2017; the Netherlands | The web-based component of e-Exercise consists of a 12-week incremental physical activity program based on graded activity, strength and stability exercises, and information on osteoarthritis-related themes. The offline component consists of up to 5 face-to-face physiotherapy sessions |
a For mixed methods designs, only the data collection, data analysis, and participants from the qualitative component are described.
b LBP: low back pain.
c TRAK: Taxonomy for the Rehabilitation of Knee Conditions.
d N/OPSC: Neurosurgical and Orthopaedic Physiotherapy Screening Clinic.
e MDS: multidisciplinary service.
f ACL: anterior cruciate ligament.
g GP: general practitioner.
h GLA:D: Good Life with Osteoarthritis in Denmark.
i RE-AIM QuEST: Reach, Effectiveness, Adoption, Implementation, and Maintenance Qualitative Evaluation for Systematic Translation.
j TMD: temporomandibular disorder.
| Study | Criteria from the Mixed Methods Appraisal Tool: qualitative studies | Total number of stars (based on the qualitative component) | |||||
| 1.1 | 1.2 | 1.3 | 1.4 | 1.5 | |||
| Aily et al [ ], 2020 | 0 | 1 | 1 | 1 | 1 | *** | |
| Arensman et al [ ], 2022 | 1 | 1 | 1 | 1 | 1 | ***** | |
| Barton et al [ ], 2022 | 1 | 1 | 1 | 1 | 1 | ***** | |
| Bossen et al [ ], 2016 | 1 | 1 | 1 | 0 | 1 | **** | |
| Button et al [ ], 2018 | 1 | 1 | 1 | 1 | 1 | ***** | |
| Martínez de la Cal et al [ ], 2021 | 1 | 1 | 1 | 1 | 1 | ***** | |
| Cottrell et al [ ], 2017 | 1 | 1 | 1 | 1 | 1 | ***** | |
| Dehainault et al [ ], 2024 | 1 | 1 | 1 | 1 | 1 | ***** | |
| Dunphy et al [ ], 2017 | 1 | 1 | 1 | 1 | 1 | ***** | |
| Egerton et al [ ] | 1 | 1 | 1 | 1 | 1 | ***** | |
| Eriksson et al [ ], 2011 | 1 | 1 | 1 | 0 | 1 | **** | |
| Ezzat et al [ ], 2022 | 1 | 1 | 1 | 1 | 1 | ***** | |
| Ezzat et al [ ], 2023 | 1 | 1 | 1 | 1 | 1 | ***** | |
| Farzad et al [ ], 2023 | 1 | 1 | 1 | 1 | 1 | ***** | |
| Geraghty et al [ ], 2020 | 1 | 1 | 1 | 1 | 1 | ***** | |
| Hasani et al [ ], 2021 | 1 | 1 | 1 | 1 | 1 | ***** | |
| Hinman et al [ ], 2017 | 1 | 1 | 1 | 1 | 1 | ***** | |
| Hjelmager et al [ ], 2019 | 1 | 1 | 1 | 1 | 1 | ***** | |
| Kairy et al [ ], 2013 | 1 | 1 | 1 | 1 | 1 | ***** | |
| Kelly et al [ ], 2022 | 1 | 1 | 1 | 1 | 1 | ***** | |
| Kingston et al [ ], 2015 | 1 | 1 | 1 | 1 | 1 | ***** | |
| Kloek et al [ ], 2020 | 1 | 1 | 1 | 1 | 1 | ***** | |
| Lamper et al [ ], 2021 | 1 | 1 | 1 | 1 | 1 | ***** | |
| Lawford et al [ ], 2019 | 1 | 1 | 1 | 1 | 1 | ***** | |
| van der Meer et al [ ], 2022 | 1 | 1 | 1 | 1 | 1 | ***** | |
| Östlind et al [ ], 2022 | 1 | 1 | 1 | 1 | 1 | ***** | |
| Palazzo et al [ ], 2016 | 1 | 1 | 1 | 1 | 1 | ***** | |
| Passalent et al [ ], 2022 | 1 | 1 | 1 | 1 | 1 | ***** | |
| Pereira et al [ ], 2023 | 1 | 1 | 1 | 1 | 1 | ***** | |
| Petrozzi et al [ ], 2021 | 1 | 1 | 1 | 1 | 1 | ***** | |
| Poolman et al [ ], 2024 | 1 | 1 | 1 | 1 | 1 | ***** | |
| Renard et al [ ], 2022 | 1 | 1 | 1 | 1 | 1 | ***** | |
| van Tilburg et al [ ], 2022 | 1 | 1 | 1 | 1 | 1 | ***** | |
| van Tilburg et al [ ], 2023 | 1 | 1 | 1 | 1 | 1 | ***** | |
| De Vries et al [ ], 2017 | 1 | 1 | 1 | 0 | 1 | **** | |
a 1.1=Is the qualitative approach appropriate to answer the research question?
b 1.2=Are the qualitative data collection methods adequate to address the research question?
c 1.3=Are the findings adequately derived from the data?
d 1.4=Is the interpretation of results sufficiently substantiated by data?
e 1.5=Is there coherence between qualitative data sources, collection, analysis, and interpretation?
Barriers and Facilitators by CFIR
An overview of CFIR constructs or subconstructs influencing implementation of digital health services for patients with musculoskeletal conditions in the primary health care setting, with the sources and reliability rating, is presented in Table 3 . An overview of the data synthesis supported by illustrative quotes, is presented in Table 4 .
| CFIR domain, construct, and subconstruct | Studies | Reliability | ||||
| Innovation source | [ , , ] | High | ||||
| Relative advantage | [ - , - , - , - ] | High | ||||
| Adaptability | [ - , , - , , , - , , , , , ] | High | ||||
| Complexity | [ - , , , - , , , , , , , , ] | High | ||||
| Design quality and packaging | [ , , , , , , , , , , , , ] | High | ||||
| Cost | [ , , , , , , , , , ] | High | ||||
| Patient needs and resources | [ , , - , , , , - , - , , - ] | High | ||||
| External policy and incentives | [ , , , , , , ] | High | ||||
| Networks and communications | [ , , ] | High | ||||
| Tension for change | [ , , , , , , ] | High | ||||
| Compatibility | [ , , , , - , , , ] | High | ||||
| Learning climate | [ , ] | High | ||||
| Available resources | [ , , , , , , , , - , , , - , , , ] | High | ||||
| Access to knowledge and information | [ - , , , ] | High | ||||
| Knowledge and beliefs about the intervention | [ , , , - , - , , , ] | High | ||||
| Opinion leaders | [ ] | Medium | ||||
| Key stakeholders (health care professional) | [ , , , ] | High | ||||
| Executing | [ ] | Medium | ||||
a CFIR: Consolidated Framework for Implementation Research.
| CFIR domain, construct, and subconstruct | Barriers (–) and facilitators (+) with illustrative quotes | ||||
| Innovation source | ] | ||||
| Relative advantage | ] | ||||
| Adaptability | |||||
| Complexity | |||||
| Design quality and packaging | |||||
| Cost | |||||
| Patient needs and resources | |||||
| External policy and incentives | |||||
| Networks and communications | |||||
| Tension for change | |||||
| Compatibility | |||||
| Learning climate | |||||
| Available resources | |||||
| Access to knowledge and information | |||||
| Knowledge and beliefs about the intervention | |||||
| Opinion leaders | |||||
| Key stakeholders (health care professional) | |||||
Domain 1: Digital Health Service Characteristics
Innovation source (high reliability).
Commercially neutral digital health services may facilitate implementation according to health care professionals because logos of, for example, pharmaceutical companies could indicate economic instead of public health interests [ 42 , 56 ]. A link with an institution with a good image, such as a specialized hospital, may also be a facilitator to implementation, according to health care professionals, because it promotes trust [ 53 ].
Relative Advantage (High Reliability)
When patients or health care professionals experience a relative advantage of digital health services over usual care, this may facilitate implementation. Mentioned relative advantages were promoting adherence [ 28 - 30 , 33 , 43 , 49 , 53 , 61 , 62 ] , self-management [ 29 - 31 , 33 , 34 , 36 , 40 , 42 - 44 , 47 , 48 , 53 , 59 ] , empowerment [ 34 , 42 , 44 , 48 , 53 , 55 ] , motivation through support [ 28 , 31 - 33 , 37 , 38 , 43 , 53 , 59 - 61 ] , access to health care [ 29 , 34 , 36 , 38 , 40 , 41 , 44 , 45 , 47 - 50 , 52 - 54 , 56 , 60 , 62 ] , creating societal awareness [ 56 ] for specific health problems, and a continuous care chain [ 33 , 36 , 39 , 42 , 44 , 55 , 61 ]. The integration of digital health and therapy sessions (blended care) is described by patients and health care professionals as a facilitator because the digital health service can then be tailored to patient’s needs, complementary therapy can be offered, and self-efficacy can be enhanced [ 28 - 30 , 32 , 35 , 39 - 44 , 48 , 52 , 53 , 56 , 62 ]. However, there were also some concerns among health care professionals that quality of care may be reduced because, for example, physical examination may not be as thorough compared to usual face-to-face care [ 30 , 32 - 34 , 36 , 38 - 44 , 52 , 54 , 57 ] . On the contrary, some health care professionals believed that extra time and encouragement for the patient through a digital health service may result in better treatment outcomes. Advantages and disadvantages related to the patient–health care professional relationship were also experienced as both barriers and facilitators to implementation by patients and health care professionals [ 29 - 31 , 33 , 34 , 40 , 41 , 44 , 47 , 50 , 52 , 53 , 55 ]. Patients reported, for example, that when having health concerns, they prefer face-to-face reassurance over reassurance through a digital health service. Physiotherapists also had some concerns about creating a professional relationship if there are none or less face-to-face sessions. In contrast, they experienced that consulting via telephone forced them to focus on effective conversations, which allowed them to talk at a more personal level with patients. In addition, privacy and safety concerns may be barriers to implementation [ 36 , 40 , 42 - 44 , 52 ]. During the COVID-19 pandemic, safely providing health care from home was reported as a facilitator for implementation.
Adaptability (High Reliability)
Both health care professionals and patients agreed that adaptability of digital health services to fit the local context may be an important facilitator to implementation. Digital health services that are flexible to tailor to specific patient needs and suitable for various groups or subgroups of patients facilitate implementation [ 28 - 34 , 39 , 41 , 42 , 44 - 46 , 48 , 50 , 52 - 54 , 56 , 57 , 59 , 61 , 62 ]. Another facilitating determinant was an evolving intervention [ 43 , 56 , 61 ]. Use of a digital health service may increase if its content changes and information and features are continuously updated.
Complexity (High Reliability)
Complexity of digital health services that affect implementation is mostly linked to usability . Facilitating determinants concerning usability may be easy installation; easy to use; simple design and interface; simple navigation; visual support of text; and a not too wordy, manageable content [ 28 - 30 , 37 , 40 , 43 - 45 , 48 , 50 , 51 , 53 , 56 , 59 , 60 ]. Barriers concerning usability may be functional limitations of digital health services used in health care compared to those available on the commercial market. Another facilitating determinant to implementation was sufficient health care professional management for patients , such as updating relevant links and personal plans or the provision of technical aid by health care professionals to reduce complexity [ 28 , 53 , 55 ].
Design Quality and Packaging (High Reliability)
Experienced excellence in design quality and packaging of digital health services, such as variety and range of content and functionalities [ 29 , 30 , 32 , 35 , 37 , 45 , 53 , 59 , 61 , 62 ] , persuasive design [ 45 , 53 , 56 ] , and modality [ 33 , 34 , 40 , 45 , 53 , 61 ], may facilitate implementation according to both patients and health care professionals. Some mentioned functionalities are personal plans, exercise logs with speech notes as an alternative to text input, information modules with educational videos alongside written information, a progress dashboard with milestones, email or chat support, reminder tools, and feedback functions. An app was preferred over a website as modality, in particular, because of offline functionalities of an app.
Cost (High Reliability)
Costs associated with digital health services may be a barrier to implementation. Next to direct costs, a potential reduced number of treatment sessions [ 29 , 46 , 52 , 55 , 62 ] may both be a barrier and facilitator to implementation. Potential loss of income because of substitution of treatment sessions was experienced as a barrier by health care professionals. However, reducing treatment sessions may be a facilitator to some health care professionals because of efficiency, and offering innovative interventions attracts new patients, which is a financial incentive. Some health care professionals mentioned that patient expenses for digital health services may be a barrier to implementation [ 29 , 34 , 40 , 41 , 47 , 54 ]. In addition, digital health services may improve access to care for patients living in remote areas and may save them travel expenses, which was experienced as a facilitator to implementation.
Domain 2: Outer Setting
Patient needs and resources (high reliability).
Needs of patients may influence the participation in digital health. Personal traits of patients , such as poor digital literacy [ 28 , 33 , 42 , 45 , 46 , 49 , 51 , 52 ], poor communication skills [ 34 , 41 , 47 ], higher age [ 36 , 41 , 42 , 44 , 45 , 56 ], lack of motivation [ 28 , 31 , 35 , 38 , 42 , 44 , 45 , 51 , 53 , 58 , 61 ], maladaptive illness perceptions [ 36 , 61 ], and feeling depressed [ 61 ], may be barriers to adherence or participation and therefore to implementation of digital health in primary care. Moreover, entertaining strategies for performing exercises, such as exercises in a video game, might improve engagement according to patients, which facilitates implementation [ 61 ].
External Policy and Incentives (High Reliability)
Broad acceptance of digital health by patients, health care professionals, and health service funders creates trust for health care professionals that implementation is worthwhile. Therefore, acceptance by these stakeholders , or even the demand by stakeholders such as patients, may be an important facilitator to implementation [ 29 , 31 , 32 , 44 , 54 ]. The absence of health care guidelines [ 44 , 46 ], standards, or protocols in using digital health and strict privacy regulations [ 41 ] may be barriers to implementation. Another barrier to health care professionals may be a lack of external financial incentive if the digital health intervention aims to substitute treatment sessions [ 62 ].
Domain 3: Inner Setting
Networks and communications (high reliability).
Effective, useful, and timely channels of communication between health care professionals involved in the use of a digital health intervention may be facilitators to implementation [ 39 , 52 , 54 ]. An example is the quality and quantity of communication between a general practitioner and a care support team that provided remotely delivered interventions in a multidisciplinary intervention. Another facilitator is some sort of personal relationship between health care professionals that are involved in using a digital health service [ 54 ].
Implementation Climate—Tension for Change (High Reliability)
Health care professionals and patients agreed that there is a need for change, which was a facilitator to implementation of digital health. Problems that create a tension for change are poor accessibility to health care [ 49 , 52 , 57 ] because of for example medical comorbidities, poor health literacy or inconvenient appointment times, large distance to health care service, high burden of health care on health care professionals, no availability of a (specialized) health care professional, and the need for trustworthy information [ 56 ] .
Implementation Climate—Compatibility (High Reliability)
Integrating digital health services into usual care requires change of treatment routines, which may be a barrier to implementation, specifically because of lack of knowledge and practice to adapt routines, lack of confidence, and resistance to change of health care professionals [ 29 , 30 , 39 , 44 , 46 - 48 , 51 , 52 , 54 ]. Positive experiences with integrating digital health services into usual care may lead to more acceptability and may overcome this barrier. Moreover, incompatibility with other initiatives and guidelines may be barriers to implementation [ 54 ]. There are many initiatives and guidelines for management of musculoskeletal conditions, and whenever these are incompatible with a digital health service, treatment routines may become complicated and confusing. In addition, incompatibility with existing payment structures may lead to inequity of care and was a barrier to implementation according to health care professionals [ 54 ]. Health care professionals mentioned that information incongruence could be another barrier to implementation [ 54 ]. Safety may be affected when patient advice and information, provided by health care professionals and via digital health services, are incongruent and as a consequence cause the health care professional to spend extra time and effort to deal with conflicting messages.
Implementation Climate—Learning Climate (High Reliability)
The extent to which health care professionals feel as essential, valued, and knowledgeable partners in the implementation process creates a better climate for implementation. Facilitators to implementation of digital health services may be support from colleagues and that the professional autonomy of health care professionals was maintained [ 45 , 46 ].
Readiness for Implementation—Available Resources (High Reliability)
Available resources, including the availability of suitable infrastructure, may facilitate the implementation of digital health. Technology-related issues may be a barrier to implementation [ 32 , 33 , 36 , 38 , 40 , 43 , 48 - 51 , 53 , 55 , 60 ]. Both patients and health care professionals mentioned several technology-related issues, including troubles with initially setting up or operating the technology, insufficient battery life, poor or no internet connection, poor video quality, and audio problems. Moreover, time may both be a barrier as well as a facilitator to implementation [ 28 , 30 , 33 , 41 , 45 , 46 , 51 , 52 , 56 ]. Some health care professionals perceived digital health services as time saving, whereas others perceived it as an additional burden. This issue involves the lack of time to familiarize with, set up, personalize, and use the technology as well as the time investment required from health care professionals to assist patients. In addition, the lack of a quiet physical space for health care professionals as well as patients specifically for telerehabilitation may be a barrier to implementation [ 33 , 44 , 52 , 61 ]. Moreover, the lack of electronic health records may be a barrier to implementation [ 33 ].
Readiness for Implementation—Access to Knowledge and Information (High Reliability)
Access of health care professionals and patients to knowledge and information about the use of digital health services may be an important determinant that influences implementation. A health care professionals’ training before using the digital health intervention may be a facilitator to implementation [ 41 , 44 - 47 , 52 , 60 ]. Access for patients to explore the digital health intervention before a consultation and clear instructions in the form of a manual, webinar, videos, or face-to-face support were facilitators to implementation [ 30 , 32 , 40 , 43 , 44 , 46 , 51 ].
Domain 4: Characteristics of Health Care Professionals (Knowledge and Beliefs About the Intervention: High Reliability)
Health care professionals’ acceptance of a digital health intervention may both be a facilitator and barrier [ 29 , 33 , 42 , 44 - 47 , 52 , 54 , 60 , 62 ]. Resistance to change of health care professionals may be a barrier to implementation, but if health care professionals trust that their efforts to embrace change will be worthwhile, this may facilitate implementation. Most health care professionals are open to digital health services, as long as they have appropriate training and time to familiarize with the intervention and its content. If experiences with a digital health intervention exceeds health care professionals’ expectations, this results in intrinsic motivation for the digital health intervention, which promotes implementation. The feeling of maintaining professional autonomy and confidence of health care professionals in being able to deliver the digital health intervention may also facilitate implementation. Concerns about patient information confidentiality, the belief that a digital health intervention will not be as good as face-to-face care, and providing digital health for conditions perceived as low priority may be barriers to implementation related to health care professional acceptance. Moreover, concerns that health care professionals’ job satisfaction may diminish may be a barrier to implementation [ 48 , 54 , 60 ]. However, if digital health services enable more contact with patients, this is experienced as a promotion of health care professionals’ satisfaction. Another contribution to satisfaction was that digital health services may lead to less physically demanding care compared to usual care, which all may facilitate implementation.
Domain 5: Process
Engaging—opinion leaders (medium reliability).
Peer opinion leaders exert influence through their representativeness and credibility. When new digital health services are presented to a health care professional by a coworker who vouches for it ( peer opinion leader ), this may facilitate implementation [ 56 ].
Engaging—Key Stakeholders (Health Care Professional; High Reliability)
Involvement of health care professionals in the implementation of digital health services is a facilitating determinant to implementation that promotes confidence in digital health services [ 60 ]. Furthermore, the willingness of health care professionals to try digital health services may facilitate implementation [ 52 ]. Organizational uncertainties among key stakeholders, such as questions like “Who does it?” and “Who pays for it?” may be barriers to implementation [ 54 ]. In addition, setting up a technical support team may lead to feelings of support by the health care professional, which may facilitate implementation [ 50 ].
Executing (Medium Reliability)
Executing the implementation of digital health services might require some justification and delegation to key involved stakeholders, such as gym staff [ 60 ]. This may be a barrier to implementation as, for example, content of the digital health intervention (eg, specific gym exercises) may not always be conventional.
Principal Findings
In this systematic review, barriers and facilitators to the implementation of digital health services for people with musculoskeletal conditions in the primary health care setting were identified and synthesized according to the CFIR. Barriers and facilitators were identified within all 5 CFIR domains, and almost all constructs or subconstructs of the CFIR with synthesized barriers or facilitators had high reliability. Various stakeholders are involved in the implementation of digital health services for patients with musculoskeletal conditions in the primary care setting. The current determinant analysis provides a generic overview of barriers and facilitators that may be considered by stakeholders, such as digital health intervention developers, health care professionals, health care organizations, health policy makers, health care funders, and researchers, to design fitting implementation strategies [ 63 ]. As stakeholders mainly have influence on barriers and facilitators in specific CFIR domains, main results for stakeholders will be presented and discussed accordingly.
Identified barriers and facilitators that may especially be important for developers are from the domain “digital health service characteristics.” Facilitators within this domain include the flexibility of digital health services to tailor to specific patient needs, suitability for various subgroups, and high usability. Digital health service developers can consider these facilitators when developing and evaluating their product by using, for example, an eHealth framework, such as the Center for eHealth Research Roadmap [ 64 ]. An example of an existing digital health service that uses some of these facilitators is eHealth platform Physitrack, which was experienced by physiotherapists as user friendly, accessible, and helpful in providing personalized care [ 65 , 66 ]. Intervention design with nonoptimal usability was also identified as a barrier to implementation in other contexts, just as costs [ 14 - 17 ]. In this study, financial aspects, such as loss of income for health care providers because of potential substitution or patient expenses, were also shown to be important barriers to implementation for this specific context. Financial strategies to overcome these barriers when implementing digital health services for the context of patients with chronic illnesses living at home, such as changing the (patient) billing systems and fee structures, were suggested in previous research and may be relevant for developers to consider [ 67 ].
Identified barriers and facilitators that are especially important to health care professionals are from the domain “digital health service characteristics” and “outer setting.” A facilitator within the domain “digital health service characteristics” is the relative advantage of digital health over usual care, such as promoting adherence, self-management, empowerment, and access to health care. Important barriers are the concern that digital health services might negatively affect patient–health care professional relationship and quality of care, experienced additional burden of digital health services, and change of treatment routines. Existing workflow was also shown to be an important barrier in other contexts [ 16 ]. To use these facilitators and overcome these barriers, health care professionals might consider using previously developed implementation strategies used in another context, such as conducting educational meetings to train and educate colleague health professionals or conducting cyclical small tests of change [ 68 ]. Personal traits of patients, such as digital literacy, maladaptive illness perceptions, poor communication skills, and lack of confidence in the patient’s own physical ability, are barriers from the “outer setting.” An example of a previously developed tool for physiotherapists is the use of the Checklist Blended Physiotherapy [ 69 ]. This clinical decision aid to support the physiotherapist in the decision of whether a digital health service should be an integral part of physiotherapy treatment for an individual patient might be a strategy, which has yet to be evaluated.
Identified barriers and facilitators that are especially important to health policy makers are mostly from the domain “outer setting.” The lack of health care guidelines and lack of an external financial incentive were identified as barriers. The World Health Organization developed guideline recommendations on digital health services that can be used to develop guidelines for local contexts [ 9 ]. Changing reimbursement policies and clinician incentives are financial strategies that may are recommended to health policy makers [ 67 ]. Moreover, broad acceptance of digital health services by patients, health care professionals, and health service funders creates trust for health care professionals that implementation is worthwhile, which may facilitate implementation.
Identified barriers and facilitators that are especially relevant to health care organizations are mostly from the domain “inner setting.” Providing access to knowledge and information about the digital health intervention was found to be an important facilitator. In addition, an opinion leader and involvement of health care professionals facilitates implementation. Therefore, it is suggested that health care organizations consider implementation strategies, such as developing and distributing educational material as well as identifying and preparing champions, and inform local opinion leaders to develop stakeholder interrelationships [ 68 ]. Important barriers to overcome are technology-related issues and incompatibility with other initiatives, guidelines, and existing payment structures. Organizational uncertainties, such as questions like “Who does it?” and “Who pays for it?” are barriers to implementation that health care organizations must mainly overcome. To overcome these barriers, health care organizations are suggested to consider new sources of funding, involve executive boards, and try to form or join an innovation network [ 68 ].
Researchers can use the generic overview of barriers and facilitators of all domains to prioritize them for a local context, develop implementation strategies, test them, and systematically evaluate implementation outcomes. This is important because determinants are specific to the local context, and local contexts are ever changing [ 19 ].
Although several studies have identified barriers and facilitators to the implementation of digital health services in other settings than primary care or complex interventions in the primary care setting, this is the first systematic review of studies identifying and analyzing the facilitators and barriers of digital health services for people with musculoskeletal conditions in the primary health care setting. The results of this study are consistent with findings in other settings or the general health care setting [ 70 ]. Although the findings on the level of CFIR domains or subdomains are comparable to other contexts, the nuance in the description of the identified barriers and facilitators are mostly specific to primary care for patients with musculoskeletal conditions.
A strength of this systematic review is that all included articles had a mixed methods or qualitative design, and end-user perspectives of both patients and health care professionals were included, which led to a rich description of barriers and facilitators. However, it is important to note that many of the included studies did not follow a structured implementation process, and it was not possible to discuss whether implementation duration influenced the participants’ perspectives. Another strength is the use of the CFIR. Synthesizing according to the CFIR makes our findings easier comparable to other implementation studies and supports the use of common terminology in this field. Despite the careful execution of this study, there are some methodological considerations. The quality of the qualitative component was assessed by presenting stars. Cutoff values were determined by the authors; however, these cutoff values are arbitrary, which may have influenced the interpretation of the quality of included articles. In addition, a reliability rating was used to indicate confidence in the findings. While this approach took consistency and quality of the studies into account, we acknowledge that tools such as GRADE-CERQual were not used, which assesses confidence in findings from a more comprehensive perspective, considering factors such as coherence and adequacy. Incorporating GRADE-CERQual or similar methods in future research could enhance confidence in findings of a qualitative data synthesis [ 71 ]. The context of this review was digital health services, the primary care setting, and musculoskeletal conditions. People with musculoskeletal conditions are one of the largest patient groups in the primary health care setting. Although this patient group is very heterogenous, there are some transcendent key recommendations for patients with musculoskeletal conditions in primary health care, which makes the context sufficiently specific to inform relevant stakeholders [ 72 ]. Specific types of digital health services researched in the included articles were also very heterogenous. Therefore, it was not possible to specify barriers and facilitators to implementation for different types of digital health services. This should be considered when developing implementation strategies for specific digital health services. This systematic review provides a generic overview, and reliability was presented on the level of subconstructs and not on the level of individual determinants. Therefore, a prioritization of determinants should be carried out for the local context, as a first step in designing implementation strategies [ 19 ].
Conclusions
This systematic review provides an extensive description of the barriers and facilitators to the implementation of digital health services for people with musculoskeletal conditions in the primary health care setting. The findings are based on the synthesis of 35 qualitative and mixed methods articles through the CFIR. Barriers and facilitators were identified across all 5 CFIR domains, and nearly all constructs or subconstructs of the CFIR with synthesized barriers or facilitators had high reliability. This suggests that the implementation process can be complex and requires implementation strategies across all CFIR domains. Stakeholders, such as digital health intervention developers, health care professionals, health care organizations, health policy makers, health care funders, and researchers, can consider the identified barriers and facilitators to design tailored implementation strategies after a prioritization has been carried out in their local context.
Acknowledgments
The authors would like to thank the authors of all data used in the review.
Data Availability
The data sets generated and analyzed during this study are available from the corresponding author on reasonable request.
Conflicts of Interest
None declared.
Search strategy.
Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) checklist.
- Cieza A, Causey K, Kamenov K, Hanson SW, Chatterji S, Vos T. Global estimates of the need for rehabilitation based on the Global Burden of Disease study 2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. Dec 19, 2021;396(10267):2006-2017. [ FREE Full text ] [ CrossRef ] [ Medline ]
- World report on ageing and health. World Health Organization. 2015. URL: https://www.who.int/publications/i/item/9789241565042#:~:text=The%20World%20report%20on%20ageing,new%20concept%20of%20functional%20ability [accessed 2024-04-29]
- GBD 2019 DiseasesInjuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. Oct 17, 2020;396(10258):1204-1222. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Friedberg MW, Hussey PS, Schneider EC. Primary care: a critical review of the evidence on quality and costs of health care. Health Aff (Millwood). May 2010;29(5):766-772. [ CrossRef ] [ Medline ]
- Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q. Oct 03, 2005;83(3):457-502. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Shi L. The impact of primary care: a focused review. Scientifica (Cairo). 2012;2012:432892. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Douthit N, Kiv S, Dwolatzky T, Biswas S. Exposing some important barriers to health care access in the rural USA. Public Health. Jun 2015;129(6):611-620. [ CrossRef ] [ Medline ]
- Bodenheimer T, Pham HH. Primary care: current problems and proposed solutions. Health Aff (Millwood). May 2010;29(5):799-805. [ CrossRef ] [ Medline ]
- WHO guideline recommendations on digital interventions for health system strengthening. World Health Organization. URL: https://www.ncbi.nlm.nih.gov/books/NBK541902/ [accessed 2024-04-29]
- Catwell L, Sheikh A. Evaluating eHealth interventions: the need for continuous systemic evaluation. PLoS Med. Aug 18, 2009;6(8):e1000126. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Elbert NJ, van Os-Medendorp H, van Renselaar W, Ekeland AG, Hakkaart-van Roijen L, Raat H, et al. Effectiveness and cost-effectiveness of ehealth interventions in somatic diseases: a systematic review of systematic reviews and meta-analyses. J Med Internet Res. Apr 16, 2014;16(4):e110. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Hewitt S, Sephton R, Yeowell G. The effectiveness of digital health interventions in the management of musculoskeletal conditions: systematic literature review. J Med Internet Res. Jun 05, 2020;22(6):e15617. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Kloek CJ, Bossen D, Spreeuwenberg PM, Dekker J, de Bakker DH, Veenhof C. Effectiveness of a blended physical therapist intervention in people with hip osteoarthritis, knee osteoarthritis, or both: a cluster-randomized controlled trial. Phys Ther. Jul 01, 2018;98(7):560-570. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Mishuris RG, Stewart M, Fix GM, Marcello T, McInnes DK, Hogan TP, et al. Barriers to patient portal access among veterans receiving home-based primary care: a qualitative study. Health Expect. Dec 12, 2015;18(6):2296-2305. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Kruse CS, Atkins JM, Baker TD, Gonzales EN, Paul JL, Brooks M. Factors influencing the adoption of telemedicine for treatment of military veterans with post-traumatic stress disorder. J Rehabil Med. May 08, 2018;50(5):385-392. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Hadjistavropoulos HD, Nugent MM, Dirkse D, Pugh N. Implementation of internet-delivered cognitive behavior therapy within community mental health clinics: a process evaluation using the consolidated framework for implementation research. BMC Psychiatry. Sep 12, 2017;17(1):331. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Batterham PJ, Sunderland M, Calear AL, Davey CG, Christensen H, Teesson M, et al. Developing a roadmap for the translation of e-mental health services for depression. Aust N Z J Psychiatry. Sep 23, 2015;49(9):776-784. [ CrossRef ] [ Medline ]
- Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. Aug 07, 2009;4(1):50. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Nilsen P, Bernhardsson S. Context matters in implementation science: a scoping review of determinant frameworks that describe contextual determinants for implementation outcomes. BMC Health Serv Res. Mar 25, 2019;19(1):189. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Tong A, Flemming K, McInnes E, Oliver S, Craig J. Enhancing transparency in reporting the synthesis of qualitative research: ENTREQ. BMC Med Res Methodol. Nov 27, 2012;12(1):181. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan-a web and mobile app for systematic reviews. Syst Rev. Dec 05, 2016;5(1):210. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. Jul 21, 2009;339:b2700. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Pluye P, Gagnon M, Griffiths F, Johnson-Lafleur J. A scoring system for appraising mixed methods research, and concomitantly appraising qualitative, quantitative and mixed methods primary studies in Mixed Studies Reviews. Int J Nurs Stud. Apr 2009;46(4):529-546. [ CrossRef ] [ Medline ]
- Souto RQ, Khanassov V, Hong QN, Bush PL, Vedel I, Pluye P. Systematic mixed studies reviews: updating results on the reliability and efficiency of the Mixed Methods Appraisal Tool. Int J Nurs Stud. Jan 2015;52(1):500-501. [ CrossRef ] [ Medline ]
- Hong QN. Reporting the results of the MMAT. Mixed Methods Appraisal Tool. URL: http://mixedmethodsappraisaltoolpublic.pbworks.com/ [accessed 2024-04-29]
- CFIR codebook. Consolidated Framework for Implementation Research. 2014. URL: https://cfirguide.org/wp-content/uploads/2019/08/cfircodebooktemplate10-27-2014.docx [accessed 2024-04-29]
- Bach-Mortensen AM, Lange BC, Montgomery P. Barriers and facilitators to implementing evidence-based interventions among third sector organisations: a systematic review. Implement Sci. Jul 30, 2018;13(1):103. [ FREE Full text ] [ CrossRef ] [ Medline ]
- de Vries HJ, Kloek CJ, de Bakker DH, Dekker J, Bossen D, Veenhof C. Determinants of adherence to the online component of a blended intervention for patients with hip and/or knee osteoarthritis: a mixed methods study embedded in the e-Exercise trial. Telemed J E Health. Dec 2017;23(12):1002-1010. [ CrossRef ] [ Medline ]
- van der Meer HA, de Pijper L, van Bruxvoort T, Visscher CM, Nijhuis-van der Sanden MW, Engelbert RH, et al. Using e-Health in the physical therapeutic care process for patients with temporomandibular disorders: a qualitative study on the perspective of physical therapists and patients. Disabil Rehabil. Feb 16, 2022;44(4):617-624. [ CrossRef ] [ Medline ]
- van Tilburg ML, Kloek CJ, Foster NE, Ostelo RW, Veenhof C, Staal JB, et al. Development and feasibility of stratified primary care physiotherapy integrated with eHealth in patients with neck and/or shoulder complaints: results of a mixed methods study. BMC Musculoskelet Disord. Mar 09, 2023;24(1):176. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Petrozzi MJ, Spencer G, Mackey MG. A process evaluation of the Mind Your Back trial examining psychologically informed physical treatments for chronic low back pain. Chiropr Man Therap. Aug 17, 2021;29(1):32. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Östlind E, Ekvall Hansson E, Eek F, Stigmar K. Experiences of activity monitoring and perceptions of digital support among working individuals with hip and knee osteoarthritis - a focus group study. BMC Public Health. Aug 30, 2022;22(1):1641. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Kelly M, Fullen BM, Martin D, Bradley C, McVeigh JG. eHealth interventions to support self-management: perceptions and experiences of people with musculoskeletal disorders and physiotherapists - 'eHealth: It's TIME': a qualitative study. Physiother Theory Pract. May 25, 2024;40(5):1011-1021. [ CrossRef ] [ Medline ]
- Renard M, Gaboury I, Michaud F, Tousignant M. The acceptability of two remote monitoring modalities for patients waiting for services in a physiotherapy outpatient clinic. Musculoskeletal Care. Sep 10, 2022;20(3):616-624. [ CrossRef ] [ Medline ]
- Poolman EY, Vorstermans L, Donker MH, Bijker L, Coppieters MW, Cuijpers P, et al. How people with persistent pain experience in-person physiotherapy blended with biopsychosocial digital health - a qualitative study on participants' experiences with Back2Action. Internet Interv. Jun 2024;36:100731. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Pereira TA, Santos IB, Mota RF, Fukusawa L, Azevedo-Santos IF, DeSantana JM. Beliefs and expectations of patients with fibromyalgia about telerehabilitation during COVID-19 pandemic: a qualitative study. Musculoskelet Sci Pract. Oct 2023;67:102852. [ CrossRef ] [ Medline ]
- Passalent L, Cyr A, Jurisica I, Mathur S, Inman RD, Haroon N. Motivators, barriers, and opportunity for e-Health to encourage physical activity in axial Spondyloarthritis: a qualitative descriptive study. Arthritis Care Res (Hoboken). Jan 20, 2022;74(1):50-58. [ CrossRef ] [ Medline ]
- Ezzat AM, Bell E, Kemp J, O'Halloran P, Russell T, Wallis J, et al. "Much better than I thought it was going to be": telehealth delivered group-based education and exercise was perceived as acceptable among people with knee osteoarthritis. Osteoarthr Cartil Open. Sep 2022;4(3):100271. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Lamper C, Huijnen I, de Mooij M, Köke A, Verbunt J, Kroese M. An eCoach-pain for patients with chronic musculoskeletal pain in interdisciplinary primary care: a feasibility study. Int J Environ Res Public Health. Nov 06, 2021;18(21):11661. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Barton CJ, Ezzat AM, Merolli M, Williams CM, Haines T, Mehta N, et al. "It's second best": a mixed-methods evaluation of the experiences and attitudes of people with musculoskeletal pain towards physiotherapist delivered telehealth during the COVID-19 pandemic. Musculoskelet Sci Pract. Apr 2022;58:102500. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Farzad M, MacDermid J, Ferreira L, Szekeres M, Cuypers S, Shafiee E. A description of the barriers, facilitators, and experiences of hand therapists in providing remote (tele) rehabilitation: an interpretive description approach. J Hand Ther. Oct 2023;36(4):805-816. [ CrossRef ] [ Medline ]
- Dehainault M, Gaillard O, Ouattara B, Peurois M, Begue C. Physical activity advice given by French general practitioners for low back pain and the role of digital e-health applications: a qualitative study. BMC Prim Care. Jan 29, 2024;25(1):44. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Arensman R, Kloek C, Pisters M, Koppenaal T, Ostelo R, Veenhof C. Patient perspectives on using a smartphone app to support home-based exercise during physical therapy treatment: qualitative study. JMIR Hum Factors. Sep 13, 2022;9(3):e35316. [ FREE Full text ] [ CrossRef ] [ Medline ]
- M Ezzat A, Kemp JL, J Heerey J, F Pazzinatto M, De Oliveira Silva D, Dundules K, et al. Implementation of the good life with osteoArthritis in Denmark (GLA:D) program via telehealth in Australia: a mixed-methods program evaluation. J Telemed Telecare. Apr 20, 2023:1357633X231167620. [ CrossRef ] [ Medline ]
- van Tilburg ML, Kloek CJ, Staal JB, Bossen D, Veenhof C. Feasibility of a stratified blended physiotherapy intervention for patients with non-specific low back pain: a mixed methods study. Physiother Theory Pract. Feb 20, 2022;38(2):286-298. [ CrossRef ] [ Medline ]
- Kloek CJ, Bossen D, de Vries HJ, de Bakker DH, Veenhof C, Dekker J. Physiotherapists' experiences with a blended osteoarthritis intervention: a mixed methods study. Physiother Theory Pract. May 28, 2020;36(5):572-579. [ CrossRef ] [ Medline ]
- Lawford BJ, Delany C, Bennell KL, Hinman RS. "I was really pleasantly surprised": firsthand experience and shifts in physical therapist perceptions of telephone-delivered exercise therapy for knee osteoarthritis-a qualitative study. Arthritis Care Res (Hoboken). Apr 28, 2019;71(4):545-557. [ CrossRef ] [ Medline ]
- Hinman RS, Nelligan RK, Bennell KL, Delany C. "Sounds a bit crazy, but it was almost more personal:" a qualitative study of patient and clinician experiences of physical therapist-prescribed exercise for knee osteoarthritis via skype. Arthritis Care Res (Hoboken). Dec 02, 2017;69(12):1834-1844. [ CrossRef ] [ Medline ]
- Martínez de la Cal J, Fernández-Sánchez M, Matarán-Peñarrocha GA, Hurley DA, Castro-Sánchez AM, Lara-Palomo IC. Physical therapists' opinion of e-Health treatment of chronic low back pain. Int J Environ Res Public Health. Feb 16, 2021;18(4):1889. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Kairy D, Tousignant M, Leclerc N, Côté AM, Levasseur M, Researchers T. The patient's perspective of in-home telerehabilitation physiotherapy services following total knee arthroplasty. Int J Environ Res Public Health. Aug 30, 2013;10(9):3998-4011. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Button K, Nicholas K, Busse M, Collins M, Spasić I. Integrating self-management support for knee injuries into routine clinical practice: TRAK intervention design and delivery. Musculoskelet Sci Pract. Feb 2018;33:53-60. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Cottrell MA, Hill AJ, O'Leary SP, Raymer ME, Russell TG. Service provider perceptions of telerehabilitation as an additional service delivery option within an Australian neurosurgical and orthopaedic physiotherapy screening clinic: a qualitative study. Musculoskelet Sci Pract. Dec 2017;32:7-16. [ CrossRef ] [ Medline ]
- Dunphy E, Hamilton FL, Spasić I, Button K. Acceptability of a digital health intervention alongside physiotherapy to support patients following anterior cruciate ligament reconstruction. BMC Musculoskelet Disord. Nov 21, 2017;18(1):471. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Egerton T, Nelligan R, Setchell J, Atkins L, Bennell KL. General practitioners' perspectives on a proposed new model of service delivery for primary care management of knee osteoarthritis: a qualitative study. BMC Fam Pract. Sep 07, 2017;18(1):85. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Eriksson L, Lindström B, Ekenberg L. Patients' experiences of telerehabilitation at home after shoulder joint replacement. J Telemed Telecare. Jan 01, 2011;17(1):25-30. [ CrossRef ] [ Medline ]
- Hjelmager DM, Vinther LD, Poulsen SH, Petersen LS, Jensen MB, Riis A. Requirements for implementing online information material for patients with low back pain in general practice: an interview study. Scand J Prim Health Care. Mar 31, 2019;37(1):60-68. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Kingston GA, Judd J, Gray MA. The experience of medical and rehabilitation intervention for traumatic hand injuries in rural and remote North Queensland: a qualitative study. Disabil Rehabil. May 26, 2015;37(5):423-429. [ CrossRef ] [ Medline ]
- Aily JB, Barton CJ, Mattiello SM, De Oliveira Silva D, De Noronha M. Telerehabilitation for knee osteoarthritis in Brazil: a feasibility study. Int J Telerehabil. Dec 08, 2020;12(2):137-148. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Geraghty AW, Roberts LC, Stanford R, Hill JC, Yoganantham D, Little P, et al. Exploring patients' experiences of internet-based self-management support for low back pain in primary care. Pain Med. Sep 01, 2020;21(9):1806-1817. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Hasani F, Malliaras P, Haines T, Munteanu SE, White J, Ridgway J, et al. Telehealth sounds a bit challenging, but it has potential: participant and physiotherapist experiences of gym-based exercise intervention for Achilles tendinopathy monitored via telehealth. BMC Musculoskelet Disord. Feb 04, 2021;22(1):138. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Palazzo C, Klinger E, Dorner V, Kadri A, Thierry O, Boumenir Y, et al. Barriers to home-based exercise program adherence with chronic low back pain: patient expectations regarding new technologies. Ann Phys Rehabil Med. Apr 2016;59(2):107-113. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Bossen D, Kloek C, Snippe HW, Dekker J, de Bakker D, Veenhof C. A blended intervention for patients with knee and hip osteoarthritis in the physical therapy practice: development and a pilot study. JMIR Res Protoc. Feb 24, 2016;5(1):e32. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Lau R, Stevenson F, Ong BN, Dziedzic K, Treweek S, Eldridge S, et al. Achieving change in primary care--causes of the evidence to practice gap: systematic reviews of reviews. Implement Sci. Mar 22, 2016;11(1):40. [ FREE Full text ] [ CrossRef ] [ Medline ]
- van Gemert-Pijnen JE, Nijland N, van Limburg M, Ossebaard HC, Kelders SM, Eysenbach G, et al. A holistic framework to improve the uptake and impact of eHealth technologies. J Med Internet Res. Dec 05, 2011;13(4):e111. [ FREE Full text ] [ CrossRef ] [ Medline ]
- van der Meer HA, Doomen A, Visscher CM, Engelbert RH, Nijhuis-van der Sanden MW, Speksnijder CM. The additional value of e-Health for patients with a temporomandibular disorder: a mixed methods study on the perspectives of orofacial physical therapists and patients. Disabil Rehabil Assist Technol. Feb 12, 2024;19(2):433-445. [ CrossRef ] [ Medline ]
- Be the hero in your client's health journey. Physitrack®. URL: https://www.physitrack.com/ [accessed 2024-04-29]
- Varsi C, Solberg Nes L, Kristjansdottir OB, Kelders SM, Stenberg U, Zangi HA, et al. Implementation strategies to enhance the implementation of eHealth programs for patients with chronic illnesses: realist systematic review. J Med Internet Res. Sep 27, 2019;21(9):e14255. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Waltz TJ, Powell BJ, Matthieu MM, Damschroder LJ, Chinman MJ, Smith JL, et al. Use of concept mapping to characterize relationships among implementation strategies and assess their feasibility and importance: results from the Expert Recommendations for Implementing Change (ERIC) study. Implement Sci. Aug 07, 2015;10(1):109. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Kloek CJ, Janssen J, Veenhof C. Development of a checklist to assist physiotherapists in determination of patients' suitability for a blended treatment. Telemed J E Health. Aug 01, 2020;26(8):1051-1065. [ CrossRef ] [ Medline ]
- Schreiweis B, Pobiruchin M, Strotbaum V, Suleder J, Wiesner M, Bergh B. Barriers and facilitators to the implementation of eHealth services: systematic literature analysis. J Med Internet Res. Nov 22, 2019;21(11):e14197. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Lewin S, Booth A, Glenton C, Munthe-Kaas H, Rashidian A, Wainwright M, et al. Applying GRADE-CERQual to qualitative evidence synthesis findings: introduction to the series. Implement Sci. Jan 25, 2018;13(Suppl 1):2. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Lin I, Wiles L, Waller R, Goucke R, Nagree Y, Gibberd M, et al. What does best practice care for musculoskeletal pain look like? Eleven consistent recommendations from high-quality clinical practice guidelines: systematic review. Br J Sports Med. Jan 2020;54(2):79-86. [ CrossRef ] [ Medline ]
Abbreviations
| Consolidated Framework for Implementation Research |
| Mixed Methods Appraisal Tool |
Edited by A Mavragani; submitted 13.06.23; peer-reviewed by J Ross, LA Gomes; comments to author 07.10.23; revised version received 01.12.23; accepted 10.04.24; published 27.08.24.
©Mark Leendert van Tilburg, Ivar Spin, Martijn F Pisters, J Bart Staal, Raymond WJG Ostelo, Miriam van der Velde, Cindy Veenhof, Corelien JJ Kloek. Originally published in the Journal of Medical Internet Research (https://www.jmir.org), 27.08.2024.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work, first published in the Journal of Medical Internet Research (ISSN 1438-8871), is properly cited. The complete bibliographic information, a link to the original publication on https://www.jmir.org/, as well as this copyright and license information must be included.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 23 August 2024
The use of artificial neural networks in studying the progression of glaucoma
- Filip Târcoveanu 1 ,
- Florin Leon 2 ,
- Cătălin Lisa 3 ,
- Silvia Curteanu 3 ,
- Andreea Feraru 4 ,
- Kashif Ali 5 &
- Nicoleta Anton ORCID: orcid.org/0000-0002-4987-5049 1
Scientific Reports volume 14 , Article number: 19597 ( 2024 ) Cite this article
120 Accesses
1 Altmetric
Metrics details
- Applied mathematics
- Eye diseases
- Optic nerve diseases
In ophthalmology, artificial intelligence methods show great promise due to their potential to enhance clinical observations with predictive capabilities and support physicians in diagnosing and treating patients. This paper focuses on modelling glaucoma evolution because it requires early diagnosis, individualized treatment, and lifelong monitoring. Glaucoma is a chronic, progressive, irreversible, multifactorial optic neuropathy that primarily affects elderly individuals. It is important to emphasize that the processed data are taken from medical records, unlike other studies in the literature that rely on image acquisition and processing. Although more challenging to handle, this approach has the advantage of including a wide range of parameters in large numbers, which can highlight their potential influence. Artificial neural networks are used to study glaucoma progression, designed through successive trials for near-optimal configurations using the NeuroSolutions and PyTorch frameworks. Furthermore, different problems are formulated to demonstrate the influence of various structural and functional parameters on the study of glaucoma progression. Optimal neural networks were obtained using a program written in Python using the PyTorch deep learning framework. For various tasks, very small errors in training and validation, under 5%, were obtained. It has been demonstrated that very good results can be achieved, making them credible and useful for medical practice.

Similar content being viewed by others

The impact of artificial intelligence in the diagnosis and management of glaucoma

An objective structural and functional reference standard in glaucoma
Deep learning in glaucoma with optical coherence tomography: a review
Introduction.
Artificial intelligence (AI) is currently one of the fastest-evolving fields, notable for its diverse techniques and applications areas. Modern medicine requires the acquisition, analysis, and processing of large amounts of data to address complex clinical tasks. In this context, AI serves as a valuable tool for clinicians, which aids in therapeutic decision-making and provides predictions that extend beyond available data.
Artificial neural networks (ANN) are modelling and classification tools with the ability to learn different types of relationships from available data. They can approximate any continuous nonlinear function, and are effective for modelling complex nonlinear systems. ANNs draw inspiration from biological neurons and the structure of the nervous system. A biological neuron comprises three main components: the cell body, dendrites, and axon, with synapses facilitating connections. These elements have artificial counterparts in the basic units of neural networks. An artificial neuron receives inputs, possibly from other neurons, each associated with a connection weight. It calculates a weighted sum of these inputs and then applies an activation function to compute the output, which can be further transmitted to other neurons.
Glaucoma is a chronic, progressive, irreversible, multifactorial optic neuropathy that mainly affects elderly people, requiring early diagnosis, individualized treatment, and lifelong monitoring.
There are many approaches in the literature that report the study of glaucoma evolution using neural networks, original articles, and numerous reviews. Mainly, there are two categories of approaches based on the data’s origin: from images or medical records , with the former being more numerous given the ease and accuracy of image acquisition. There are specific AI algorithms for segmenting and automatically enhancing ocular images from optical coherence tomography (OCT) and processing fundus images.
On the other hand, using data from medical records is more laborious because it requires comprehensive datasets, but, by processing these data with AI algorithms, more information can be obtained, useful for the ophthalmologist, as the dataset can include numerous analyses, possibly influencing glaucoma.
The most common use of artificial intelligence techniques in ophthalmology has been in the early diagnosis of glaucoma when there are diagnostic doubts. Neural networks, in particular, have played a significant role in determining the need for early antiglaucoma therapy to prevent disease progression.
The first studies on using ANNs in interpreting incipient perimetric lesions in glaucoma belong to Anton et al. 1 . The authors concluded that neural networks can differentiate incipient lesions caused by glaucoma from those caused by other diseases with 97% accuracy.
In 2005, Bowd et al. 2 used two algorithms (RVM—Relevance Vector Machine and SVM—Support Vector Machine) for classifying healthy eyes and eyes affected by glaucoma, using information based on the retinal nerve fiber layer (RNFL) and thickness measurements obtained through scanning laser polarimetry (SLP).
Previously, the same author 3 had used different artificial intelligence tools to determine the evolutionary changes in the visual field in glaucoma patients and predict the glaucoma stage. Similar concerns were held by Simon et al. 4 , Hernández et al. 5 , Grewal et al. 6 , Parsaei et al. 7 , who used various artificial intelligence tools (neural networks with different learning algorithms) to determine possible visual field progression in glaucoma patients.
Zhu et al. 8 developed a neural network using a Bayesian-type function to establish the relationship between structure and visual function in glaucoma; the results showed that the network could improve the prediction of visual function. Based on the analysis of the specialized literature, they showed that diabetes is an individual risk factor for the development of open-angle glaucoma.
An interesting study on the utility of ANNs in ophthalmology is found in a doctoral thesis at UMF Iași 9 . For the first time, artificial neural networks are used to demonstrate the existence of a relationship between glaucoma and diabetes, as well as in predicting the progression of diabetic ocular changes (diabetic retinopathy) in patients with glaucoma and diabetes. The constructed neural models demonstrated the possibility of using them in predicting mean deviation (MD) deterioration, with the best results obtained using Jordan Elman-type neural networks 10 .
In a recent review, Devalla et al. 11 discuss the role of AI in glaucoma diagnosis and prognosis. They show that while early studies relied on simple ANNs to detect glaucoma using perimetric data (visual field), modern deep learning (DL) systems have successfully exploited high-resolution images from fundus photography and OCT. The use of AI algorithms can help, by collecting data from multiple tests, to detect anomalies, and perform relevant screenings. This reduces the workload for clinicians, minimizes diagnostic errors, and improves the quality of care for glaucoma patients. This will lead to early detection of glaucoma and promote research and development of new drugs in treatment. Also, pre-perimetric changes can be identified, likely leading to advances in research and clinical practice.
Bizios et al. 12 conducted a study comparing artificial neural networks and support vector machines for glaucoma diagnosis, measuring the thickness of the retinal nerve fiber layer obtained with OCT. Both algorithms provided satisfactory results.
Yousefi et al. 13 developed a DL-based algorithm that detected visual field (VF) progression earlier than conventional strategies. Although lowering intraocular pressure (IOP) has proven to be therapeutically effective in delaying glaucoma progression, some authors have shown that disease progression is still inevitable, suggesting that optimal treatment regimens for different forms of glaucoma have not yet been achieved.
Guangzhou et al. 14 published a study addressing the task of optic disc classification in glaucoma. A total of 163 eyes from 105 glaucoma patients were utilized, divided into training and testing datasets, to establish classification criteria to aid clinical assistance in glaucoma management. Ocular images were obtained using optical coherence tomography techniques and retinal perfusion was investigated using laser flowgraphy. A total of 91 parameters were extracted from each eye, and general patient information was included. Classification methods tested in the study included neural networks, naive Bayes classifiers, support vector machines, and gradient boosted decision trees. The results of the performance comparison of the three classification methods showed that neural networks achieved the best classification with an accuracy of 87.8% using only nine ocular parameters.
The study of glaucoma progression, through simulation with artificial intelligence tools, consisted of structural , functional , or mixed approaches .
Functionally, several studies have been conducted aiming to compare the performance of various machine learning classifiers with global indices from STATPAC and human experts 15 , 16 , 17 .
Visual fields are used as input data, and the classifiers’ ability to predict the development of abnormal fields in subsequent examinations of hypertensive eyes (OHT) with initially normal visual fields is evaluated, as well as to identify and quantify areas of progression in standard automated perimetry fields 18 .
In addition, some studies compare the performance of machine learning algorithms with traditional algorithms in detecting glaucomatous visual field defects. The studies employ various techniques such as multi-layer perceptrons (MLP), support vector machines (SVM), Gaussian classifiers (MoG), generalized Gaussian classifiers (MGG), variational Bayesian independent component analysis models (vB-ICA-mm), and deep convolutional neural networks (CNN) 19 , 20 . Results indicate that machine learning algorithms can improve STATPAC global indices and identify glaucomatous changes earlier in standard visual fields, sometimes up to 3.92 years earlier than traditional methods.
It is concluded that machine learning algorithms have the potential to reduce testing time by decreasing the number of visual field location measurements. Moreover, the results show that machine learning algorithms have higher diagnostic performance compared to traditional algorithms, and the proposed glaucoma progression index based on CNN and machine learning outperforms global, regional, and point indices in detecting longitudinal visual field progression in glaucoma.
On the other hand, various studies have focused on detecting structural progression in glaucoma by analysing OCT and fundus images with AI and DL algorithms.
The first study mentioned was conducted by Christopher et al. 21 , which used PCA to identify new glaucoma-related structural features based on SS-OCT images. This study obtained significantly higher accuracy for glaucoma detection with an AUC of 0.95.
The second study, conducted by Medeiros et al. 22 , used a deep learning convolutional neural network to predict average RNFL thickness based on fundus photographs, achieving good performance in discriminating glaucomatous eyes from healthy eyes.
Devalla et al. 11 reviewed the role of AI in glaucoma diagnosis and prognosis, discussing the advantages and challenges of using AI systems in clinics and predicting potential areas of progress in the future in this field.
Another study, conducted by Ran et al. 23 , discussed the potential clinical impact of DL models and identified areas for future research.
In 2022, Hood et al. 24 described an automated method for detecting glaucoma without the need for a clinician’s judgment, using a simple anatomical artifact model to help distinguish artifacts from actual glaucomatous changes in OCT probability maps. In the same year, Li et al. 25 developed a deep learning system for the automatic detection of angle closure in AS-OCT images. The results showed that the deep learning system performed better compared to the one based on quantitative features.
Chaurasia et al. 26 conducted, in 2022, a meta-analysis to determine the overall performance of AI in glaucoma diagnosis and identify potential factors affecting their implementation. The results showed that AI algorithms performed well in detecting glaucoma.
The specialized literature contains various hybrid studies (functional and structural approaches) that have used artificial intelligence for diagnosing and managing glaucoma. The studies included various combinations of techniques, such as ANN, optical coherence tomography (OCT), standard automated perimetry (SAP), short-wavelength automated perimetry (SWAP), and confocal scanning laser ophthalmoscopy (CSLO).
As early as 1996, Brigatti et al. 27 used a two-layer back-propagation network to assign each eye an estimated probability of having glaucoma and correctly identified 88% of all eyes with 90% sensitivity and 84% specificity.
Another study conducted by Mardin et al. 28 used six different combinations of morphological data and visual field data to diagnose the disease, applying machine learning classifiers. The combination of Heidelberg Retina Tomograph (HRT), standard Octopus output (HRT/PERI1), and standard deviations (HRT/PERI2) achieved the highest sensitivity (95%) and specificity (91%).
Other studies 16 , 29 , 30 have investigated the use of structural and functional measurements, such as OCT and standard automated perimetry SAP, using machine learning classifiers to identify eyes with glaucoma with high accuracy. These studies have shown that the optimized combination of data can improve diagnostic accuracy. In addition, some studies have investigated the use of an ANN-based approach to differentiate the diagnosis of open-angle glaucoma from glaucoma suspicion without a visual field test 18 and found that this approach can be a cost-effective screening tool. Overall, these studies have shown that AI can be a powerful tool for diagnosing and managing open-angle glaucoma.
Modern AI algorithms are specifically adapted to extract significant features from complex and high-dimensional data for screening, diagnosis, management, and follow-up of glaucoma based on the interpretation of functional and/or structural parameters 12 , 31 .
Numerous other studies in specialized literature demonstrate the successful use of artificial intelligence tools in Ophthalmology, such as evaluating visual fields, optic nerves, retinal nerve fiber layers, thus providing better accuracy in identifying glaucoma progression and retinal changes in diabetes. The main advantages of using these techniques in medical diagnosis are: the ability to process large amounts of data, low probability of overlooking relevant information, and reduced time for diagnosing.
Singh et al. 32 , 33 , 34 , 35 , 36 have important contributions in identification of symptoms for glaucoma and glaucoma affected retinal images, using Machine Learning or Deep Learning Techniques. They show that important steps in applying machine learning techniques for automatic detection of glaucoma are retinal image acquisition, image preprocessing, feature extraction, classification of symptoms of glaucoma affected image, and evaluating the performance 33 . In order to overcome some difficulties related to conventional diagnostic methods utilized by ophthalmologists, Singh et al. 36 propose a computer-assisted diagnosis systems by using machine learning approaches to classify retinal pictures as “healthy” or “infected”. Different AI methodologies are explored for glaucoma detection: Differential Evolution based multi objective feature selection technique 32 , Particle Swarm Optimization 34 , 36 , Artificial Bee Colony, Binary Cuckoo Search, Random Forest, Support Vector Machine, used individually or in ensembles 36 . The efficiency of these methos has been proved by the obtained results—accuracy with value between 0.91 and 0.99.
The objective of the paper involves creating a database with medical records of glaucoma patients and formulating problems to determine relevant input and output parameters related to glaucoma progression. This includes selecting or developing suitable AI methodologies (artificial neural networks) and software, and comparing the effectiveness of different methods. Additionally, the results are compared with existing literature to highlight the benefits of simulations for glaucoma patients and ophthalmologists' decisions.
An important contribution of the research is the use of data from medical records, containing multiple information from investigations and visits, compared to most studies in the literature that address this topic and that use data from acquired images. The use of data from medical files allows the consideration of various information with possible influence in glaucoma. ANNs are developed using the NeuroSolutions and PyTorch frameworks. The best results are obtained in the second case, when the errors in the testing phase are very small, which gives credibility to the models and high chances that they can provide reliable and useful information to the specialist doctor. Therefore, the main original contribution of this work lie in the applied methodology, which includes extensive and diverse data extracted from the medical records of glaucoma patients, the formulation of problems to evaluate glaucoma progression, and the implementation of various neural network models using PyTorch .
The work is organized in the following sections: " Introduction ", experimental part that includes " Datasets " and " Modelling methodology ", " Results ", " Discussion ", " Conclusions " and References.
Most simulation approaches in the literature for studying glaucoma use data acquired from images. These have several advantages related to the fact that they are numerous and accurate since the images are obtained with high-performance devices, and any number of points desired by the user can be read from an image.
Much more difficult and, therefore, less used, is the collection of data from medical records, each entry representing a consultation and results of a whole set of tests. Time and accuracy are the major difficulties in building the dataset. However, once such a task is formulated and addressed, the advantages become evident through the information that can be obtained about the factors influencing the disease, its progression, and even the most suitable treatment.
In this paper, glaucoma, a chronic, progressive, irreversible, and multifactorial optic neuropathy, is analysed using data from medical records.
To create the dataset, medical records of glaucoma patients examined at Countess of Chester Hospital in the UK were used, and the study was retrospective, following patients who had at least three consecutive check-ups between 2018 and 2021 and underwent all necessary investigations to be included in the study. Precise inclusion and exclusion criteria 37 were established, and two distinct datasets were created.
Inclusion criteria for this study were: open-angle glaucoma or intraocular hypertension, with or without associated diabetes. Only patients who had the following investigations recorded at each of the three visits were selected: visual field assessment, macula and optic nerve OCT, intraocular pressure measurement on both eyes, visual acuity measurement, pachymetry, HbA1c measurement, and baseline IOP documented at the time of glaucoma diagnosis.
Criteria for the diagnosis of primary open-angle glaucoma (POAG) considered were: age over 40 years, IOP greater than 21 mm Hg without treatment at the time of diagnosis, open-angle in the anterior chamber upon gonioscopy, typical optic nerve damage in glaucoma (C/D ratio > 0.5), abnormal visual field (by Humphrey Field Analyzerperimetry), and retinal nerve fiber layer thickness impairment measured by Heidelberg OCT. Patients with ocular hypertension (OHT) were also included, with diagnostic criteria such as: age over 40 years, IOP greater than 21 mm Hg without treatment at the time of diagnosis, open-angle in the anterior chamber upon gonioscopy. These patients may have a normal visual field, normal optic nerve appearance (C/D ratio < 0.5), and normal retinal nerve layer thickness measured by OCT.
Our approach, based on modeling with artificial neural networks, starts with the following considerations regarding to normal values and deviations from them, for the quantities considered in the evaluation of glaucoma progression:
Mean Deviation (MD), with normal range greater than − 2 dB, measures the overall depression of the visual field. A value less than − 2 dB suggests abnormality, with more negative values indicating more severe loss.
Pattern Standard Deviation (PSD), with normal range close to 0 dB, indicates the irregularity of the visual field loss. Higher values suggest more localized defects; normal values are usually near 0, with higher values indicating glaucomatous damage.
Visual Field Index (VFI), with normal range of 100%, represents the percentage of normal visual function. Lower percentages indicate more significant visual field loss; normal values are near 100%, with lower values indicating more severe glaucoma.
Retinal Nerve Fiber Layer (RNFL), with normal range of 80–100 µm, is a critical indicator of glaucomatous damage. Values below the normal range suggest thinning due to glaucoma.
Intraocular Pressure (IOP), with normal range of 10–21 mmHg, is a significant risk factor for glaucoma. Values above 21 mmHg may indicate glaucoma or risk of developing it, although some patients with normal IOP can also have glaucoma (normal-tension glaucoma).
The medical investigations represented the 47 attributes, from which the inputs and outputs were selected for the modeling action, corresponding to the formulation of various problems through which the progression of glaucoma could be evaluated. Fifty patients were included in the database, each with three check-ups, resulting in 150 visits with 300 entries (for both eyes). These constitute the records or instances of the database. From this information, two datasets were formed: considering the visits of a patient as distinct records (dataset 1) and attributing these visits to the patient who performed them (dataset 2).
Compared to the modeling on dataset 1, where the values corresponding to each visit were considered as separate records (as if they belonged to different patients), in dataset 2 these values were attributed to the same patient, becoming additional inputs. The database thus configured includes 100 records (instances).
Various tasks were formulated in the sense of choosing different sets of input and output parameters because in this way there is the possibility of obtaining multiple and varied information. From this point of view, factors that may contribute to the progression of glaucoma were selected, such as: patient age, glaucoma age, intraocular pressure, central corneal thickness, phakic or pseudophakic status, as well as factors monitoring the severity of the disease: visual field values (VFI), mean deviation (MD), retinal nerve fiber layer thickness (RNFL). A binary encoding (0 and 1, Yes and No) was used to represent glaucoma progression. Inputs and outputs were different for different datasets, the distinct approaches aiming to obtain additional information about the studied conditions. Thus, modelling the dependence between functional and structural glaucomatous damage and common glaucoma risk factors was carried out in various ways, the results obtained providing information about the severity of the disease and recommended treatment. Alternatives for testing different influencing factors in glaucoma represent a study method of this condition, with possibilities to extract different information.
Modelling methodology
The tools used to monitor the evolution of glaucoma were artificial neural networks, designed using two methods: successive attempts with the NeuroSolutions program and an original implementation in PyTorch using the Python programming language.
Different types of neural models were tested, for which parameters that might influence the modelling results were varied: network topology, learning method, data partitioning into training and validation sets, transfer functions, the number of training epochs. The first model design method was based on trial and error , the error being evaluated at each variant, i.e., combination of parameters.
The first attempt to predict glaucoma progression using neural networks was based on the NeuroSolutions program, a specialized software product developed by Neurodimension . It allows the design, training, and validation of ANN models, as well as making predictions with them. Featuring a graphical user interface, the program can be easily operated by non-specialists who should nevertheless possess basic knowledge ANNs. It should be noted that the essential elements ensuring success in modelling are the quality of the dataset and the formulation of the task. Specifically, the data must be accurate, sufficiently large, and uniformly distributed across the investigated domain. In terms of task formulation, the inputs and outputs must be correctly chosen, considering the interdependencies and functional relationships between parameters.
A second methodology applied in this article is based on original programs written in Python using the PyTorch deep learning framework. PyTorch has implementations of several gradient-descent optimization algorithms, such as Adam (Adaptive Moment Estimation), RMSprop (Root Mean Square Propagation), or SGD (Stochastic Gradient Descent). In our case, the Adam algorithm was used. The parameters of the algorithm, such as the learning rate and regularization factor, should also be set. PyTorch has already implemented several loss such functions, but the choice here depends on the nature of the task. For example, for a classification task, the cross-entropy function can be used, while for a regression task, the mean square error can be used.
The training and prediction sections can be repeated a number of times to statistically estimate the performance of a combination of parameters. Both data partitioning into training and testing sets and optimization algorithm results are stochastic, so a statistical evaluation is beneficial.
In the case of both methods, different problems were formulated, aiming to track glaucoma progression through structural, functional, or combined (hybrid) parameters. By considering different input–output combinations, the attempts were made to highlight factors with significant influence on disease progression, these factors coming from data included in the patient files. In this way, through the predictions of neural models (credible predictions in the case of models with small testing errors), the ophthalmologist can have additional information and suggestions regarding the treatment to be followed.
Institutional review board
The study was approved by the Ethics Commission of the University Hospital Sf. Spiridon Iasi, approval no. 38/24.04.2023 and Countess of Chester Hospital, Liverpool Rd, Chester approved no. 28.04.2023, in compliance with ethical and deontological rules for medical and research practice. The study was conducted in accordance with the Helsinki Declaration.
Informed consent
Informed consent was obtained from all subjects involved in the study.
Neural networks models determined using NeuroSolutions
Different tasks were formulated and solved on the two datasets, denoted 1 and 2, distinguished by differentiating the parameters corresponding to the three visits (dataset 2).
The following case studies were performed using dataset 1, which neglects the third visits.
Case study 1: modelling the dependence between functional and structural glaucomatous damage and common glaucoma risk factors. The factors that can contribute to glaucoma progression (patient age, glaucoma age, IOP, Base IOP, IOL, CCT) were selected as inputs and the variables that monitor the severity of the disease (VFI, PSD, RNFL) were selected as outputs. The lower the VFI, the higher the PSD, and the lower the RNFL values, the more advanced the glaucoma.
The testing plan included various neural network methodology options, evaluated by the mean square error ( MSE ) and the correlation coefficient ( r ). Specifically, we used neural networks with one or two layers and a variable number of intermediate neurons, different percentages for splitting data between training and testing sets (85–15%, 80–20%, 75–25%, 70–30%), training algorithms (backpropagation with momentum and Levenberg–Marquardt), and different numbers of training epochs (500, 2000, 10000, 20000).
An MLP(6:24:8:3) network (multilayer perceptron with 6 inputs and 3 outputs, and 2 hidden layers with 24 and 8 neurons) recorded very small training errors: an MSE ranging from 0.00012 (minimum) to 0.0163 (maximum), and an r ranging from 0.9493 to 0.99958. The average relative errors in training and testing phases for the three outputs were: 0.34% and 5.44% for VFI, 0.18% and 9.85% for PSD, and 1.96% and 14.79% for RNFL.
The results obtained are considered satisfactory in the context of formulating a complex task where the simultaneous prediction of three real-value outputs was sought: VFI, PSD, RNFL. But to increase the degree of confidence, other methods that improved the generalization capacity were further tested.
Case study 2: modelling the dependence between IOP, CCT, and the degree of visual field loss. In this study, a simpler model was sought with a single output, namely VFI. This parameter reflects the integrity of the visual field and extrapolates the degree of visual field loss in glaucoma. Three inputs were considered: baseline IOP, current visit IOP, and corneal thickness (pachymetry), as these three characteristics help to form an idea about the desired pressure control. The working parameters were: 75% of data for training and 25% for testing, the use of the Levenberg–Marquardt algorithm for training, the hyperbolic tangent ( tanh ) as the activation function, and different types of network architectures: multilayer perceptron, generalized feed-forward network, and Jordan-Elman network. The choice of the working characteristics for these models was made after comparing the results (i.e., errors) of successive trials.
The best ANN model was MLP(3:24:8:1) with an average percentage error of 0.20% in the training phase and 3.23% in the testing phase; these results can be appreciated as very good.
Figures 1 and 2 show the training and testing phases, respectively comparisons between VFI obtained from clinical observations and predictions of the best neural model.
VFI—comparisons between clinical observations and predictions of the MLP(3:24:8:1) network in the training phase.
VFI—comparisons between clinical observations and predictions of the MLP(3:24:8:1) network in the testing phase.
In Fig. 1 , corresponding to the training phase, the placement of the points on the line proves that the response of the neural network coincides with the VFI values obtained from clinical observations. Figure 2 reflects the fact that VFI obtained experimentally (from clinical observations, blue rectangles) has values close to those provided by the neural network (red rectangles). This being the testing phase, the good generalization capacity of the neural model is demonstrated, thus the high probability of predicting the evolution of glaucoma.
Case study 3: modelling the dependency between IOP, CCT, and the degree of optic nerve damage. Similar to the previous case study, the same inputs were maintained, namely baseline IOP, current visit IOP, and corneal thickness, and the output considered was the thickness of the retinal nerve fiber layers (RNFL), which reflects the degree of structural damage in glaucoma based on the same three inputs.
The best model, MLP(3:24:8:1), was obtained with MSE = 0.0000845, r = 0.9997, average training error = 0.11%, and average testing error = 5.44%, which also represent satisfactory results.
In this case, where RNFL was considered as the only output, the average testing error was 5.44%, compared to the modelling in case study 1, where RNFL was one of the three outputs, and the testing error was 14.79%. This improvement comes from changing the task formulation of mapping the inputs to outputs, which led to more accurate predictions.
Case study 4, inputs: patient age, patient sex, glaucoma age, diabetes age, HbA1c, B-IOP, IOP, IOL, CCT, output: VFI. The best model was MLP(9:36:9:1), obtained with MSE = 0.000001, r = 0.999984, and E p = 0.05%.
Case study 5, inputs: patient age, patient sex, glaucoma age, diabetes age, HbA1c, B-IOP, IOP, IOL, CCT, output: MD. The best model was MLP(9:36:9:1), obtained with MSE = 0.000004, r = 0.999933, and E p = 0.05%.
Case study 6, inputs: patient age, patient sex, glaucoma age, diabetes age, HbA1c, B-IOP, IOP, IOL, CCT, output: PSD. The best model was MLP(9:36:9:1), obtained with MSE = 0.000004, r = 0.999633, and E p = 2.088632%.
Case study 7, inputs: patient age, patient sex, glaucoma age, diabetes age, HbA1c, B-IOP, IOP, IOL, CCT, output: RNFL. The best model was MLP(9:36:9:1), obtained with MSE = 0, r = 1, and E p = 0.00265%. Figures 3 and 4 show graphical results for this case, specifically the training and testing phases for the best model. A correlation coefficient of 1 demonstrates that the model has well learned the relationships and patterns in the data (Fig. 3 ). In the testing phase, the r coefficient value is also close to 1, which gives credibility to the determined model (Fig. 4 ). The figures include the coefficient of determination R 2 as a performance metric, which is the square of the correlation coefficient r .

Experimental RNFL the predictions provided by an MLP(9:36:9:1) in the training phase.
Experimental RNFL and the predictions provided by an MLP(9:36:9:1) in the testing phase.
For cases studies 4–7, the presented results are very good, and the obtained models are relatively simple.
Dataset 2 includes information related to the progression of glaucoma in 50 patients aged between 50 and 94 years, 52% of whom are male, with a glaucoma history ranging from 0 to 28 years. In this case, the modelling was carried out under the following conditions. The input data considered were: VFI, MD, PSD, and RNFL, measured at each of the three evaluation visits for both eyes, and indexed as 1, 2, and 3. The output variable, glaucoma progression, was encoded as (1, 0) for “yes”(there is progression in glaucoma) and (0, 1) for “no” (there is no progression in glaucoma). Multilayer perceptron neural models were constructed with 12 inputs, 2 outputs, and one or two hidden layers of neurons. The number of neurons used in the hidden layers varied between 6 and 30. The tanh activation function and the backpropagation with momentum algorithm were used.
The best model, MLP(12:24:6:2), had the following performance in the training phase: MSE = 0.000223, r = 0.999782, and E p = 0.192070. For the testing phase, several results are given in Table 1 . The probability of a correct answer for the prediction of glaucoma progression was 93.3%, which is a satisfactory accuracy.
Neural networks models determined using PyTorch
PyTorch is an open-source deep learning framework developed by Facebook’s AI Research lab. It provides a flexible and efficient platform for building and training neural networks. It supports computations on both CPU (central processing unit/computer’s processor) and GPU (graphics processing unit), which enables faster processing of large datasets. It has an intuitive design and a robust library of pre-built functions and models, which make it popular among researchers and practitioners in machine learning. One of its key features is the dynamic computation graph, i.e., a network where nodes represent mathematical operations and edges represent the data flow between these operations. This graph structure is essential for defining and optimizing complex computations in neural network models. Automatic differentiation is another fundamental feature of PyTorch . The “autograd” system automatically tracks all operations on tensors (multi-dimensional arrays) and enable the automatic computation of gradients during gradient-descent optimization such as backpropagation and its more advanced versions. By applying the chain rule to the computational graph, PyTorch efficiently calculates the derivatives needed to update model parameters. This capability simplifies the training process, making it more straightforward to implement and optimize deep learning models.
The first task to be solved uses dataset 2, the dataset where three visits were considered for a patient. In this case, there are 12 inputs: VFI 1 , VFI 2 , VFI 3 , MD 1 , MD 2 , MD 3 , PSD 1 , PSD 2 , PSD 3 , RNFL 1 , RNFL 2 , RNFL 3 , and the output of the model is represented by glaucoma progression, encoded by YES or NO. The configured dataset includes 100 records (instances).
The proposed architectures have two fully-connected layers with different number of neurons in the two hidden layers, using the tanh activation function. Since this a binary classification problem expressed using one-hot encoding, a softmax layer is used before the output. Softmax is a function that converts an array of real-valued numbers into a probability distribution.
The training algorithm is Adam (Adaptive Moment Estimation), a well-known optimization algorithm based on the principles of gradient descent. It computes individual adaptive learning rates for each network parameter using estimates of first and second moments of gradients. The specified learning rate is 0.001, which defines the size of steps taken to update the model parameters during training. A smaller learning rate, such as 0.001, implies smaller steps, often leading to more stable convergence. Weight decay is set to 10 −5 , serving as a regularization term during training. It helps prevent overfitting by adding a penalty to the model weights.
In order to determine the best architecture, fivefold cross-validation (CV) was implemented, meaning that in one iteration 80% of the data is used for training and 20% for testing. This methodology helps assess the generalization capabilities of the neural models. We also included a statistical approach of evaluating the architectures, running the CV process multiple times (in this case, 200 times). This decreases the influence of particular data splits in a single CV operation. The number of training epochs ranged between 50 and 100. It was observed that a larger number of epochs led to overfitting.
The best result was provided by a feedforward network, MLP(12:33:11:2), with two intermediate layers containing 33 and 11 neurons, respectively. The average error for the training phase was 0.09%, and 0.19% for testing, which represents a very good result.
After this process of identifying the best configuration, we used the process of splitting the data into 80% for training and 20% for testing, and selecting the model with the lowest testing error for prediction out of 20 repeated trials.
Another task to be solved with this method was modelling the evolution of glaucoma reflected by the values of the third visit. In this case, glaucoma progression was tracked by predicting the value of a specific parameter at the third visit of the patient included in the dataset. These parameters were, in turn, VFI 3 , MD 3 , PSD 3 , RNFL 3 , and IOP 3 . Considering 16 input sizes, 5 tasks were formulated and solved, corresponding to the mentioned outputs (Fig. 5 ).
Modelling glaucoma progression by predicting the results of the third visit.
The training methodology is similar, but in this case we are dealing with regression problems, therefore the architectures involve a fully-connected layer with 1 output instead of a softmax layer.
Table 2 displays the results of the runs, showing the best determined network along with the corresponding errors observed during the training and testing phases.
Next, some detailed results are presented, either in graphical format or in tables. For example, for MD 3 , Figs. 6 and 7 compare the experimental data (from the dataset) with those provided by the determined neural model, both for the training phase and for the testing phase, in an Microsoft Excel trendline format.
MD 3 experimental and obtained through neural modelling in the training phase.
MD 3 experimental and obtained through neural modelling in the testing phase.
In other words, comparing the experimental data with those provided by the best neural model involves evaluating the distance of the points from the straight line. The closer the points are to the straight line (or even on the line), it means that the values of the two datasets (experimental/investigations and prediction) are closer. The graphs also show the coefficient of determination R 2 whose value is close to 1.
The results presented in Table 2 (row 2) and Figs. 6 and 7 show that MD at the third visit can be approximated with an accuracy of 98.75% based on the values recorded at the previous visits.
For the PSD parameter (task 3 in Table 2 ), Figs. 8 and 9 show comparatively some of the training and testing data, this time through bar graphs.
PSD 3 experimental and obtained through neural modelling in the training phase.
PSD 3 experimental and obtained through neural modelling in the testing phase.
An accuracy of 99.25% for estimating PSD at the third visit represents a reliable prediction for this parameter.
For task 4, with the output being RNFL at the third visit, the comparison of the values from the dataset with those provided by the model (for a sample of data) is presented in table format (Table 3 ), which allows visualization and comparison of values for each pair of data.
As in the previous tasks, the RNFL prediction at the third visit can be made, based on the determined model, with very high accuracy, specifically 98.33%, which means a faithful estimation of the structural progression.
For the last task (noted 5 in Table 2 ), with the IOP output at the third visit, the experimental vs. NN comparisons are given in graphical form in Figs. 10 and 11 .
IOP 3 experimental and obtained through neural modelling in the training phase.
IOP 3 experimental and obtained through neural modelling in the testing phase.
Another proposed task consisted in developing a neural network model to check if, during the three visits, it was necessary to add more drops to control glaucoma or if surgical manoeuvres were needed to control pressure. Thus, 11 inputs were used: base IOP, IOP 1 , IOP 2 , IOP 3 , VFI 1 , VFI 2 , VFI 3 , RNFL 1 , RNFL 2 , RNFL 3 , and CCT, with a single output, TRATMOD (YES or NO): “YES” for the situation where it was necessary to add more drops to control glaucoma or surgical manoeuvres were needed to control pressure, and “NO” for cases that were stable.
The PyTorch program determined an MLP(11:25:2) model with an average training error of 0.40% and an average testing error of 0.70%, making only one wrong classification out of 100; thus, 99 instances were correctly classified.
For the first modelling methodology, namely determining neural networks through trial and error, different tasks were formulated, each type of modelling potentially contributing to obtain different information regarding disease progression and necessary treatment.
In these tasks, various types of neural models were tested, both structurally (one or two intermediate layers with different numbers of neurons) and parametrically (different transfer functions, training algorithms). Also, different variants (percentages) of data splitting into training and testing sets were tried, with performance evaluation in all cases based on errors (percentage, mean squared) or the correlation coefficient. Thus, the best model determination was done through trial and error.
For the tasks of dataset 1, a satisfactory generalization capacity was obtained, especially for the last four case studies containing a single output size, thus a simpler formulation.
Compared to the studies encountered in the literature addressing glaucoma through simulation using artificial intelligence tools, it is noted that these approaches use data extracted from OCT images 13 , 14 , 38 , 39 with relatively few parameters.
Considering the modelling results obtained on dataset 2 (which is, in fact, the complete dataset), namely one wrong answer out of 15 possible (95.33% correct answers), these are close to what other researchers have reported or even better. Shon et al. 40 predicted glaucoma progression based on visual field (VF) test information using neural networks and, although they had a much larger dataset than the one included in this study, they achieved 86.40% accuracy.
Shuldiner et al. 41 tested several artificial intelligence tools: support vector machine, neural networks, random forest, logistic regression, naïve Bayes, and hybrid models for predicting glaucoma progression, obtaining an accuracy of 72%. They included in the input data visual field parameters, MD (mean deviation), and PSD (pattern standard deviation). Logistic regression applied by these researchers to the available data highlighted the fact that the advanced age of patients and the high value of PSD can influence the rapid progression of glaucoma.
In recent studies, Anton et al. 42 , 43 demonstrated, using neural networks, that changes in visual field parameters, MD and PSD, are related to the influence of sleep apnoea syndrome on glaucoma.
Glaucoma causes visual disability, so it is crucial to find ways to predict its progression, enabling timely intervention to reduce its effects. Most existing studies in the literature rely on artificial intelligence tools to predict glaucoma progression based on spatial features embedded in fundus images 2 , 3 , 7 , 25 , 38 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 . All these studies demonstrate the ability of AI techniques to identify glaucoma and its progression from fundus images, suggesting that they can assist Ophthalmologists quickly and accurately. It can also be argued that artificial intelligence strategies can detect glaucoma progression earlier than conventional methods 48 , 51 . Most of these existing studies in the specialized literature, which are using fundus images report an accuracy of over 90% for predicting glaucoma progression. Compared to these, it is worth mentioning that the models developed in this paper use data collected from patients’ medical records.
Regarding the second modelling methodology, it included the implementation of a neural network design method, specifically a PyTorch program, which provides very good functional neural network models, i.e., network parameters. It is essential to note that very small errors were obtained during the testing phase, giving credibility to the models used in predicting glaucoma.
The program is flexible, allowing for the selection of the best values for the parameters; it works with: optimizer type, learning rate, weight decay, number of attempts, number of epochs, and data splitting into training and testing sets.
It was found that a larger network can provide better results; the same configuration, MLP(16:42:14:1), yielded very small errors in training and testing for all parameters for which predictions were made (VFI, MD, PSD, RNFL, IOP). The average testing errors were below 5%. A comparison can be made with previously reported results 37 obtained with the dedicated Weka machine learning software. In both cases, the same dataset (dataset 2) was used, and the same task was solved, answering the question of whether glaucoma had progressed, considering the same 12 inputs. The best result obtained with Weka was a MLP(12:8:1), which provided 92 correct answers out of 100 possible, so a relative error of 8%, compared to the network determined in PyTorch , with 99 correct classifications out of a total of 100 instances.
The PyTorch ANN models provided very good results for predicting the visual field parameters (VFI, MD, and PSD) based on previous visit investigations. In the literature, similar research 16 presents the possibility of making predictions for 24–2 visual field defects up to 5.5 years into the future. It is a complex approach, with a large number of parameters, based on deep learning neural networks that uses points from visual field images. Indeed, relatively small prediction errors are obtained, but, in our approach, the predictions for the visual field parameter values are smaller than those reported by Wen and colleagues 16 . Also, our methodology assumes the use of patient medical record data by a simple method.
When using AI models to analyze eye-related glaucoma illness datasets, several potential disadvantages and repercussions must be considered. The diversity of medical records means that more parameters may need to be considered for studying glaucoma progression than those offered by images alone. This paper uses such a diverse database as a challenge to find solutions that are accurate and methodologically sound. While it can be demonstrated that credible and useful results can be obtained with appropriate tools, several risks remain.
One significant risk is the potential for false diagnoses, including false-negative results, which can lead to missed diagnoses and delayed treatment. Such errors could have serious repercussions, including blindness if the glaucoma progresses untreated. If clinical decisions are based directly on AI system interpretations, the responsibility of the ophthalmologist becomes critical, necessitating the development of medico-legal protocols that involve both the clinician and the AI methods.
Additionally, there are limitations to using AI in clinical practice, such as patient mistrust in remote screening and doctors' dependency on technology. Despite these limitations, AI systems combined with ocular imaging in telemedicine could offer a cost-effective long-term solution to enhance screening efficiency and patient monitoring. This underscores the importance of integrating AI carefully and responsibly into medical practice to maximize benefits and minimize risks.
Conclusions
Glaucoma, a cause of irreversible blindness, represents a public health issue (global prevalence of 3.5%, affecting individuals aged between 40 and 80 years old and an estimation of 112 million cases worldwide by 2040). Early diagnosis and accurate monitoring of glaucoma progression are essential for controlling this disease and providing personalized treatment. In recent years, AI tools have been increasingly used for diagnosis, monitoring, and prognosis of glaucoma.
The initial trial and error method is simple but time-consuming. Moreover, it does not guarantee the determination of the best model. However, good results have been obtained, depending on the task formulated and the parameters considered.
Very good neural networks were obtained using the PyTorch deep learning framework. For various tasks, very small errors in training and testing, under 5%, were obtained. The networks can model both binary outputs, indicating whether glaucoma progresses, and real-valued outputs for variables that provide information on glaucoma progression (VFI, MD, PSD, RNFL, IOL). Predictions made by the PyTorch neural networks achieved over 98% accuracy for both functional (visual field parameters) and structural (retinal nerve fiber layer thickness) progression of glaucoma. This approach proved superior for developing efficient neural models to estimate the course of glaucomatous disease in clinical practice.
As future research directions, we propose testing the already developed software tools on additional datasets, as well as exploring other AI tools that are likely to be effective in simulation studies of glaucoma (for instance neuro-fuzzy technique).
Data availability
The datasets used and analyzed during the current study, as well as the source code of the software, are available from the corresponding author on reasonable request.
Antón, A., Jordano, J. & Maquet, J. D. Sistema experto de diagnóstico de glaucoma. Archivos de la Sociedad Española de Oftalmologia 69 (1), 23–28 (1995).
Google Scholar
Bowd, C. et al. Relevance vector machine and support vector machine classifier analysis of scanning laser polarimetry retinal nerve fiber layer measurements. Invest. Ophthalmol. Vis. Sci. 46 , 1322–1329 (2005).
Article PubMed Google Scholar
Bowd, C. et al. Comparing neural networks and linear discriminant functions for glaucoma detection using confocal scanning laser ophthalmoscopy of the optic disc. Invest. Ophthalmol. Vis. Sci. 43 (11), 3444–3454 (2002).
PubMed Google Scholar
Simon, M., Alonso, L. & Alfonso, A. A hybrid visual field classifier to support early glaucoma diagnosis. Inteligencia Artificial Revista Iberoamericana de Inteligencia Artificial 9 (26), 9–17 (2005).
Hernández, G. E., Santos-García, G. & Inés, F. B. Identification of glaucoma stages with artificial neural networks using retinal nerve fibre layer analysis and visual field parameters. Innov. Hybrid Intell. Syst. 44 , 418–424 (2007).
Grewal, D., Jain, R., Grewal, S. & Rihani, V. Artificial neural network-based glaucoma diagnosis using retinal nerve fiber layer analysis. Eur. J. Ophthalmol. 18 (6), 915–921 (2018).
Article Google Scholar
Parsaei, H., Moradi, P. & Parsaei, R. Development and verification of artificial neural network classifiers for eye diseases diagnosis. in Proceedings of the 14th ICBME . 398–402 (2008).
Zhou, M. et al. Diabetes mellitus as a risk factor for open-angle glaucoma: A systematic review and meta-analysis. PLoS One 9 (8), e102972 (2014).
Article ADS PubMed PubMed Central Google Scholar
Anton Apreutesei, N. The influence of glaucoma on the ocular changes of diabetes. PhD thesis UMF Iași, (2015).
Anton Apreutesei, N. et al. Predictions of ocular changes caused by diabetes in glaucoma patients. Comput. Methods Progr. Biomed. 154 , 183–190 (2018).
Devalla, S. et al. Glaucoma management in the era of artificial intelligence. Br. J. Ophthalmol. 104 (3), 301–311 (2019).
Bizios, D., Heijl, A., Hougaard, J. L. & Bengtsson, B. Machine learning classifiers for glaucoma diagnosis based on classification of retinal nerve fibre layer thickness parameters measured by Stratus OCT. Acta Ophthalmol. 88 (1), 44–52 (2010).
Yousefi, S., Kiwaki, T. & Zheng, Y. Detection of longitudinal visual field progression in glaucoma using machine learning. Am. J. Ophthalmol. 193 , 71–79 (2018).
Guangzhou, A. et al. Comparison of machine-learning classification models for glaucoma management. J. Health Ing. 2018 , 1–8 (2018).
Bizios, D., Heijl, A. & Bengtsson, B. Trained artificial neural network for glaucoma diagnosis using visual field data: A comparison with conventional algorithms. J. Glaucoma 16 , 20–28 (2007).
Wen, J. C. et al. Forecasting future Humphrey visual fields using deep learning. PLoS One 14 , e0214875 (2019).
Article CAS PubMed PubMed Central Google Scholar
Sample, P. A. et al. Using machine learning classifiers to identify glaucomatous change earlier in standard visual fields. Invest. Ophthalmol. Vis. Sci. 43 , 2660–2665 (2002).
Sample, P. A. et al. Unsupervised machine learning with independent component analysis to identify areas of progression in glaucomatous visual fields. Invest. Ophtalmol. Vis. Sci. 46 , 3684–3692 (2005).
Goldbaum, M. et al. Comparing machine learning classifiers for diagnosing glaucoma from standard automated perimetry. Invest. Ophthalmol. Vis. Sci. 43 (1), 162–169 (2002).
Chan, K. et al. Comparison of machine learning and traditional classifiers in glaucoma diagnosis. IEEE Trans. Biomed. Eng. 49 , 963–974 (2002).
Christopher, M. et al. Retinal nerve fiber layer features identified by unsupervised machine learning on optical coherence tomography scans predict glaucoma progression. Invest. Ophthalmol. Vis. Sci. 59 (7), 2748–2756 (2018).
Article PubMed PubMed Central Google Scholar
Medeiros, F., Jammal, A. A. & Thompson, A. C. From machine to machine: An OCT-trained deep learning algorithm for objective quantification of glaucomatous damage in fundus photographs. Ophthalmology 126 (4), 513–521 (2019).
Ran, A. R. et al. Deep learning in glaucoma with optical coherence tomography: A review. Eye 35 (1), 188–201 (2021).
Hood, D. C. et al. Detecting glaucoma with only OCT: Implications for the clinic, research, screening, and AI development. Prog. Retin. Eye Res. 90 (9), 101052 (2022).
Article CAS PubMed Google Scholar
Li, F. et al. A deep-learning system predicts glaucoma incidence and progression using retinal photographs. J. Clin. Invest. 132 (11), e157968 (2022).
Chaurasia, A. K., Greatbatch, C. J. & Hewitt, A. W. Diagnostic accuracy of artificial intelligence in glaucoma screening and clinical practice. Glaucoma 31 (5), 285–299 (2022).
Brigatti, L., Hoffman, D. & Caprioli, J. Neural networks to identify glaucoma with structural and functional measurements. Am. J. Ophthalmol. 121 (5), 511–521 (1996).
Mardin, C. Y., Peters, A., Horn, F., Jünemann, A. G. & Lausen, B. Improving glaucoma diagnosis by the combination of perimetry and HRT measurements. J. Glaucoma 15 (4), 299–305 (2006).
Yousefi, S. et al. Monitoring glaucomatous functional loss using an artificial intelligence-enabled dashboard. Ophthalmology 127 (9), 1170–1178 (2020).
Nair, M., Tagare, S., Venkatesh, R. & Odayappan, A. Artificial intelligence in glaucoma. Indian J. Ophthalmol. 70 (5), 1868–1869 (2022).
Ittoop, S. M., Jaccard, N., Lanouette, G. & Kahook, M. Y. The role of artificial intelligence in the diagnosis and management of glaucoma. J. Glaucoma 31 (3), 137–146 (2022).
Singh, L. K. & Garg, H. Detection of glaucoma in retinal images based on multiobjective approach. Int. J. Appl. Evolut. Comput. 11 (2), 13 (2020).
CAS Google Scholar
Singh, L. K., Garg, H. & Pooja, A. Automated glaucoma type identification using machine learning or deep learning techniques. Adv. Mach. Intell. Interact. Med. Image Anal. 241–263 (2019).
Singh, L. K., Munish, K. & Shankar, T. A novel hybrid robust architecture for automatic screening of glaucoma using fundus photos, built on feature selection and machine learning-nature driven computing. Expert Syst. 39 , e13069 (2022).
Singh, L. K., Munish, K., Shankar, T. & Singh, R. Deep-learning based system for effective and automatic blood vessel segmentation from Retinal fundus images. Multimed. Tools Appl. 83 , 1–45 (2023).
Singh, L. K., Munish, K., Shankar, T. & Singh, R. Nature-inspired computing and machine learning based classification approach for glaucoma in retinal fundus images. Multimed. Tools Appl. 82 , 1–49 (2023).
Article CAS Google Scholar
Târcoveanu, F. E. et al. Classification algorithms used in predicting glaucoma progression. Healthcare 10 , 1831 (2022).
Elze, T. et al. Patterns of functional vision loss in glaucoma determined with archetypal analysis. J. R. Soc. Interface 12 (10), 1098 (2015).
Raja, C. & Gangatharan, N. Appropriate sub-band selection in wavelet packet decomposition for automated glaucoma diagnosis. Int. J. Autom. Comput. https://doi.org/10.1007/s11633-014-0858-6 (2015).
Shon, K., Sung, K. & Shin, J. Can artificial intelligence predict glaucomatous visual field progression? A spatial-ordinal convolutional neural network model. Am. J. Ophthalmol. 233 , 124–134 (2022).
Shuldiner, S. et al. Predicting eyes at risk for rapid glaucoma progression based on an initial visual field test using machine learning. PLoS One 16 (4), e0249856 (2021).
Anton, N. et al. Use of artificial neural networks to predict the progression of glaucoma in patients with sleep apnea. Appl. Sci. 12 (12), 6061 (2022).
Anton, N. et al. Assessing changes in diabetic retinopathy caused by diabetes mellitus and glaucoma using support vector machines in combination with differential evolution algorithm. Appl. Sci. 11 (9), 3944 (2021).
Wang, S. Y., Tseng, B. & Hernandez-Boussard, T. Deep learning approaches for predicting glaucoma progression using electronic health records and natural language processing. Ophthalmol. Sci. 2 (2), 100127 (2020).
Thompson, A., Jammal, A. & Medeiros, F. A review of deep learning for screening, diagnosis, and detection of glaucoma progression. Trans. Vis. Sci. Tech. 9 (2), 42–42 (2020).
Hemelings, R. et al. Accurate prediction of glaucoma from colour fundus images with a convolutional neural network that relies on active and transfer learning. Acta Ophthalmol. 98 (1), e94–e100 (2020).
Mirzania, D., Thompson, A. C. & Muir, K. W. Applications of deep learning in detection of glaucoma: A systematic review. Eur. J. Ophthalmol. 31 (4), 1618–1642 (2020).
Zafar, A. et al. A Comprehensive convolutional neural network survey to detect glaucoma disease. Mob. Inf. Syst. Hindawi 2022 , 3971516 (2022).
Mursch-Edlmayr, A. S. et al. Artificial intelligence algorithms to diagnose glaucoma and detect glaucoma progression: Translation to clinical practice. Trans. Vis. Sci. Tech. 9 (2), 55 (2020).
Belgacem, R., Malek, I. T., Trabelsi, H. & Jabri, I. A supervised machine learning algorithm SKVMs used for both classification and screening of glaucoma disease. N. Front. Ophthalmol. 4 (4), 1–27 (2018).
Li, Z. et al. Efficacy of a deep learning system for detecting glaucomatous optic neuropathy based on color fundus photographs. Ophthalmology 125 (8), 1199–1206 (2018).
Download references
Acknowledgements
This work was supported by Exploratory Research Project PN-III-P4-ID-PCE-2020-0551, no. 91/2021, financed by UEFISCDI Romania. Funding: Research Project PN-III-P4-ID-PCE-2020-0551, no. 91/2021.
Research Project PN-III-P4-ID-PCE-2020-0551, no. 91/2021.
Author information
Authors and affiliations.
Ophthalmology Department, Faculty of Medicine, University of Medicine and Pharmacy “Gr. T. Popa” Iasi, University Street No 16, 700115, Iasi, Romania
Filip Târcoveanu & Nicoleta Anton
Faculty of Automatic Control and Computer Engineering, “Gheorghe Asachi” Technical University of Iasi, 27 Mangeron Street, 700050, Iasi, Romania
Florin Leon
Department of Chemical Engineering, Faculty of Chemical Engineering and Environmental Protection “Cristofor Simionescu”, “Gheorghe Asachi” Technical University of Iasi, 73 Mangeron Street, 700050, Iasi, Romania
Cătălin Lisa & Silvia Curteanu
Faculty of Economic Science, “Vasile Alecsandri” University of Bacau, Calea Marasesti 156, 600115, Bacau, Romania
Andreea Feraru
Countess of Chester Hospital, Liverpool Rd, Chester, CH21UL, UK
You can also search for this author in PubMed Google Scholar
Contributions
Conceptualization, N.A., F.T. and S.C.; methodology, N.A., F.T., S.C, F.L; software, formal analysis C.L, A.F; resources, data curation, validation F.T, N.A, F.L, S.C, K.A; investigation, F.T, K.A, N.A and F.L, visualization, supervision N.A, S.C; writing—original draft, writing—review and editing, N.A., S.C; project administration, funding acquisition S.C, F.L.
Corresponding authors
Correspondence to Silvia Curteanu or Nicoleta Anton .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/ .
Reprints and permissions
About this article
Cite this article.
Târcoveanu, F., Leon, F., Lisa, C. et al. The use of artificial neural networks in studying the progression of glaucoma. Sci Rep 14 , 19597 (2024). https://doi.org/10.1038/s41598-024-70748-1
Download citation
Received : 10 May 2024
Accepted : 20 August 2024
Published : 23 August 2024
DOI : https://doi.org/10.1038/s41598-024-70748-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Artificial neural networks
- Simulation studies
- Modelling and optimization
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing: AI and Robotics newsletter — what matters in AI and robotics research, free to your inbox weekly.
Warning: The NCBI web site requires JavaScript to function. more...
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.

StatPearls [Internet].
Root cause analysis and medical error prevention.
Gunjan Singh ; Raj H. Patel ; Sarosh Vaqar ; Joshua Boster .
Affiliations
Last Update: February 12, 2024 .
- Continuing Education Activity
The term "medical error" encompasses diverse events that vary in magnitude and can potentially harm the patient. According to the 2019 World Health Organization (WHO) Patient Safety Factsheet, adverse events due to unsafe patient care are among the top 10 causes of death and disability worldwide. However, understanding that healthcare delivery involves multiple variables in a dynamic environment with many critical decisions made quickly is essential to finding the underlying causes of adverse events. Reducing medical errors requires a multifaceted approach at various levels of healthcare. In the event of a sentinel occurrence or adverse patient outcomes, a thorough evaluation is warranted to prevent such events. Root cause analysis provides a method of assessment for these situations so that a system-based intervention can be implemented rather than blaming individual clinicians. Upon completing this activity, healthcare professionals will gain a comprehensive understanding that root cause analysis (RCA) is a mandated process for healthcare institutions to mitigate future errors and promote patient safety. By acquiring proficiency in RCA application and methodology, healthcare professionals can effectively drive changes and improvements within the healthcare setting, resulting in enhanced patient care and a reduction in medical errors. The course also highlights the interprofessional team's role in performing this analysis to prevent medical errors and improve clinical outcomes.
- Implement effective root cause analysis of a sentinel event and strategies for prevention.
- Apply root cause analysis reporting standards in accordance with the Joint Commission requirements.
- Identify the indications for reporting sentinel events to the Joint Commission and the steps that should be taken following the occurrence of such incidents.
- Collaborate within an interprofessional team to prevent the most common types of clinical errors and improve clinical outcomes.
- Introduction
Medical error is an unfortunate reality of the healthcare industry and a continuously discussed topic due to its grave impact on patient care and outcomes. In a 1999 publication by the Institute of Medicine (IOM), it was highlighted that deaths resulting from medical error exceeded those attributed to motor vehicle accidents, breast cancer, or AIDS. [1] One study reported that approximately 400,000 hospitalized patients experience some preventable harm each year, while another estimated that >200,000 patient deaths annually were due to preventable medical errors. [2] [3] [4] Moreover, the reported cost of medical errors is wide-ranging, with some experts estimating healthcare costs of $20 billion each year, while others approximate costs of $35.7 to $45 billion annually from hospital-acquired infections alone. [2] [3] Subsequent reports that discuss potential etiologies of medical errors have blamed systemic issues. Others have focused attention on certain groups of patients that may be more vulnerable to medical error than others. [5] [6] Recently, the impact of medical errors on a patient's family members and healthcare professionals has been emphasized due to its effects on exacerbating burnout, poor work performance, mental health decline, and even suicidal ideation. [7] [8]
Though pinpointing the definitive cause of medical error in certain situations may be challenging, evaluating strategies that can be used to mitigate and prevent these adverse events from occurring in the first place is essential. One such method is root cause analysis, which has been shown to reduce clinical and surgical errors in various specialties by establishing a quality improvement framework. [9] This article will discuss the application of root cause analysis in medical error prevention and strategies for maintaining continuous quality improvement in the healthcare setting.
Sentinel Events and Root Cause Analysis
The Institute of Medicine defines a medical error as "the failure of a planned action to be completed as intended or the use of a wrong plan to achieve an aim." [1] Recognizing the differences between medical malpractice and medical error is essential. An adverse event in a healthcare setting may be attributed to medical error and not meet the threshold of malpractice or negligence. Medical errors generally result from the improper execution of a plan or improper procedural planning. Thus, the complexity of the occurrence of a medical error can range widely and manifest in any aspect of patient care, from hospital admission to discharge, as well as the outpatient setting. Medical errors may occur without directly harming the patient; however, even in these instances, evaluating the cause of any medical error, whether or not the patient is harmed, and developing guidelines and strategies to prevent future occurrences is critical. [10] [11]
The Joint Commission defines a sentinel event as any unexpected adverse event "involving death, serious physical or psychological injury, or the risk thereof. The phrase 'or the risk thereof' includes any process variation for which a recurrence would carry a significant chance of a serious adverse outcome." Sentinel events indicate the need for an immediate investigation to discover the cause and develop corrective measures. Moreover, the Joint Commission reviews all sentinel events that have resulted in unexpected mortality, significant permanent harm, or severe, temporary harm requiring intervention to sustain life, which they require all member healthcare agencies to report. [12] [13] These events are not only debilitating to patients but can also impact the livelihood of healthcare providers. Sentinel events are unrelated to the patient's underlying medical condition but are attributable to improper medical intervention or improper technique. For instance, if a patient receives medication and experiences an anaphylactic reaction, clinicians must determine whether the reaction was due to the medication or failure to review the patient's allergies before administration. Thus, these cases must be critically reviewed to delineate whether or not the etiology of the error was preventable, which is often a challenging task.
Root cause analysis (RCA) is a process for identifying the causal factors of a medical error that may result in a sentinel event. A standardized RCA process is mandated by the Joint Commission to determine the cause of medical errors and thus allow healthcare institutions to develop strategies to mitigate future errors. [13] Despite broad adoption in the business, engineering, and industrial sectors, RCA use in the medical field has been limited. The RCA process aims not to assign individual blame but to identify lapses in system-level processes that can be restructured to prevent patient harm and reduce the likelihood of future sentinel events. Thus, identifying the root cause of a medical error can better direct the need for additional training and resources.
Applying Root Cause Analysis
For accreditation purposes, the Joint Commission requires that healthcare institutions have a comprehensive process for systematically analyzing sentinel events. The RCA process is one of the most commonly utilized tools for this purpose. Through the RCA process, healthcare institutions attempt to identify all the contributing factors that led to an adverse event. Essentially, RCA investigations continually question why a medical error occurred until all underlying deficiencies in a system are found. RCA emphasizes lapses in system-level processes rather than individual actions. Following a sentinel event, a designated RCA team must be assembled to review and identify necessary changes at the systematic level that can improve performance and reduce the likelihood of a repeat sentinel event. [14] Failure to perform an RCA within 45 days of a sentinel event may result in the healthcare institution being placed on an accreditation watch, which is public information. Repeat violations may result in an onsite review by the Joint Commission that may jeopardize accreditation. [15]
An RCA's initial step is forming an interprofessional team to investigate and define the problem. Typically, a designated process is implemented to communicate with senior leadership throughout the investigation, establish internal target dates, and meet Joint Commission deadlines. After identifying the problem, the team should evaluate systematic factors contributing to the error. Throughout the process, collecting data regarding the potential underlying causes is essential. The team should propose and implement immediate changes so that a repeat sentinel event does not occur during the RCA process. While developing these interventions, the team should evaluate the list of root causes, consider their interrelationships, and explore risk-reduction and process improvement strategies to prevent future errors at the systematic level. Furthermore, the team should discuss the proposed process modification with senior leadership and key stakeholders and determine if they are acceptable. There are various models used to guide RCA inquiries. One model is referred to as "The Swiss Cheese Model." According to this framework, errors occur due to failures on 4 primary levels, classified as unsafe acts, preconditions for unsafe acts, supervisory factors, and organizational influences that can allow patient injury when lined up. Therefore, RCA teams work to identify breakdowns on each of these levels that led to an adverse event. [16]
The Joint Commission has also created a framework with a series of 24 questions to organize an RCA and as a general template to prepare the report submitted to the Joint Commission. The 24-question guide considers various situational factors that may have contributed to a sentinel event. This includes examining the systematic process, human factors, equipment malfunctions, environmental factors, uncontrollable external factors, organizational factors, staffing and qualifications, contingency plans, performance expectations, communication issues, and technology. [13] With detailed consideration of each of these topics, an in-depth analysis of the cause of the sentinel event can occur. Communication is one factor examined in several of the 24 questions, including communication within organizational structure, conveying messages effectively and efficiently, and ensuring a proper communication system. Environmental factors should also be examined to determine if any situational issues were ongoing during the sentinel event that may have impacted the outcome. Moreover, staffing is another issue that should be examined during an RCA review to determine if the staff were appropriately qualified, competent, and portioned for their assigned duties. [17]
After discussion, evaluation, and analysis, corrective actions should be developed, identifying areas for targeted improvement. While utilizing the 24-question framework, causative etiologies should be considered to help determine areas that can be restructured to reduce risk. The root cause analysis should be clear and precise while providing appropriate depth and scope. The Joint Commission has identified a series of adverse events subject to their purview. Primarily, this would be a sentinel event that has resulted in death or permanent loss of function unrelated to any underlying medical conditions, including: [17]
- Patient suicide involving any patient who received care from a healthcare system, including the emergency department, within 72 hours following their discharge
- The unanticipated health issue of a full-term infant
- An infant discharged to the wrong family
- Abduction of any patient receiving care, treatment, or services
- Elopement of a patient within a healthcare setting, leading to harm
- Hemolytic transfusion reaction requiring administration of blood products
- Rape, assault, or homicide of anyone on healthcare premises
- Wrong patient, site, or procedure for any surgical procedures
- Unintended retention of a foreign body in a patient following surgery
- Severe neonatal hyperbilirubinemia
- Prolonged fluoroscopy with cumulative dose to the wrong body region
- Fire, flame, or unanticipated smoke, heat, or flashes during patient care
- Intrapartum maternal death
- Severe maternal morbidity
The finalized RCA report must follow a set standard to meet the Joint Commission's requirements, including:
- Participation of the organization's leadership and key stakeholders
- Thorough explanation of all findings
- Consideration of any relevant or applicable studies
- Internal accuracy and consistency, without contradictions or unanswered questions
Case Illustrations with Root Cause Analysis Interventions
The following cases illustrate various types of medical errors, the process of root cause analysis through which failures were identified, and how interventions were implemented in each situation to prevent similar errors in the future.
Case example 1
A 42-year-old primigravida woman at 34 weeks gestation was brought to the obstetric emergency department at midnight with complaints of severe headache, blurry vision, and right upper quadrant pain for the last 5 to 6 hours. She noted lower extremity edema and facial swelling that was gradually increasing. She has gestational hypertension and, 1 week ago, was prescribed labetalol 200 mg twice a day. On initial presentation, her blood pressure was 190/110 mm Hg on 2 separate occasions, 5 minutes apart. She had gained 2 kilograms since her last antenatal checkup in the clinic a week ago. The patient was diagnosed with severe preeclampsia. The senior obstetric resident ordered a loading dose of magnesium sulfate to prevent imminent seizure. The hospital protocol used an intravenous (IV) and intramuscular (IM) regimen where the patient received a 4 g IV bolus and a 10 g IM dose administered as 5 g in each buttock. The senior resident gave verbal orders for magnesium sulfate administration to the junior resident, who verbally communicated the order to the nurse.
The magnesium sulfate dosing regimen was complex, with multiple doses in different locations, and was incorrectly prepared by the nurse who felt rushed in an urgent situation. Because the chart displaying magnesium sulfate's preparation in the drug preparation room had faded, the nurse relied on her memory. As part of the protocol, the nurse recited the dosage to another nurse, who cross-checked it from a printed chart and noted the error in time. The senior resident also identified the error as the dose was communicated aloud, and the drug administration was stopped.
- Root cause analysis with corrective measures : A root cause analysis was performed, and measures were taken to avoid this problem. As the Institute of Safe Medication Practices recommended, magnesium sulfate was marked as a high-alert medication. Furthermore, premixed solutions prepared by the pharmacy for the bolus dosing were instituted instead of requiring nurses to mix this high-risk medication on the unit. The second nurse verification measure was retained, with the second nurse instructed to double-check all doses, pump settings, drug names, and concentrations before administration of any drugs. Moreover, the RCA recommended that all medication orders be provided in writing and entered in the electronic medical record using computerized provider order entry (CPOE) systems, regardless of the situation's urgency, to avoid dosing errors. The RCA team emphasized that verbal communication for medication administration should always be avoided. If verbal communication is necessary or unavoidable, the RCA recommended that the nurse taking the order read back the order given to the prescribing physician to minimize any prescribing errors.
Case example 2 (The name and date of birth used in this example are for illustrative purposes and do not represent an actual patient. Any similarities if noted, are purely coincidental.)
Anna Joy, date of birth October 30, 1991, was a primigravida at 30 weeks gestation admitted to a busy obstetric ward with complaints of intermittent cramping abdominal pain. She had come from Spain to visit her sister, who was living in Boston. The patient's ability to communicate in English was limited, preferring to speak Spanish. However, her husband and sister were fluent in English and assisted with translation throughout the history, exam, and admission. The patient was seen by an obstetrician who advised routine threatened preterm labor evaluation and observation.
Another patient, Ann Jay, date of birth September 30, 1991, was 34 weeks gestation and admitted to the same ward for gestational diabetes mellitus with hyperglycemia. A consulting endocrinologist advised glucose monitoring and insulin administration. The nurse taking care of the patient was given orders, performed a finger-stick blood glucose check, and informed the endocrinologist about the results over the phone. The endocrinologist advised 6 units of regular insulin before lunch. After being told by the nurse that the patient was feeling decreased fetal movement, the admitting obstetrician recommended ongoing observation and fetal kick counts.
The family members of the first patient, Anna Joy, informed the nurse that they were going to lunch. The morning shift nurse later required a half-day leave because of personal issues and quickly handed her patients to another nurse. The ward was busy and running at full capacity. The new nurse decided to give the insulin injection first as the patient was about to receive her lunch. She did not know that Anna Joy preferred communication in Spanish. The nurse asked a few questions and rushed through patient identification with the help of 2 unique patient identifiers. She administered the insulin injection to the first patient, only realizing later that the insulin was supposed to be given to the second patient, Ann Jay. The attending obstetrician and the endocrinologist were informed. They took the necessary measures and closely monitored the patient for the next few hours; however, no adverse effects were noted.
- Root cause analysis with corrective measures : A root cause analysis was performed, and measures were taken to avoid this problem. The RCA team noted that the nurse caring for both patients had worked in the hospital for 5 years and was recently transitioned to the obstetric ward. This had never happened to her before. The team recognized that the modern patient care delivery process relies on an interprofessional care team's efficient and effective integration. A clear, consistent, and standardized communication method between the team members contributes to safe patient care and minimizes the risk of adverse outcomes. The RCA team did not lay blame on the nurse involved. They instead instituted a standardized handoff platform and required all patient handoffs to occur using this format in the future. During shift change, the handoff between clinicians and nurses is pivotal in providing high-quality care. The aim should be to provide the oncoming team with up-to-date, accurate, and complete information. The RCA team outlined clinical education programs for nurses and clinicians to ensure high-quality and effective handoff occurs at every shift change and patient handoff. They also instituted mandatory use of hospital-based interpreters when communicating with patients who are not fluent in English. The hospital procedure for verifying patient identification using two unique patient identifiers, the name and the date of birth, was retained. However, an additional mandatory step of verifying the patient's identity using an arm-band barcode was instituted before every medication administration. They also highlighted patient charts and rooms when patients had similar names and dates of birth.
Case example 3
A 26-year-old primigravida at 39 weeks gestation with no associated high-risk factors was admitted to a busy labor and delivery floor with labor pains. The patient was managed according to routine labor protocol. When the patient had reached a cervical dilatation of 4 cm, the cardiotocograph showed prolonged fetal bradycardia lasting for 3.5 minutes, which did not resolve with conservative interventions. The patient was transferred to the operating room for an emergent cesarean section. The baby was delivered in good condition, with no intraoperative complications. Before closure, the operating obstetrician asked the scrub nurse to perform a surgical count. The scrub nurse reported a missing gauze piece from the surgical trolley. Therefore, the scrub and the floor nurses performed additional counts several times. A second on-call obstetrician was summoned to assist the primary surgeon in checking the surgical field for the missing gauze piece. The surgical gauze had a heat-bonded barium sulfate marker embedded in the fabric to help with x-ray identification. An intraoperative x-ray was obtained to evaluate for a retained sponge, and the results were negative. After discussing the case with the department chief, the abdomen was closed. Due to the associated delays, the operative time was significantly lengthened, totaling 2 hours and 30 minutes.
- Root cause analysis with corrective measures : An RCA of the event revealed inconsistent practices regarding the surgical count before initiating the procedure. Moreover, only the scrub nurse was responsible for performing this count. The RCA team determined that the surgical count is critical and must be performed in a standardized fashion to eliminate variation and minimize human error. They highlighted international standards that recommend standardizing the counting process and systematically tracking the instruments, gauze, and sponges in the sterile field. Subsequently, they instituted the World Health Organization's Surgical Safety Checklist as a mandatory step for all procedures, regardless of the urgency of the procedure. The team also recommended that the counting process be concurrently audible and visual, performed by the scrub nurse and the circulating nurse independently, and done before and after every procedure. They emphasized that the best practices for surgical count be followed regardless of the clinical situation.
Case example 4
A 25-year-old man presented for bilateral LASIK surgery at a same-day surgery center. The operating surgeon, a community-based surgeon not routinely operating at this facility, examined the patient, and informed consent was obtained preoperatively. The refractive error was -4 D for the right eye and – 5 D for the left eye. The plan was to remove the refractive error altogether. There was a timeout to ensure the correct patient and procedure. The LASIK procedure commenced by creating corneal flaps on both eyes, which was completed uneventfully. Then, the patient was adjusted on the operating microscope so that the first eye was directly under the excimer laser, and iris recognition was attempted before the laser-guided corneal power correction was performed. Though the machine did not recognize the iris pattern after 3 attempts, the surgeon decided to proceed. The technician thought this was rare as they had good iris recognition rates of >98% this month. However, he did not want to contradict the surgeon. Before the procedure, the circulating nurse noted that the patient's table was adjusted to the wrong side with the left eye under the laser instead of the right. She pressed the emergency stop button, and the treatment was terminated. After identifying the mistake, the surgeon and technician restarted the machine to treat the correct eyes in the correct sequence.
- Root cause analysis with corrective measures : Unlike unilateral procedures, bilateral procedures are especially challenging, particularly if the treatment varies between the 2 sides. An example is LASIK, where both eyes are typically corrected simultaneously, and there is no obvious pathology on the eye except for the refractive error. The correction is determined preoperatively, and the result is not immediately titrated. Therefore, the risk for wrong-site procedures is significant, given these ambiguities. To avoid these adverse events, the RCA team implemented a verification procedure where the optometrist, technician, and surgeon must verify each eye's refractive error before the procedure and after programming the laser. Some advanced laser machines have a built-in layer of defense where the iris pattern of the eye is uniquely identified via iris recognition, helping to determine the correct eye and enhance treatment protocol. Some treatments, however, do not include iris recognition, and therefore, the onus lies on the technicians, nurses, and surgeons to identify the appropriate eye correctly.
Case example 5
A community clinic treats approximately 110 patients daily. The clinic is run by 2 primary care physicians, with the assistance of 2 nurses and scribes. A 10-year-old boy was brought to the clinic by his parents due to a runny nose for the last 10 days. On examination, the primary care physician diagnosed allergic rhinitis and advised them to use over-the-counter cetirizine. One of the scribes had called in sick that day, so a secretary was assisting the physician. The physician advised the parents that cetirizine is an over-the-counter medication that could be obtained at their pharmacy of choice. After 2 days, the patient's mother returned to the clinic and reported that the child was lethargic. The clinic front desk staff told the mother they would convey this to the physician, who was very busy that day. The physician instructed the staff to inform the parents that somnolence was typical for children taking cetirizine and to keep the child at home for the next few days. The message was conveyed to the mother, who decided to take the child to another specialist as she was concerned by the sedation. The specialist noted that the child was taking a 10-mg cetirizine tablet twice a day, which is double the recommended amount.
- Root cause analysis with corrective measures : An RCA review at the primary clinic identified a typographical error in the patient instruction handout. Instead of 5 mg twice daily, the instructions had a dosage of 10 mg twice daily. Subsequently, the RCA recommended a verbal and written verification procedure be instituted with the prescribing physicians of all drugs and dosages transcribed by the scribes or office personnel. Moreover, the physician and staff were to read prescription and over-the-counter drug recommendations and doses to the patient or caregiver from the visit summary instructions to verify a match with the clinician's notes. The RCA also mandated a document review for all patient callbacks or return visits before communicating with a patient to avoid future errors.
Case example 6
All-Eyes Laser Center is a busy same-day ophthalmic laser center that performs multiple laser procedures daily but specializes in retinal and anterior segment lasers. A 60-year-old man, JM, suffered from chronic angle-closure glaucoma and had been advised to undergo a Yttrium-Aluminum-Garnett (YAG) laser iridotomy, which involves creating a small hole in the peripheral part of the iris to increase the aqueous flow between the anterior and the posterior chamber. This treatment is frequently performed to prevent an angle-closure attack and further glaucoma progression. This laser surgeon also does another laser procedure called a YAG capsulotomy in which the posterior capsule in a pseudophakic eye is lasered to create an opening to improve vision impaired by after-cataract posterior capsular opacity. The YAG laser device platform allows both procedures to be performed with one machine.
The day JM was scheduled for the YAG procedure was unusually busy at the laser center, and the surgeon was running behind schedule. There were 5 patients ahead of JM, and an approximately 2-hour delay was anticipated. With each patient, the typical practice before a YAG iridotomy procedure consisted of the nurse practitioner checking the patient history, confirming examination findings, and instilling 2% pilocarpine eye drops to cause constriction and ensure good exposure of the peripheral iris crypts. The laser surgeon would then perform the procedure, directing the laser to create a small iridotomy.
After JM was taken to the procedure room, a proper timeout was confirmed, including the correct eye and procedure. However, when the patient was positioned at the laser machine, the surgeon noticed that the pupil was dilated rather than constricted. The surgeon again verified the patient's tag and name and the correct procedure. Though the patient and the procedure were both determined to be correct, the surgeon believed attempting an iridotomy on a dilated pupil would be dangerous. Therefore, the procedure was not performed, and the patient was transferred out of the laser suite. The patient was informed of the error and instructed that he would be rescheduled for the correct procedure in a few days. The error was attributed to the nurse administering the wrong eye drop, secondary to high patient volume and practice inconsistencies.
- Root cause analysis with corrective measures : An RCA was performed, and measures were taken to avoid this problem in the future. Though this error did not harm the patient, the risk of the wrong procedure being performed was high. Therefore, the RCA team recommended segregating patients for YAG capsulotomy and YAG iridotomy to different seating areas that were clearly labeled. The 2 eye drops, tropicamide and pilocarpine, were kept in their respective areas, and the staff was not allowed to take them out from their designated area. A barcode-based verification was also instituted and used each time the drop was instilled. Many clinics utilize precautions for similar-sounding medications and patient names. However, in a clinic where multiple procedures with a relatively quick turnover are being performed, pre-procedure medications without designated patient areas have a significant risk of being mixed. Using the precautions such as those mentioned above can help reduce medication errors.
- Issues of Concern
The IOM identifies medical errors as a leading cause of death and injury. [1] According to the 2019 World Health Organization (WHO) Patient Safety Factsheet, adverse events due to unsafe patient care are among the top ten causes of death and disability worldwide. Preventable adverse events in the US cause an estimated 44,000 to 98,000 hospital deaths annually, which exceeds motor vehicle collision deaths. [1] Furthermore, in terms of health care, disability, and loss of productivity, medical errors are estimated to cost the community an additional 37.6 to 50 billion dollars. [1] The most severe consequences of medical errors are the adverse events patients and their families suffer. Therefore, utilizing RCA is critical to identify systemic flaws that led to a medical error so that corrective measures can be promptly implemented.
Types of Medical Errors
Healthcare professionals should be familiar with the different types of medical errors to understand better the adverse events that may be caused. Errors are not always due to human miscalculation or miscommunication, as outlined by the cases above. Some errors are inherent to clinical situations, such as patient falls in hospital settings and healthcare-associated infections. Common types of medical errors include surgical errors, diagnostic errors, medication errors, equipment failures, patient falls, hospital-acquired infections, and communication failures. [3] [18]
- Surgical errors : Errors in surgery have the highest risk of severe patient injury and death. Intraoperative errors are estimated to be the primary issue in 75% of malpractice cases involving surgeons. Surgical errors involving the wrong site, patient, or procedure should never occur. Investigations into the factors that led to these types of surgical errors have demonstrated that common causes include clinician factors (eg, feeling rushed, distractions, and fatigue), miscommunication, changing or inadequate staffing, organizational factors (eg, discarding specimens as waste and not labeling specimens), medical record issues, and cognitive errors. [19]
- Diagnostic errors : The National Academy of Medicine defines a diagnostic error as "the failure to establish an accurate and timely explanation of a patient's health problems or to communicate that explanation to the patient," therefore, delayed or missed diagnoses are considered errors as well. [20] According to the Joint Commission, diagnostic errors result in the death or injury of 40,000 to 80,000 patients annually. Diagnostic errors are most common in primary care solo practices due to workload, time constraints, and the inability to confer easily with colleagues. [21] Malignancies, surgical complications, and neurological, cardiac, and urological issues are the 5 conditions most frequently misdiagnosed. [22] [23] [24] According to studies, these conditions are frequently misdiagnosed secondary to knowledge gaps, resulting in deficient bedside assessment and clinical reasoning. Identifying these commonly misdiagnosed conditions is beneficial, as diagnostic errors are primarily cognitive rather than organization-based errors; therefore, clinicians can be forewarned of the potential challenges when caring for these patients. [25] In addition to a clinical knowledge deficiency, common contributing factors to diagnostic error include a clinician's fatigue, distraction, failure to consider differential diagnoses, neglect of diagnostic testing follow-up, and inadequate patient follow-up care. [11] [21]
- Medication errors : These errors are widely accepted as the most common and preventable cause of patient injury. [26] Because there are several components involved with patient medications (eg, prescribing, dispensing, dosing, and administering), errors can occur in any of those areas. The reported incidence of medication error-associated adverse events in acute hospitals is approximately 6.5 events per 100 admissions. [26] Medication errors before or after discharge from an acute care facility are the most easily overlooked or missed errors. [26]
- Equipment errors : Medical equipment design flaws, mishandling, user error, and malfunction are common causes of medical errors. Additionally, a significant number of medical devices have been implanted in patients (eg, pacemakers, defibrillators, and nerve and brain stimulators), which may malfunction and result in life-threatening complications. Equipment errors can be due to device differences between manufacturers, inadequate testing and maintenance, poor design, and poor maintenance. Errors involving tube and catheter connections (eg, using catheters for unintended purposes, running the wrong line through a pump, and misplacing feeding tubes into the lung) are also common. These adverse events can have life-threatening effects if a misconnection is not corrected early. [27] [28] To complicate the situation further, medications and food supplements are often delivered via these routes, and placement errors can result in administration or omission mistakes.
- Hospital-acquired infections : Healthcare-related infections are considered a failure of the system. As many as 1 in 20 hospitalized patients may acquire a healthcare-related infection, increasing complications and the length and cost of the hospital stay. Healthcare-related infections add close to $35 billion to the annual cost of healthcare in the United States. [29] Common causes of hospital-acquired infections include failure to practice basic hand hygiene and poor technique in placing indwelling urinary and vascular catheters. Subsequently, the most prevalent infections are catheter-associated urinary tract infections, surgical site infections, hospital-acquired pneumonia, central line-associated sepsis, and care-related skin and soft tissue infections. [29]
- Patient falls : Each year, over one-third of people older than 65 suffer a fall, with one-third of these causing injury. [30] In a healthcare setting, several factors may further increase the risk of falls, including blood loss medication side effects, post-anesthesia effects, decreased blood sugar, altered mental status, advanced age, mobility impairment, and inadequate staffing. [31]
- Communication errors : Optimal interprofessional communication, as well as with patients, is essential for patient care. Therefore, communication errors commonly result in adverse events. [32] Reasons for impaired communication include disruptive patient behavior, environmental distractions (eg, cell phones and pagers), cultural differences, hierarchy issues, personality differences, language barriers, and socioeconomic variables, such as education and literacy. [11] Additionally, errors in written communication, such as using nonstandard abbreviations, illegible handwriting, failure to question inappropriately written orders, and failure to complete correct specimen labeling, frequently occur. [11]
- Clinical Significance
RCA helps healthcare organizations study events that resulted in patient harm or undesired clinical outcomes and identify strategies to reduce further medical errors and improve patient safety. Clinician participation in root cause analysis is vital as these initiatives recognize and address essential patient care aspects. Through a review of data gathered by the Joint Commission, the most common categories of clinical error resulting in patient death, which can be prevented through root cause analysis, have been identified. These sentinel events, which account for a significant proportion of morbidity and mortality within the hospital setting, include: [13]
- Surgical errors
- Diagnostic errors
- Patient suicide
- Medication errors
- Equipment errors
- Hospital-acquired infections
- Patient falls
- Communication errors
Medical Error Prevention Measures
By identifying the deficiencies, failures, and risk factors that lead to an adverse event, corrective measures can be developed to prevent similar errors. Subsequently, individuals involved in every aspect of healthcare can help implement appropriate preventative strategies to reduce future medical errors and improve patient safety. [17] The following interventions are some strategies institutions have implemented to address these common systemic flaws.
Surgical Errors
Preventative measures for surgical errors have frequently consisted of adopting checklists, counting instruments, initiating antibiotic prophylaxis for deep vein thrombosis, and utilizing radio-frequency marked sponges. [3] Additionally, the performance of a surgical time-out has become a widespread strategy to reduce surgical errors. A time-out is a pause before a surgical procedure begins. The surgical team pauses and reviews the patient's identity, the consent form, the procedure being performed, and the correct anatomical structures and side involved, which should be marked on the patient's skin. If multiple procedures by separate surgical teams are planned, separate time-outs must be done. Surgeons and every surgical team member involved in the procedure must be present during the time-out, and any disagreement during the time-out should trigger an investigation by the surgical team until the discrepancy is resolved. [33]
Wrong-site surgery is a major cause of medical errors that can be mitigated through various preoperative safety checkpoints and has been the subject of a sentinel event alert by the Joint Commission. [13] [34] These errors have most commonly been noted in orthopedic surgeries. [35] Risk factors include several surgeons involved in surgical care or transfers to another surgeon for patient care, multiple procedures on a single patient, time constraint pressures, and unique circumstances requiring unusual or special positioning during a surgical procedure. [34] Wrong-site surgeries can easily be mitigated by ensuring proper preoperative measures, such as labeling the correct surgical site with an indelible pen or distinctively marking the nonsurgical site before the surgery. Intraoperative radiography can also assist in aiding the correct surgical site during the procedure.
Diagnostic Errors
Diagnostic errors such as misdiagnoses, delayed diagnostic test results, lack of staffing or physician availability, delays in order fulfillment, inadequate treatment, and delays within the emergency department can cause delays in medical treatment that may result in patient death and permanent injuries. Reducing diagnostic errors requires a comprehensive approach that implements various strategies due to the many factors that can lead to these errors. System-based safety checks and cognitive aids are often recommended as interventions to help prevent diagnostic errors. Cognitive aids include algorithms to help guide decision-making based on accepted guidelines, "trigger tools" within electronic health records that remind clinicians to consider differential diagnoses for commonly misdiagnosed conditions, and checklists to prevent the omission of critical steps. [11] [36] According to a 2015 New England Journal of Medicine article, trigger tools are essential in reducing this type of medical error. [36] Trigger tools are electronic algorithms that identify potential adverse events. This is accomplished by searching electronic health records and flagging specific occurrences. [36] The use of cognitive aids and trigger tools has been shown to decrease the rate of misdiagnoses in recent studies. [36] Addressing deficiencies through various other strategies (eg, device-based decision support, simulation-based training, and increased specialist utilization) may also help reduce diagnostic errors. [24] Though ingrained practice methods and physician overconfidence can attenuate the success of these interventions, fostering critical thinking and promoting "pause and reflect" methods have been found to help avert diagnostic errors, especially in cases with obscure clinical findings or unexpected clinical trajectories. [37] [25] Aside from encouraging critical thinking, opportunities for case discussions and second opinions should be made available for the treating providers. Healthcare facilities should also provide avenues for second opinions or interdisciplinary teams where cases can be discussed. [37] Other interventions to reduce diagnostic errors of commonly misdiagnosed conditions include simulation-based training, performance feedback, and encouraging the contributions of nurses, pharmacists, and other health professionals during patient care. [24]
Patient Suicide
Patient suicide is an unfortunate cause of death commonly seen in psychiatric care settings. [13] Several risk-reduction methods can be implemented for this adverse event, including ensuring a controlled environment free of hazardous materials, frequent patient observation, effective communication, adequate staffing in the facility, suicide assessment upon admission, regular psychiatric evaluation, and assessment for the presence of contraband.
Medication Errors
Medication administration errors are a common and avoidable adverse event that can occur at various patient care levels, involving many individuals in a multidisciplinary patient care team. [38] Barcode administration and handheld personal digital assistants increase medication administration safety by providing real-time patient information, medication profiles, laboratory values, drug information, and documentation. Moreover, electronic medication administration helps identify incorrect medications and orders that have been canceled or modified. However, circumventing barcode procedures decreases safety at the point of care. Automatic dispensing systems that quickly make drugs available to patients allow pharmacy clinicians to engage in other safety activities, such as medication reconciliation. Additionally, look-alike medications should be stored away from more dangerous medications. Hospitals can also standardize storage areas and avoid medication containers that have a similar appearance. Pharmacy clinicians should remove dangerous medications from floor stock and discard out-of-date drugs as a preventative measure. Other strategies include using color-coded intravenous lines, utilizing standard concentrations of vasoactive agents, labeling syringes immediately after preparation, and capitalizing the differences on the labels of medications with similar names. [11] [3]
Equipment Errors
Health professionals should be involved in setting and evaluating institutional, organizational, and public technology-related policies. Safety primarily can be improved by developing protocols for equipment maintenance, training, monitoring, and reporting adverse events related to technology. Additionally, clinicians should be educated in remaining vigilant despite clinical assistance by devices and able to manage equipment failure situations. [39] Unique connectors for anesthesia catheters and feeding tubes can be used to reduce the chances of tubing misconnections. [40] Furthermore, clinicians and support staff should always trace lines back to the origin before connecting or disconnecting devices or starting infusions and labeling high-risk catheters. [27] [28]
Hospital-acquired Infections
Changing the behaviors of healthcare team members is effective in reducing iatrogenic infections. Hand hygiene campaigns have been shown to decrease the number of nosocomial infection rates for various infections and should be universally endorsed. [41] Most healthcare facilities now employ specific protocols for minimizing central venous and urinary catheter use and using protective measures such as chlorhexidine for vascular catheter site care to reduce the incidence of healthcare-associated bloodstream infections, ventilator-associated pneumonia, and catheter-associated urinary tract infections. [3] Minimizing the duration of use of indwelling catheters has also effectively reduced the incidence of associated infections. [41] [3]
To decrease the risk of nosocomial infections, pharmacy-driven antibiotic stewardship programs should be regularly employed in all patients admitted to a healthcare facility. [42] Frequent skin assessment and evaluation by wound care teams with regular and focused nursing education and evidence-based treatments should be routinely employed to lower healthcare-associated pressure injuries. [43] The care of surgical sites should follow similar protocols, with some studies proposing chlorhexidine-impregnated dressings to decrease the incidence of surgical site infections. [3]
Patient Falls
Similarly, patient falls are a constant source of injury within healthcare facilities. Patients at high risk for falls should be identified, and appropriate safety precautions should be taken. Elderly patients tend to be prone to falls due to their age-related changes in vision or cardiovascular problems. Elderly patients also frequently have increased balance issues and muscle weakness over time, leading to ambulatory dysfunction. Having fall-prevention protocols in place, identifying potential high-risk areas within the home, and mitigating them through safety measures can improve patient safety and outcomes. [13]
Standardized protocols can reduce fall rates by ensuring a safe environment for risk-prone patients. Patient factors contributing to falls include advanced age, mobility impairment, and postsurgical effects. [31] Inadequate nurse staffing, an increased portion of staff made of new nurses, and increased shift hours are organizational factors that can lead to patient falls. [31] Implementing fall prevention protocols in hospitals and long-term care facilities has significantly reduced these errors. Furthermore, standardized fall risk assessments such as the Morse Fall Scale can decrease patient falls. [3] Institutional interventions such as staff education, patient mobility training with rehabilitation professionals, and nutritionist support have also been shown to reduce patient falls. [3] Other strategies include identifying patients at high risk for falls, providing patient safety companions, educating caregivers about fall prevention, and setting bed alarms and frequent safety rounds for all high-risk patients. [3]
Communication Errors
A courteous and respectful workplace where the interprofessional team collaborates promotes a safe work environment for all healthcare team members, families, and patients. Risk management committees and interprofessional task forces should work collaboratively on risk assessment and reduction. Joint education programs help providers and support staff learn roles and develop relationships to improve safety. The Joint Commission's Safety Goals require that for critical test results and verbal or telephone orders, a "read-back" verbatim to the practitioner by the person receiving and recording the result or order. The practitioner should then verbally acknowledge the accuracy of the order. [11]
Additionally, healthcare staff should avoid common errors in written communication, such as using nonstandard abbreviations, illegible handwriting, failure to question inappropriately written orders, and failure to complete correct specimen labeling. Therefore, staff should be encouraged to ask questions when uncertain and trained to double-check that the patient's name is spelled correctly and their correct date of birth is present. The Joint Commission requires healthcare professionals to use 2 or more patient identifiers when labeling, delivering, and maintaining specimens. Since this is a National Patient Safety Goal, The Joint Commission closely monitors healthcare institutions' adherence to this requirement as they prepare medications and transfusions and transfer patients from unit to unit. [11]
Clinicians should also follow well-communicated protocols that guide care and communication with patients. Age-associated hearing and cognitive decline increase the likelihood of communication errors regarding medications. Ensuring appropriate communication skills tailored to distinct patient groups is crucial in preventing such errors. Young children and infants are similarly prone to common medical errors due to the lack of direct participation in decision-making and patient care. Thus, specialized communication is needed to convey medical instructions to elderly and younger patients and their caregivers to ensure no lapses in communication. Providers should listen to patients' questions concerning how care is delivered. Concerns must be respected and accepted if care plans contradict established evidence-based medicine. Moreover, the Joint Commission has supported "speak up" initiatives, which encourage hospitals to inform patients about the importance of their contributions to the care they receive in preventing medical errors. To make patients active participants in avoiding medical errors, encourage patients to ask about unfamiliar tests, unplanned diagnostic tests, and medications and to verify the correct surgical site. [11] Additionally, skilled medical interpreters can be crucial in effectively communicating instructions and information to patients instead of family members, who may often be biased. Implementing standardized clinician-family communication at the patient bedside with family engagement and bidirectional communication also decreased the frequency of harmful medical errors and positively impacted the family experience. [44]
Communication errors during patient hand-offs can occur when incorrect information is passed to the receiving clinician, or pertinent information is omitted. [45] Several techniques developed to minimize errors when handing off patients include using electronic records and mnemonics (eg, situation, background, assessment, and recommendation [SBAR]) to address all pertinent information. [46] [47] The SBAR tool is considered a best-practice communication technique to deliver information in an organized and logical fashion during hand-off and critical patient care situations. [47] The US's National Academies of Sciences, Engineering, and Medicine also recommend that these hand-offs occur in real-time and allow the opportunity to ask and respond to questions regarding pertinent facts about patient care. [48] This principle should be used when discharging patients from the hospital as well. Clinicians should remember to perform a final bedside evaluation and review discharge instructions before sending any patient home, including giving the patient a thorough written follow-up plan, counseling on new medications, and instruction to return to the hospital or office for new or worsening symptoms.
- Enhancing Healthcare Team Outcomes
Medical errors are undeniably an essential cause of patient morbidity and mortality within the United States healthcare system. These errors are prevalent at rampant levels, and the consequences of such errors can severely impact the patient, family members, and clinicians. The interprofessional healthcare team plays an invaluable role in preventing medical errors; team effort is crucial in identifying strategies and solutions to reduce the burden of medical error on the healthcare system. Nurses, pharmacists, rehabilitation professionals, nutritionists, and physicians are integral to the patient care team and crucial in preventing medical errors. Practitioners who work in error-prone environments must recognize their roles as healthcare team members responsible for reducing unnecessary errors. [49] The interprofessional team members comprising the RCA team should include professionals from all disciplines to ensure an effective investigation and implementation of corrective measures.
Clinicians should not hesitate to provide their peers with assistance in recognizing particular sources of common medical errors to deliver better patient care. Equal accountability and responsibility of all healthcare team members are critical in preventing errors and providing superior patient safety. [1] Quality assurance teams should employ RCAs with every sentinal event, especially in situations when the identification of medical errors becomes difficult or complex due to many underlying factors. RCAs can help identify factors within the healthcare delivery process that may impede the ability to provide quality patient care. Given the preventable nature of most medical errors, a thorough RCA can improve patient safety and allow healthcare organizations to serve as a model for others.
Healthcare professionals should be aware of common medical error sources and work as a team to identify possible risks when they become apparent. Doing so will increase the quality and efficiency of the healthcare industry and patient trust in the healthcare system. When an RCA is performed, the cooperation of all healthcare team members and clinicians involved in patient care is critical to understanding the underlying source of a medical error and identifying future strategies to mitigate such errors and improve patient outcomes.
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Disclosure: Gunjan Singh declares no relevant financial relationships with ineligible companies.
Disclosure: Raj Patel declares no relevant financial relationships with ineligible companies.
Disclosure: Sarosh Vaqar declares no relevant financial relationships with ineligible companies.
Disclosure: Joshua Boster declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Singh G, Patel RH, Vaqar S, et al. Root Cause Analysis and Medical Error Prevention. [Updated 2024 Feb 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Medical Error Reduction and Prevention. [StatPearls. 2024] Medical Error Reduction and Prevention. Rodziewicz TL, Houseman B, Vaqar S, Hipskind JE. StatPearls. 2024 Jan
- Prevention of Surgical Errors. [StatPearls. 2024] Prevention of Surgical Errors. Santos G, Jones MW. StatPearls. 2024 Jan
- Medication Dispensing Errors and Prevention. [StatPearls. 2024] Medication Dispensing Errors and Prevention. Tariq RA, Vashisht R, Sinha A, Scherbak Y. StatPearls. 2024 Jan
- Review Improving safety for children with cardiac disease. [Cardiol Young. 2007] Review Improving safety for children with cardiac disease. Thiagarajan RR, Bird GL, Harrington K, Charpie JR, Ohye RC, Steven JM, Epstein M, Laussen PC. Cardiol Young. 2007 Sep; 17 Suppl 2:127-32.
- Review Tuberculosis. [Major Infectious Diseases. 2017] Review Tuberculosis. Bloom BR, Atun R, Cohen T, Dye C, Fraser H, Gomez GB, Knight G, Murray M, Nardell E, Rubin E, et al. Major Infectious Diseases. 2017 Nov 3
Recent Activity
- Root Cause Analysis and Medical Error Prevention - StatPearls Root Cause Analysis and Medical Error Prevention - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers

Important Factors in Healthcare Litigation
Effective healthcare litigation outcomes hinge on multiple critical factors. Meticulous documentation and record-keeping are indispensable, as incomplete or inaccurate records can compromise credibility and influence case outcomes. Clear communication with patients is also imperative, enabling informed decisions and managing expectations. Qualified specialist witness testimony, thorough risk management strategies, and strong peer review and quality assurance processes are likewise pivotal. Furthermore, compliance with regulatory standards and objective, unbiased medical opinions are necessary to establish credibility and facilitate successful litigation outcomes. A thorough understanding of these factors is necessary to traversing the complexities of healthcare litigation.
Table of Contents
Meticulous Documentation and Record-Keeping
Accurate and detailed documentation of patient care and treatment is crucial in healthcare litigation, as it provides a verifiable record of events that can substantially impact the outcome of legal proceedings. Incomplete or inaccurate records can lead to adverse inferences, compromising the credibility of healthcare providers and potentially influencing the outcome of legal cases.
To ensure data integrity, healthcare organizations must implement robust documentation systems that capture accurate and comprehensive information about patient care. This includes maintaining detailed records of diagnoses, treatments, medications, and test results. Regular compliance audits are also essential to verify the accuracy and completeness of documentation, identifying any discrepancies or gaps that require correction. By prioritizing meticulous documentation and record-keeping, healthcare providers can demonstrate a commitment to quality care, reduce the risk of litigation, and ensure that their records withstand scrutiny in legal proceedings.
Effective Communication With Patients
Effective communication with patients is a critical aspect of healthcare litigation, as it can substantially impact the outcome of legal proceedings. Setting clear expectations and establishing open communication channels with patients can help prevent misunderstandings and foster trust, thereby reducing the likelihood of litigation. By prioritizing clear and transparent communication, healthcare providers can proactively address patient concerns and mitigate potential risks.
Clear Expectations Set
In healthcare settings, establishing clear expectations with patients is vital, as it enables them to make informed decisions about their care and reduces the likelihood of misunderstandings that can lead to litigation. By setting realistic timelines for treatment outcomes, healthcare providers can manage patient expectations and avoid potential conflicts. This approach also promotes patient empowerment, as individuals are more likely to take an active part in their care when they understand what to expect.
Clear expectations also facilitate informed consent, making patients aware of potential risks and benefits associated with their treatment. This, in turn, reduces the risk of allegations of misdiagnosis or malpractice. Additionally, clear expectations help to establish a sense of trust between healthcare providers and patients, which is critical in building a strong patient-provider relationship. By prioritizing clear expectations, healthcare providers can reduce the risk of litigation and improve overall patient outcomes. Ultimately, establishing clear expectations is a critical component of effective communication in healthcare settings, as it supports a collaborative dynamic where patients feel informed and healthcare providers can provide high-quality care.
Open Communication Channels
Establishing open communication channels is crucial in healthcare settings, as it enables patients to ask questions, express concerns, and receive timely updates about their care, thereby fostering a collaborative relationship between patients and healthcare providers. Effective communication with patients is fundamental in preventing misunderstandings, alleviating anxiety, and promoting adherence to treatment plans. However, cultural barriers and language disparities can hinder open communication. Healthcare providers must be sensitive to these differences and take steps to address them, such as using interpreters or providing multilingual resources. Additionally, technological limitations, such as outdated electronic health records or inadequate patient portals, can also impede communication. To overcome these challenges, healthcare organizations must invest in modern technologies that facilitate seamless communication and provide ongoing training to staff on effective communication strategies. By prioritizing open communication channels, healthcare providers can guarantee that patients receive high-quality care, reduce the risk of adverse events, and minimize the likelihood of litigation.
Qualified Expert Witness Testimony
Frequently, the credibility of a medical malpractice case hinges on the testimony of a qualified authority, whose objective analysis and tailored knowledge can substantially influence the outcome of a trial. The testimony of an expert witness can make or break a case, as it provides the jury with a deeper understanding of the medical standards and practices in question. Credibility factors, such as the witness's qualifications, experience, and impartiality, play a significant role in shaping jury perceptions. A qualified expert witness can establish credibility by demonstrating a thorough understanding of the relevant medical issues, providing clear and concise explanations, and avoiding bias or emotional appeals.
The jury's perception of the expert witness's credibility is critical, as it directly impacts the weight given to their testimony. A credible expert witness can increase the plaintiff's chances of success by providing persuasive testimony that resonates with the jury. Conversely, a witness lacking credibility can undermine the plaintiff's case, leading to a verdict in favor of the defendant. Therefore, it is essential to identify and engage a qualified expert witness who can provide objective, authoritative testimony that effectively communicates complex medical concepts to the jury.
Thorough Risk Management Strategies
Effective risk management is a vital component of healthcare litigation prevention, and a thorough strategy involves pinpointing zones of high risk, developing targeted mitigation measures, and regularly monitoring and updating these protocols to guarantee maximum protection. By identifying vulnerabilities and addressing them proactively, healthcare providers can substantially reduce their liability exposure. A thorough risk management approach enables healthcare organizations to anticipate and respond to potential threats, ultimately minimizing the likelihood of litigation.
Identify High-Risk Areas
In the pursuit of thorough risk management, pinpointing high-risk sections within healthcare organizations is crucial to mitigating potential legal liabilities and promising excellent patient care. Identifying these segments enables healthcare providers to allocate resources effectively and develop targeted strategies to minimize risks.
Vulnerable populations, such as pediatric and geriatric patients, are often at higher risk of adverse events due to their unique needs and circumstances. Healthcare organizations must prioritize these groups and implement measures to safeguard their safety. Medication errors, for instance, can have devastating consequences, particularly among vulnerable populations. A thorough risk management strategy should involve regular audits and assessments to identify potential vulnerabilities in medication administration processes, thereby protecting patients and preventing harm in this critical sector.
Implement Mitigation Measures
Having identified high-risk regions, healthcare organizations can proactively develop and implement thorough risk management strategies to mitigate potential legal liabilities and provide excellent patient care. This involves conducting an exhaustive risk assessment to identify vulnerabilities and prioritize sectors that require improvement. A thorough risk management strategy should comprise policies, procedures, and guidelines that address high-risk sectors, guaranteeing that healthcare providers are equipped to manage risks effectively.
Implementing mitigation measures also requires a cultural shift within the organization. Healthcare providers must adopt a culture of transparency, accountability, and open communication to foster a safe and reliable environment. This can be achieved by promoting a just culture, where mistakes are viewed as opportunities for growth and improvement, rather than punished. By implementing thorough risk management strategies and fostering a cultural shift, healthcare organizations can reduce the likelihood of adverse events, improve patient outcomes, and minimize the risk of litigation.
Monitor and Update
Regular monitoring and updating of thorough risk management strategies are essential to verify their continued relevance and effectiveness in mitigating legal liabilities and improving patient care. This involves conducting regular system checks to identify potential vulnerabilities and implementing policy revisions as needed. By doing so, healthcare organizations can ensure that their risk management strategies remain effective in preventing adverse events and reducing the likelihood of litigation.
| Patient consent forms | Quarterly | Changes in regulatory requirements or patient feedback |
| Medication administration protocols | Bi-annually | Updates in medical research or manufacturer guidelines |
| Staff training programs | Annually | Changes in industry best practices or staff feedback |
Through regular monitoring and updating, healthcare organizations can demonstrate a proactive approach to risk management, which can help to reduce legal liabilities and improve patient outcomes. By staying up-to-date with industry best practices and regulatory requirements, healthcare organizations can ensure that their risk management strategies remain effective and relevant.
Strong Peer Review and QA Process
A robust peer review and quality assurance (QA) process serves as a cornerstone of healthcare litigation defense, providing a critical layer of protection against medical malpractice claims. This process ensures that healthcare providers are held to high standards of care and that any deviations from these standards are identified and addressed promptly. Effective peer oversight and review protocols are essential components of a strong QA process.
Some key elements of a robust peer review and QA process include:
- *Establishing clear review protocols and criteria*
- *Conducting regular peer review of patient care and outcomes*
- *Identifying and addressing areas for improvement*
- *Providing ongoing education and training for healthcare providers*
- *Maintaining accurate and detailed records of peer review activities and QA initiatives*
Compliance With Regulatory Standards
In addition to a robust peer review and QA process, adherence to regulatory standards is vital in healthcare litigation defense, as it demonstrates a healthcare organization's commitment to providing high-quality patient care and reducing the risk of medical malpractice claims. Regulatory standards, such as those set by the Joint Commission and HIPAA, provide a framework for healthcare organizations to verify they are meeting minimum requirements for patient care and safety. Compliance with these standards is imperative, as non-compliance can lead to enforcement actions, fines, and reputational damage. Furthermore, staying up-to-date with regulatory updates is vital, as new regulations and guidelines are constantly being introduced. Healthcare organizations must have a system in place to monitor and implement these updates to avoid potential legal and financial consequences. By prioritizing compliance with regulatory standards, healthcare organizations can demonstrate a proactive approach to patient safety and quality care, which can be a powerful defense in the event of litigation.
Objective and Unbiased Medical Opinions
Compliance with regulatory standards sets the foundation for a robust defense in healthcare litigation, and objective and unbiased medical opinions serve as a critical component in supporting this defense. These opinions are essential in establishing the standard of care, assessing treatment decisions, and evaluating patient outcomes. Moreover, they play a crucial role in resolving disputes and allocating liability.
To ensure the credibility of medical opinions, several factors must be considered:
- Credibility factors : The expert's qualifications, experience, and reputation significantly impact the weight given to their opinion.
- Opinion variability : The degree of consensus among medical professionals on a particular issue can influence the persuasiveness of an opinion.
- Evidence-based medicine : Opinions grounded in scientific evidence and current medical literature carry more weight than those based on anecdotal experience or personal preference.
- Objectivity : Opinions should be free from bias, conflicts of interest, and emotional influence.
- Clear and concise communication : Opinions should be articulated in a clear, concise, and easily understandable manner to facilitate effective communication with judges, juries, and other stakeholders. By considering these factors, healthcare providers can ensure that their medical opinions are objective, unbiased, and credible, ultimately strengthening their defense in litigation.
Frequently Asked Questions
Can healthcare providers be liable for third-party vendor negligence?.
Healthcare providers can be liable for third-party vendor negligence if they fail to exercise due diligence in vendor selection and oversight, including inadequate vendor contracts and lack of regular third-party audits to verify compliance with regulatory standards.
Are Electronic Health Records More Susceptible to Errors?
Electronic health records (EHRs) are vulnerable to errors due to compromised data integrity, often stemming from user fatigue, inadequate training, and insufficient quality control measures, which can lead to inaccurate or incomplete patient information.
Do Hospitals Have a Responsibility to Report Medical Errors?
Hospitals have a moral and ethical responsibility to report medical errors, promoting transparent error disclosure that prioritizes patient safety, fostering trust and facilitating quality improvement initiatives to prevent recurring errors and enhance overall care outcomes.
Can Patients Sue for Emotional Distress Without Physical Harm?
In medical malpractice cases, patients may sue for emotional distress without physical harm if they exceed the Anxiety Threshold, demonstrating a Fear Factor that meets the legal standard for negligent infliction of emotional distress.
Are Healthcare Providers Liable for Patient Non-Compliance?
Healthcare providers are not typically liable for patient non-compliance, as patient autonomy prioritizes individual decision-making. However, providers must guarantee or certify informed consent and clear communication to facilitate treatment adherence, mitigating potential liability risks.
- Open access
- Published: 19 August 2024
The impact of study habits and personal factors on the academic achievement performances of medical students
- Mohammed A. Aljaffer 1 ,
- Ahmad H. Almadani 1 ,
- Abdullah S. AlDughaither 2 ,
- Ali A. Basfar 2 ,
- Saad M. AlGhadir 2 ,
- Yahya A. AlGhamdi 2 ,
- Bassam N. AlHubaysh 2 ,
- Osamah A. AlMayouf 2 ,
- Saleh A. AlGhamdi 3 ,
- Tauseef Ahmad 4 &
- Hamza M. Abdulghani 5
BMC Medical Education volume 24 , Article number: 888 ( 2024 ) Cite this article
440 Accesses
2 Altmetric
Metrics details
Academic achievement is essential for all students seeking a successful career. Studying habits and routines is crucial in achieving such an ultimate goal.
This study investigates the association between study habits, personal factors, and academic achievement, aiming to identify factors that distinguish academically successful medical students.
A cross-sectional study was conducted at the College of Medicine, King Saud University, Riyadh, Saudi Arabia. The participants consisted of 1st through 5th-year medical students, with a sample size of 336. The research team collected study data using an electronic questionnaire containing three sections: socio-demographic data, personal characteristics, and study habits.
The study results indicated a statistically significant association between self-fulfillment as a motivation toward studying and academic achievement ( p = 0.04). The results also showed a statistically significant correlation between recalling recently memorized information and academic achievement ( p = 0.05). Furthermore, a statistically significant association between preferring the information to be presented in a graphical form rather than a written one and academic achievement was also found ( p = 0.03). Students who were satisfied with their academic performance had 1.6 times greater chances of having a high-grade point average (OR = 1.6, p = 0.08).
The results of this study support the available literature, indicating a correlation between study habits and high academic performance. Further multicenter studies are warranted to differentiate between high-achieving students and their peers using qualitative, semi-structured interviews. Educating the students about healthy study habits and enhancing their learning skills would also be of value.
Peer Review reports
Introduction
Academic performance is a common indicator used to measure student achievement [ 1 , 2 ]. It is a compound process influenced by many factors, among which is study habits [ 2 , 3 ]. Study habit is defined as different individual behavior in relation to studying, and is a combination of study methods and skills [ 2 , 3 , 4 ]. Put differently, study habits involve various techniques that would increase motivation and transform the study process into an effective one, thus enhancing learning [ 5 ]. Students’ perspectives and approaches toward studying were found to be the key factors in predicting their academic success [ 6 , 7 ]. However, these learning processes vary from one student to another due to variations in the students’ cognitive processing [ 8 ].
The study habits of students are the regular practices and habits they exhibit during the learning process [ 9 , 10 ]. Over time, several study habits have been developed, such as time management, setting appropriate goals, choosing a comfortable study environment, taking notes effectively, choosing main ideas, and being organized [ 11 ]. Global research shows that study habits impact academic performance and are the most important predictor of it [ 12 ]. It is difficult for medical students to organize and learn a lot of information, and they need to employ study skills to succeed [ 1 , 2 , 5 , 13 ].
Different lifestyle and social factors could affect students’ academic performance. For instance, Jafari et al. found that native students had better study habits compared to dormitory students [ 1 ]. This discrepancy between native and dormitory students was also indicated by Jouhari et al. who illustrated that dormitory students scored lower in attitude, test strategies, choosing main ideas, and concentration [ 10 ]. Regarding sleeping habits, Curcio G et al. found that students with a regular and adequate sleeping pattern had higher Grade Point Average (GPA) scores [ 14 ]. Lifestyle factors, such as watching television and listening to music, were shown to be unremarkable in affecting students’ grades [ 15 , 16 ]. Social media applications, including WhatsApp, Facebook, and Twitter, distract students during learning [ 16 , 17 ].
Motivation was found to be a major factor in students’ academic success. Bonsaksen et al. found that students who chose “to seek meaning” when studying were associated with high GPA scores [ 18 ]. In addition, low scores on “fear of failure” and high scores on “achieving” correlated with a higher GPA [ 8 , 18 ].
Resource-wise, Alzahrani et al. found that 82.7% of students relied on textbooks assigned by the department, while 46.6% mainly relied on the department’s lecture slides [ 19 ]. The study also indicated that 78.8% perceived that the scientific contents of the lectures were adequate [ 19 ]. Another study found that most students relied on the lecture slides (> 83%) along with their notes, followed by educational videos (76.1%), and reference textbooks (46.1%) [ 20 ]. Striking evidence in that study, as well as in another study, indicated that most students tended to avoid textbooks and opted for lecture slides, especially when preparing for exams [ 20 , 21 ].
Several researchers studied the association between different factors and academic performance; however, more is needed to know about this association in the process of education among medical students [ 15 , 20 , 22 ], with some limitations to the conducted studies. Such limitations include the study sample and using self-reported questionnaires, which may generate inaccurate results. Moreover, in Saudi Arabia in particular, the literature concerning the topic remains limited. Since many students are unsatisfied with their performance and seek improvement [ 10 ], the present study was designed and conducted.
Unlike other studies in the region, this study aims to investigate the relationship between study habits and personal factors and measure their influence on academic achievement. The results of this study could raise awareness regarding the effect of study habits and personal factors on students’ performance and would also guide them toward achieving academic success. The study also seeks to identify the factors that distinguish academically successful students from their peers.
Study design, setting, and participants
This observational cross-sectional study, which took place between June and December 2022, was conducted among students attending the College of Medicine at King Saud University (KSU), Riyadh, Saudi Arabia. Its targeted population included all male and female medical students (first to fifth years) attending KSU during the academic year 2021/2022. Whereas, students at other colleges and universities, those who failed to complete the questionnaire, interns (the students who already graduated), and those who were enrolled in the university’s preparatory year, were all excluded from the current study. The sample size was calculated based on a study conducted in 2015 by Lana Al Shawwa [ 15 ]. Using the sample size formula for a single proportion (0.79), the required sample size was 255 using a confidence interval of 95% and a margin of error of 5%. After adding a 20% margin to accommodate non-responses and incomplete responses, the calculated sample size required for this study was 306. However, our research team collected a total of 336 participants for this study to ensure complete representation.
Study instrument
The research team developed and used an electronic questionnaire. The rationale is that no standardized questionnaire measuring the study objectives was found in the literature. However, the questionnaire was tested on a pilot of 15 students to test its clarity and address any possible misconceptions and ambiguity. The study questionnaire was distributed randomly to this cohort, who were asked to fill out the questionnaire. The students reported a complete understanding of the questionnaire’s contents, so the same questionnaire was used without any modifications. The questionnaire, written in English, consisted of three parts. The first part included eleven questions about the socio-demographic status of the participants. The second part contained twenty-one questions examining personal factors such as sleep and caffeine consumption. The last part included twenty-one questions regarding students’ study habits. The questionnaire was constructed based on an ordinal Likert scale which had: strongly agree, agree, neutral, disagree, and strongly disagree as possible answers. The questionnaire was sent to participants through email and social media applications like Twitter and WhatsApp to increase the study response. An informed consent that clearly states the study’s purpose was taken from all participants at the beginning of the questionnaire. In addition, all participants were assured that the collected data would be anonymous and confidential. Each participant was represented by a code for the sole purpose of analyzing the data. Furthermore, no incentives or rewards were given to the participants for their participation.
Study variables
Socio-demographic information (such as age, gender, and academic year), and personal factors (such as motivation, sleeping status, caffeine consumption, and self-management) were the independent variables. Study habits such as attendance, individual versus group study, memorization techniques, revision, learning style, and strategies were also independent variables.
Academic achievement refers to a student’s success in gaining knowledge and understanding in various subjects, as well as the ability to apply that knowledge effectively [ 23 ]. It is a measure of the student’s progress throughout the educational journey, encompassing both academic achievements and personal growth [ 3 , 24 ]. Academic achievement is judged based on the student’s GPA or performance score. In this study, students’ GPA scores, awareness, and satisfaction regarding their academic performance were the dependent variables.
We divided the study sample into two groups based on the GPA. We considered students with high GPAs to be exposed (i.e. exposed to the study habits we are investigating), and students with low GPAs to be the control group. The purpose of this study was to determine why an exposed group of students gets high grades and what study factors they adopt. Based on this exposure (high achieving students), we concluded what methods they used to achieve higher grades. Those in the first group had a GPA greater or equal to 4.5 (out of 5), while those in the second group had a GPA less than 4.5. The students’ data were kept confidential and never used for any other purpose.
Data analysis
The data collected were analyzed by using IBM SPSS Statistical software for Windows version 24.0. Descriptive statistics such as frequency and percentage were used to describe the socio-demographic data in a tabular form. Furthermore, data for categorical variables, including different study habits, motivation factors, memorizing and revising factors, and lifestyle factors, were tabulated and analyzed using the odds ratio test. Finally, we calculated the odds ratio statistic and a p-value of 0.05 to report the statistical significance of our results.
Ethical approval and consent to Participate
Before conducting the study, the research team obtained the Ethics Committee Approval from the Institutional Review Board of the College of Medicine, KSU, Riyadh, Saudi Arabia (project No. E-22-7044). Participants’ agreement/consent to participate was guaranteed by choosing “agree” after reading the consent form at the beginning of the questionnaire. Participation was voluntary, and consent was obtained from all participants. The research team carried out all methods following relevant guidelines and regulations.
The total 336 medical students participated in the study. All participants completed the study questionnaire, and there were no missing or incomplete data, with all of them being able to participate. As shown in Table 1 9.3% of participants were between 18 and 20, 44.9% were between the ages of 21 and 22, and 35.8% were 23–28 years old. In the current study, 62.5% of the participants were males and 37.5% were females. The proportion of first-year students was 21.4%, 20.8% of second-year students, 20.8% of third-year students, 18.2% of fourth-year students, and 18.8% of fifth-year students, according to academic year levels. Regarding GPA scores, 36.9% scored 4.75-5 and 32.4% scored 4.5–4.74. 23.8% achieved 4-4.49, 6.5% achieved 3-3.99, and only 0.4% achieved 2.99 or less. Participants lived with their families in 94.6% of cases, with friends in 1.2% of cases, and alone in 4.2% of cases. For smoking habits, 86.3% did not smoke, 11% reported using vapes, 2.1% used cigarettes, and 0.6% used Shisha. 91.4% of the participants did not report any chronic illnesses; however, 8.6% did. In addition, 83% had no mental illness, 8.9% had anxiety, 6% had depression, and 2.1% reported other mental illnesses.
Table 2 shows motivational factors associated with academic performance. There was a clear difference in motivation factors between students with high and low achievement in the current study. Students with high GPAs were 1.67 times more motivated toward their careers (OR = 1.67, p = 0.09) than those with low GPAs. Furthermore, significant differences were found between those students who had self-fulfillment or ambitions in life they had ~ 2 times higher (OR = 1.93, p = 0.04) GPA scores than low GPA students. Exam results did not motivate exposed or high GPA students (46%) or control students with low GPA students (41%), but the current study showed test results had little impact on low achiever students (OR = 1.03, p = 0.88). Furthermore, 72.6% of high achievers were satisfied with their academic performance, while only 41% of low achiever students were satisfied. Therefore, students who were satisfied with their academic performance had 1.6 times greater chances of a higher GPA (OR = 1.6, p = 0.08). Students who get support and help from those around them are more likely to get high GPAs (OR = 1.1, p = 0.73) than those who do not receive any support. When students reported feeling a sense of family responsibility, the odds (odds ratio) of their receiving higher grades were 1.15 times higher (OR = 1.15, p = 0.6) compared to those who did not feel a sense of family responsibility. The p-value, which indicates the level of statistical significance, was 0.6.
Table 3 shows the study habits of higher achiever students and low achiever students. Most of the high-achieving students (79.0%) attended most of the lectures and had 1.6 times higher chances of getting higher grades (OR = 1.6, p = 0.2) than those who did not attend regular lectures. The current study found that studying alone had no significant impact on academic achievement in either group. However, those students who had studied alone had lower GPAs (OR = 1.07, p = 0.81). The current study findings reported 29.8% of students walk or stand while studying rather than sit, and they had 1.57 times higher GPA chances compared to students with lower GPAs (OR = 0.73, p = 0.27). High achievers (54.0%) preferred studying early in the morning, and these students had higher chances of achieving good GPAs (OR = 1.3, p = 0.28) than low achiever groups of students. The number of students with high achievement (39.5%) went through the lecture before the lesson was taught. These students had 1.08 times higher chances of achieving than low achiever groups of students. Furthermore, students who made a weekly study schedule had 1.3 times higher chances of being good academic achievers than those who did not (OR = 1.3, p = 0.37). Additionally, high-achieving students paid closer attention to the lecturer (1.2 times higher). In addition, students with high GPAs spent more time studying when exam dates approached (OR = 1.3, p = 0.58).
Table 4 demonstrates the relationship between memorizing and revising with high and low GPA students. It was found that high achiever students (58.9%) studied lectures daily and had 1.4 times higher chances of achieving high grades (OR = 1.4, p = 0.16) than the other group. It was found that most of the high achievers (62.1%) skim the lecture beforehand before memorizing it, which led to 1.8 times higher chances of getting good grades in this exam (OR = 1.8, p = 0.06). One regular activity reported by high GPA students (82.3%) was recalling what had just been memorized. For this recalling technique, we found a significant difference between low-achieving students (OR = 0.8, p = 0.63) and high-achieving students (OR = 1.83, p = 0.05). A high achiever student writes notes before speaking out for the memorizing method, which gives 1.2 times greater chances of getting high grades (OR = 1.2, p = 0.55) than a student who does not write notes. A major difference in the current study was that high GPA achievers (70.2%) revise lectures more frequently than low GPA achievers (57.1%). They had 1.5 times more chances of getting high grades if they practiced and revised this method (OR = 1.5, p = 0.13).
Table 5 illustrates the relationship between negative lifestyle factors and students’ academic performance. The current study found that students are less likely to get high exam grades when they smoke. Students who smoke cigarettes and those who vape are 1.14 and 1.07 times respectively more likely to have a decrease in GPA than those who do not smoke. Those students with chronic illnesses had 1.22 times higher chances of a downgrade in the exam (OR = 1.22, p = 0.49). Additionally, students with high GPAs had higher mental pressures (Anxiety = 1.2, Depression = 1.18, and other mental pressures = 1.57) than those with low GPAs.
Learning is a multifaceted process that evolves throughout our lifetimes. The leading indicator that sets students apart is their academic achievement. Hence, it is crucial to investigate the factors that influence it. The present study examined the relationship between different study habits, personal characteristics, and academic achievement among medical students. In medical education, and more so in Saudi Arabia, there needs to be more understanding regarding such vital aspects.
Regarding motivational factors, the present study found some differences between high and low achievers. Students with high GPA scores were more motivated toward their future careers (OR = 1.67, p = 0.09). The study also indicated that students who had ambitions and sought self-fulfillment were more likely to have high GPA scores, which were statistically significant (OR = 1.93, p = 0.04). This was consistent with Bin Abdulrahman et al. [ 20 ], who indicated that the highest motivation was self-fulfillment and satisfying family dreams, followed by a high educational level, aspirations to join a high-quality residency program, and high income. Their study also found that few students were motivated by the desire to be regarded as unique students. We hypothesize that this probably goes back to human nature, where a highly rewarding incentive becomes the driving force of our work. Hence, schools should utilize this finding in exploring ways to enhance students’ motivation toward learning.
The present study did not find a significant effect of previous exam results on academic performance (OR = 1.03, p = 0.88). However, some studies reported that more than half of the high-achieving students admitted that high scores acquired on previous assessments are an important motivational factor [ 15 , 25 , 26 ]. We hypothesize that as students score higher marks, they become pleased and feel confident with their study approach. This finding shows how positive measurable results influence the students’ mentality.
The present study also explored the social environment surrounding medical students. The results indicated that those who were supported by their friends or family were slightly more likely to score higher GPAs (OR = 1.1, p = 0.73); however, the results did not reach a statistical significance. We hypothesize that a supportive and understanding environment would push the students to be patient and look for a brighter future. Our study results were consistent with previous published studies, which showed an association [ 3 , 27 , 28 , 29 , 30 ]. We hypothesize that students who spend most of their time with their families had less time to study, which made their study time more valuable. The findings of this study will hopefully raise awareness concerning the precious time that students have each day.
The association of different study habits among medical students with high and low GPAs was also studied in our study. It was noted that the high-achieving students try to attend their lectures compared to the lower achievers. This was in line with the previous published studies, which showed that significant differences were observed between the two groups regarding the attendance of lectures, tutorials, practical sessions, and clinical teachings [ 31 , 32 ]. The present study found that most students prefer to study alone, regardless of their level of academic achievement (82.1%). This finding is consistent with the study by Khalid A Bin Abdulrahman et al., which also showed that most students, regardless of their GPA, favored studying alone [ 20 ].
The present study findings suggest that a small number of students (29.8%) prefer to walk or stand while studying rather than sit, with most being high achievers (OR = 1.57, P = 0.15). A study reported that 40.3% of students with high GPAs seemed to favor a certain posture or body position, such as sitting or lying on the floor [ 15 ]. These contradictory findings might indicate that which position to adopt while studying should come down to personal preference and what feels most comfortable to each student. The present study also found that high achievers are more likely to prefer studying early in the morning (OR = 1.3, P = 0.28). The authors did not find similar studies investigating this same association in the literature. However, mornings might allow for more focused studying with fewer distractions, which has been shown to be associated with higher achievement in medical students [ 3 , 15 , 33 ].
Our study also found that 39.5% of the academically successful students reviewed pre-work or went through the material before they were taught it (OR = 1.08, p = 0.75), and 25% were neutral. Similar findings were reported in other studies, showing that academically successful students prepared themselves by doing their pre-work, watching videos, and revising slides [ 3 , 9 , 34 ]. Our study showed that 75% of high-achieving students tend to listen attentively to the lecturer (OR = 1.2, p = 0.48). Al Shawa et al. found no significant differences between the high achievers and low achievers when talking about attending lectures [ 15 ]. This could be due to the quality of teachers and the environment of the college or university.
Regarding the relationship between memorizing and revising with high and low GPA students, the present study found that students who study lectures daily are more likely to score higher than those who do not (OR = 1.4, p = 0.16). This finding is consistent with other studies [ 3 , 19 , 35 ]. For skimming lectures beforehand, an appreciable agreement was noted by high GPA students (62.1%), while only (42%) of low GPA students agreed to it. Similarly, previous published studies also found that highlighting and reading the content before memorization were both common among high-achieving students [ 15 , 36 ]. Furthermore, the present study has found recalling what has just been memorized to be statistically significantly associated with high GPA students (OR = 1.83, p = 0.05). Interestingly, we could not find any study that investigated this as an important factor, which could be justified by the high specificity of this question. Besides, when it comes to writing down/speaking out what has just been memorized, our study has found no recognizable differences between high-achieving students (75%) and low-achieving students (69%), as both categories had remarkably high percentages of reading and writing while studying.
The present study has found no statistical significance between regularly revising the lectures and high GPA ( p > 0.05), unlike the study conducted by Deborah A. Sleight et al. [ 37 ]. The difference in findings between our study and Deborah A. Sleight et al. might be due to a limitation of our study, namely the similar backgrounds of our participants. Another explanation could be related to curricular differences between the institutions where the two studies were conducted. Moreover, a statistically significant correlation between not preferring the data being presented in a written form instead of a graphical form and high GPA scores have been found in their study ( p < 0.05). However, a study conducted by Deborah A. Sleight et al. indicated that 66% of high achievers used notes prepared by other classmates compared to 84% of low achievers. Moreover, their study showed that only 59% of high achievers used tables and graphs prepared by others compared to 92% of low achievers. About 63% and 61% of the students in their study reported using self-made study aids for revision and memory aids, respectively [ 37 ].
The present study also examined the effects of smoking and chronic and mental illness, but found no statistical significance; the majority of both groups responded by denying these factors’ presence in their life. A similar finding by Al Shawwa et al. showed no statistical significance of smoking and caffeine consumption between low GPA and high GPA students [ 15 ]. We hypothesize that our findings occurred due to the study’s broad approach to examining such factors rather than delving deeper into them.
High-achieving students’ habits and factors contributing to their academic achievement were explored in the present study. High-achieving students were found to be more motivated and socially supported than their peers. Moreover, students who attended lectures, concentrated during lectures, studied early in the morning, prepared their weekly schedule, and studied more when exams approached were more likely to have high GPA scores. Studying techniques, including skimming before memorizing, writing what was memorized, active recall, and consistent revision, were adopted by high-achievers. To gain deeper insight into students’ strategies, it is recommended that qualitative semi-structured interviews be conducted to understand what distinguishes high-achieving students from their peers. Future studies should also explore differences between public and private university students. Additionally, further research is needed to confirm this study’s findings and provide guidance to all students. Future studies should collect a larger sample size from a variety of universities in order to increase generalizability.
Limitations and recommendations
The present study has some limitations. All the study’s findings indicated possible associations rather than causation; hence, the reader should approach the results of this study with caution. We recommend in-depth longitudinal studies to provide more insight into the different study habits and their impact on academic performance. Another limitation is that the research team created a self-reported questionnaire to address the study objectives, which carries a potential risk of bias. Hence, we recommend conducting interviews and having personal encounters with the study’s participants to reduce the risk of bias and better understand how different factors affect their academic achievement. A third limitation is that the research team only used the GPA scores as indicators of academic achievement. We recommend conducting other studies and investigating factors that cannot be solely reflected by the GPA, such as the student’s clinical performance and skills. Lastly, all participants included in the study share one background and live in the same environment. Therefore, the study’s findings do not necessarily apply to students who do not belong to such a geographic area and point in time. We recommend that future studies consider the sociodemographic and socioeconomic variations that exist among the universities in Saudi Arabia.
Availability of data materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
Grade Point Average
King Saud University
Institutional review board
Statistical package for the social sciences
Jafari H, Aghaei A, Khatony A. Relationship between study habits and academic achievement in students of medical sciences in Kermanshah-Iran. Adv Med Educ Pract. 2019;10:637–43.
Article Google Scholar
Abid N, Aslam S, Alghamdi AA, Kumar T. Relationships among students’ reading habits, study skills, and academic achievement in English at the secondary level. Front Psychol. 2023;14:1020269.
Abdulghani HM, Al-Drees AA, Khalil MS, Ahmad F, Ponnamperuma GG, Amin Z. What factors determine academic achievement in high achieving undergraduate medical students? A qualitative study. Med Teach. 2014;36(Suppl 1):S43–48.
Muntean LM, Nireștean A, Sima-Comaniciu A, Mărușteri M, Zăgan CA, Lukacs E. The relationship between personality, motivation and academic performance at Medical students from Romania. Int J Environ Res Public Health 2022, 19(15).
Reza HM, Alireza HJIJME. Investigating study Habits of Library and Information Sciences Students of Isfahan University and Isfahan University of Medical Sciences. 2014, 14:751–757.
Kurtz SM, Silverman JD. The Calgary-Cambridge Referenced Observation guides: an aid to defining the curriculum and organizing the teaching in communication training programmes. Med Educ. 1996;30(2):83–9.
Pun J, Kong B. An exploratory study of communication training for Chinese medicine practitioners in Hong Kong to integrate patients’ conventional medical history. BMC Complement Med Ther. 2023;23(1):10.
İlçin N, Tomruk M, Yeşilyaprak SS, Karadibak D, Savcı S. The relationship between learning styles and academic performance in TURKISH physiotherapy students. BMC Med Educ. 2018;18(1):291.
McKeirnan KC, Colorafi K, Kim AP, Stewart AS, Remsberg CM, Vu M, Bray BS. Study behaviors Associated with Student pharmacists’ academic success in an active Classroom Pharmacy Curriculum. Am J Pharm Educ. 2020;84(7):ajpe7695.
Jouhari Z, Haghani F, Changiz T. Assessment of medical students’ learning and study strategies in self-regulated learning. J Adv Med Educ Professionalism. 2016;4(2):72–9.
Google Scholar
Proctor BE, Prevatt FF, Adams KSS, Reaser A, Petscher Y. Study skills profiles of normal-achieving and academically-struggling College students. J Coll Student Dev. 2006;47(1):37–51.
Kyauta AMASY, Garba HS. The role of guidance and counseling service on academic performance among students of umar suleiman college of education, Gashua, Yobe State, Nigeria. KIU J Humanit. 2017;2(2):59–66.
Eva KW, Bordage G, Campbell C, Galbraith R, Ginsburg S, Holmboe E, Regehr G. Towards a program of assessment for health professionals: from training into practice. Adv Health Sci Education: Theory Pract. 2016;21(4):897–913.
Curcio G, Ferrara M, De Gennaro L. Sleep loss, learning capacity and academic performance. Sleep Med Rev. 2006;10(5):323–37.
Al Shawwa L, Abulaban AA, Abulaban AA, Merdad A, Baghlaf S, Algethami A, Abu-Shanab J, Balkhoyor A. Factors potentially influencing academic performance among medical students. Adv Med Educ Pract. 2015;6:65–75.
Ibrahim NK, Baharoon BS, Banjar WF, Jar AA, Ashor RM, Aman AA, Al-Ahmadi JR. Mobile Phone Addiction and its relationship to Sleep Quality and Academic Achievement of Medical students at King Abdulaziz University, Jeddah, Saudi Arabia. J Res Health Sci. 2018;18(3):e00420.
Alkhalaf AM, Tekian A, Park YS. The impact of WhatsApp use on academic achievement among Saudi medical students. Med Teach. 2018;40(sup1):S10–4.
Bonsaksen T, Brown T, Lim HB, Fong K. Approaches to studying predict academic performance in undergraduate occupational therapy students: a cross-cultural study. BMC Med Educ. 2017;17(1):76.
Alzahrani HA, Alzahrani OH. Learning strategies of medical students in the surgery department, Jeddah, Saudi Arabia. Adv Med Educ Pract. 2012;3:79–87.
Bin Abdulrahman KA, Khalaf AM, Bin Abbas FB, Alanazi OT. Study habits of highly effective medical students. Adv Med Educ Pract. 2021;12:627–33.
Jameel T, Gazzaz ZJ, Baig M, Tashkandi JM, Alharenth NS, Butt NS, Shafique A, Iftikhar R. Medical students’ preferences towards learning resources and their study habits at King Abdulaziz University, Jeddah, Saudi Arabia. BMC Res Notes. 2019;12(1):30.
Abdulghani HM, Alrowais NA, Bin-Saad NS, Al-Subaie NM, Haji AM, Alhaqwi AI. Sleep disorder among medical students: relationship to their academic performance. Med Teach. 2012;34(Suppl 1):S37–41.
Hwang G-J, Wang S-Y, Lai C-L. Effects of a social regulation-based online learning framework on students’ learning achievements and behaviors in mathematics. Comput Educ. 2021;160:104031.
Gamage KAA, Dehideniya D, Ekanayake SY. The role of personal values in learning approaches and student achievements. Behav Sci (Basel Switzerland) 2021, 11(7).
Linn Z, Tashiro Y, Morio K, Hori H. Peer evaluations of group work in different years of medical school and academic achievement: how are they related? BMC Med Educ. 2022;22(1):102.
Avonts M, Michels NR, Bombeke K, Hens N, Coenen S, Vanderveken OM, De Winter BY. Does peer teaching improve academic results and competencies during medical school? A mixed methods study. BMC Med Educ. 2022;22(1):431.
Topor DR, Keane SP, Shelton TL, Calkins SD. Parent involvement and student academic performance: a multiple mediational analysis. J Prev Interv Community. 2010;38(3):183–97.
Veas A, Castejón JL, Miñano P, Gilar-Corbí R. Relationship between parent involvement and academic achievement through metacognitive strategies: a multiple multilevel mediation analysis. Br J Educ Psychol. 2019;89(2):393–411.
Núñez JC, Regueiro B, Suárez N, Piñeiro I, Rodicio ML, Valle A. Student Perception of teacher and parent involvement in Homework and Student Engagement: the mediating role of motivation. Front Psychol. 2019;10:1384.
Abdulghani AH, Ahmad T, Abdulghani HM. The impact of COVID-19 pandemic on anxiety and depression among physical therapists in Saudi Arabia: a cross-sectional study. BMC Med Educ. 2022;22(1):751.
Park KH, Park JH, Kim S, Rhee JA, Kim JH, Ahn YJ, Han JJ, Suh DJ. Students’ perception of the educational environment of medical schools in Korea: findings from a nationwide survey. Korean J Med Educ. 2015;27(2):117–30.
Ahrberg K, Dresler M, Niedermaier S, Steiger A, Genzel L. The interaction between sleep quality and academic performance. J Psychiatr Res. 2012;46(12):1618–22.
Dikker S, Haegens S, Bevilacqua D, Davidesco I, Wan L, Kaggen L, McClintock J, Chaloner K, Ding M, West T, et al. Morning brain: real-world neural evidence that high school class times matter. Soc Cognit Affect Neurosci. 2020;15(11):1193–202.
Pittenger AL, Dimitropoulos E, Foag J, Bishop D, Panizza S, Bishop JR. Closing the Classroom Theory to practice gap by simulating a Psychiatric Pharmacy Practice Experience. Am J Pharm Educ. 2019;83(10):7276.
Walck-Shannon EM, Rowell SF, Frey RF. To what extent do Study habits relate to performance? CBE Life Sci Educ. 2021;20(1):ar6.
Abdulghani HM, Alanazi K, Alotaibi R, Alsubeeh NA, Ahmad T, Haque S. Prevalence of potential dropout thoughts and their influential factors among Saudi Medical Students. 2023, 13(1):21582440221146966.
Sleight DA, Mavis BE. Study skills and academic performance among second-Year Medical students in Problem-based learning. Med Educ Online. 2006;11(1):4599.
Download references
Acknowledgements
The authors are grateful to the Deanship of Scientific Research, King Saud University, for.
support through the Vice Deanship of Scientific Research Chairs.
Author information
Authors and affiliations.
Department of Psychiatry, College of Medicine, King Saud University, Riyadh, Saudi Arabia
Mohammed A. Aljaffer & Ahmad H. Almadani
College of Medicine, King Saud University, Riyadh, Saudi Arabia
Abdullah S. AlDughaither, Ali A. Basfar, Saad M. AlGhadir, Yahya A. AlGhamdi, Bassam N. AlHubaysh & Osamah A. AlMayouf
Department of Psychiatry, College of Medicine, Imam Mohammad Ibn Saud Islamic University, Riyadh, Saudi Arabia
Saleh A. AlGhamdi
Department of Medical Education, College of Medicine, King Saud University, P.O. Box: 230155, Riyadh, 11321, Saudi Arabia
Tauseef Ahmad
Department of Medical Education and Family Medicine, College of Medicine, King Saud University, Riyadh, Saudi Arabia
Hamza M. Abdulghani
You can also search for this author in PubMed Google Scholar
Contributions
Conception or design: AHA, MAA, and HMA. Acquisition, analysis, or interpretation of data: AAB, SMA, ASA, YAA, BNA, OAA and SAA. Drafting the work or revising: TA, AHA, ASA AAB. Final approval of the manuscript: MAA, HMA., AHA, and TA. The author(s) read and approved the final manuscript.
Corresponding author
Correspondence to Tauseef Ahmad .
Ethics declarations
Conflict of interest.
The Authors declare that they have no conflict of interest.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Human ethics and consent to participate declarations
Additional information, publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/ .
Reprints and permissions
About this article
Cite this article.
Aljaffer, M.A., Almadani, A.H., AlDughaither, A.S. et al. The impact of study habits and personal factors on the academic achievement performances of medical students. BMC Med Educ 24 , 888 (2024). https://doi.org/10.1186/s12909-024-05889-y
Download citation
Received : 26 September 2023
Accepted : 12 August 2024
Published : 19 August 2024
DOI : https://doi.org/10.1186/s12909-024-05889-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Medical students
- Study habits
- Academic achievement
- Saudi Arabia
BMC Medical Education
ISSN: 1472-6920
- General enquiries: [email protected]
Let’s Open Our Minds to the DOOR
This event has passed and can no longer be viewed.
This event was presented live or live-streamed and has not been designated for on-demand presentation.
This Neonatology Medical Literature Review session will take place on Thursday, March 12, 2024 at 12:00 p.m. Attendance will be available remotely through Zoom. Click here to receive CME credit: Attendees must complete the Session Evaluation .
Activity Information
Needs statement.
Physicians, residents, fellows, nurse practitioners, and other healthcare professionals involved in the care of neonates need to receive regular updates on the best strategies for reviewing, analyzing, and applying medical literature to clinical practice. The series aims to expand the knowledge of learners with regard to clinical epidemiology, biostatistics, and other research methodologies. The series also aims to review the most current research evidence related to neonatal disease processes, diagnostic and treatment modalities, quality of neonatal care, and improvement of patient outcomes.
Educational Objectives
At the conclusion of the session, the participants should be able to:
- List various cord management strategies and their implications in clinical practice.
- Analyze the findings of the Milking in Nonvigorous Infants (MINVI) trial.
- Summarize the advantages and challenges of using composite outcomes in clinical trials.
- Outline the design, outcomes, operation, and results (DOOR) approach to the analysis of clinical trials and apply it to MINVI trial results.
Target Audience
Professional categories.
- Medical Students
- Other Health Professionals
Specialties
Interest groups.
- Hospital Medicine
Accreditation/Credit Designation
Baylor College of Medicine is accredited by the Accreditation Council for Continuing Medical Education (ACCME) to provide continuing medical education for physicians.
Baylor College of Medicine designates this live activity for a maximum of 1.0 AMA PRA Category 1 Credit(s)™ . Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Activity Director
Michael e. speer, m.d., disclosure policy.
Baylor College of Medicine (BCM) is accredited by the Accreditation Council for Continuing Medical Education (ACCME) to provide continuing medical education (CME) for physicians. BCM is committed to sponsoring CE activities that are scientifically based, accurate, current, and objectively presented.
In accordance with the ACCME Standards for Commercial Support, BCM has implemented a mechanism requiring everyone in a position to control the content of an educational activity (i.e., directors, planning committee members, faculty) to disclose any relevant financial relationships with commercial interests (drug/device companies) and manage/resolve any conflicts of interest prior to the activity. Individuals must disclose to participants the existence or non-existence of financial relationships at the time of the activity or within 24 months prior.
In addition, BCM has requested activity faculty/presenters to disclose to participants any unlabeled use or investigational use of pharmaceutical/device products; to use scientific or generic names (not trade names) in referring to products; and, if necessary to use a trade name, to use the names of similar products or those within a class. Faculty/presenters have also been requested to adhere to the ACCME's validation of clinical content statements.
BCM does not view the existence of financial relationships with commercial interests as implying bias or decreasing the value of a presentation. It is up to participants to determine whether the relationships influence the activity faculty with regard to exposition or conclusions. If at any time during this activity you feel that there has been commercial/promotional bias, notify the Activity Director or Activity Coordinator. Please answer the questions about balance and objectivity in the activity evaluation candidly.
All of the relevant financial relationships listed for these individuals have been mitigated.
Disclosures
The following individual(s) has/have reported financial or other relationship(s) with commercial entities whose products/services may relate to the educational content of this activity:
Srirupa Hari Gopal, M.D.
Disclosure:.
Nothing to disclose.
- Intellectual Property: Wolters Kuwer Health: UpToDate®
Planning Committee Members
Faeq al-mudares, m.d., melissa mora carbajal, m.d., joseph l. hagan, sc.d., m.s.p.h., mohan pammi, m.d., ph.d..
- Intellectual Property: UpToDate® (Wolters Kuwer Health)
Amanda Zayek, M.D.
Health topics.
- Subscribe to this topic Unsubscribe from this topic

You May Also Be Interested In
- Sign In for Notifications
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Communicating with patients about medical errors: a review of the literature
Affiliation.
- 1 Meyers Primary Care Institute, University of Massachusetts Medical School, and Fallon Foundation, Worcester 01605, USA. [email protected]
- PMID: 15302641
- DOI: 10.1001/archinte.164.15.1690
Background: Ethical and professional guidelines recommend disclosure of medical errors to patients. The objective of this study was to review the empirical literature on disclosure of medical errors with respect to (1) the decision to disclose, (2) the process of informing the patient and family, and (3) the consequences of disclosure or nondisclosure.
Methods: We searched 4 electronic databases (MEDLINE, CINAHL, PsycINFO, and Social Sciences Citations Index) and the reference lists of relevant articles for English-language studies on disclosure of medical errors. From more than 800 titles reviewed, we identified 17 articles reporting original empirical data on disclosure of medical errors to patients and families. We examined methods and results of the articles and extracted study designs, data collection procedures, populations sampled, response rates, and definitions of error.
Results: Available research findings suggest that patients and the public support disclosure. Physicians also indicate support for disclosure, but often do not disclose. We found insufficient empirical evidence to support conclusions about the disclosure process or its consequences.
Conclusions: Empirical research on disclosure of medical errors to patients and families has been limited, and studies have focused primarily on the decision stage of disclosure. Fewer have considered the disclosure process, the consequences of disclosure, or the relationship between the two. Additional research is needed to understand how disclosure decisions are made, to provide guidance to physicians on the process, and to help all involved anticipate the consequences of disclosure.
PubMed Disclaimer
Similar articles
- How surgeons disclose medical errors to patients: a study using standardized patients. Chan DK, Gallagher TH, Reznick R, Levinson W. Chan DK, et al. Surgery. 2005 Nov;138(5):851-8. doi: 10.1016/j.surg.2005.04.015. Surgery. 2005. PMID: 16291385
- Health plan members' views on forgiving medical errors. Mazor KM, Simon SR, Yood RA, Martinson BC, Gunter MJ, Reed GW, Gurwitz JH. Mazor KM, et al. Am J Manag Care. 2005 Jan;11(1):49-52. Am J Manag Care. 2005. PMID: 15697100
- Disclosure of medical error: is it worth the risk? Straumanis JP. Straumanis JP. Pediatr Crit Care Med. 2007 Mar;8(2 Suppl):S38-43. doi: 10.1097/01.PCC.0000257736.34737.2D. Pediatr Crit Care Med. 2007. PMID: 17496831
- Bioethics for clinicians: 23. Disclosure of medical error. Hébert PC, Levin AV, Robertson G. Hébert PC, et al. CMAJ. 2001 Feb 20;164(4):509-13. CMAJ. 2001. PMID: 11233873 Free PMC article. Review.
- Disclosure of CAM use to medical practitioners: a review of qualitative and quantitative studies. Robinson A, McGrail MR. Robinson A, et al. Complement Ther Med. 2004 Jun-Sep;12(2-3):90-8. doi: 10.1016/j.ctim.2004.09.006. Complement Ther Med. 2004. PMID: 15561518 Review.
- Disclosure following a medical error: lessons learned from a national initiative of workshops with patients, healthcare teams, and executives. Finkelstein A, Brezis M, Taub A, Arad D. Finkelstein A, et al. Isr J Health Policy Res. 2024 Mar 11;13(1):13. doi: 10.1186/s13584-024-00599-8. Isr J Health Policy Res. 2024. PMID: 38462624 Free PMC article.
- Reasoning on Rounds: a Framework for Teaching Diagnostic Reasoning in the Inpatient Setting. Penner JC, Shipley LC, Minter DJ. Penner JC, et al. J Gen Intern Med. 2023 Oct;38(13):3041-3046. doi: 10.1007/s11606-023-08359-1. Epub 2023 Aug 14. J Gen Intern Med. 2023. PMID: 37580633
- Strengthening open disclosure after incidents in maternity care: a realist synthesis of international research evidence. Adams M, Hartley J, Sanford N, Heazell AE, Iedema R, Bevan C, Booker M, Treadwell M, Sandall J. Adams M, et al. BMC Health Serv Res. 2023 Mar 27;23(1):285. doi: 10.1186/s12913-023-09033-2. BMC Health Serv Res. 2023. PMID: 36973796 Free PMC article.
- Defining Objective Measures of Physician Stress in Simulated Critical Communication Encounters. Wolfe AHJ, Hinds PS, du Plessis AJ, Gordish-Dressman H, Arnold RM, Soghier L. Wolfe AHJ, et al. Crit Care Explor. 2022 Jun 30;4(7):e0721. doi: 10.1097/CCE.0000000000000721. eCollection 2022 Jul. Crit Care Explor. 2022. PMID: 35795402 Free PMC article.
- Empirical Investigation on the Characteristics and Perceived Value of Patients in Medical Treatment Seeking: In-Depth Research in Zhejiang Province of China. Qian H, Lu W, Zhang D. Qian H, et al. Biomed Res Int. 2021 Dec 24;2021:5245041. doi: 10.1155/2021/5245041. eCollection 2021. Biomed Res Int. 2021. Retraction in: Biomed Res Int. 2023 Dec 29;2023:9758574. doi: 10.1155/2023/9758574. PMID: 34977240 Free PMC article. Retracted.
Publication types
- Search in MeSH
Related information
- Cited in Books
Grants and funding
- U18HS10391-01/HS/AHRQ HHS/United States
- U18HS11843-01/HS/AHRQ HHS/United States
LinkOut - more resources
Full text sources.
- Ovid Technologies, Inc.
- Silverchair Information Systems
- MedlinePlus Health Information
- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.

IMAGES
COMMENTS
Medical errors include errors in diagnosis ("diagnostic errors"), errors in the administration of drugs and other medications ("medication errors"), errors in the performance of surgical procedures, in the use of other varieties of therapy, in the use of equipment, and the interpretation of laboratory findings. [ 1, 2, 3] It is critical ...
Abstract. Objective: Medical errors represent a leading cause of patient morbidity and mortality. The aim of this study was to quantitatively analyze the existing scientific literature on medical errors in order to gain new insights in this important medical research area. Study Design: Web of Science database was used to identify relevant ...
However, the aim of this review is to provide a summary of medication errors reporting culture, incidence reporting systems, creating effective reporting methods, analysis of medication error reports, and recommendations to improve medication errors reporting systems.
Better preparing nurses to safely fulfil the task of medication administration in the clinical environment, with increased confidence in the face of interruptions, could lead to a reduction in errors and concomitant improvements to patient safety.
Background and Aims: Medication errors occur at any point of the medication management process, and are a major cause of death and harm globally. The objective of this review was to compare the effectiveness of different interventions in reducing prescribing, dispensing and administration medication errors in acute medical and surgical settings.
This narrative review aimed to explore the impact of checklists and error reporting systems on hospital patient safety and medical errors.A systematic…
We identified such interventions. Methods: We conducted a systematic review of systematic reviews by searching four databases (PubMed, Scopus, Ovid Medline, and Embase) until January 2021 to elicit interventions that have the potential to decrease medical errors. Two reviewers independently conducted data extraction and analyses.
Several primary studies and systematic reviews have explored factors contributing to medication errors. Given the plethora of systematic reviews investigating contributory factors to medication errors, there is a need to identify, critically appraise, and synthesize these factors via an umbrella review.
Conclusions Medication errors are classified based on multifaceted criteria and there is a need to standardize the recommendations and make them a central goal all over the globe for the best practice. Nurses are the frontlines of clinical settings, encouraged to be one integrated body to prevent the occurrence of medication errors.
Underreporting of medical errors is a common and a challenging obstacle in the fight for patient safety. The goal of this study is to review common barriers to reporting medical errors. Methods. We systematically reviewed the literature by searching the MEDLINE and SCOPUS databases for studies on barriers to reporting medical errors.
Medical errors are a substantial problem in health care. Understanding the effect of medical errors on health care providers as the "second victims" is necessary to maintain safe, quality patient care for the good of both patients and providers. We report an integrative literature review of the effe …
Abstract. Background: Medical errors are one of the most important quality problems in health care today. The best insight into the incidences and characteristics of medical errors is through studies on adverse events (AEs) since a considerable fraction of AEs are results of errors and as such preventable. Even though prevention is where effort ...
The review also found four leadership actions - regular checks on the front line and promoting teamwork, psychological safety and open communication - associated with successful outcomes. The review concluded that leadership appeared to be the preeminent factor in reducing medical errors and improving patient safety.
Background Ethical and professional guidelines recommend disclosure of medical errors to patients. The objective of this study was to review the empirical literature on disclosure of medical errors with respect to (1) the decision to disclose, (2) the process of informing the patient and...
Medical errors have more recently been recognized as a serious public health problem, reported as the third leading cause of death in the US.[1] However, because medical errors are comprised of different types of failures (eg, diagnostic or medication errors) that can result in various outcomes (eg, near-miss, injury, or no harm), estimates of the incidence of medical errors vary widely in ...
Thus, this narrative review aims to analyze and describe the relationship between medical errors, medical negligence, and the practice of D.M.
Chapte r 2. Medication-Relate d Errors: A Literature Review of. Incidenc e and Antecedents. Gay a Carlton and Mary A. Blegen. ABSTRAC T. Patient safety has become a major concern for both society ...
Keywords: literature review, medication errors, patient safety Study search and selection flow Percentage of Medication Errors Occurrence
Diagnostic errors are associated with patient harm and suboptimal outcomes. Despite national scientific efforts to advance definition, measurement and interventions for diagnostic error, diagnosis in mental health is not well represented in this ongoing work. We aimed to summarise the current state of research on diagnostic errors in mental health and identify opportunities to align future ...
Background: Diagnostic errors are an underappreciated cause of preventable mortality in hospitals and pose a risk for severe patient harm and increase hospital length of stay. Objective: This study aims to explore the potential of machine learning and natural language processing techniques in improving diagnostic safety surveillance. We conducted a rigorous evaluation of the feasibility and ...
The phrase medical errors is an umbrella term for all errors that occur within the health care system, including mishandled surgeries, diagnostic errors, equipment failures, and medication errors. This article is a review and discussion of the literature on the scope of medical errors, with a focus on drug-related problems and medication errors.
Objective: This systematic literature review aims to identify barriers and facilitators to the implementation of digital health services for people with musculoskeletal conditions in the primary health care setting. Methods: PubMed, Embase, and CINAHL were searched for eligible qualitative and mixed methods studies up to March 2024.
The phrase medical errors is an umbrella term for all errors that occur within the health care system, including mishandled surgeries, diagnostic errors, equipment failures, and medication errors. This article is a review and discussion of the literature on the scope of medical errors, with a focus on drug-related problems and medication errors.
An important contribution of the research is the use of data from medical records, containing multiple information from investigations and visits, compared to most studies in the literature that ...
Equipment errors: Medical equipment design flaws, mishandling, user error, and malfunction are common causes of medical errors. Additionally, a significant number of medical devices have been implanted in patients (eg, pacemakers, defibrillators, and nerve and brain stimulators), which may malfunction and result in life-threatening complications.
A systematic literature review was performed to identify trials that assessed the efficacy and safety of interventions used in patients that progressed on prior ARAT therapies. A literature search was conducted using the OVID platform that searched the EMBASE, MEDLINE, and CENTRAL bibliographic databases.
A robust peer review and quality assurance (QA) process serves as a cornerstone of healthcare litigation defense, providing a critical layer of protection against medical malpractice claims. This process ensures that healthcare providers are held to high standards of care and that any deviations from these standards are identified and addressed ...
Background Academic achievement is essential for all students seeking a successful career. Studying habits and routines is crucial in achieving such an ultimate goal. Objectives This study investigates the association between study habits, personal factors, and academic achievement, aiming to identify factors that distinguish academically successful medical students. Methods A cross-sectional ...
This Neonatology Medical Literature Review session will take place on Thursday, March 12, 2024 at 12:00 p.m. Attendance will be available remotely through Zoom. ... and applying medical literature to clinical practice. The series aims to expand the knowledge of learners with regard to clinical epidemiology, biostatistics, and other research ...
Abstract Background: Ethical and professional guidelines recommend disclosure of medical errors to patients. The objective of this study was to review the empirical literature on disclosure of medical errors with respect to (1) the decision to disclose, (2) the process of informing the patient and family, and (3) the consequences of disclosure or nondisclosure.