Search by category
Popular searches.


Eating disorder case study

Discover another eating disorder recovery story
"eating disorders tend to hide and they don't want to be seen, and if somebody else can see it ... it's a lot harder to hide".

Contact us to make an enquiry or for more information
Antonella: ‘A Stranger in the Family’—A Case Study of Eating Disorders Across Cultures
- Open Access
- First Online: 12 December 2020
Cite this chapter
You have full access to this open access chapter

- Vincenzo Di Nicola 6 , 7
8115 Accesses
2 Citations
7 Altmetric
The story of Antonella illustrates the way in which cultural and other values impact on the presentation and treatment of eating disorders. Displaced from her European home culture to live in Canada, Antonella presents with an eating disorder and a fluctuating tableau of anxiety and mood symptoms linked to her lack of a sense of identity. These arose against a background of her adoption as a foundling child in Italy and her attachment problems with her adoptive family generating chronically unfixed and unstable identities, resulting in her cross-cultural marriage as both flight and refuge followed by intense conflicts. Her predicament is resolved only when after an extended period in cultural family therapy she establishes a deep cross-species identification by becoming a breeder of husky dogs. The wider implications of Antonella’s story for understanding the relationship between cultural values and mental health are briefly considered.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others

Overlaps and Disjunctures: A Cultural Case Study of a British Indian Young Woman’s Experiences of Bulimia Nervosa
René girard and the mimetic nature of eating disorders, the rise of eating disorders in asia: a review.
- Eating disorders
- Anorexia multiforme
- Cultural values
- Uniqueness of the individual
- Role of animals
- Cross-species identification
- Cultural family therapy
1 Introduction
Eating disorders are a potentially fruitful area of study for understanding the links between values—in particular cultural values—and mental distress and disorder. Eating disorders show widely different prevalence rates across cultures, and much attention has been given to theories linking these differences with variations in cultural values. In particular, the cultural value placed on ‘fashionable slimness’ in the industrialised world has for some time been identified with the greater prevalence of eating disorders among women in Western societies [ 1 ]. Consistently with this view, the growing prevalence of eating disorders in other parts of the world does seem to be correlated with increasing industrialisation [ 2 , 3 ]. In my review of cultural distribution and historical evolution of eating disorders , I was so struck by its protean nature and its variability of clinical presentations of anorexia nervosa that I renamed this predicament ‘anorexia multiforme’ [ 4 , 5 ].
The story of Antonella that follows illustrates the potential importance of contemporary theories linking cultural values with eating disorders though also some of their limitations.
2 Case Narrative: Antonella’s Story
Ottawa in the early 1990s. Antonella Trevisan, a 24-year-old woman, was referred to me by an Italian psychiatrist and family therapist, Dr. Claudio Angelo, who had treated her in Italy [ 6 ] . When Antonella came to Canada to live with a man she had met through her work, Dr. Angelo referred her to me. Antonella’s presenting problems concerned two areas of her life: her eating problems, which emerged after her emigration from Italy, and her relationship with her partner in Canada.
2.1 Antonella’s Predicament
My initial psychiatric consultation (conducted in Italian) revealed the complexities of Antonella’s life. This was reflected in the difficulty of making an accurate diagnosis. Her food-related problems had some features of eating disorders , such as restriction of intake, the resulting weight loss, and a history of weight gain and being teased for it. What was missing was the ‘psychological engine’ of an eating disorder: a drive for thinness or a morbid fear of fatness. Her problem was perhaps better understood as a food-related anxiety arising from a ‘globus’ sensation (lump in the throat) and a learned avoidance response that generalized from one specific situation to eating in any context.
Although it was clear that her weight gain in late adolescence and the teasing and insults from her mother had sensitized her, other factors had to be considered. Antonella showed an exquisite rejection sensitivity that both arose from and was a metaphor for the circumstances of her birth and adoption. Her migration to Canada also seemed to generate anxieties and uncertainties, and there were hints of conflicts with her partner. Was she also re-enacting another, earlier trauma? In the first journey of her life, she was given up by her birth mother (or taken away?) and left on the steps of a foundry. In the first year of her life, Antonella had shown failure to thrive and developmental delays. And she had, at best, an insecure attachment to her adoptive family, predisposing her to lifelong insecurities.
2.2 A Therapeutic Buffet
After my assessment, we faced a choice: whether to treat the eating problem concretely, in purely behavioral terms, or more metaphorically, with some form of psychotherapy. Given the stabilization of her eating pattern and her weight and the larger context of her predicament, we negotiated to do psychotherapy. There were several components to her therapy. Starting with a psychiatric consultation, three types of therapy were negotiated, with Antonella sampling a kind of ‘therapeutic buffet’ over a period of some 2 years: individual therapy for Antonella, couple therapy for Antonella and Rick, and brief family therapy with Antonella’s adoptive family visiting from Italy.
The individual work with Antonella was at first exploratory, getting to know the complex bicultural world of the Italian Alps, how she experienced the move to Canada, examining her choices to move here and live with Rick. Sessions were conducted in a mix of Italian and English. At first, the Italian language was like a ‘transitional object’ in her acculturation process; slowly, as she gained confidence in her daily life, English began to dominate her sessions. Under stress, however, she would revert to Italian. I could follow her progress just by noting the balance of Italian and English in each session. This does not imply any superiority of English or language preferences; rather, it acknowledges the social realities of culture making its demands felt even in private encounters. This is the territory of sociolinguistics [ 7 , 8 ] . Like Italian, these individual sessions were a secure home base to which Antonella returned during times of stress or between other attempts to find solutions.
After some months in Canada and the stabilization of her eating problems, Antonella became more invested in examining her relationship to Rick. They had met through work while she was still in Italy. After communicating on the telephone, she daringly took him up on an offer to visit. During her holiday in Canada, a romance developed. After her return to Italy, Antonella made the extraordinary decision to emigrate, giving up an excellent position in industry, leaving her family for a country she did not know well. Rick is 22 years her senior and was only recently separated from his first wife.
In therapy she not only expressed ambivalence about her situation with Rick but enacted it. She asked for couple sessions to discuss some difficulties in their relationship. Beyond collecting basic information, couple sessions were unproductive. While Rick was frank about his physical attraction to her and his desire to have children, Antonella talked about their relationship in an oddly detached way. She could not quite articulate her concerns. As we got closer to examining the problems of their relationship, Antonella abruptly announced that they were planning their wedding. The conjoint sessions were put on hold as they dealt with the wedding arrangements.
Her parents did not approve of the marriage and boycotted the wedding. Her paternal aunt, however, agreed to come to Canada for the wedding. Since I was regarded by Antonella as part of her extended family support system, she brought her aunt to meet me. It gave me another view of Antonella’s family. Her aunt was warm and supportive of Antonella, trying to smooth over the family differences. A few months later, at Christmas time, her parents and sister visited, and Antonella brought them to meet me. To understand these family meetings, however, it is necessary to know Antonella’s early history.
2.3 A Foundling Child
Antonella was a foundling child. Abandoned on the steps of a foundry in Turin as a newborn, she was the subject of an investigation into the private medical clinics of Turin. This revealed that the staff of the clinic where she was born was ‘paid off to hide the circumstances of my birth.’ As a result, her date of birth could only be presumed because the clinic staff destroyed her birth records. She was taken into care by the state and, as her origins could not be established, she was put up for adoption.
Antonella has always tried to fill in this void of information with meaning that she draws from her own body. She questions me closely: ‘Just look at me. Don’t you think I look like a Japanese?’ She feels that her skin tone is different from other Italians, that her facial features and eyes have an ‘Asian’ cast. With a few, limited facts, and some speculation, she has constructed a personal myth: that she is the daughter of an Italian mother from a wealthy family (hence her hidden birth in a private clinic) and a Japanese father (hence her ‘Asian’ features). It is oddly reassuring to her, but also perhaps a source of her alienation from her family.
At about 6 months of age, Antonella was adopted into a family in the Italian Alps, near the border with Austria. This is a bicultural region where both Italian and German are spoken and services are available in both languages (much like Ottawa, which is bilingually English and French). Her father, Aldo, who is Italian, is a retired FIAT factory worker. Annalise, her mother, who is a homemaker, had an Italian father and an Austrian mother. About her family she said, ‘I had a wonderful childhood compared to what came afterwards.’ Years after her adoption, her parents had a natural child, Oriana, who is 15.
She describes her mother as the disciplinarian at home. Her mother, she said, was ‘tough, German.’ When she visited her Austrian grandmother, no playing was allowed in that strict home. Her own mother allowed her ‘no friends in the house,’ but her father ‘was my pal when I was a kid.’ Although she had a good relationship with her father, he became ‘colder’ when she turned 13. Her parents’ relationship is remembered as cordial, but she later learned that they had many marital problems. Mother told her that she married to get away from home, but in fact she was in love with someone else. Overall, the feeling is of a rigid family organization. Her father is clearly presented by Antonella as warmer and more sociable. She experiences her mother as being ‘tough’. But she is crying all the time, feeling betrayed by everybody.
2.4 A Family Visit from the Italian Alps
When her family finally came to visit, Antonella brought them to see me. At first, the session had the quality of a student introducing out-of-town parents to her college teacher. They were pleased that I spoke Italian and knew Dr. Angelo, who they trusted. I soon found that the Trevisans were hungry to tell their story. Instead of a social exchange of pleasantries, this meeting turned into the first session of an impromptu course of brief family therapy.
Present were Antonella’s parents, Aldo and Annalise, and her sister, Oriana. Annalise led the conversation. Relegating Aldo to a support role. Oriana alternated between disdain and agitation, punctuated by bored indifference. Annalise had much to complain about: her own troubled childhood, her sense of betrayal and abandonment, heightened by Antonella’s departure from the family and from Italy. I was struck by the parallel themes of abandonment in mother and daughter. Mother clearly needed to tell this story, so I tried to set the stage for the family to hear her, what narrative therapists call ‘recruiting an audience’ [ 9 ] . I used Antonella, who I knew best, as a barometer of the progress of the session, and by that indicator, believed it had gone well.
When I saw them again some 10 days later, I was stunned by the turn of events. Oriana had assaulted her parents. The father had bandages over his face and the mother had covered her bruises with heavy make-up and dark glasses. Annalise was very upset about Oriana, who was defiant and aggressive at home. For her part, Oriana defended herself by saying she had been provoked and hit by her mother. Worried by this dangerous escalation, I tried to open some space for a healthy standoff and renegotiation.
Somehow, the concern had shifted away from Antonella to Oriana. Antonella was off the hook, but I waited for an opening to deal with this. I first tried to explore the cultural attitudes to adolescence in Italy by asking how the Italian and the German subcultures in their area understood teenagers differently. What were Oriana’s concerns? Had they seen this outburst coming? The whole family participated in a kind of sociological overview of Italian adolescence, with me as their grateful audience. The parents demonstrated keen insight and empathy. Concerned about Oriana’s experience of the session, I made a concerted effort to draw her into it. Eventually, the tone of the session lightened. Knowing they would return to Italy soon, I explored whether they had considered family work. Since they had met a few times with Dr. Angelo over Antonella’s eating problems, they were comfortable seeing Dr. Angelo as a family to find ways to understand Oriana and her concerns and for Oriana to explore other, nonviolent ways to be heard in the family. I agreed to meet them again before their departure and to communicate with Dr. Angelo about their wishes. On their way out, I wondered aloud about the apparent switch in their focus from Antonella to Oriana. The parents reassured me that they were ready to let Antonella live her own life now.
When they returned to say goodbye, we had a brief session. Oriana and Antonella were oddly buoyant and at ease. The parents were relieved. Antonella had offered the possibility of Oriana returning to spend the summer in Canada with her. I tried to connect this back to the previous session, wondering how much the two sisters supported each other. I was delighted, I said emphatically, by the family’s apparent approval of Antonella’s marriage to Rick. It was striking that, even from a distance of thousands of miles away, Antonella was still a part of the Trevisan family. And Rick was still not in the room.
3 Discussion
In this section, I will consider the impact of cultural and other values on Antonella and those around her and then look briefly at the wider implications of her story for our understanding not only of eating disorders but of mental distress and disorders in general.
3.1 Antonella: Life Before Man
The key to understanding Antonella’s attachments was her passion for her Siberian huskies. In the language of values-based practice , it was above all her huskies that mattered or were important to her. And it is not hard to see why. From the beginning of her relationship with Rick, she used her interest in dogs as a way for them to be more socially active as a couple, getting them out of the house to go to dog shows, for example. As her interests expanded, she wanted to buy bitches for breeding and to set up a kennel. Rick was only reluctantly supportive in this. Nonetheless, they ended up buying a home in the country where she could establish a kennel. Her haggling with Rick over the dogs was quite instrumental on her part, representing her own choices and interests and a test of the extent to which Rick would support her.
Yet the importance to Antonella of her huskies rests I believe on deeper cultural factors, both negative and positive. As to negative factors , these are evident in the fact that from the first days of her life, Antonella was rejected by her birth parents, literally abandoned and exposed, and later adopted by what she experienced as a non-nurturing family. Positive cultural factors , on the other hand, are evident in the way that having thrown her net wider afield, she looked initially to Canada, and to Rick, for nurturance and for identity. Then, finding herself only partly satisfied, she turned to the nonhuman world for the constancy of affection she could not find with people. Her huskies gave her pleasure, a task, and an identity. She spent many sessions discussing their progress, showing me pictures of her dogs and their awards. As it happened, my secretary at the time was also a dog lover who raised Samoyed dogs (related to huskies) and the two of them exchanged stories of dog lore.
As to positive factors , again, is there something, too, in the mythology of Canada that helps us understand Antonella? Does Canada still hold a place in the European imagination as a ‘New World’ for radical departures and identity makeovers? Or does Canada specifically represent the ‘malevolent North,’ as Margaret Atwood [ 10 ] calls it in her exploration of Canadian fiction? Huskies are a Northern animal, close to the wolf in their origins and habits. Bypassing the human world, Antonella finds her identity within a new world through its animals. If people have failed her, then she will leave not only her own tribe (Italy), but skip the identification with Canada’s Native peoples, responding to the ‘call of the wild’ to identify with a ‘life before man’ (to use another of Atwood’s evocative phrases, [ 11 ]), finding companionship and solace with her dogs.
3.2 Wider Implications of Antonella’s Story
Antonella may seem on first inspection something of an outlier to the human tribe. Orphaned from her culture of origin, she finds her place not in another country but by identification with another and altogether wilder species, her husky dogs. Yet, understood through the lens of values-based practice Antonella’s story has, I believe, wider significance at a number of levels.
First, Antonella’s story is significant for our understanding of the role of values – of what is important or matters to the individual concerned – in the presentation and treatment of eating disorders , and, by extension, of perhaps many other forms of mental distress and disorder. Specifically, her story provides at least one clear ‘proof of principle’ example supporting the role of cultural values.
As noted in my introduction, much attention has been given in the literature to the correlations between the uneven geographical distribution of eating disorders and cultural values. Correlations are of course no proof of causation. But in Antonella’s story at least the role of cultural values seems clearly evident. They were key to understanding her presenting problems. And this understanding in turn proved to be key to the cultural family therapy [ 12 ] through which these problems were, at least to the extent of her presenting eating disorder, resolved.
The cultural values involved, it is true, were not those of fashionable slimness so widely discussed in the literature. But this takes us to a second level at which Antonella’s story has wider significance. For it shows that to the extent that cultural values are important in eating disorders , their importance plays out at the level of individually unique persons. In this sense, social stresses and cultural values are played out in the body of the individual suffering with an eating disorder, making her body the ‘final frontier’ of psychiatric phenomenology [ 13 ]. Yes, there are no doubt valid cultural generalisations to be made about eating disorders and mental disorders of other kinds. And yes, these generalisations no doubt include generalisations about cultural values—about things that matter or are important to this or that group of people as a whole. Yet, this does not mean that we can ignore the values of the particular individual concerned. It has been truly said in values-based practice that as to their values, everyone is an ‘ n of 1’ [ 14 ]. Antonella, then, in the very idiosyncrasies of her story, reminds us of the idiosyncrasies of the stories of each and every one of us, whatever the culture or cultures to which we belong.
Antonella’s identification with animals , furthermore, to come to yet another level at which her story has wider significance, was a strongly positive factor in her recovery. As with other areas of mental health, it is with the negative impact of cultural values that the literature has been largely concerned: the pathogenetic influences of cultural values of slimness being a case in point in respect of eating disorders . Antonella’s story illustrates what has been clear for some time in the ‘recovery movement’, that positive values are often the very key to recovery. Not only that, but as Antonella’s passion for her husky dogs illustrates, the particular positive values concerned may, and importantly often are, individually unique.
Not, it is worth adding finally, that Antonella’s values were in this respect entirely unprecedented. Animals , after all, are widely valued, positively and negatively, and for many different reasons, in many cultures [ 11 ]. Their healing powers are indeed acknowledged. Just how far these powers depend on the kind of cross-species identification shown by Antonella, remains a matter for speculation. But, again, her story even in this respect is far from unique. Elsewhere, I have described the story of a white boy with what has become known as the ‘Grey Owl Syndrome’ , wishing to be native [ 12 , chapter 5 ]. Similarly, in Bear , Canadian novelist Marion Engel [ 15 ] portrays Lou, a woman who lives in the wilderness and befriends a bear. Lou seeks her identity from him: ‘Bear, make me comfortable in the world at last. Give me your skin’ [ 15 , p. 106]. After some time with the bear, the woman changes: ‘What had passed to her from him she did not know…. She felt not that she was at last human, but that she was at last clean’ [ 15 , p. 137]. It was perhaps to some similarly partial resolution that Antonella came.
4 Conclusions
Antonella’s story as set out above goes to the heart of the importance of cultural values in mental health. Her presenting eating disorder develops when, displaced from her culture of origin in Italy, and in effect rejected by her birth family, she finds healing only through cross-species identification with the wildness of husky dogs in her adoptive country of Canada. Although somewhat unusual in its specifics, her story illustrates the importance of cultural values at a number of levels in the presentation and management of eating and other forms of mental distress disorder.
And Antonella? I met her again in a gallery in Ottawa, rummaging through old prints. She was asking about prints of dogs; I was looking for old prints of Brazil where my father had made a second life. How was she, I asked? ‘Well …,’ she said hesitantly. Was that a healthy ‘well’ or the start of an explanation? ‘Me and Rick are splitting up,’ she said without ceremony, ‘but I still have the huskies.’ For each of us, the prints represented another world of connections.
Makino M, Tsuboi K, Denerson L. Prevalence of eating disorders: a comparison of Western and non-Western countries. MedGenMed. 2004;6(3):49. Published online 2004 Sep 27 at: https://www.ncbi.nlm.nih.gov/pubmed .
PubMed PubMed Central Google Scholar
Erskine HE, Whiteford HA, Pike KM. The global burden of eating disorders. Curr Opin Psychiatry. 2016;29(6):346–53.
Article Google Scholar
Selvini Palazzoli M. Anorexia nervosa: a syndrome of the affluent society. Transcult Psychiatr Res Rev. 1985;22( 3 ):199–205.
Google Scholar
Di Nicola VF. Overview: anorexia multiforme: self-starvation in historical and cultural context. I: self-starvation as a historical chameleon. Transcult Psychiatr Res Rev. 1990;27(3):165–96.
Di Nicola VF. Overview: anorexia multiforme: self-starvation in historical and cultural context. II: anorexia nervosa as a culture-reactive syndrome. Transcult Psychiatr Res Rev. 1990;27(4):245–86.
Andolfi M, Angelo C, de Nichilo M. The myth of atlas: families and the therapeutic story. Edited & translated by Di Nicola VF. New York: Brunner-Routledge; 1989.
Douglas M. Humans speak. Ch 11. In: Implicit meanings: essays in anthropology. London: Routledge & Kegan Paul; 1975. p. 173–80.
Crystal D. The Cambridge encyclopedia of language. Cambridge: Cambridge University Press; 1987.
Parry A, Doan RE. Story re-visions: narrative therapy in the postmodern world. New York: Guilford Press; 1995.
Atwood M. Strange things: the malevolent north in Canadian literature. Oxford: Oxford University Press; 1995.
Atwood M. Life before man: a novel. New York: Anchor Books; 1998.
Di Nicola VF. A stranger in the family: culture, families, and therapy. New York: W.W. Norton & Co.; 1997.
Nasser M, Di Nicola V. Changing bodies, changing cultures: an intercultural dialogue on the body as the final frontier. Ch 9. In: Nasser M, Katzman MA, Gordon RA, editors. Eating disorders and cultures in transition. East Sussex: Brunner-Routledge; 2001. p. 171–93.
Fulford KWM, Peile E, Carroll H. A smoking enigma: getting and not getting the knowledge. Ch 6. In: Fulford KWM, Peile E, Carroll H, editors. Essential values-based practice: clinical stories linking science with people. Cambridge: Cambridge University Press; 2012. p. 65–82.
Chapter Google Scholar
Engel M. Bear: a novel. Toronto: Emblem (Penguin Random House Books); 2009.
Download references
Acknowledgements
The story of Antonella was first published in reference [ 12 ] (pp. 214–220) and presented at the Advanced Studies Seminar of the Collaborating Centre for Values-based Practice in Health and Social Care at St Catherine’s College, Oxford in October 2019. The names and other details of the case have been altered to maintain confidentiality. Parts of the discussion are adapted from that publication and the Oxford seminar. I am grateful to the publishers for permission to reproduce these materials here and to Professor Fulford and the members of the Advanced Studies Seminar for their stimulating exchanges. The subheading to the discussion of Antonella’s story (‘Life before Man’) was inspired by Margaret Atwood’s novel, Life Before Man [ 11 ].
Author information
Authors and affiliations.
Canadian Association of Social Psychiatry (CASP), World Association of Social Psychiatry (WASP), Department of Psychiatry and Addictions, University of Montreal, Montreal, QC, Canada
Vincenzo Di Nicola
Department of Psychiatry and Behavioral Sciences, The George Washington University, Washington, DC, USA
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Vincenzo Di Nicola .
Editor information
Editors and affiliations.
Medical University Plovdiv, Plovdiv, Bulgaria
Drozdstoy Stoyanov
St Catherine’s College, University of Oxford, Oxford, UK
Bill Fulford
Department of Psychological, Health & Territorial Sciences, “G. D’Annunzio” University, Chieti Scalo, Italy
Giovanni Stanghellini
Centre for Ethics and Philosophy of Health Sciences, University of Pretoria, Pretoria, South Africa
Werdie Van Staden
Department of Psychiatry, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Hong Kong, China
Michael TH Wong
Guide to Further Sources
For a more extended treatment of the role of culture in eating disorders and family therapy see:
Di Nicola VF (1990a) Overview: Anorexia multiforme: Self-starvation in historical and cultural context. I: Self-starvation as a historical chameleon. Transcultural Psychiatric Research Review, 27(3): 165–196.
Di Nicola VF (1990b) Overview: Anorexia multiforme: Self-starvation in historical and cultural context. II: Anorexia nervosa as a culture-reactive syndrome. Transcultural Psychiatric Research Review, 27(4): 245–286.
Di Nicola, V (1997) A Stranger in the Family: Culture, Families, and Therapy . New York & London: W.W. Norton & Co.
Nasser M and Di Nicola, V. (2001) Changing bodies, changing cultures: An intercultural dialogue on the body as the final frontier. In: Nasser M, Katzman M A, and Gordon R A, eds. Eating Disorders and Cultures in Transition . East Sussex, UK: Brunner-Routledge, pp. 171–193.
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Reprints and permissions
Copyright information
© 2021 The Author(s)
About this chapter
Di Nicola, V. (2021). Antonella: ‘A Stranger in the Family’—A Case Study of Eating Disorders Across Cultures. In: Stoyanov, D., Fulford, B., Stanghellini, G., Van Staden, W., Wong, M.T. (eds) International Perspectives in Values-Based Mental Health Practice. Springer, Cham. https://doi.org/10.1007/978-3-030-47852-0_3
Download citation
DOI : https://doi.org/10.1007/978-3-030-47852-0_3
Published : 12 December 2020
Publisher Name : Springer, Cham
Print ISBN : 978-3-030-47851-3
Online ISBN : 978-3-030-47852-0
eBook Packages : Medicine Medicine (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
BRIEF RESEARCH REPORT article
Toward a biological, psychological and familial approach of eating disorders at onset: case-control anobas study.

- 1 Department of Biological and Health Psychology, School of Psychology, Autonomous University of Madrid, Madrid, Spain
- 2 Department of Cognitive Psychology, School of Psychology, Autonomous University of Madrid, Madrid, Spain
- 3 Immunonutrition Research Group, Department of Metabolism and Nutrition, Institute of Food Science, Technology and Nutrition (ICTAN), Spanish National Research Council (CSIC), Madrid, Spain
- 4 Pediatric Pneumology, Niño Jesús University Children’s Hospital, Madrid, Spain
- 5 Psychiatry Service, Hospital Universitario del Sureste, Arganda del Rey, Spain
- 6 Department of Child and Adolescent Psychiatry and Psychology, Niño Jesús University Children’s Hospital, Madrid, Spain
- 7 CIBERSAM, Madrid, Spain
Eating disorders (ED) are considered as heterogeneous disorders with a complex multifactor etiology that involves biological and environmental interaction.
Objective: The aim was to identify specific ED bio-psychological-familial correlates at illness onset.
Methods: A case-control (1:1) design was applied, which studied 50 adolescents diagnosed with ED at onset (12–17 years old) and their families, paired by age and parents’ socio-educational level with three control samples (40 with an affective disorder, 40 with asthma, and 50 with no pathology) and their respective families. Biological, psychological, and familial correlates were assessed using interviews, standardized questionnaires, and a blood test.
Results: After performing conditional logistic regression models for each type of variable, those correlates that showed to be specific for ED were included in a global exploratory model ( R 2 = 0.44). The specific correlates identified associated to the onset of an ED were triiodothyronine (T3) as the main specific biological correlate; patients’ drive for thinness, perfectionism and anxiety as the main psychological correlates; and fathers’ emotional over-involvement and depression, and mothers’ anxiety as the main familial correlates.
Conclusion: To our knowledge, this is the first study to use three specific control groups assessed through standardized interviews, and to collect a wide variety of data at the illness onset. This study design has allowed to explore which correlates, among those measured, were specific to EDs; finding that perfectionism and family emotional over-involvement, as well as the T3 hormone were relevant to discern ED cases at the illness onset from other adolescents with or without a concurrent pathology.
Introduction
Eating disorders (ED) are severe psychiatric disorders characterized by pathological attitudes and behaviors related to food. All of them share a common major characteristic: the over-evaluation of shape and weight, and their control. Other common traits are body dissatisfaction and a persistent desire for thinness, which are present throughout the course of the illness [ American Psychiatric Association (APA), 2013 ]. EDs usually begin in early adolescence, being the most frequent diagnosis among adolescents in mental health inpatient units and the third most common chronic illness in female adolescents ( Nicholls et al., 2011 ). Although previous studies have expanded our knowledge about risk factors associated with ED, few have been able to answer whether those risk factors were general or specific to ED psychopathology ( Fairburn et al., 1999 ; Pike et al., 2008 ; Machado et al., 2014 ; Gonçalves et al., 2016 ).
Regarding biological variables, pubertal status, excess body fat mass, and fluctuations in weight are factors associated with ED ( Bakalar et al., 2015 ). Changes in biological variables have been broadly related to homeostatic adaptations to malnutrition, although previous studies have also proposed that some of these, such as appetite-regulating hormones, also contribute to the development and maintenance of different behaviors related to ED ( Monteleone and Maj, 2013 ; Misra and Klibanski, 2014 ). Peripheral signals, such as fat mass derived hormones and gastrointestinal peptides may act on the central nervous system to influence eating behaviors, energy balance, and mood. In addition, the interactions between leptin, cortisol, and cytokine levels appear to be important mediators in an ED onset and its course, but their true relevance as primary or secondary alterations is mostly unknown ( Elegido et al., 2017 ).
Regarding psychological variables, multiple studies have identified perfectionism as one of the most relevant risk factors of this population ( Culbert et al., 2015 ). Another well-known risk factor for ED is negative affectivity ( Dakanalis et al., 2017 ) which has been shown to persist even after recovery ( Klump et al., 2000 ). However, whereas Fairburn et al. (1999) and Stice (2002) identified perfectionism and negative affectivity as specific risk factors for ED, another study considered perfectionism as a correlate and negative affectivity as a non-specific risk factor ( Jacobi et al., 2004 ). Body dissatisfaction was also found to be an important predictor of ED ( Stice et al., 2011 ; Jacobi and Fittig, 2012 ). Related to it, shape and weight concern has been confirmed as one of the most potent factors for the onset of an ED ( Keel and Forney, 2013 ).
On the other hand, different familial factors have been identified, such as familial pressure and discord ( Fairburn et al., 1999 ; Pike et al., 2008 ), teasing ( Neumark-Sztainer et al., 2007 ), negative perception of parental attitudes ( Kluck, 2010 ; Parks et al., 2017 ), high expressed emotion, and family history of ED ( Sepúlveda et al., 2012 , 2014 ; Hilbert et al., 2014 ). Furthermore, other authors ( Le Grange et al., 2010 ; Machado et al., 2014 ) have found that familial factors, except family history of ED, were non-specific factors as they were related to increased risk of general psychopathology. Moreover, one of the inherent difficulties of research on familial risk factors of ED is the overrepresentation of mothers’ data, as analyzing the contribution of each parent separately could improve the knowledge about the whole family system ( Anastasiadou et al., 2014 ; Gonçalves et al., 2016 ).
Previous ED etiological models have agreed that the etiology is complex, and includes biological, psychological, and socioenvironmental factors interacting at the onset and maintenance of the ED ( Treasure et al., 2008 , 2020 ). The aim of this article was to identify specific biological, psychological, and familial ED correlates associated with the onset of the disorder. Following the Kraemer et al. (1997) ’s risk factors classification, correlates are the kind of factors that cannot demonstrate precedence over the outcome. To evaluate the specificity of these correlates, three control samples were chosen: affective disorders (AD group), asthma pathology (AP group), and a non-pathological group (NP group). EDs present high comorbidity with affective disorders ( Ferreiro et al., 2011 ), suggesting that common and specific ED factors could be pointed out. Asthma sufferers present similarities on the familial level, as both disorders are considered chronic psychosomatic diseases, present severe attacks, which can be life-threatening, and pose high demands of care representing a significant impact on the physical and psychological wellbeing of the families ( Theodoratou-Bekou et al., 2012 ; Verkleij et al., 2015 ). A control group without pathology was selected in order to control the role of the adolescence as an important risk factor for an ED ( Keel and Forney, 2013 ). Consistent with the scientific literature, we hypothesized that some biological correlates (biochemical, neuroendocrine, and immunological), some psychological correlates (attitudes and behaviors related to eating psychopathology, body dissatisfaction, perfectionism and anxious, depressive, and obsessive symptomatology), and some familial correlates (family functioning, expressed emotion and anxious, depressive, and obsessive symptomatology) were specific correlates associated with the onset of an ED. We also hypothesized that an exploratory bio-psycho-familiar model based on these specific correlates would allow to identify the ED group.
Materials and Methods
Design and procedure.
The current research follows a cross-sectional case-control design, using an ED group as the case group and matching with three control groups by sex and age of the patients and socioeconomic status of the parents, following the Hollingshead Redlich Scale ( Hollingshead and Redlich, 1953 ). A complete sample description of the ANOBAS protocol and a detailed explanation of the suitability of the study control groups is provided in Sepulveda et al. (2021) .
The recruitment was carried out during 4 years. Firstly, the ED sample was recruited at the outpatient Eating Disorders Unit at the Niño Jesús University Children’s Hospital in Madrid, Spain. The samples for the three control groups was then recruited, in order to match the characteristics of each ED adolescent (1:1). The AD sample was recruited at different Mental Health Centers in the Community of Madrid. In both psychiatric groups, patients had been diagnosed by mental health professionals. In addition, AP participants were recruited at the Pneumology Department at the Niño Jesús University Children’s Hospital and the NP group was recruited at different schools in the Community of Madrid. Short telephone interviews were conducted to confirm the sociodemographic variables, and once informed written consent was obtained from adolescents and their parents, the cases were matched. The first assessment included a socio-demographic interview, a semi-structured psychiatric interview to confirm the previous diagnoses and to assess new possible comorbid psychiatric diagnoses, and a battery of questionnaires for both parents and daughters. Participants had 1 week to complete the questionnaires. This assessment was followed by a full blood test. The blood sample was collected at the Niño Jesús University Children’s Hospital and evaluated by the Immunonutrition Group at the Institute of Food Science, Technology and Nutrition (ICTAN-CSIC). Fasting venous blood samples were collected between 8 and 9 AM from patients and controls in an EDTA-K3E Vacutainer (BD Biosciences) tubes. Plasma was obtained by centrifugation during 15 min at 1,300 g and 4°C. Aliquots were frozen at −80°C until analysis.
Confidentiality was guaranteed for all the participants. The study received ethical approval by the Hospital Ethics Committee (Ref. Code, R-0009/10), and the corresponding University Research Ethics Committee (UAM, CEI 25-673).
Participants
The sample was made up by 180 females, with ages between 12 and 17 years, and their parents. Four groups were recruited: 50 adolescents diagnosed with an ED at onset of the illness, 40 adolescents diagnosed with an affective disorder at onset (AD group), 40 adolescents diagnosed with severe asthma pathology (AP group), and 50 adolescents without a pathology (NP group). Depending on the sample, data was collected from between 30 and 40 fathers, and 40 and 50 mothers.
Exclusion criteria for all groups were to suffer any metabolic conditions known to influence Body Mass Index (BMI) or a psychotic disorder, and for the three control groups, to present an ED or a BMI above 30 or below 17.5. Inclusion criteria for the ED and AD group were to present an early stage of the illness at first diagnosis (a year or less of illness duration). Inclusion criteria for the AD group were to present a diagnosis of an affective disorder without ED diagnosis. Inclusion criteria for the AP group were to have been diagnosed before the age of 7 with asthma and to have visited at least three times an emergency service, which allowed us to select more severe asthma cases. Overall, nine participants were excluded from the study after the assessment because of co-occurrence of ED and AD ( n = 2), co-occurrence of ED or AP ( n = 2), presence of psychosis ( n = 1), presence of a metabolic disorder ( n = 1), and ED pathology in the NP group ( n = 3). All of the excluded participants were not considered for matching.
Regarding the sample size, taking into account weight concerns assessed through the Eating Disorders Inventory ( Garner, 1991 ), considered as one of the most well-supported risk factor for ED, a mean effect size of AUC = 0.746 was found in one of the main reviews about risk factors in this pathology ( Jacobi et al., 2004 ). Based on that mean effect size, the Cohen’s d was calculated ( d = 0.936). The G ∗ Power program was used in order to calculate the sample size needed to detect this effect, obtaining an estimated sample size per group of 27. Based on these suggestions, a sample size of 40 or 50 was considered enough to reach good effect sizes.
Diagnostic Assessment
Current and lifetime psychiatric disorders were evaluated with the Kiddie-Schedule for Affective Disorders and Schizophrenia Interview (K-SADS-PL; Kaufman et al., 1997 ); a semi-structured interview developed to diagnose children and adolescents using DSM-IV diagnoses. Diagnoses were adapted to the DSM-5 [ American Psychiatric Association (APA), 2013 ].
Biological Assessment
A physical examination and laboratory analysis of blood markers related to nutritional and immunological status were assessed, including the following types of variables:
(a) Anthropometric variables: weight, height, and BMI.
(b) Biochemical variables: alkaline phosphatase, total cholesterol, ferritin, vitamin B12, with automated analyzer using colorimetric and nephelometric techniques and by electric potential using a selective electrode (Na, K).
(c) Neuroendocrine and Immunological variables: free tetra-iodothyronine (T4), tri-iodothyronine (T3), cortisol, estradiol, insulin like growth factor-1 (IGF1), IGF-binding protein-3 (IGFBP3), complement component 3 (C3), tumor necrosis factor α (TNF-α), leptin, soluble leptin receptor, adiponectin, by RIA, ELISA, and xMAP Technology for immunoassay of multiple analyses (Millipore).
Blood collected in EDTA-K3 vacumtainers was used for a lymphocyte subset analysis. Immediately after collection, 1 mL of blood was mixed with an equal volume (1 mL) of preservative solution and refrigerated for 2–6 days for processing and flow cytometry analysis. Unfortunately, due to budget limitations, the asthma group did not have their immunological variables measured.
Psychological Correlates Assessment
Each adolescent completed a battery of different instruments, which have shown adequate psychometric validity in Spanish adolescent samples (in the current study Cronbach α ranged between 0.81 and 0.98). Attitudes and behaviors related to eating psychopathology were assessed with the Eating Disorders Inventory-II (EDI-II; Garner, 1991 ). Body dissatisfaction was evaluated with the Body Shape Questionnaire (BSQ; Cooper et al., 1987 ). Depression was assessed with the Child Depression Inventory (CDI; Kovacs, 1992 ); anxiety with the State-Trait Anxiety Inventory for Children (STAIC; Spielberger et al., 1973 ) and obsessiveness with the Leyton Obsessional Inventory-Child Version (LOI-CV; Berg et al., 1986 ). Lastly, we used the Child Adolescent Perfectionism Scale (CAPS; Flett et al., 2000 ) to evaluate perfectionism.
Familial Correlates Assessment
The parents of each participant completed a battery of five questionnaires. These measures have shown adequate psychometric validity across Spanish populations (in the current study Cronbach α ranged between 0.78 and 0.92). To evaluate the psychological well-being of the parents we used the Beck Depression Inventory (BDI; Beck et al., 1961 ) to assess depressive symptoms, the State-Trait Anxiety Inventory (STAI, Spielberger et al., 1970 ) to assess the level of anxiety, and the Obsessive-Compulsive Inventory-Revised (OCI-R; Foa et al., 2002 ) to assess obsessive-compulsive symptoms. Regarding family functioning variables, we used the Family Adaptability and Cohesion Scale (FACES-II; Olson et al., 1982 ) to assess adaptability and cohesion, and the Family Questionnaire (FQ; Wiedemann et al., 2002 ) to evaluate critical comments (CC) and emotional over-involvement (EOI).
Data Analysis
All the statistical analyses were performed with R software.
Firstly, conditional logistic regressions were conducted for each risk factor using the survival package. Conditional logistic regressions compare each ED participant with her matching case-control participant from the AD, AP, and NP groups. More specifically, each ED participant was compared with a strata of her matching case-control AD, AP, and NP participants. Conditional logistic regressions were then conducted for each group of biological, psychological, and familial correlates where a stepwise model selection was applied to select the most relevant correlates in the model using the AIC indices of the MASS package. The statistical significance of individual correlates was corrected using Holm–Bonferroni correction for multiple comparisons. All the variables were standardized and no multicollinearity was observed, neither in biological, familial nor psychological models.
Secondly, the same conditional logistic regressions procedure was followed to estimate an exploratory bio-psycho-familial model. In this case, the complexity and the computational burden of the statistical model forced us to impute missing values by the mean of each group (missing patterns were isolated to specific cases, but listwise deletion inherent to conditional logistic regressions would considerably reduce the number of observations). In the bio-psycho-familial model, we only included those correlates that were previously conserved by stepwise model selections using the AIC indices. All the variables were standardized to estimate the bio-psycho-familial model because they had different score ranges. Finally, a stepwise model selection was applied in this model in order to determine the most relevant correlates to discriminate between ED and the control groups (AD, AP, and NP participants).
Sociodemographic Characteristics of the Participants
Participants’ sociodemographics are described in Table 1 , in which each control sample is compared with the ED sample. Given the design, no differences were found for participants’ age and socioeconomic status of the parents. In addition, no differences were found between the psychiatric groups (ED and AD) for illness duration. We only found statistically significant differences between the groups controlling by their case-control matching in the patients’ BMI. ED participants presented the following diagnoses: anorexia nervosa (AN) restrictive subtype (70%); AN purgative subtype (16%) and other specified feeding and eating disorder (14%). AD participants presented the following diagnoses: major depressive disorder (90%); dysthymia (7.5%); adjustment disorder with depressive symptoms (2.5%).
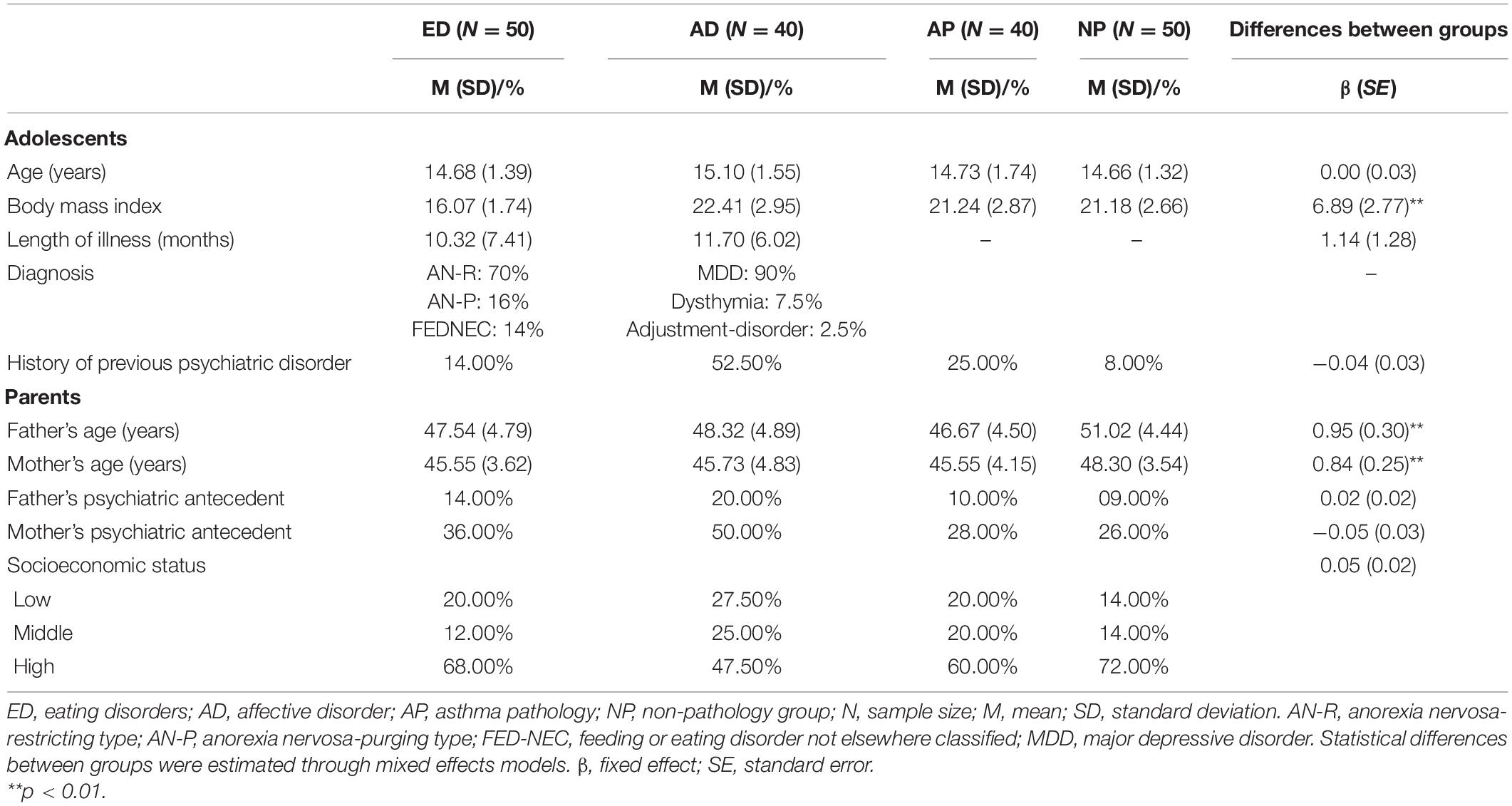
Table 1. Descriptive analyses of the sociodemographic characteristics of the participants, and mixed-effects results to test the differences between case-control with individual matching.
Examining Biological Correlates for Eating Disorders
Conditional logistic regressions were computed for each biological correlate (see Table 2 ). Results showed that higher values of vitamin B12, IGFBP3, total cholesterol, and adiponectin were relevant to differentiate the ED group with the control groups. On the other hand, the reduced values of T3 and IGF-1 were also relevant to differentiate the ED group with the control groups.
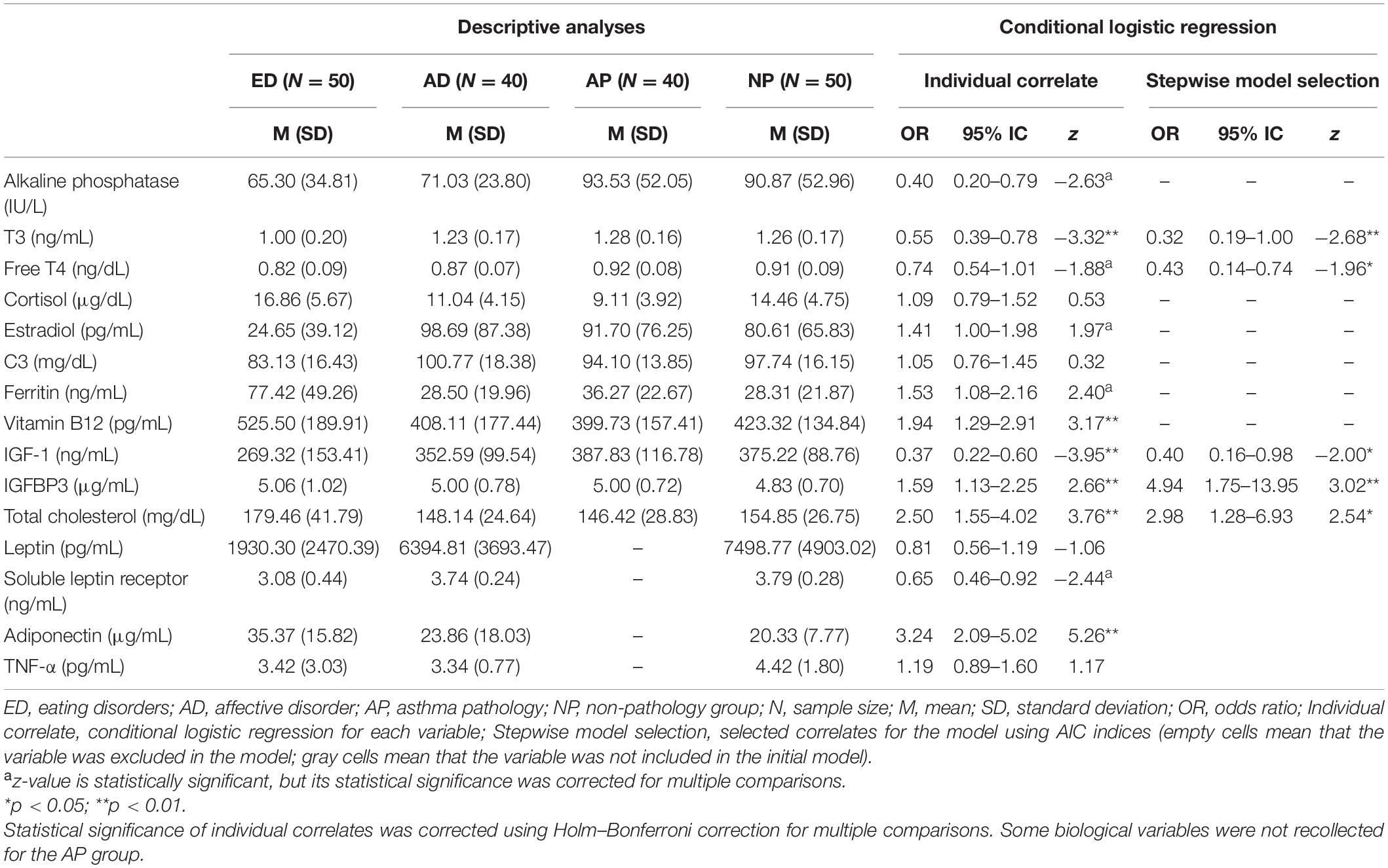
Table 2. Descriptive analyses and conditional logistic regressions for biological correlates.
A conditional logistic regression was estimated using all of the biological correlates (except leptin, soluble leptin receptor, adiponectin, and TNF-α because they were not collected in the AP group) as covariates. Stepwise model selection showed that the most relevant variables to differentiate the ED group with the control groups were T3, free T4, IGF-1, IGFBP3, and total cholesterol.
Examining Psychological Correlates for Eating Disorders
Conditional logistic regressions were computed for each psychological correlate (see Table 3 ). Results showed that the ED group reported more drive for thinness, body dissatisfaction (BSQ) and self-directed perfectionism than control groups.
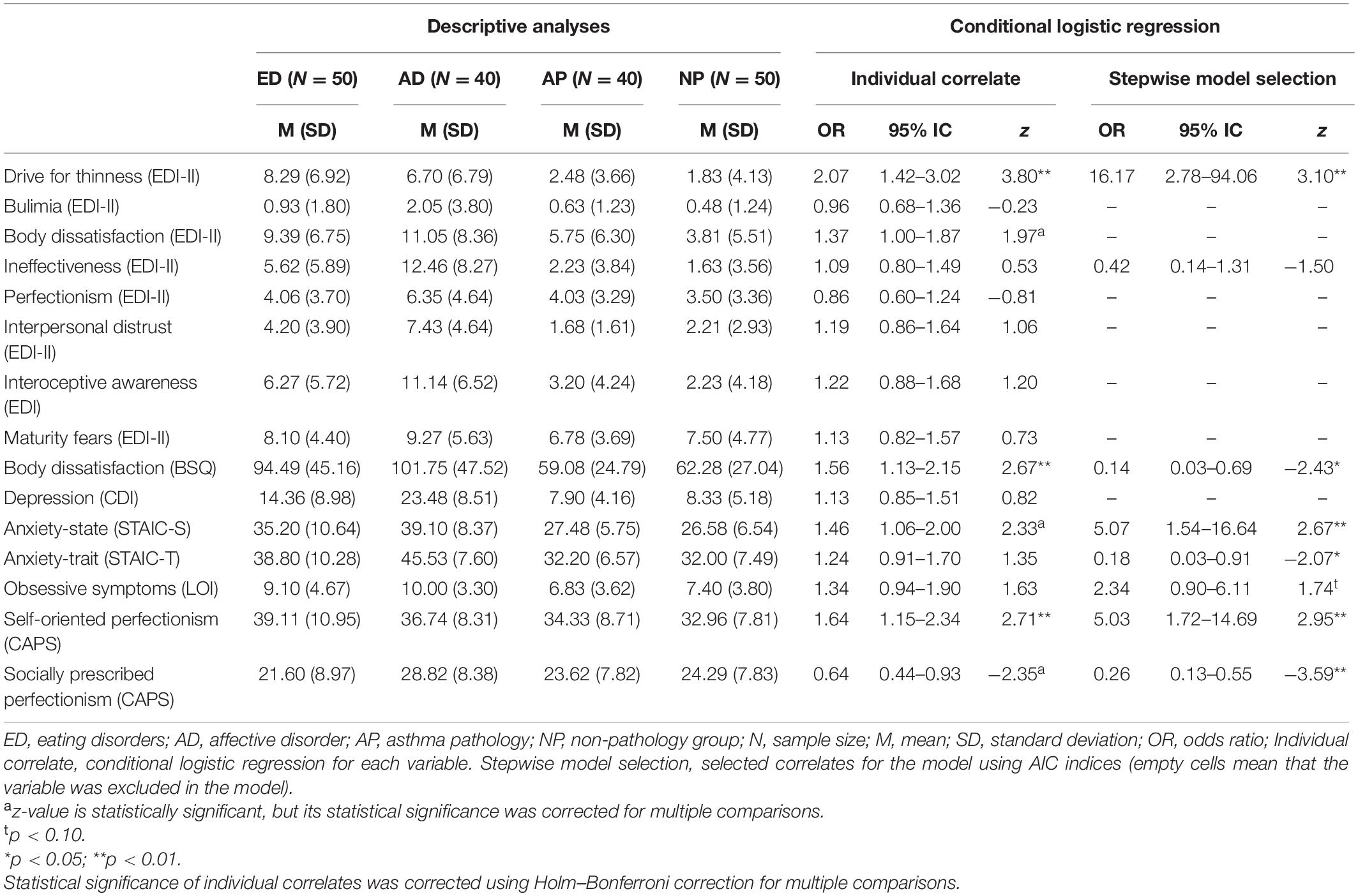
Table 3. Descriptive analyses and conditional logistic regressions for psychological correlates.
Also, a conditional logistic regression was estimated using all of the psychological correlates as covariates. A stepwise model selection showed that patients with ED reported more drive for thinness, anxiety-state, obsessive symptoms, and self-oriented perfectionism. However, patients with ED reported less body dissatisfaction, trait-anxiety, and socially prescribed perfectionism than the control groups.
Examining Familial Correlates for Eating Disorders
Conditional logistic regressions were computed for each familial correlate (see Table 4 ). Results showed that the ED group was more exposed to both fathers’ and mothers’ emotional over-involvement and mothers’ anxiety-state compared to the control groups.
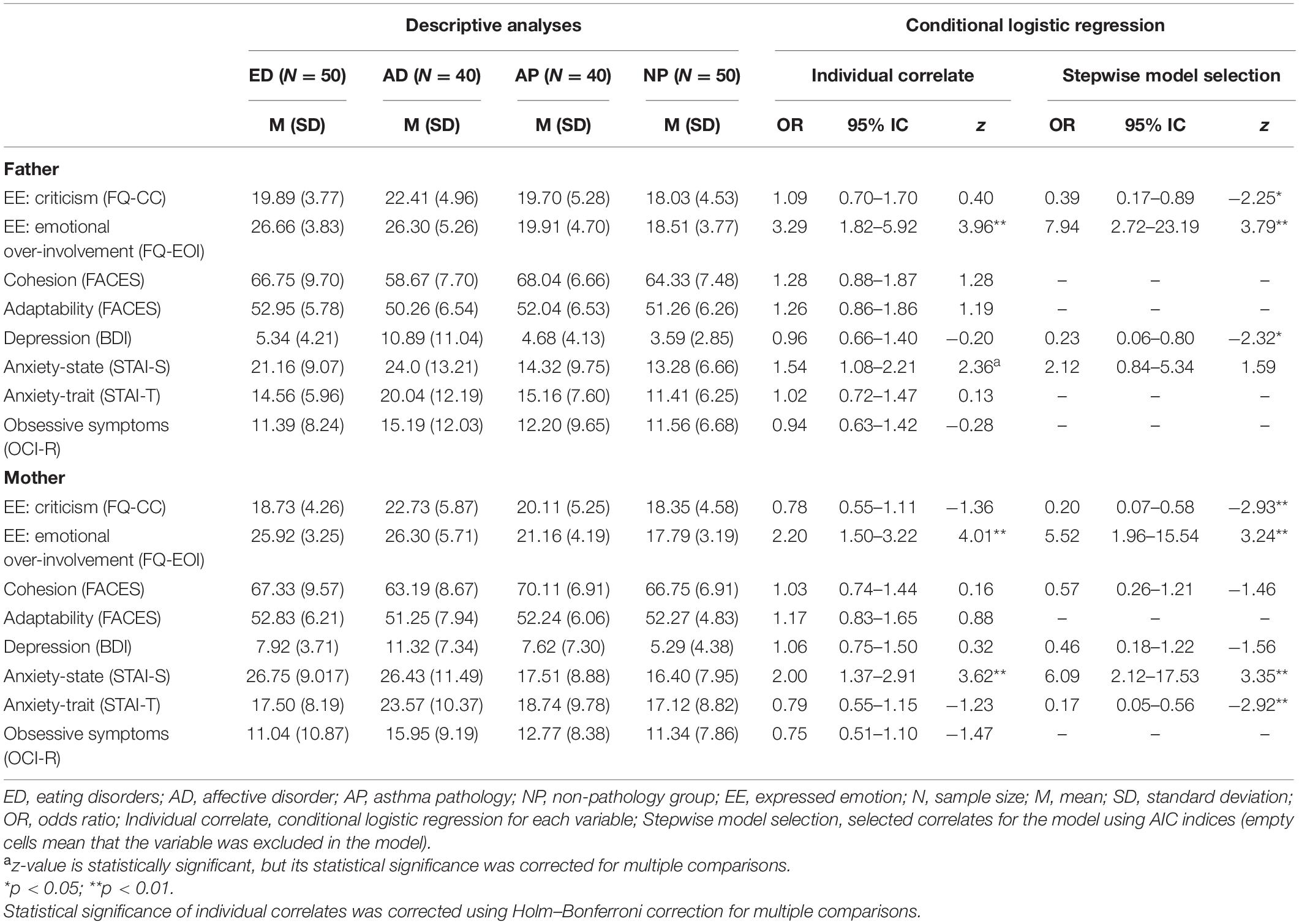
Table 4. Descriptive analyses and conditional logistic regressions for family correlates.
A conditional logistic regression was then estimated using all the familial correlates as covariates. A stepwise model selection showed that patients with an ED were more exposed to fathers’ EOI, mothers’ EOI, and mother’s anxiety-state. However, patients with ED were less exposed to fathers’ criticism and mothers’ criticism, fathers’ depression, and mothers’ trait-anxiety than the control groups.
An Exploratory Bio-Psycho-Familial Model of Specific Correlates for Eating Disorders
Once all the relevant variables were selected in the previous analyses, a bio-psycho-familial model was estimated (see Table 5 ). The complexity and thus the computational burden of the full model forced us to remove total cholesterol, IGFBP3, and mothers’ state-anxiety from the full model. The most relevant variables of this full model were selected by a stepwise model selection using the AIC indices. This model was composed by biological, psychological and familial correlates that explained a considerable part of the variance of the dependent variable ( R 2 = 0.44). In the case of biological correlates, the reduction in T3 was relevant to differentiate between case-control groups. In the case of familial correlates, we found that the ED group was more exposed to fathers’ emotional over-involvement, and less exposed to fathers’ depression and mothers’ trait-anxiety, compared to control groups. In the case of psychological correlates, we found that the ED group reported more drive for thinness and self-oriented perfectionism, and that they reported less trait-anxiety and socially prescribed perfectionism, compared to the control groups.
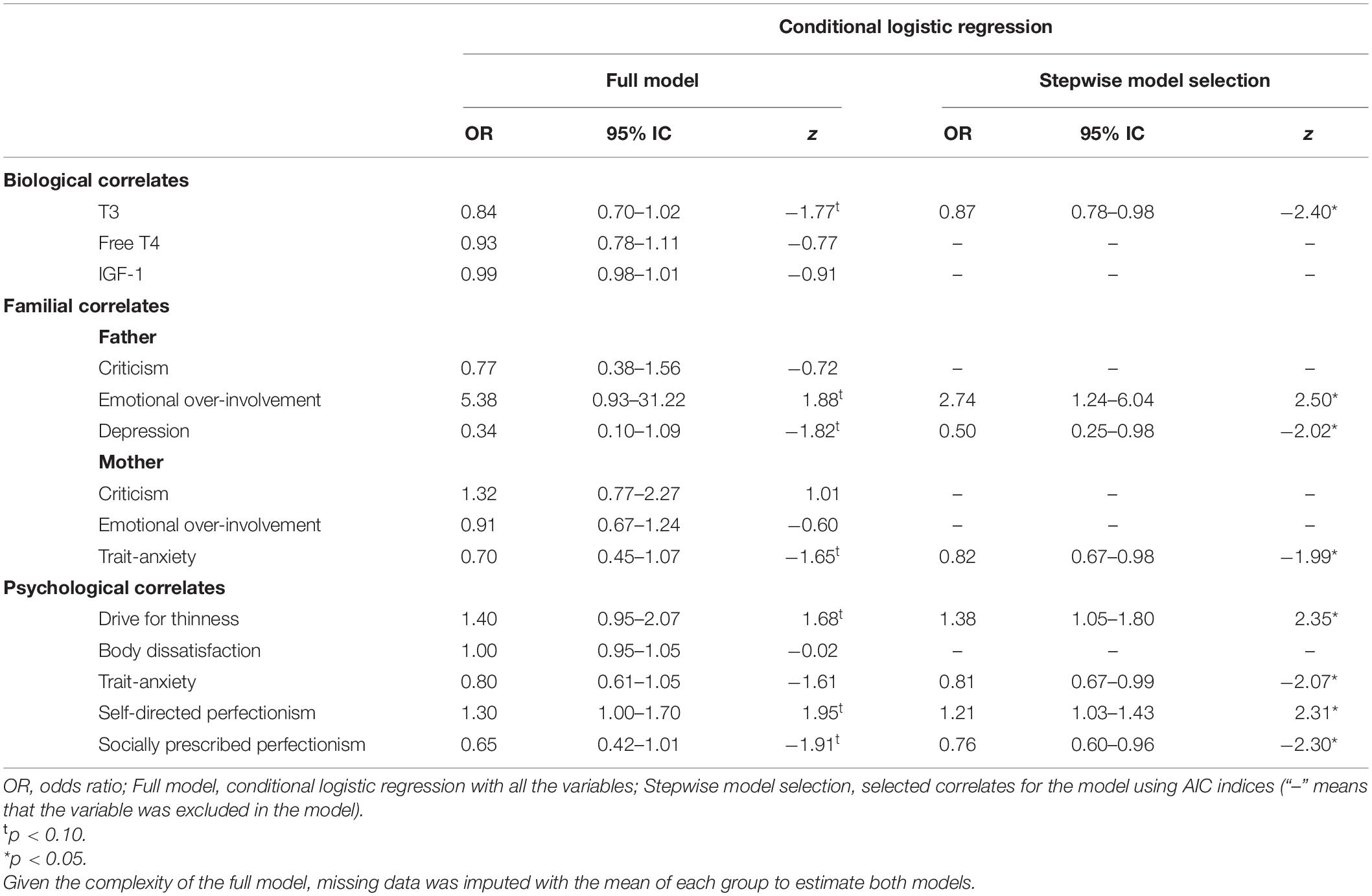
Table 5. Conditional logistic regressions to determine a bio-psycho-familial model of correlates for eating disorders.
To our knowledge, this is the first study to use three specific control groups, with standardized interviews for all the participants, collecting wide variety of data that included the capture of family functioning from both parents’ perspectives. Furthermore, ED patients were recruited at the onset of their illness, something that helped us to identify specific correlates associated with the development of an ED, in order to generate an exploratory bio-psychological-familial model.
Regarding biological variables, the biochemical variables vitamin B12 and total cholesterol, as well as the neuroendocrine variables T3, IGF1, IGFBP, and adiponectin, were relevant to differentiate the ED group with the control groups. However, when all the biological variables were considered conjointly, all these variables except vitamin B12 and adiponectin, appeared with free T4 to be the most relevant specific correlates associated with the onset of an ED. These are all endocrine variables directly related to energy availability for metabolic functions. T3 and Free T4 are usually low in AN patients in order to decrease energy requirements, while IGF-1 is a hormone produced in many cells in response to the growth hormone, it has widespread metabolic functions and is greatly involved in the adaptation to starvation ( Misra and Klibanski, 2014 ). IGF-1 has been shown to decrease in acute stages of AN, IGFBP-1 is increases, and IGFBP-3 levels are less clear. The high levels of cholesterol has been related to the decrease of T3 and T4 ( Matzkin et al., 2007 ; Himmerich et al., 2019 ). In addition, a trend toward the normalization of these molecules with anthropometrical recovery has been shown ( Støving et al., 2007 ). Thus, it appears that these molecules are good correlates to identify ED patients with a low BMI who have been recently diagnosed, and are, thus, under the effects of maintained restrictive behaviors. However, their usefulness as a potential predictor is low since their alteration is believed to be secondary to malnutrition.
The psychological correlates that have shown to be specific correlates for ED were drive for thinness, body dissatisfaction, and self-oriented perfectionism. However, when all the psychological variables were considered conjointly, the role of body dissatisfaction was not maintained and other correlates, such as obsessive symptoms, anxiety, and socially prescribed perfectionism, appeared as important correlates. Whereas body dissatisfaction was found as an important predictor for ED ( Stice et al., 2011 ), it could also act as a predictor for an affective disorder ( Ferreiro et al., 2011 ; Bornioli et al., 2021 ). In addition, their prevalence is high in adolescence ( Stice, 2002 ) and mainly in females ( Al Sabbah et al., 2009 ), and it appears to not be a specific correlate. Furthermore, other researchers’ findings underline the role of perfectionism in ED ( Fairburn et al., 1999 ; Pike et al., 2008 ; Machado et al., 2014 ), similar to our findings. Nevertheless, an important difference was found between self-oriented perfectionism and socially prescribed perfectionism. Castro-Fornieles et al. (2007) found that self-oriented perfectionism was more specific for EDs and socially prescribed perfectionism appeared in similar levels in other psychiatric disorders.
On the other hand, emotional over-involvement of both parents and mother state-anxiety emerged as specific familial correlates for an ED. When all the familial variables were considered conjointly, the reduction of both parents’ criticism, fathers’ depression and mothers’ trait-anxiety appeared as specific correlates for ED. These results may suggest that psychological distress (characterized by severe depression and trait-anxiety) and high expressed emotion of family members may be associated with an ED, consistent with the review done by Zabala et al. (2009) . Likewise, the difference in the dimensions of expressed emotion is in accordance with the tendency of higher levels of EE-EOI compared to EE-CC in families with an ED, a finding which was reported by Anastasiadou et al. (2016) .
The exploratory bio-psychological-familial model showed that the increase of fathers’ EOI, patients’ drive of thinness and self-oriented perfectionism together with the decrease of T3, anxiety and socially prescribed perfectionism of the adolescents as well as the decrease of fathers’ depression and mothers’ anxiety were specifically associated to the onset of an ED. The fathers’ EOI appeared as a robust specific correlate, in contrast to a recent systematic review which proposed that mothers were more emotionally over-involved than fathers, who tend to be more critical ( Anastasiadou et al., 2014 ). However, in this review several studies did not include comparison groups. In our research, mothers of the AD group showed higher levels of emotional over-involvement as well as fathers for the AD group showed higher levels of criticism compared to parents with ED. It seems that in the ED group, fathers play an important role, which can differentiate this group from other control groups even better than mothers, suggesting that future research should include them in the assessment.
These results also contrast with the studies that have suggested that familial factors are non-specific factors for the onset of an ED ( Le Grange et al., 2010 ; Herpertz-Dahlmann et al., 2011 ; Machado et al., 2014 ). Indeed, some authors have emphasized the possibility that these factors would be an accommodation to the illness rather than predisposing factors that explain it ( Le Grange et al., 2010 ). Regardless of their role, expressed emotion is a potential prognostic indicator, that is stable in periods of up to 2 years and that predicts poor outcomes for treatment ( Peris and Miklowitz, 2015 ). Further studies are needed in order to clarify the role of familial correlates in ED.
In addition, the decrease of fathers’ levels of depression and mothers’ trait anxiety followed a similar tendency as the adolescents’ decreased in the trait-anxiety. Several studies have examined the similarities between the negative affectivity dimension and the factors measured by BDI or STAI scales, and have concluded that they should be considered as a measure of general negative affect ( Balsamo et al., 2013 ). Therefore, our findings do not support the centrality of negative affectivity as a specific correlate for ED, in concordance with similar recent studies that have considered it as a general psychopathological risk factor ( Jacobi and Fittig, 2012 ; Machado et al., 2014 ).
Lastly, two psychological variables, perfectionism and drive for thinness, and one biological variable, T3, appeared to be specific correlates associated with the onset of an ED. The literature broadly supports the role of these variables. Indeed, a recent study has revealed that Free-T3 is a specific and sensitive correlate in distinguishing constitutional thinness and AN groups, showing significantly lower values in the latter with similar BMI between groups ( Estour et al., 2017 ). Thus, although the low levels are thought to normalize with weight gain, evidence shows its relevance in AN patients and therefore, an early assessment in adolescents with a suspected ED is advisable.
The current study presents several limitations. Firstly, the cross-sectional case-control nature of the study does not allow inferring causality. However, Jacobi et al. (2004) suggested that using a case-control study is a good way to analyze correlates in a wide sample that can then be contrasted in a longitudinal study. Secondly, we only considered patients with a maximum of a 1-year course in order to reduce bias due to retrospective recall, although some of them had a history of a previous psychiatric disorders. Consequently, the involvement of other informants, such as parents, is important to contrast the information given by the adolescents. Thirdly, females with high socioeconomic status were predominant in this sample. Although it may be a limitation for the generalization of the results, high socioeconomic status is also frequent in EDs ( Striegel-Moore and Bulik, 2007 ), and matching for parental socioeconomic status reduces differences in family experiences related to the availability of resources.
To summarize, this study proposes a complex model, which shows the importance of different correlates that are associated with the onset of an ED, although our findings require further research that can be contrasted in longitudinal studies and assessed in comparison with other control groups in order to confirm the specificity of the correlates. Most of the correlates found in this study are a replication of previously found risk factors in the literature, whereas the specificity and their relation have not been fully investigated. All of the participants have been assessed with reliable measures (blood test, clinical interview, and questionnaires). In our bio-psycho-familial model, eight correlates were specifically related to ED, therefore, the study confirms the importance of these three types of variables, which could be the target of future prevention and treatment interventions.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
Ethics Statement
The studies involving human participants were reviewed and approved by approval was granted by the Ethic Committee of the Niño Jesús University Children’s Hospital (Ref Code. R-0009/10) and by the Autonomous University of Madrid Ethic Research Committee (UAM, CEI 25-673). Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin.
Author Contributions
AS, EN, AM, JV-A, EM, and MG contributed to conception and design of the study. DA, SG-M, and AM organized the database. JMH performed the statistical analysis. AM wrote the manuscript. All authors contributed to manuscript revision, read, and approved the submitted version.
This work was supported by the Spanish Ministry of Science and Innovation (RYC-2009-05092 and PSI2011-23127) and the Education Ministry of Spain (FPU15/05783).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We express our gratitude to all the families, staff hospital, and psychiatrists from the Mental Health Centers who helped us in the recruitment process. Likewise, we are very grateful to the headmasters and teachers from this three Secondary Schools: IES La Estrella, IES Las Musas, and IES Alameda de Osuna, that facilitated the recruitment stage. We would finally like to express our gratitude to T. Alvarez, L. Gonzalez, and C. Bustos.
Al Sabbah, H., Vereecken, C. A., Elgar, F. J., Nansel, T., Aasvee, K., Abdeen, Z., et al. (2009). Body weight dissatisfaction and communication with parents among adolescents in 24 countries: international cross-sectional survey. BMC Public Health 9:52. doi: 10.1186/1471-2458-9-52
PubMed Abstract | CrossRef Full Text | Google Scholar
American Psychiatric Association (APA). (2013). The Diagnostic and Statistical Manual of Mental Disorders , 5th Edn. Arlington: American Psychiatric.
Google Scholar
Anastasiadou, D., Medina-Pradas, C., Sepulveda, A. R., and Treasure, J. (2014). A systematic review of family caregiving in eating disorders. Eat. Behav. 15, 464–477. doi: 10.1016/j.eatbeh.2014.06.001
Anastasiadou, D., Sepulveda, A. R., Sánchez, J. C., Parks, M., Álvarez, T., and Graell, M. (2016). Family functioning and quality of life among families in eating disorders: a comparison with substance-related disorders and healthy controls. Eur. Eat. Disord. Rev. 24, 294–303. doi: 10.1002/erv.2440
Bakalar, J. L., Shank, L. M., Vannucci, A., Radin, R. M., and Tanofsky-Kraff, M. (2015). Recent Advances in Developmental and Risk Factor Research on Eating Disorders. Curr. Psychiatry Rep. 17:42. doi: 10.1007/s11920-015-0585-x
Balsamo, M., Romanelli, R., Innamorati, M., Ciccarese, G., Carlucci, L., and Saggino, A. (2013). The state-trait anxiety inventory: shadows and lights on its construct validity. J. Psychopathol. Behav. Assess. 35, 475–486. doi: 10.1007/s10862-013-9354-5
CrossRef Full Text | Google Scholar
Beck, A. T., Ward, C. H., Mendelson, M., Mock, J., and Erbaugh, J. (1961). An inventory for measuring depression. Arch. Gen. Psychiatry 4, 561–571. doi: 10.1001/archpsyc.1961.01710120031004
Berg, C. J., Rapoport, J. L., and Flament, M. (1986). The Leyton Obsessional Inventory-Child Version. J. Am. Acad. Child Psychiatry 25, 84–91. doi: 10.1016/S0002-7138(09)60602-6
Bornioli, A., Lewis-Smith, H., Slater, A., and Bray, I. (2021). Body dissatisfaction predicts the onset of depression among adolescent females and males: a prospective study. J. Epidemiol. Community Health 75, 343–348. doi: 10.1136/jech-2019-213033
Castro-Fornieles, J., Gual, G., Lahortiga, F., Gila, A., Casulà, V., Fuhrmann, C., et al. (2007). Self-Oriented Perfectionism in Eating Disorders. Int. J. Eat. Disord. 40, 562–658.
Cooper, P., Taylor, M. J., Cooper, Z., and Fairbum, C. (1987). The development and validation of the body shape questionnaire. Int. J. Eat. Disord. 6, 485–494. doi: 10.1002/1098-108X(198707)6:4<485::AID-EAT2260060405<3.0.CO;2-O
Culbert, K. M., Racine, S. E., and Klump, K. L. (2015). Research Review: what we have learned about the causes of eating disorders - A synthesis of sociocultural, psychological, and biological research. J. Child Psychol. Psychiatry Allied Discip. 56, 1141–1164. doi: 10.1111/jcpp.12441
Dakanalis, A., Clerici, M., Bartoli, F., Caslini, M., Crocamo, C., Riva, G., et al. (2017). Risk and maintenance factors for young women’ s DSM-5 eating disorders. Arch. Womens. Ment. Health 20, 721–731. doi: 10.1007/s00737-017-0761-6
Elegido, A., Graell, M., Andrés, P., Gheorghe, A., Marcos, A., and Nova, E. (2017). Increased naive CD4+ and B lymphocyte subsets are associated with body mass loss and drive relative lymphocytosis in anorexia nervosa patients. Nutr. Res. 39, 43–50. doi: 10.1016/j.nutres.2017.02.006
Estour, B., Marouani, N., Sigaud, T., Lang, F., Fakra, E., Ling, Y., et al. (2017). Differentiating constitutional thinness from anorexia nervosa in DSM 5 era. Psychoneuroendocrinology 84, 94–100. doi: 10.1016/j.psyneuen.2017.06.015
Fairburn, C. G., Cooper, Z., Doll, H. A., and Welch, S. L. (1999). Risk Factors for Anorexia Nervosa. Arch. Gen. Psychiatry 56, 468–476.
Ferreiro, F., Seoane, G., and Senra, C. (2011). A prospective study of risk factors for the development of depression and disordered eating in adolescents. J. Clin. Child Adolesc. Psychol. 40, 500–505. doi: 10.1080/15374416.2011.563465
Flett, G. L., Hewitt, P. L., Besser, A., Su, C., Vaillancourt, T., Boucher, D., et al. (2000). The Child-Adolescent Perfectionism Scale. J. Psychoeduc. Assess. 34, 634–652. doi: 10.1177/0734282916651381
Foa, E. B., Huppert, J. D., Leiberg, S., Langner, R., Kichic, R., Hajcak, G., et al. (2002). The Obsessive-Compulsive Inventory: development and validation of a short version. Psychol. Assess. 14:485. doi: 10.1037/1040-3590.14.4.485
Garner, D. M. (1991). Eating Disorder Inventory-2 Professional Manual. Odessa: Psychological Assessment Resources.
Gonçalves, S., Machado, B. C., Martins, C., Hoek, H. W., and MacHado, P. P. P. (2016). Retrospective Correlates for Bulimia Nervosa: a Matched Case-Control Study. Eur. Eat. Disord. Rev. 24, 197–205. doi: 10.1002/erv.2434
Herpertz-Dahlmann, B., Seitz, J., and Konrad, K. (2011). Aetiology of anorexia nervosa: from a “‘psychosomatic family model”’ to a neuropsychiatric disorder? Eur. Arch. Psychiatry Clin. Neurosci. 261, 177–181. doi: 10.1007/s00406-011-0246-y
Hilbert, A., Pike, K. M., Goldschmidt, A. B., Wilfley, D. E., Fairburn, C. G., Dohm, F. A., et al. (2014). Risk factors across the eating disorders. Psychiatry Res. 220, 500–506. doi: 10.1016/j.psychres.2014.05.054
Himmerich, H., Bentley, J., Kan, C., and Treasure, J. (2019). Factores de riesgo genéticos para los trastornos alimentarios: una actualización e información sobre la fisiopatología. Rev. Toxicom. 82, 3–18.
Hollingshead, A. B., and Redlich, F. C. (1953). Social Stratification and Psychiatric Disorders. American Sociological Rev. 18, 163–169.
Jacobi, C., and Fittig, E. (2012). Psychosocial Risk Factors for Eating Disorders. doi: 10.1093/oxfordhb/9780195373622.013.0008
Jacobi, C., Hayward, C., De Zwaan, M., Kraemer, H. C., and Agras, W. S. (2004). Coming to Terms With Risk Factors for Eating Disorders: application of Risk Terminology and Suggestions for a General Taxonomy. Psychol. Bull. 130, 19–65. doi: 10.1037/0033-2909.130.1.19
Kaufman, J., Birmaher, B., Brent, D., Rao, U. M. A., Flynn, C., Moreci, P., et al. (1997). Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): initial reliability and validity data. J. Am. Acad. Child Adolesc. Psychiatry 36, 980–998. doi: 10.1097/00004583-199707000-00021
Keel, P. K., and Forney, K. J. (2013). Psychosocial Risk Factors for Eating Disorders. Int. J. Eat. Disord. 46, 433–439.
Kluck, A. S. (2010). Family influence on disordered eating: the role of body image dissatisfaction. Body Image 7, 8–14. doi: 10.1016/j.bodyim.2009.09.009
Klump, K. L., Bulik, C. M., Pollice, C., Halmi, K. A., Fichter, M. M., Berrettini, W. H., et al. (2000). Temperament and character in women with anorexia nervosa. J. Nervous Ment. Dis. 188, 559–567.
Kovacs, M. (1992). Children’s Depression Inventory CDI Manua. New York: Multi-Health Systems.
Kraemer, H. C., Kazdin, A. E., and Offord, D. E. (1997). Coming to Terms With the Terms of Risk. Arch. Gen. Psychiatry 54, 337–343. doi: 10.1001/archpsyc.1997.01830160065009
Le Grange, D., Lock, J., Loeb, K., and Nicholls, D. (2010). Academy for eating disorders position paper: the role of the family in eating disorders. Int. J. Eat. Disord. 43, 1–5. doi: 10.1002/eat.20751
Machado, B. C., Gonçalves, S. F., Martins, C., Hoek, H. W., and Machado, P. P. (2014). Risk factors and antecedent life events in the development of anorexia nervosa: a Portuguese case-control study. Eur. Eat. Disord. Rev. 22, 243–251. doi: 10.1002/erv.2286
Matzkin, V., Slobodianik, N., Pallaro, A., Bello, M., and Geissler, C. (2007). Risk factors for cardiovascular disease in patients with anorexia nervosa. Int. J. Psychiatr. Nurs. Res. 13, 1531–1545.
Misra, M., and Klibanski, A. (2014). Endocrine Consequences of Anorexia Nervosa Madhusmita. Lancet Diabetes Endocrinol. 2, 581–592. doi: 10.1016/S2213-8587(13)70180-3
Monteleone, P., and Maj, M. (2013). Dysfunctions of leptin, ghrelin, BDNF and endocannabinoids in eating disorders: beyond the homeostatic control of food intake. Psychoneuroendocrinology 38, 312–330. doi: 10.1016/j.psyneuen.2012.10.021
Neumark-Sztainer, D. R., Wall, M. M., Haines, J. I., Story, M. T., Sherwood, N. E., and van den Berg, P. A. (2007). Shared Risk and Protective Factors for Overweight and Disordered Eating in Adolescents. Am. J. Prev. Med. 33, 359–369. doi: 10.1016/j.amepre.2007.07.031
Nicholls, D. E., Lynn, R., and Viner, R. M. (2011). Childhood eating disorders: british national surveillance study. Br. J. Psychiatry 198, 295–301. doi: 10.1192/bjp.bp.110.081356
Olson, D. H., Portner, J., and Bell, R. Q. (1982). FACES II: family Adaptability and Cohesion Evaluation Scales. United States: University of Minnesota.
Parks, M., Anastasiadou, D., Sánchez, J. C., Graell, M., and Sepulveda, A. R. (2017). Experience of caregiving and coping strategies in caregivers of adolescents with an eating disorder: a comparative study. Psychiatry Res. 260, 241–247. doi: 10.1016/j.psychres.2017.11.064
Peris, T. S., and Miklowitz, D. J. (2015). Parental Expressed Emotion and Youth Psychopathology: new Directions for an Old Construct. Child Psychiatry Hum. Dev. 46, 863–873. doi: 10.1007/s10578-014-0526-7
Pike, K. M., Hilbert, A., Wilfley, D. E., Fairburn, C. G., Dohm, F. A., Walsh, B. T., et al. (2008). Toward an understanding of risk factors for anorexia nervosa: a case-control study. Psychol. Med. 38, 1443–1453. doi: 10.1017/S0033291707002310
Sepúlveda, A. R., Anastasiadou, D., Rodríguez, L., Almendros, C., Andrés, P., Vaz, F., et al. (2014). Spanish validation of the Family Questionnaire (FQ) in families of patients with an eating disorder. Psicothema 26, 321–327. doi: 10.7334/psicothema2013.310
Sepúlveda, A. R., Graell, M., Berbel, E., Anastasiodou, D., Botella, J., Carrobles, J. A., et al. (2012). Factors Associated with Emotional Wellbeing in Primary and Secondary Caregivers of Patients with Eating Disorders. Eur. Eat. Dis. Rev. 20, e78–84. doi: 10.1002/erv.1118
Sepulveda, A. R., Moreno-Encinas, A., Nova, E., Gomez, S., Carrobles, J. A., and Graell, M. (2021). Biological, psychological and familial specific correlates in eating disorders at onset: a control-case study protocol (ANOBAS). Actas Esp. Psiquiatr.
Spielberger, C. D., Edwards, C. D., Lushene, R. E., Montuori, J., and Platzek, A. (1973). State-Trait Anxiety Inventory for Children. Palo Alto: Consulting Psychologists Press.
Spielberger, C. D., Gorsuch, R., and Lushene, R. (1970). Manual for the State-Trait Anxiety Inventory. Palo Alto: Consulting Psychologist Press.
Stice, E. (2002). Risk and maintenance factors for eating pathology: a meta-analytic review. Psychol. Bull. 128, 825–848. doi: 10.1037/0033-2909.128.5.825
Stice, E., Marti, C. N., and Durant, S. (2011). Risk factors for onset of eating disorders: evidence of multiple risk pathways from an 8-year prospective study. Behav. Res. Ther. 49, 622–627. doi: 10.1016/j.brat.2011.06.009
Støving, R. K., Chen, J. W., Glintborg, D., Brixen, K., Flyvbjerg, A., Hørder, K., et al. (2007). Bioactive Insulin-like Growth Factor (IGF) I and IGF-binding protein-1 in anorexia nervosa. J. Clin. Endocrinol. Metab. 92, 2323–2329. doi: 10.1210/jc.2006-1926
Striegel-Moore, R. H., and Bulik, C. M. (2007). Risk Factors for Eating Disorders. Am. Psychol. 62, 181–198. doi: 10.1037/0003-066X.62.3.181
Theodoratou-Bekou, M., Andreopoulou, O., Andriopoulou, P., and Wood, B. (2012). Stress-related asthma and family therapy: case study. Ann. Gen. Psychiatry 11, 1–10. doi: 10.1186/1744-859X-11-28
Treasure, J., Duarte, T. A., and Schmidt, U. (2020). Eating disorders. Lancet 395, 899–911. doi: 10.1016/S0140-6736(20)30059-3
Treasure, J., Sepúlveda, A. R., Macdonald, P., Whitaker, W., Lopez, C., Zabala, M., et al. (2008). The assessment of the family of people with eating disorders. Eur. Eat. Dis. Rev. 16, 247–255. doi: 10.1002/erv.859
Verkleij, M., Van De Griendt, E.-J., Colland, V., Van Loey, N., Beelen, A., and Geenen, R. (2015). Parenting Stress Related to Behavioral Problems and Disease Severity in Children with Problematic Severe Asthma. J. Clin. Psychol. Med. 22, 179–93. doi: 10.1007/s10880-015-9423-x
Wiedemann, G., Rayki, O., Feinstein, E., and Hahlweg, K. (2002). The Family Questionnaire: development and validation of a new self-report scale for assessing expressed emotion. Psychiatry Res. 109, 265–279. doi: 10.1016/S0165-1781(02)00023-9
Zabala, M. J., Macdonald, P., and Treasure, J. (2009). Appraisal of caregiving burden, expressed emotion and psychological distress in families of people with eating disorders: a systematic review. Eur. Eat. Disord. Rev. 17, 338–349. doi: 10.1002/erv.925
Keywords : eating disorders, case-control study, biological correlates, psychological correlates, familial correlates
Citation: Sepúlveda AR, Moreno-Encinas A, Martínez-Huertas JA, Anastasiadou D, Nova E, Marcos A, Gómez-Martínez S, Villa-Asensi JR, Mollejo E and Graell M (2021) Toward a Biological, Psychological and Familial Approach of Eating Disorders at Onset: Case-Control ANOBAS Study. Front. Psychol. 12:714414. doi: 10.3389/fpsyg.2021.714414
Received: 25 May 2021; Accepted: 20 August 2021; Published: 09 September 2021.
Reviewed by:
Copyright © 2021 Sepúlveda, Moreno-Encinas, Martínez-Huertas, Anastasiadou, Nova, Marcos, Gómez-Martínez, Villa-Asensi, Mollejo and Graell. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ana Rosa Sepúlveda, [email protected] ; Alba Moreno-Encinas, [email protected]
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Expert Review
- Open access
- Published: 20 May 2022
What next for eating disorder genetics? Replacing myths with facts to sharpen our understanding
- Laura M. Huckins ORCID: orcid.org/0000-0002-5369-6502 1 , 2 , 3 , 4 , 5 , 6 ,
- Rebecca Signer 1 , 2 , 3 ,
- Jessica Johnson 1 ,
- Ya-Ke Wu 7 , 8 ,
- Karen S. Mitchell 9 , 10 &
- Cynthia M. Bulik ORCID: orcid.org/0000-0001-7772-3264 8 , 11 , 12
Molecular Psychiatry volume 27 , pages 3929–3938 ( 2022 ) Cite this article
6767 Accesses
7 Citations
50 Altmetric
Metrics details
- Psychiatric disorders
Substantial progress has been made in the understanding of anorexia nervosa (AN) and eating disorder (ED) genetics through the efforts of large-scale collaborative consortia, yielding the first genome-wide significant loci, AN-associated genes, and insights into metabo-psychiatric underpinnings of the disorders. However, the translatability, generalizability, and reach of these insights are hampered by an overly narrow focus in our research. In particular, stereotypes, myths, assumptions and misconceptions have resulted in incomplete or incorrect understandings of ED presentations and trajectories, and exclusion of certain patient groups from our studies. In this review, we aim to counteract these historical imbalances. Taking as our starting point the Academy for Eating Disorders (AED) Truth #5 “Eating disorders affect people of all genders, ages, races, ethnicities, body shapes and weights, sexual orientations, and socioeconomic statuses”, we discuss what we do and do not know about the genetic underpinnings of EDs among people in each of these groups, and suggest strategies to design more inclusive studies. In the second half of our review, we outline broad strategic goals whereby ED researchers can expand the diversity, insights, and clinical translatability of their studies.
Similar content being viewed by others

Genetics and neurobiology of eating disorders
Polygenic association with severity and long-term outcome in eating disorder cases

The impact of genetic risk for schizophrenia on eating disorder clinical presentations
Over the past decade, substantial progress has been made in understanding the genetic etiology of anorexia nervosa (AN) and related eating disorders (EDs). Global collaborative efforts have yielded large-scale linkage, and later, genome-wide associations studies [ 1 , 2 , 3 , 4 ], revealing the first genome-wide significant loci [ 1 ] and 53 genes associated with AN across tissues [ 5 ]. These studies have led to new insights and hypotheses about the etiopathology of AN including evidence of psychiatric and metabolic risk factors [ 1 ]; shared genetic etiology with metabolic, anthropometric, and psychiatric traits [ 1 ]; and evidence for clinical consequences of predicted aberrant AN-gene expression [ 5 ]. Similar analyses of other EDs are underway. However, substantial unanswered questions remain about the biological mechanisms underlying AN and EDs; this gap in our understanding is a key contributor to the lack of effective, personalized treatments. ED science faces an uphill battle in replacing decades of myths, misunderstandings, and stereotypes about the presentation, demographics, symptoms, and etiopathology of EDs. Moreover, these misconceptions are subtly embedded in the research questions that have contributed to fundamental knowledge in the field and have influenced the populations we recruit and study.
To contextualize ED genetic research, we take as a starting point an aspirational document prepared and disseminated (available in 34 languages) by the Academy for Eating Disorders (AED), titled the Nine Truths About Eating Disorders [ 6 ]. Ongoing ED research is addressing several of the AED truths [ 7 ]. We focus on AED Truth #5 “Eating disorders affect people of all genders, ages, races, ethnicities, body shapes and weights, sexual orientations, and socioeconomic statuses” to illustrate how inclusivity in genetic research can contribute to a more comprehensive understanding of the full spectrum of EDs and ultimately revolutionize our understanding of this disease cluster.
AED Truth #5 directly counters many of the stereotypes that have hindered ED science. Dissecting this truth illustrates the importance of broad representation to prevent biased or distorted understanding of the causes and impact of EDs. The failure to acknowledge the diversity of individuals affected by EDs has led to narrow definitions of disease and diagnostic criteria, and consequently incomplete assessments of disease characteristics, risk factors, and etiology. Accordingly, individuals who fall outside of these parameters (i.e., those who are not young, thin, affluent white women) have been excluded from research and even from treatment. Stereotypes propagated by the media as well as the medical profession have contributed to under-detection and under-treatment of individuals with EDs who do not conform to these expectations. Under-detection, under-diagnosis, and under-referral for specialist treatment have been documented in men [ 8 , 9 ], in people of color [ 10 , 11 , 12 , 13 , 14 ], in older individuals [ 15 ], in the LGBTQIA+ community [ 16 , 17 , 18 ], and in individuals living in larger bodies [ 19 ]. Failure to include these communities truncates our observations of risk factors and symptoms of EDs to a narrow slice of the affected population. Without representation, we cannot begin to understand the full spectrum of risk, and the mechanisms underlying EDs.
Expansion of genetic studies to include diverse presentations of EDs, and to capture the full spectrum of symptoms, behaviors, and outcomes that characterize EDs will yield increased power for discovery overall, but, more importantly, may also yield insights into specific genetic underpinnings of different facets of the disorders. Analytical approaches that can identify symptom-specific associations and account for potential biases can help reshape the understanding of EDs in the minds of researchers, clinicians, and the general public. In the Section “Background”, we outline what is known about EDs across the various groups referenced in AED Truth #5, and highlight existing genetic studies in these groups. In the Section “Large-scale approaches to address diversity in ED genetics”, we propose strategies for enhancing genetic research to advance the science of EDs.
EDs affect people of all genders and sexual orientations
ED research, diagnoses, treatment guidelines, and public attention have overwhelmingly focused on women and girls. Although men might be included in studies, numbers are often too small to warrant analysis or to generate confident conclusions (Fig. 1 ). Although EDs occur within and across gender and sexual orientation spectra [ 8 , 16 , 17 , 18 , 20 ], the underlying genetic and environmental risk factors may be very different within and across groups, necessitating specialized screening, prevention, and treatment. In this review, we use ‘sex’ to refer to categorical variables including ‘male’ and ‘female’ as defined in the original studies, and ‘gender’ to refer to socially constructed behaviors and identities, rather than biological attributes [ 21 , 22 ].
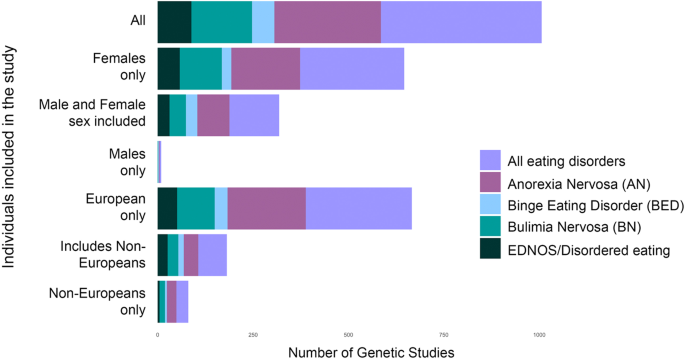
Data include all genetic studies from 1980–2021. Studies where sex or race/ethnicity were not recorded are included in ‘all’. Studies with at least one male participant are included in ‘male and female sexes included’; studies with at least one non-European participant are included in ‘includes non-Europeans’. We caution that, for many of these studies, numbers of males/non-Europeans are very small.
EDs in boys and men
According to a recent large meta-analysis, the gender ratio for AN is estimated to be 7:1 [ 23 ], for bulimia nervosa (BN) ~3.2:1 [ 23 ], and for binge-eating disorder (BED) 2.8:1 [ 23 ]. The lifetime prevalence of EDs was 8.4% for women and 2.2% for men around the world, based on an analysis of 94 articles with ED diagnoses from 28 countries (e.g., Argentina, Brazil, Canada, China, Finland, Germany, Italy, Japan, and Portugal) [ 23 ]. Globally, the lifetime prevalence of AN was 1.4% for women and 0.2% for men; BN was 1.9% for women and 0.6% for men; and BED was 2.8% for women and 1.0% for men [ 23 ]. These figures reflect diagnostic criteria developed based on clinical presentation in women and likely underestimate the prevalence in men. For example, whereas women (in Western countries) address their underlying “drive for thinness” and concern with weight and shape by focusing on being thin and losing weight, men tend to show more concern for building lean muscle [ 24 ] and express that drive via reducing body fat percentage or striving for muscle definition. Compensatory behaviors also differ, with women being more likely to engage in self-induced vomiting and diuretic/laxative use, whereas men are more likely to exercise excessively and take anabolic steroids or supplements to pursue their ideal body shape [ 25 ]. In addition, the long history of EDs being considered a female disorder increases hesitancy and shame in males decreasing help-seeking [ 24 ], and hinders detection by clinicians who do not include EDs on the differential for male patients [ 9 ].
EDs in the LGBTQIA+ population
LGBTQIA+ individuals report increased prevalence of psychiatric disorders, including all EDs [ 16 , 17 , 18 ], due at least in part to the systematic discrimination, harassment, and violence they experience [ 16 , 17 , 18 , 26 ]. Watson, et al. [ 17 ], found that “enacted stigma” (the collective experience of systematic discrimination) was associated with multiple disordered eating phenotypes such as binge eating, fasting, and vomiting. Subsequent studies have confirmed internalized trans- and homophobia as risk factors for EDs [ 26 ]. Underlying facets of body image and shape concerns as risk factors for EDs may differ dramatically between transgender and cisgender individuals [ 26 , 27 ]. Alignment with specific gender presentations may present as a key motivation for disordered eating [ 26 , 27 , 28 , 29 ]; for example, the desire to suppress menstruation through restriction and excessive exercise has been observed in transgender men [ 27 , 30 ].
What we know and do not know about ED genetics relative to gender and sexual orientation
Genetic studies have identified both shared and distinct genetic risk factors across sexes. For example, female relatives of men with AN have an elevated crude relative risk of AN (20.3) [ 31 ], implying at least some shared genetic risk. However, studies comparing same- and opposite-sex twins found that only 50% of the genetic risk for ED behaviors was shared between the sexes, with females having a higher loading of genetic risk [ 32 ]. Heritability patterns also differ developmentally: twin studies of boys and young men estimate ~50% heritability across pre-pubescence, adolescence, and into adulthood; whereas, heritability among girls and young women was undetectable (~0%) until puberty, reaching 50% only in adulthood [ 33 ]. More recent studies have leveraged genetic correlation analyses to examine sex-specific relationships between AN and anthropometric traits. For example, AN and body fat percentage (BF%) are more highly genetically correlated among females than among males [ 34 , 35 ], and partitioned heritability analyses of SNP-h 2 showed that BF% female was significantly enriched for CNS tissue while BF% male was enriched for adipose tissue [ 35 ].
No explicit research exists on the genetic risk of EDs among LGBTQIA+ individuals, though we can reasonably assume that many of the same genetic influences on EDs are acting on these individuals as cisgender and heterosexual individuals, although environmental risk factors may differ. What is essential for ED genetic studies is that these individuals are included and unique risk factors that contribute to their experience of EDs are considered and assessed.
It is overly simplistic to conclude that AN and anthropometric traits have different genetic risk factors between men and women. Such an interpretation ignores the historical bias in ED research. Because diagnostic guidelines were developed and tailored to the presentation of EDs in women and girls, assessment instruments likely have differential accuracy and sensitivity according to sex and gender [ 36 ]. Moreover, heritability and expression of a trait do not occur in a vacuum. Diagnosis of a disorder (and consequent inclusion in research) is representative not just of genetics and downstream biology, but of a constellation of social and environmental exposures, including ED risk factors, but also vigilance of caregivers and clinicians to ED symptoms, and access to appropriate treatment. Similarly, studies of anthropometric traits will likely be confounded by gendered societal pressure for thinness, such that women are exposed to higher rates of bullying, shame, and pressure to lose weight. These factors might account for the brain-specific heritability of body fat percentage in women [ 34 ]. Such considerations are key to introducing equity into studies of EDs, and will be notable throughout our discussions not just of gender, but of race and ethnicity, age of onset, and socio-economic status. Finding ways to address, account for, or remove these factors will be key to furthering our understanding of EDs.
EDs affect people of all races and ethnicities
Ed prevalence across races and ethnicities.
The limited available data from population-based studies report few racial or ethnic differences in the prevalence of EDs among adults, although results are inconsistent. Nationally representative studies in the US report no significant racial or ethnic differences in the prevalence of AN, BN, or BED [ 8 ], although more recent studies report significantly lower lifetime prevalence of AN among Black and Hispanic/Latinx participants [ 37 ], higher prevalence of BN among Hispanic/Latinx adolescents [ 38 ], and higher prevalence of general ED pathology among American Indian/Alaskan Native and Hispanic/Latinx college students [ 39 ]. There have been few representative, population-based studies of ED prevalence outside of the U.S., Europe, and Australasia. The World Health Organization World Mental Health surveys reported prevalence estimates for BN and BED from 14 countries, including Columbia (0.4% BN, 0.9%, BED), Brazil (2.0% BN, 4.7% BED), Mexico (0.8% BN, 1.6% BED), Romania (0.0% BN, 0.2% BED), Belgium (1.0% BN, 1.2% BED), France (0.7% BN, 1.7% BED), Germany (0.3% BN, 0.5% BED), Italy (0.1% BN, 0.7% BED), the Netherlands (0.9% BN, 0.9% BED), New Zealand (1.3% BN, 1.9% BED), Northern Ireland (0.5% BN, 1.5% BED), Portugal (0.8% BN, 2.4% BED), Spain (0.7% BN, 0.8% BED), and the U.S. (1.0% BN, 2.6% BED) [ 40 ]. A 2013 review of prevalence investigations of EDs included studies from the World Mental Health surveys, the U.S., Western Europe, Latin America, South Korea, and New Zealand. The authors reported that the pooled prevalence of lifetime EDs was higher among Western countries (1.29%) compared to the South Korean sample (0.21%) [ 41 ]. A review of epidemiological studies of EDs in African countries found that most included relatively small community or student samples. No cases of AN were reported. The pooled prevalence of BN was 0.87%, and the pooled prevalence of Eating Disorders Not Otherwise Specified was 4.45% [ 42 ].
Furthermore, studies have reported differing prevalence of component symptoms of binge eating, purging, body dissatisfaction, and fear of weight gain across races and ethnicities. For example, Asian men and women with EDs tend to exhibit lower fear of fatness [ 43 , 44 , 45 ], a key DSM-5 diagnostic criterion, as well as higher levels of thin ideal internalization compared to European Americans and African Americans [ 46 ], possibly influencing ED prevalence estimates among Asian men and women.
Detection and referral and assessment of EDs in diverse populations
Differences in prevalence estimates may reflect that people of color are less likely to be diagnosed with an ED, to seek treatment, and to be referred for specialist treatment [ 10 , 13 , 14 ]. As outlined in the section on gender and sexual orientation, historical biases in ED research have yielded diagnostic schema and treatment guidelines based on very specific presentations. Diagnoses and guidelines may disproportionately address clinical features expected in a prototype white cisgender female patient, reducing applicability across racial and ethnic groups. Similarly, cultural differences in environmental exposures and racial/ethnic differences in ED symptomatology are rarely captured by existing ED assessments. Studies using established assessments are able to say whether individuals report standard symptoms, but inadequately address unique symptoms or risk factors that may characterize the illnesses across diverse groups—again potentially hampering knowledge and perpetuating health disparities.
What we know and do not know about ED genetics relative to race and ethnicity
It is widely known that complex trait genetics has focused overwhelmingly on individuals of European ancestry [ 47 , 48 ], including over 90% of individuals in psychiatric genetics GWAS [ 49 ]. Large GWAS of non-Europeans (e.g., the PAGE consortium [ 50 ]) have enabled trans-ancestry fine-mapping and led to discovery of novel disease-associated genes, even using substantially smaller sample sizes [ 50 , 51 ]. Although relatively underpowered, multi-ancestry sequencing studies of schizophrenia indicate that rare variant burdens are similar across ancestries [ 52 ]. The success of cross-ancestry GWAS and sequencing studies in these traits shows the promise of trans-ancestry fine-mapping loci using diverse cohorts and may increase the likelihood that causal variants can be found [ 49 , 50 , 51 ]. Although early work on candidate genes, genome-wide microsatellite studies, and replications emerged from Japan [ 2 , 53 , 54 ], subsequent AN GWAS have been restricted to European-ancestry populations. Although large diverse samples are not yet available in EDs, this is poised to change as the ED Working Group of the Psychiatric Genomics Consortium (PGC-ED) has highlighted diversification of samples and engagement of international researchers as a priority [ 55 ].
EDs affect individuals across the lifespan
EDs affect people of all ages [ 15 ], although symptoms, presentation and prevalence may change over the lifespan. As with gender and race, a historical focus on a specific presentation (i.e., young girls and women) may have introduced age bias into diagnostic criteria, assessment instruments, and treatment guidelines. Across the lifespan, disparate genetic and environmental risk factors may underlie superficially similar ED behaviors. Investigating genetic factors underlying motivations and emotions related to EDs, as well as specific behaviors and anthropometric phenotypes across the lifespan may provide novel insights into the psychiatric and metabolic causes and mechanisms underlying EDs.
EDs in youth
Disordered eating behaviors occur in young children, but can differ in clinical presentation. For example, “avoidant/restrictive food intake disorder (ARFID)” [ 56 ] occurs in 1.5–3.2% of children and adolescents [ 57 , 58 ], and is characterized by food restriction for a variety of non-weight related reasons, including sensory sensitivities (e.g., texture aversions), fear of choking or vomiting (i.e., phobic avoidance), or low interest in food and low appetite [ 59 ]. The restriction associated with ARFID does not include fear of weight gain or body dysmorphia [ 59 ] as in AN. Similarly, loss-of-control eating (LOC), a clear precursor to binge eating [ 60 ] occurs in more than one quarter of children with overweight or obesity [ 61 ], and is characterized by feeling unable to control what or how much one is eating [ 62 , 63 ]. Although both ARFID and LOC can occur alone, they also commonly co-occur with other psychiatric disorders. The risk of LOC is elevated in children with ADHD [ 64 ], anxiety [ 65 , 66 ], and in children who have experienced weight-related bullying [ 67 ], and the risk of ARFID is elevated among children with autism spectrum disorder [ 68 ], and vice-versa [ 69 ]. Moreover, both LOC and ARFID exhibit complex relationships with metabolic factors: for example, youth with LOC who showed greater anxiety had higher leptin levels [ 65 ] and more frequent metabolic syndrome [ 66 ]. The extent to which these childhood presentations are precursors for later AN, BN, and BED is not entirely clear; however, ongoing developmental research aims to characterize developmental continuities and discontinuities in EDs.
EDs in midlife and beyond
EDs that occur in midlife and beyond can represent persistent cases, relapsing cases in individuals with initial onset in childhood or adolescence, or most uncommonly, new onset cases [ 70 ]. The requirement for an extremely low BMI in AN diagnosis likely biases toward a younger cohort, as BMI naturally increases with age [ 71 , 72 ], perhaps explaining patterns of earlier AN incidence (peaking at 16 [ 73 ]) compared to Other Specific Feeding and Eating Disorder (OSFED; peak 18–30 [ 73 ]). Further, inclusion of amenorrhea in diagnostic criteria naturally biases clinicians towards people who menstruate i.e., missing pre-pubertal and post-menopausal females and males. EDs do, however, occur in midlife and beyond. In fact, Eating Disorder Examination-Questionnaire (EDE-Q) scores among women do not decline until after age 54, whereas scores in men peak at ages 55–64 [ 74 ]. Further, 15.7% of respondents aged 40–60 have clinically meaningful EDE-Q scores [ 75 ], and 13% of women aged 50+ report at least one core ED symptom [ 76 ]. Moreover, familiar factors are cited as contributors, including self-esteem [ 75 , 77 ], body dissatisfaction [ 78 , 79 ], BMI [ 79 , 80 ], perfectionism [ 78 ], and societal pressure for thinness [ 78 ].
What we know and do not know about ED genetics across the lifespan
Little is known about the genetic risk factors underlying ED onset at different ages. A recent GWAS examined genetic etiology of AN age-of-onset, and compared early onset (defined as <13 years of age) to typical-onset AN [ 81 ]. Distinct genetic risk factors were associated with early onset compared to typical onset, including a potentially causal correlation between younger age at menarche and early onset, and associations between typical age of onset and a range of anthropometric traits [ 81 ]. No explicit research exists on the genetics of age-of-onset in other EDs; nor have any studies to our knowledge investigated the genetics of later onset AN. However, given the shared and distinct features of EDs across the lifespan, including age-diverse samples will be essential to capture context- and developmentally-specific differences in environmental and genetic risk factors.
EDs affect individuals across socioeconomic groups
EDs affect individuals at all socioeconomic status (SES) levels. However, individuals with lower SES are less likely to receive screening or treatment for EDs and thus remain underrepresented among clinical samples [ 82 ], particularly in the U.S. Although early findings suggested that AN was associated with higher SES [ 83 ], a more recent systematic review of U.S. and Europe community and population-based studies concluded that EDs are not disorders of affluence [ 84 ]. Further, in a cohort of two million men and women in Sweden, a country with free or low-cost healthcare, an ED diagnosis was associated with parent education but not income after adjusting for education, suggesting that SES was not systematically associated with seeking healthcare for EDs [ 85 ]. Little is known regarding associations between EDs and SES in non-Western countries, likely due to the paucity of prevalence studies as discussed earlier. For example, in the 2010 Global Burden of Disease study, regions other than North American had poor coverage of epidemiological data on EDs [ 86 ]. In the aforementioned World Mental Health surveys, only one country (Columbia) was considered low-income, while the other 13 countries were upper-middle to high-income [ 40 ]. However, this study did not statistically compare prevalence across countries. In a study of National Health Insurance data from Taiwan, which includes 99% of the Taiwanese population, findings indicated that the incidence and prevalence of EDs had increased over the previous decade. However, estimates were lower than those obtained from community samples, suggesting that factors other than treatment affordability may have impacted treatment-seeking in this sample [ 87 ].
Other factors related to lower SES may be associated with increased risk for EDs. Some studies in U.S. samples have found evidence that food insecurity or insufficiency is associated with BED and BN [ 88 , 89 ], while stress and childhood adversity are associated with ED symptoms, further underscoring the need to ensure that individuals across the SES spectrum are represented in ED studies and treatment settings [ 90 , 91 ].
What we know and do not know about ED genetics and SES
Indicators of SES, including education, social deprivation, and household income, have heritable components [ 92 ], and studies have revealed genetic correlations between SES and psychiatric disorders [ 93 ]. A recent study found that SES was positively genetically correlated with AN [ 94 ]. Partitioning out the genetic SES variance resulted in reduced genetic variation for AN, and reduced genetic cross-trait associations among psychiatric disorders [ 94 ]. These results emphasize the importance of controlling for SES in order to reduce bias in estimates of genetic variance. A twin study revealed that neighborhood disadvantage was associated with increased disordered eating in girls across all stages of pubertal development, and the expected pubertal increases in genetic influences on disordered eating were only observed in girls from advantaged backgrounds [ 95 ]. Genetic influences on disordered eating were potentiated much earlier for girls living in disadvantaged contexts, suggesting interplay between genetic risk and SES.

EDs affect individuals of all body shapes and weights
Disproportionate attention to AN has obscured the fact that EDs occur in individuals of all body shapes and sizes. Although low BMI is required for a diagnosis of AN, BN can occur in individuals across the BMI spectrum, and BED occurs in individuals with typical and higher weight bodies. The DSM-5 now recognizes atypical AN (AAN) in which individuals meet all diagnostic criteria for AN including weight loss but do not present with low weight [ 20 , 96 ]. AAN has been associated with poor nutritional and medical status secondary to weight loss [ 97 ], poor quality of life [ 98 ], premorbid overweight and obesity [ 99 ], and history of weight-based teasing [ 100 ]. Despite this, individuals with AAN are less likely than those with AN to be screened for and to receive treatment [ 101 , 102 ]. Considerably more work is required to understand the full array of presentations of AAN across the diverse populations highlighted in this review.
What we know and do not know about ED genetics relative to body shape and weight
Genetic research has addressed body shape and weight in three ways. First, GWAS have highlighted shared genetic factors between AN and body shape and weight, including negative genetic correlations between AN and body fat percentage ( r = −0.36), fat mass ( r = −0.33), BMI ( r = −0.32), waist to hip ratio (r = −0.2), hip circumference ( r = −0.2) and waist circumference ( r = −0.24) [ 1 ], suggesting that many of the same genes that increase risk for AN also contribute to these anthropometric traits. However, existing GWAS have focused exclusively on AN in individuals with low BMIs, leaving individuals with EDs in larger bodies unstudied (although such studies are underway). Second, applying polygenic risk scores (PRS) in biobank data demonstrates that AN-PRS are associated with weight loss, even among adults who have never been diagnosed with AN [ 103 ]. Further, while AN, BN, and BED have similar psychiatric trait associations, they diverge in their associations with metabolic and anthropometric traits [ 104 ]. Although AN and anthropometric measures are negatively correlated, BED is significantly positively associated with several body shape and weight measures, suggesting that BMI-associated genomic variants are broadly relevant for all three EDs, but may act in opposite directions [ 104 ]. Third, phenome-wide association studies (PheWAS) showed that AN-genes are associated with anthropometric traits (including lowest recorded weight and weight change over time) in a clinical cohort with no history of AN; further, AN-gene associations with chronic pain, substance use and cholesterol levels were mediated by BMI [ 5 ].
In addition, genetic research has the potential to shed light on the extent to which restrictive EDs in individuals with larger bodies (i.e., AAN) are genetically similar to AN. Comparing GWAS of AN and AAN could inform nosology and shed light on whether it is actually appropriate (from a genetic perspective) to label this presentation as a form of AN. Divergent results could inform whether AN and AAN share the same underlying genetics and only differ in BMI or represent genetically distinct syndromes.
Large-scale approaches to address diversity in ED genetics
In the Section “Background”, we outlined ways in which stereotypes and misconceptions have biased our understanding of and research on EDs. Here, we suggest five overarching foci to improve the applicability of genetic research on EDs to the full spectrum of afflicted individuals (Fig. 2 ).

Here we diagram the broad goals and specific actions we propose to address and the current challenges in eating disorder research. More detailed descriptions of the challenges and recommended actions are addressed in this review.
Broader and more inclusive recruitment
As there is no guarantee that the same genetic and environmental factors influence risk for EDs across demographic groups, innovative practices are essential to ensure representation of individuals of diverse ancestry, gender and sexual orientation, age, SES, and body sizes. Strategies to recruit and retain diverse participants have been discussed in detail elsewhere [ 105 ], but several core points warrant emphasis. First, participants report that seeing themselves represented in study personnel and in recruitment materials and websites increases interest in participation. Likewise, participants who share their personal stories about being from a minoritized group and suffering from an ED can help reduce shame and encourage participation. A clear explanation of why representation is important can also help potential participants decide to volunteer. Many fear that researchers desire for inclusivity is simply to tick a demographic checkbox, but feel more inclined to participate when they learn that their participation will contribute to ensuring that any treatments that emerge from the science will be relevant to others who share their background. Understanding the actual downstream implications of participation can be a powerful incentive to join a study. Finally, engaging participants in the process from the earliest phases of study design (i.e., co-design [ 106 ]) and providing regular updates about the study progress (websites, blogs) creates a sense of ownership and community that allows participants to feel like part of a larger team.
Building capacity
The ED research workforce is overwhelmingly white, which is also true for the ED genetics workforce. Building capacity to diversify the workforce has to start early in the educational trajectory. Recruiting interested individuals into science, technology, engineering and mathematics (STEM) as early as middle school (~ages 11–14) and engaging them in research related to eating, body composition, nutrition, psychology, psychiatry, and EDs will ensure a more diverse workforce in the future. Moving away from a purely sociocultural theory of ED etiology will engage more individuals interested in science (including genetics) and encourage more research on the biology of EDs.
Restructuring diagnostic guidelines and disease nosology
A recurring theme in Part 1 was the extent to which the narrow focus on young white thin females with AN in both research and in lay circles has shaped and biased the diagnostic schema, instruments, and research conclusions in the ED field. This restricted perspective has considerable downstream implications—from individuals outside of this stereotype who are neither detected nor referred for treatment, to who volunteers to participate in studies, to the conclusions that are drawn from samples that are mostly of European ancestry. The bias is compounding because any findings from these samples only serve to reinforce existing stereotypes about disease prevalence and presentation. Failure to include people of color and of size, other genders, and children and older people in our research studies severely limits our understanding. Moving the field forward will require a careful reconsideration of disease nosology and treatment guidelines. Guidelines should be restructured to consider differing presentations, behaviors, environmental risk factors, and psychological drivers, bearing in mind that many of the marginalized identities discussed in this review are intersectional, meaning that diagnostic criteria need to be flexible and applicable simultaneously to many different groups and presentations.
Researchers should also attend to nomenclature used outside of the DSM and ICD that often emerges from traditional and social media to describe dysfunctional eating behavior. Popular terms like disordered eating, body dysmorphia, food addiction, orthorexia, and relative energy deficiency in sport (previously female athlete triad) often capture trends in the population that describe what people are actually experiencing. The breadth in naming and lack of parallel to current treatment guidelines presents a variety of challenges. First, by using the above terms in the medical literature without defined criteria, we exacerbate challenges in clinical translation, as findings related to disordered eating might not easily be applied to a patient with AN or BN presenting to clinic. Second, we may unknowingly exclude historically marginalized groups who might find one of the above terms to be more representative of their lived experience. For example, if an individual identifies with a diagnosis of body dysmorphia, but researchers only recruit patients with atypical AN, we may miss including that participant and others like them. Lastly, the ED field suffers from chronic underfunding due in part to a dilution of recognition of the true prevalence of the disorders and resulting public health impact [ 107 ]. By addressing the many names and experiences lived with ED we can improve treatment access to the public and improve funding and discovery in research.
Success in this area will require a multi-pronged approach. First, the creation and deployment of more broadly useful screening tools and questionnaires should include opportunities to describe symptoms and behaviors falling outside stereotyped expectations for each condition; should not include BMI stratification or BMI-based inclusion/exclusion criteria; and should be appropriate cross-culturally.
Researchers should also explore alternative or additional phenotyping approaches that rely on observed behaviors, specific symptoms, and digital phenotyping. Other examples include electronic-health record-based phenotype inference [ 108 , 109 , 110 ] or analysis of specific reported symptoms and behaviors from population and biobank studies. However, we caution that these approaches are also susceptible to bias; creating phenotype algorithms without first interrogating any assumptions and implicit biases risks automating inequalities [ 11 , 111 ]. For example, a previous study used 18 ICD codes to identify potential AN cases in a large healthcare system [ 71 ], selecting positive cases for further chart review. However, 6/18 codes related or referred to menstruation (despite the demonstrated ineffectiveness of amenorrhea as a diagnostic criterion [ 112 , 113 , 114 , 115 ]), substantially biasing the sample towards people who menstruate.
Researchers should leverage insights from genetic studies to reshape disease nosology. Novel analytical approaches such as pathway-based PRS, transcriptomic imputations, and incorporating electronic and longitudinal health records afford researchers an unprecedented opportunity to study disease on an individual rather than population level. Such analyses might allow researchers to infer molecular subtypes of disease, identifying for example clinically-relevant subgroups associated with specific molecular signatures. Alternatively, these analyses might reveal that clinically distinct presentations are not rooted in genetic differences, rather stemming from societal or environmental exposures. Any assessment of environmental risk factors or correlates must account for the broad range of experiences that individuals with EDs from diverse backgrounds might have. Beyond the historical focus on the societal thin ideal, space must be made for assessing main effects of group-specific or shared factors (e.g., weight-based stigmatization or discrimination, food insufficiency, teasing and bullying, race-based discrimination) as well as gene x environment interplay. Understanding these disparate presentations, behaviors and symptoms will also represent a significant step towards personalizing treatment options, effectively identifying interventions and therapies that match specific symptoms and behaviors.
More sophisticated analytical approaches to refine phenotype-genotype associations
Although there are substantial insights to be gained from larger, more inclusive GWAS of AN, it is imperative that we expand our analytical approaches, adopting cutting edge statistical techniques in order to more fully elucidate the genetic architecture of EDs. Elegant and intentional study design may increase our power to understand disease as much as increasing sample size.
Substantial attention should be paid to approaches that can identify shared and distinct associations between ED diagnoses, or within disorders between subtypes. Explicit comparison of cases between psychiatric disorders has previously been shown to elucidate disorder-specific genic associations [ 116 ]. As such, genetic studies that compare and contrast AN and BN, for example, might increase our power to detect genetic correlates of shared and distinct symptoms and behaviors. These studies might include joint analysis across subtypes; case-case GWAS that explicitly compare individuals with different ED subtypes; PRS or LDScore approaches, or next generation analytical approaches such as genomic structural equation modeling (SEM). Further, these studies may also bring us closer to clinical utility: the diagnostic challenge for a clinician is rarely ‘whether’ an individual will develop a disorder: rather, the challenge is to identify the correct diagnosis among several similar possibilities, or to predict disease prior to onset. For this goal, differentiating AN from BN will be more useful than AN from controls.
Researchers should also investigate the role of potentially clinically relevant endophenotypes. For example, comparing genetic risk factors across the lifespan may elucidate relationships with specific biological pathways and mechanisms. Studies of younger cohorts may reveal the role of metabolic and hunger/satiety dysregulation in AN, whilst examining ED onset in older cohorts may elucidate specifically the role of psychiatric pathways. Investigating these groups may also yield insights into the role of hormones associated with menarche and menopause to ED pathology through BMI and/or body dissatisfaction [ 117 ]. A secondary analysis of a genome-wide association study of AN with 9,335 cases and 31,981 controls found that early-onset AN was significantly genetically correlated with younger age at menarche, and Mendelian randomization analysis supported a causal link between younger age at menarche and early-onset AN [ 81 ]. Further work needs to be completed to determine the hormonal relationship between estrogen fluctuations, appetite and satiety hormones, BMI, body satisfaction, and psychiatric phenotypes.
Researchers should also undertake approaches that can identify clinical consequences of genetic associations. For example, phenome-wide association studies (PheWAS) test for associations between genetic risk factors and the full patient phenome, including diagnostic records, reactions to medications, substance use/abuse, and longitudinal trajectories. These approaches might be particularly useful in disentangling whether specific comorbidities occur due to genetic pleiotropy (i.e., shared genetic underpinnings), healthcare pleiotropy (i.e., due to common mis-diagnosis, or as common ‘stops’ on a diagnostic trajectory), or due to diagnostically meaningful overlap.
Expand insights beyond genotype, towards biology and environmental interactions
Approaches that rely on genotype alone will ultimately be limited in the potential for translational and clinical insights. A full dissection of potential functional genomics approaches and integrative analyses is outside the scope of this review, and indeed has been explored in detail elsewhere [ 118 , 119 , 120 , 121 , 122 ]. However, we caution that researchers must consider factors beyond genetics in their interpretations of GWAS and consequent associations. Failure to consider the biological, environmental, and societal contexts under which genetic studies are conceived, recruited, and analyzed risks mis-interpreting or over-interpreting the relevance of our findings, and potentially entrenching bias and stereotypes throughout our research. Put simply, expanding our samples and approaches will be pointless if we do not also consider carefully all the implications of our findings.
We should be wary of over-interpreting differential heritability, correlations, or relative lack of genome-wide associations between two groups. For example, it might be tempting to interpret differential heritability between sexes as explaining sex differences in ED diagnoses. However, genetic associations are only as good as the phenotypes we provide; researchers should consider that phenotyping instruments might have differential power; diagnostic contamination might occur at different rates; disease severity might be substantially different between groups; and study participation rates may differ dramatically. If indeed researchers identify true sex-specific effects (or other differential associations across groups) that are not confounded by diagnostic differences, it is important not to default to assumptions of genetic essentialism [ 22 ]. Instead, the next step must be to consider how these interact with biology and environment to cause disease; for example, considering the effects of specific variants on hormone biology, age at menarche, or related factors that might influence ED development. Understanding the role of these environmental contexts will be key in pinpointing appropriate treatments in differing life stages and contexts, and perhaps in understanding why some treatments are less effective in certain patient groups.
Consideration of the impact of societal factors is also essential. These may include exposure to stress and early life adversity; access to therapy and/or healthcare; access to healthy foods and opportunities for exercise; and support networks of family and friends. On the surface these factors are not genetic; however, it is likely that they correlate with genetic factors, as evidenced for example by recent GWAS of SES [ 94 , 123 ] and loneliness [ 124 ]. Most obviously, healthcare access differs substantially among countries, and will likely influence disease trajectory, diagnostic rates, and study participation. Even within countries, systemic racism prevents equal access to early life support, healthcare services and referrals to specialists, and may increase exposure to a variety of disease risk factors [ 11 , 12 , 111 , 125 , 126 , 127 , 128 , 129 , 130 , 131 , 132 ]. These factors may confound our studies, with the degree of confounding significantly correlated with genetic factors. As such, we might expect our GWAS and genetic studies to be differentially powered across ancestries, as increased environmental risks in one group might decrease our ability to detect genetic associations [ 11 ]. These issues should be borne in mind when interpreting GWAS associations and underscore the need to collect large and diverse GWAS samples.
Finally, we note that expanding inclusion within our studies is vital to equity in research and clinical care. The ability to participate in studies and research, and access to the findings and benefits of that research, should be equally available to all. Increasing diversity will inarguably increase our insight and understanding of ED biology, and indeed of psychiatric disease genetics more broadly; however, the goal of inclusion and equity alone is a sufficient motivator. Research conclusions that emerge from the study of a narrow and privileged subset of individuals with EDs and the treatment approaches they generate overestimate our actual understanding of disease and further perpetuate already damaging health disparities. This work is both hard and expensive, but must be a priority to replace myths with facts and to sharpen our understanding of EDs.
Watson HJ, Yilmaz Z, Thornton LM, Hübel C, Coleman JRI, Gaspar HA, et al. Genome-wide association study identifies eight risk loci and implicates metabo-psychiatric origins for anorexia nervosa. Nat Genet. 2019;51:1207–14.
CAS PubMed PubMed Central Google Scholar
Boraska V, Franklin CS, Floyd JAB, Thornton LM, Huckins LM, Southam L, et al. A genome-wide association study of anorexia nervosa. Mol Psychiatry. 2014;19:1085–94.
Duncan L, Yilmaz Z, Gaspar H, Walters R, Goldstein J, Anttila V, et al. Significant locus and metabolic genetic correlations revealed in genome-wide association study of anorexia nervosa. Am J Psychiatry. 2017;174:850–8.
Huckins LM, Hatzikotoulas K, Southam L, Thornton LM, Steinberg J, Aguilera-Mckay F, et al. Investigation of common, low-frequency and rare genome-wide variation in anorexia nervosa. Mol Psychiatry. 2018;23:1169–80.
Johnson JS, Cote AC, Dobbyn A, Sloofman LG, Xu J, Cotter L, et al. Mapping anorexia nervosa genes to clinical phenotypes. Psychol Med. 2022:1–15. https://doi.org/10.1017/S0033291721004554 Epub ahead of print.
Nine Truths About Eating Disorders—Academy for Eating Disorders. https://www.aedweb.org/publications/nine-truths . Accessed 30 December 2021.
Schaumberg K, Welch E, Breithaupt L, Hübel C, Baker JH, Munn-Chernoff MA, et al. The science behind the academy for eating disorders’ nine truths about eating disorders. Eur Eat Disord Rev. 2017;25:432–50.
PubMed PubMed Central Google Scholar
Hudson JI, Hiripi E, Pope HG, Kessler RC. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biol Psychiatry. 2007;61:348–58.
PubMed Google Scholar
Strother E, Lemberg R, Stanford SC, Turberville D. Eating disorders in men: underdiagnosed, undertreated, and misunderstood. Eat Disord. 2012;20:346–55.
Sonneville KR, Lipson SK. Disparities in eating disorder diagnosis and treatment according to weight status, race/ethnicity, socioeconomic background, and sex among college students. Int J Eat Disord. 2018;51:518–26.
CAS PubMed Google Scholar
Dueñas HR, Seah C, Huckins LM. Implicit bias of encoded variables: Frameworks for addressing structured bias in EHR data. Hum Mol Genet. 2020;29:R33–41.
Seah C, Dueñas HR, Huckins LM Characterising racism in psychiatric diagnoses using EHR. In Prep. 2020.
Becker AE, Franko DL, Speck A, Herzog DB. Ethnicity and differential access to care for eating disorder symptoms. Int J Eat Disord. 2003;33:205–12.
Marques L, Alegria M, Becker AE, Chen C, Fang A, Chosak A, et al. Comparative prevalence, correlates of impairment, and service utilization for eating disorders across US ethnic groups: Implications for reducing ethnic disparities in health care access for eating disorders. Int J Eat Disord. 2011;44:412–20.
Bulik CM. Towards a science of eating disorders: Replacing myths with realities: The fourth Birgit Olsson lecture. Nord J Psychiatry. 2016;70:224–30.
Kamody RC, Grilo CM, Udo T. Disparities in DSM-5 defined eating disorders by sexual orientation among U.S. adults. Int J Eat Disord. 2020;53:278–87.
Watson RJ, Veale JF, Saewyc EM. Disordered eating behaviors among transgender youth: Probability profiles from risk and protective factors. Int J Eat Disord. 2017;50:515–22.
Nagata JM. Challenges, health implications, and advocacy opportunities for lesbian, gay, bisexual, and transgender global health providers. Glob Health Promot. 2018;25:70–3.
Rastogi R, Md ESR. Restrictive eating disorders in previously overweight adolescents and young adults. CCJM. 2020;87:165–71.
Google Scholar
Association AP. Diagnostic and Statistical Manual of Mental Disorders (DSM-5®). American Psychiatric Association Publications; 2013.
Garcia-Sifuentes Y, Maney DL. Reporting and misreporting of sex differences in the biological sciences. ELife 2021;10:e70817.
Miyagi M, Guthman EM, Sun SD-K, Transgender rights rely on inclusive language. Science. 2021. 24 December 2021. https://doi.org/10.1126/science.abn3759 .
Galmiche M, Déchelotte P, Lambert G, Tavolacci MP. Prevalence of eating disorders over the 2000-2018 period: a systematic literature review. Am J Clin Nutr. 2019;109:1402–13.
Lavender JM, Brown TA, Murray SB. Men, muscles, and eating disorders: an overview of traditional and muscularity-oriented disordered eating. Curr Psychiatry Rep. 2017;19:32.
Anderson CB, Bulik CM. Gender differences in compensatory behaviors, weight and shape salience, and drive for thinness. Eat Behav. 2004;5:1–11.
Bell K, Rieger E, Hirsch JK. Eating disorder symptoms and proneness in gay men, lesbian women, and transgender and gender non-conforming adults: Comparative Levels and a proposed mediational model. Front Psychol. 2019;9:2692.
Parker LL, Harriger JA. Eating disorders and disordered eating behaviors in the LGBT population: a review of the literature. J Eat Disord. 2020;8:51.
McGuire JK, Doty JL, Catalpa JM, Ola C. Body image in transgender young people: Findings from a qualitative, community based study. Body Image. 2016;18:96–107.
Becker I, Nieder TO, Cerwenka S, Briken P, Kreukels BPC, Cohen-Kettenis PT, et al. Body image in young gender dysphoric adults: A European multi-center study. Arch Sex Behav. 2016;45:559–74.
Coelho JS, Suen J, Clark BA, Marshall SK, Geller J, Lam P-Y. Eating disorder diagnoses and symptom presentation in transgender youth: A scoping review. Curr Psychiatry Rep. 2019;21:107.
Strober M, Freeman R, Lampert C, Diamond J, Kaye W. Males with anorexia nervosa: a controlled study of eating disorders in first-degree relatives. Int J Eat Disord. 2001;29:263–9.
Baker JH, Maes HH, Lissner L, Aggen SH, Lichtenstein P, Kendler KS. Genetic risk factors for disordered eating in adolescent males and females. J Abnorm Psychol. 2009;118:576–86.
Klump KL, Culbert KM, Slane JD, Burt SA, Sisk CL, Nigg JT. The effects of puberty on genetic risk for disordered eating: evidence for a sex difference. Psychol Med. 2012;42:627–37.
Hübel C, Gaspar HA, Coleman JRI, Finucane H, Purves KL, Hanscombe KB, et al. Genomics of body fat percentage may contribute to sex bias in anorexia nervosa. Am J Med Genet B Neuropsychiatr Genet. 2019;180:428–38.
Hübel C, Gaspar HA, Coleman JRI, Hanscombe KB, Purves K, Prokopenko I, et al. Genetic correlations of psychiatric traits with body composition and glycemic traits are sex- and age-dependent. Nat Commun. 2019;10:5765.
Gallagher KA, Sonneville KR, Hazzard VM, Carson TL, Needham BL. Evaluating gender bias in an eating disorder risk assessment questionnaire for athletes. Eat Disord. 2021;29:29–41.
Udo T, Grilo CM. Prevalence and correlates of DSM-5-defined eating disorders in a nationally representative sample of U.S. adults. Biol Psychiatry. 2018;84:345–54.
Swanson SA, Crow SJ, Le Grange D, Swendsen J, Merikangas KR. Prevalence and correlates of eating disorders in adolescents. Results from the National Comorbidity Survey Replication adolescent supplement. Arch Gen Psychiatry. 2011;68:714–23.
Burke NL, Hazzard VM, Karvay YG, Schaefer LM, Lipson SK, Rodgers RF. Eating disorder prevalence among multiracial US undergraduate and graduate students: Is multiracial risk different than the sum of each identity? Eat Behav. 2021;41:101501.
Kessler RC, Berglund PA, Chiu WT, Deitz AC, Hudson JI, Shahly V, et al. The prevalence and correlates of binge eating disorder in the World Health Organization World Mental Health Surveys. Biol Psychiatry. 2013;73:904–14.
Qian J, Hu Q, Wan Y, Li T, Wu M, Ren Z, et al. Prevalence of eating disorders in the general population: a systematic review. Shanghai Arch Psychiatry. 2013;25:212–23.
van Hoeken D, Burns JK, Hoek HW. Epidemiology of eating disorders in Africa. Curr Opin Psychiatry. 2016;29:372–7.
Lee S, Ng KL, Kwok K, Fung C. The changing profile of eating disorders at a tertiary psychiatric clinic in Hong Kong (1987–2007). Int J Eat Disord. 2010;43:307–14.
Lee S, Ng KL, Kwok KPS, Thomas JJ, Becker AE. Gastrointestinal dysfunction in Chinese patients with fat-phobic and nonfat-phobic anorexia nervosa. Transcult Psychiatry. 2012;49:678–95.
Nakai Y, Nin K, Teramukai S, Taniguchi A, Fukushima M, Wonderlich SA. Typical and atypical anorexia nervosa in a Japanese sample. Int J Eat Disord. 2014;47:130–7.
Cheng ZH, Perko VL, Fuller- Marashi L, Gau JM, Stice E. Ethnic differences in eating disorder prevalence, risk factors, and predictive effects of risk factors among young women. Eat Behav. 2019;32:23–30.
Popejoy A, Fullerton S. Genomics is failing on diversity. Nature 2016;538:161–4.
Bustamante CD, De La Vega FM, Burchard EG. Genomics for the world. Nature 2011;475:163–5.
Peterson RE, Kuchenbaecker K, Walters RK, Chen C-Y, Popejoy AB, Periyasamy S, et al. Genome-wide association studies in ancestrally diverse populations: Opportunities, methods, pitfalls, and recommendations. Cell 2019;179:589–603.
Wojcik GL, Graff M, Nishimura KK, Tao R, Haessler J, Gignoux CR, et al. Genetic analyses of diverse populations improves discovery for complex traits. Nature 2019;570:514–8.
Highland HM, Wojcik GL, Graff M, Nishimura KK, Hodonsky CJ, Baldassari AR, et al. Predicted gene expression in ancestrally diverse populations leads to discovery of susceptibility loci for lifestyle and cardiometabolic traits. Am J Hum Genet. 2022;109:669–79.
Liu D, Meyer D, Fennessy B, Feng C, Cheng E, Johnson JS, et al. Rare schizophrenia risk variant burden is conserved in diverse human populations. medRxiv:2022.01.03.22268662.
Ando T, Tamura N, Mera T, Morita C, Takei M, Nakamoto C, et al. Association of the c.385C>A (p.Pro129Thr) polymorphism of the fatty acid amide hydrolase gene with anorexia nervosa in the Japanese population. Mol Genet Genom Med. 2014;2:313–8.
CAS Google Scholar
Nakabayashi K, Komaki G, Tajima A, Ando T, Ishikawa M, Nomoto J, et al. Identification of novel candidate loci for anorexia nervosa at 1q41 and 11q22 in Japanese by a genome-wide association analysis with microsatellite markers. J Hum Genet. 2009;54:531–7.
Eating Disorders. Psychiatric Genomics Consortium. https://www.med.unc.edu/pgc/pgc-workgroups/eating-disorders/ . Accessed 29 December 2021.
Attia E, Becker AE, Bryant-Waugh R, Hoek HW, Kreipe RE, Marcus MD, et al. Feeding and eating disorders in DSM-5. Am J Psychiatry. 2013;170:1237–9.
Eddy KT, Thomas JJ, Hastings E, Edkins K, Lamont E, Nevins CM, et al. Prevalence of DSM-5 avoidant/restrictive food intake disorder in a pediatric gastroenterology healthcare network. Int J Eat Disord. 2015;48:464–70.
Kurz S, van Dyck Z, Dremmel D, Munsch S, Hilbert A. Early-onset restrictive eating disturbances in primary school boys and girls. Eur Child Adolesc Psychiatry. 2015;24:779–85.
Seetharaman S, Fields EL. Avoidant/restrictive food intake disorder. Pediatr Rev. 2020;41:613–22.
Vannucci A, Nelson EE, Bongiorno DM, Pine DS, Yanovski JA, Tanofsky-Kraff M. Behavioral and neurodevelopmental precursors to binge-type eating disorders: support for the role of negative valence systems. Psychol Med. 2015;45:2921–36.
He J, Cai Z, Fan X. Prevalence of binge and loss of control eating among children and adolescents with overweight and obesity: An exploratory meta-analysis. Int J Eat Disord. 2017;50:91–103.
Kelly NR, Shank LM, Bakalar JL, Tanofsky-Kraff M. Pediatric feeding and eating disorders: current state of diagnosis and treatment. Curr Psychiatry Rep. 2014;16:446.
Byrne ME, LeMay-Russell S, Tanofsky-Kraff M. Loss-of-control eating and obesity among children and adolescents. Curr Obes Rep. 2019;8:33–42.
Reinblatt SP, Mahone EM, Tanofsky-Kraff M, Lee-Winn AE, Yenokyan G, Leoutsakos J-MS, et al. Pediatric loss of control eating syndrome: Association with attention-deficit/hyperactivity disorder and impulsivity. Int J Eat Disord. 2015;48:580–8.
Byrne ME, Tanofsky-Kraff M, Jaramillo M, Shank LM, LeMay-Russell S, Rubin SG, et al. Relationships of trait anxiety and loss of control eating with serum leptin concentrations among youth. Nutrients 2019;11:E2198.
Byrne ME, Tanofsky-Kraff M, Kelly NR, Grammer AC, Jaramillo M, Mi SJ, et al. Pediatric loss-of-control eating and anxiety in relation to components of metabolic syndrome. J Pedia Psychol. 2019;44:220–8.
Rubin AG, Schvey NA, Shank LM, Altman DR, Swanson TN, Ramirez E, et al. Associations between weight-based teasing and disordered eating behaviors among youth. Eat Behav. 2021;41:101504.
Farag F, Sims A, Strudwick K, Carrasco J, Waters A, Ford V, et al. Avoidant/restrictive food intake disorder and autism spectrum disorder: clinical implications for assessment and management. Dev Med Child Neurol. 2021. 17 August 2021. https://doi.org/10.1111/dmcn.14977 .
Inoue T, Otani R, Iguchi T, Ishii R, Uchida S, Okada A, et al. Prevalence of autism spectrum disorder and autistic traits in children with anorexia nervosa and avoidant/restrictive food intake disorder. Biopsychosoc Med. 2021;15:9.
Micali N, Martini MG, Thomas JJ, Eddy KT, Kothari R, Russell E, et al. Lifetime and 12-month prevalence of eating disorders amongst women in mid-life: a population-based study of diagnoses and risk factors. BMC Med. 2017;15:12.
Gordon-Larsen P, Adair LS, Nelson MC, Popkin BM. Five-year obesity incidence in the transition period between adolescence and adulthood: the National Longitudinal Study of Adolescent Health. Am J Clin Nutr. 2004;80:569–75.
Viner RM, Cole TJ. Who changes body mass between adolescence and adulthood? Factors predicting change in BMI between 16 year and 30 years in the 1970 British Birth Cohort. Int J Obes. 2006;30:1368–74.
Javaras KN, Runfola CD, Thornton LM, Agerbo E, Birgegård A, Norring C, et al. Sex- and age-specific incidence of healthcare-register-recorded eating disorders in the complete swedish 1979-2001 birth cohort. Int J Eat Disord. 2015;48:1070–81.
Hilbert A, de Zwaan M, Braehler E. How frequent are eating disturbances in the population? Norms of the eating disorder examination-questionnaire. PLoS One. 2012;7:e29125.
Drobnjak S, Atsiz S, Ditzen B, Tuschen-Caffier B, Ehlert U. Restrained eating and self-esteem in premenopausal and postmenopausal women. J Eat Disord. 2014;2:23.
Gagne DA, Von Holle A, Brownley KA, Runfola CD, Hofmeier S, Branch KE, et al. Eating disorder symptoms and weight and shape concerns in a large web-based convenience sample of women ages 50 and above: Results of the gender and body image (GABI) study. Int J Eat Disord. 2012;45:832–44.
Matz PE, Foster GD, Faith MS, Wadden TA. Correlates of body image dissatisfaction among overweight women seeking weight loss. J Consult Clin Psychol. 2002;70:1040–4.
Midlarsky E, Nitzburg G. Eating disorders in middle-aged women. J Gen Psychol. 2008;135:393–408.
Hrabosky JI, Grilo CM. Body image and eating disordered behavior in a community sample of Black and Hispanic women. Eat Behav. 2007;8:106–14.
McLean SA, Paxton SJ, Wertheim EH. Factors associated with body dissatisfaction and disordered eating in women in midlife. Int J Eat Disord. 2010;43:527–36.
Watson HJ, Thornton LM, Yilmaz Z, Baker JH, Coleman JR, Adan RA, et al. Common genetic variation and age at onset of anorexia nervosa. Biol Psychiatry: GOS. 2021. https://doi.org/10.1016/j.bpsgos.2021.09.001 .
Kazdin AE, Fitzsimmons-Craft EE, Wilfley DE. Addressing critical gaps in the treatment of eating disorders. Int J Eat Disord. 2017;50:170–89.
McClelland L, Crisp A. Anorexia nervosa and social class. Int J Eat Disord. 2001;29:150–6.
Huryk KM, Drury CR, Loeb KL. Diseases of affluence? A systematic review of the literature on socioeconomic diversity in eating disorders. Eat Behav. 2021;43:101548.
Goodman A, Heshmati A, Koupil I. Family history of education predicts eating disorders across multiple generations among 2 million Swedish males and females. PLOS ONE. 2014;9:e106475.
Baxter AJ, Patton G, Scott KM, Degenhardt L, Whiteford HA. Global epidemiology of mental disorders: what are we missing? PLoS One. 2013;8:e65514.
Tsai M-C, Gan S-T, Lee C-T, Liang Y-L, Lee L-T, Lin S-H. National population-based data on the incidence, prevalence, and psychiatric comorbidity of eating disorders in Taiwanese adolescents and young adults. Int J Eat Disord. 2018;51:1277–84.
Lydecker JA, Grilo CM. Food insecurity and bulimia nervosa in the United States. Int J Eat Disord. 2019;52:735–9.
Rasmusson G, Lydecker JA, Coffino JA, White MA, Grilo CM. Household food insecurity is associated with binge-eating disorder and obesity. Int J Eat Disord. 2019;52:28–35.
Blodgett Salafia EH, Lemer JL. Associations between multiple types of stress and disordered eating among girls and boys in middle school. J Child Fam Stud. 2012;21:148–57.
Hazzard VM, Bauer KW, Mukherjee B, Miller AL, Sonneville KR. Associations between childhood maltreatment latent classes and eating disorder symptoms in a nationally representative sample of young adults in the United States. Child Abus Negl. 2019;98:104171.
Hill WD, Hagenaars SP, Marioni RE, Harris SE, Liewald DCM, Davies G, et al. Molecular genetic contributions to social deprivation and household income in UK Biobank. Curr Biol. 2016;26:3083–9.
Anttila V, Bulik-Sullivan B, Finucane HK, Walters RK, Bras J, Duncan L, et al. Analysis of shared heritability in common disorders of the brain. Science. 2018. 2018. https://doi.org/10.1126/science.aap8757 .
Marees AT, Smit DJA, Abdellaoui A, Nivard MG, van den Brink W, Denys D, et al. Genetic correlates of socio-economic status influence the pattern of shared heritability across mental health traits. Nat Hum Behav. 2021;5:1065–73.
Mikhail ME, Carroll SL, Clark DA, O’Connor S, Burt SA, Klump KL. Context matters: Neighborhood disadvantage is associated with increased disordered eating and earlier activation of genetic influences in girls. J Abnorm Psychol. 2021;130:875–85.
Moskowitz L, Weiselberg E. Anorexia nervosa/atypical anorexia nervosa. Curr Probl Pediatr Adolesc Health Care. 2017;47:70–84.
Garber AK, Cheng J, Accurso EC, Adams SH, Buckelew SM, Kapphahn CJ, et al. Weight loss and illness severity in adolescents with atypical anorexia nervosa. Pediatrics 2019;144:e20192339.
Pauls A, Dimitropoulos G, Marcoux-Louie G, Singh M, Patten SB, Psychological characteristics and childhood adversity of adolescents with atypical anorexia nervosa versus anorexia nervosa. Eat Disord. 2020:1–13.
Sawyer SM, Whitelaw M, Le Grange D, Yeo M, Hughes EK. Physical and psychological morbidity in adolescents with atypical anorexia nervosa. Pediatrics 2016;137:e20154080.
Matthews A, Kramer RA, Mitan L. Eating disorder severity and psychological morbidity in adolescents with anorexia nervosa or atypical anorexia nervosa and premorbid overweight/obesity. Eat Weight Disord. 2022;27:233–42.
Kennedy GA, Forman SF, Woods ER, Hergenroeder AC, Mammel KA, Fisher MM, et al. History of overweight/obesity as predictor of care received at 1-year follow-up in adolescents with anorexia nervosa or atypical anorexia nervosa. J Adolesc Health. 2017;60:674–9.
Harrop EN, Mensinger JL, Moore M, Lindhorst T. Restrictive eating disorders in higher weight persons: A systematic review of atypical anorexia nervosa prevalence and consecutive admission literature. Int J Eat Disord. 2021;54:1328–57.
Xu J, Johnson JS, Eating Disorders Working Group of the Psychiatric Genomics Consortium, Birgegård A, Jordan J, Kennedy MA, et al. Exploring the clinical consequences and genetic aetiology of adult weight trajectories. In press: Lancet Digital Health.
Hübel C, Abdulkadir M, Herle M, Loos RJF, Breen G, Bulik CM, et al. One size does not fit all. Genomics differentiates among anorexia nervosa, bulimia nervosa, and binge-eating disorder. Int J Eat Disord. 2021;54:785–93.
MacDermod C, Pettie MA, Carrino EA, Cruz Garcia S, Padalecki S, Finch JE, et al. Recommendations to encourage participation of individuals from diverse backgrounds in psychiatric genetic studies. Am J Psychiatric Genet Part B: Neuropsychiat Genet. in press.
InsideOut Institute. Australian Eating Disorders Research & Translation Strategy. 2021.
Social and economic cost of eating disorders in the US | Deloitte Australia | Deloitte Access Economics. Deloitte Australia. https://www2.deloitte.com/au/en/pages/economics/articles/social-economic-cost-eating-disorders-united-states.html . Accessed 22 December 2021.
Lebovitch DS, Johnson JS, Dueñas HR, Huckins LM Phenotype risk scores: moving beyond ‘cases’ and ‘controls’ to classify psychiatric disease in hospital-based biobanks. medRxiv. 2021:2021.01.25.21249615.
Bastarache L, Hughey JJ, Hebbring S, Marlo J, Zhao W, Ho WT, et al. Phenotype risk scores identify patients with unrecognized Mendelian disease patterns. Science. 2018;359:1233–9.
Wendt FR, Pathak GA, Deak JD, De Angelis F, Koller D, Cabrera-Mendoza B, et al. Using phenotype risk scores to enhance gene discovery for generalized anxiety disorder and posttraumatic stress disorder. Mol Psychiatry. 2022. https://doi.org/10.1038/s41380-022-01469-y .
Eubanks V AUTOMATING INEQUALITY How High-Tech Tools Profile, Police, and Punish the Poor. St. Martin’s Press; 2018.
Garfinkel PE, Lin E, Goering P, Spegg C, Goldbloom D, Kennedy S, et al. Should amenorrhoea be necessary for the diagnosis of anorexia nervosa? Evidence from a Canadian community sample. Br J Psychiatry. 1996;168:500–6.
Poyastro Pinheiro A, Thornton LM, Plotonicov KH, Tozzi F, Klump KL, Berrettini WH, et al. Patterns of menstrual disturbance in eating disorders. Int J Eat Disord. 2007;40:424–34.
Abraham SF, Pettigrew B, Boyd C, Russell J, Taylor A. Usefulness of amenorrhoea in the diagnoses of eating disorder patients. J Psychosom Obstet Gynaecol. 2005;26:211–5.
Attia E, Roberto CA. Should amenorrhea be a diagnostic criterion for anorexia nervosa? Int J Eat Disord. 2009;42:581–9.
Ruderfer DM, Ripke S, McQuillin A, Boocock J, Stahl EA, Pavlides JMW, et al. Genomic dissection of bipolar disorder and schizophrenia, including 28 subphenotypes. Cell. 2018;173.
Baker JH, Runfola CD. Eating disorders in midlife women: A perimenopausal eating disorder? Maturitas 2016;85:112–6.
Cano-Gamez E, Trynka G. From GWAS to function: Using functional genomics to identify the mechanisms underlying complex diseases. Front Genet. 2020;11:424.
Young H, Cote AC, Huckins LM Chapter 17: Integration with systems biology approaches and -omics data to characterize risk variation. Psychiatric Genomics, vol. 1, Elsevier; 2022.
Townsley KG, Brennand KJ, Huckins LM. Massively parallel techniques for cataloguing the regulome of the human brain. Nat Neurosci. 2020;23:1509–21.
Sullivan PF, Geschwind DH. Defining the genetic, genomic, cellular, and diagnostic architectures of psychiatric disorders. Cell 2019;177:162–83.
Gallagher MD, Chen-Plotkin AS. The Post-GWAS era: from association to function. Am J Hum Genet. 2018;102:717–30.
Wendt FR, Pathak GA, Lencz T, Krystal JH, Gelernter J, Polimanti R. Multivariate genome-wide analysis of education, socioeconomic status and brain phenome. Nat Hum Behav. 2021;5:482–96.
Gao J, Davis LK, Hart AB, Sanchez-Roige S, Han L, Cacioppo JT, et al. Genome-wide association study of loneliness demonstrates a role for common variation. Neuropsychopharmacology 2017;42:811–21.
Brodie N, Perdomo JE, Silberholz EA. The dual pandemics of COVID-19 and racism: impact on early childhood development and implications for physicians. Curr Opin Pediatr. 2021;33:159–69.
Landon BE, Onnela J-P, Meneades L, O’Malley AJ, Keating NL. Assessment of racial disparities in primary care physician specialty referrals. JAMA Netw Open. 2021;4:e2029238.
Williams DR, Lawrence JA, Davis BA, Vu C. Understanding how discrimination can affect health. Health Serv Res. 2019;54(Suppl 2):1374–88.
Ahmad NJ, Shi M. The need for anti-racism training in medical school curricula. Acad Med. 2017;92:1073.
Noble SU, Algorithms of oppression: how search engines reinforce racism. New York: New York University Press; 2018.
APA’s Apology to Black, Indigenous and People of Color for its support of structural racism in psychiatry. https://www.psychiatry.org/newsroom/apa-apology-for-its-support-of-structural-racism-in-psychiatry . Accessed 8 May 2021.
What is environmental racism and how can we fight it? World Economic Forum. https://www.weforum.org/agenda/2020/07/what-is-environmental-racism-pollution-covid-systemic/ . Accessed 8 May 2021.
Khan S, Mian A. Racism and medical education. Lancet Infect Dis. 2020;20:1009.
Download references
Acknowledgements
LMH is supported by NIMH (R01MH118278; R01MH124839); NIEHS (R01ES033630); the Klarman Family Foundation (2019 Eating Disorders Research Grants Program); the Seaver Family Foundation. JJ is supported by the NIMH (R01MH118278) and the Klarman Family Foundation (2019 Eating Disorders Research Grants Program). RS is supported by the Klarman Family Foundation (2019 Eating Disorders Research Grants Program). CMB is supported by NIMH (R01MH120170; R01MH124871; R01MH119084; R01MH118278; R01 MH124871); Brain and Behavior Research Foundation Distinguished Investigator Grant; Swedish Research Council (Vetenskapsrådet, award: 538-2013-8864); Lundbeck Foundation (Grant no. R276-2018-4581). YKW reports funding from International Society of Nurses in Genetics (ISONG).
Open access funding provided by Karolinska Institute.
Author information
Authors and affiliations.
Pamela Sklar Division of Psychiatric Genomics, Icahn School of Medicine at Mount Sinai, New York, NY, 10029, USA
Laura M. Huckins, Rebecca Signer & Jessica Johnson
Department of Psychiatry, Icahn School of Medicine at Mount Sinai, New York, NY, 10029, USA
Laura M. Huckins & Rebecca Signer
Department of Genetics and Genomic Sciences, Icahn School of Medicine at Mount Sinai, New York, NY, 10029, USA
Icahn Institute for Genomics and Multiscale Biology, Icahn School of Medicine at Mount Sinai, New York, NY, 10029, USA
Laura M. Huckins
Seaver Autism Center for Research and Treatment, Icahn School of Medicine at Mount Sinai, New York, NY, 10029, USA
Mental Illness Research, Education and Clinical Centers, James J. Peters Department of Veterans Affairs Medical Center, Bronx, NY, 14068, USA
School of Nursing, University of North Carolina at Chapel Hill, Chapel Hill, NC, USA
Department of Psychiatry, University of North Carolina at Chapel Hill, Chapel Hill, NC, USA
Ya-Ke Wu & Cynthia M. Bulik
National Center for PTSD at VA Boston Healthcare System, Boston, MA, USA
Karen S. Mitchell
Department of Psychiatry, Boston University School of Medicine, Boston, MA, USA
Department of Medical Epidemiology and Biostatistics, Karolinska Institutet, Stockholm, Sweden
Cynthia M. Bulik
Department of Nutrition, University of North Carolina at Chapel Hill, Chapel Hill, NC, USA
You can also search for this author in PubMed Google Scholar
Contributions
LMH drafted portions of manuscript, coordinated sections, and approved figures and final draft; RS; drafted portions of manuscript, created figures, and approved final draft; JJ drafted portions of manuscript, created figures and cover image, and approved final draft; Y-KW drafted portions of manuscript and approved figures and final draft; KM drafted portions of manuscript and approved figures and final draft; CMB: drafted portions of manuscript and approved figures and final draft.
Corresponding author
Correspondence to Cynthia M. Bulik .
Ethics declarations
Competing interests.
LMH, JJ, RS, KM, and Y-KW declare no conflicts of interest. CMB reports: Shire/Takeda (Grant recipient, Scientific Advisory Board member); Idorsia (consultant); Lundbeckfonden (grant recipient); Pearson (author, royalty recipient); Equip Health Inc. (Clinical Advisory Board).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Huckins, L.M., Signer, R., Johnson, J. et al. What next for eating disorder genetics? Replacing myths with facts to sharpen our understanding. Mol Psychiatry 27 , 3929–3938 (2022). https://doi.org/10.1038/s41380-022-01601-y
Download citation
Received : 31 December 2021
Revised : 20 April 2022
Accepted : 26 April 2022
Published : 20 May 2022
Issue Date : October 2022
DOI : https://doi.org/10.1038/s41380-022-01601-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Cookies on the NHS England website
We’ve put some small files called cookies on your device to make our site work.
We’d also like to use analytics cookies. These send information about how our site is used to a service called Google Analytics. We use this information to improve our site.
Let us know if this is OK. We’ll use a cookie to save your choice. You can read more about our cookies before you choose.
Change my preferences I'm OK with analytics cookies
First Episode Rapid Early Intervention for Eating Disorders (FREED)
There are two key things that can prevent early intervention in eating disorders: difficulties spotting the illness early, and difficulties in accessing help. FREED has made its aim to address both sets of difficulties.
Services across the country using the FREED model provide rapid, specialised treatment for young people with a recent onset eating disorder (anorexia nervosa, bulimia nervosa, binge eating disorder or another eating disorder). The FREED model gives special attention to challenges young people face during these critical years of their life as they transition to adulthood, making it much more effective than traditional service models at reversing the changes to brain, body and behaviour caused by eating disorders. As a result, young people are less likely to miss out on study, relationships and other opportunities because of their illness.
George moved to London when she was 21 and shares how her eating disorder worsened as she moved to the capital on her own. After persuasion from her family, George visited the GP who referred her to an eating disorders service delivering the FREED programme. Within two weeks, George was meeting with a psychologist for a Cognitive Behavioural Therapy (CBT) session. George was with the service for 18 months and recognises the service not only supported her to manage her eating disorder but also with other challenges she had to face: having surgery, changing jobs, moving homes and acclimatising to the new city.
George said: “My treatment was completely tailored to me and my lifestyle. After my treatment was finished, I left the programme so optimistic and grateful for everything they had given me.”
The FREED model is highly recommended by patients and families and is associated with substantial improvements in clinical outcomes and cost-savings through reduction in hospital admissions.
Having been designed to reduce barriers and improve access to treatment for the 16- 25s, it provides a truly equitable and specific early intervention eating disorder treatment pathway (duration of less than 3 years) for all of young people and families within the service.
Sue shares her experience of the FREED programme as it helped support her 18-year old daughter who was the first person outside of London to use the programme in her local eating disorder service. Sue noted how her daughter was a bit apprehensive at first, but she built a genuine bond with her psychotherapist. Sue witnessed how the support from FREED was having a positive change to her daughter’s approach to food and exercise. From the dedication from her support worker, to the involvement of the dietician, Sue watched her daughter’s life and eating disorder improve.
“I totally trusted the professionals involved in my daughter’s FREED experience and that’s what helped me help her. Without any question FREED should be seen as the gold standard of eating disorders care.”
The focus on early intervention works towards removing disparities in perceived diagnosis and need for treatment. The promotion of the early intervention pathway, with the proactive community outreach is hoped to assist those from a Black and Minority Ethnic background to feel more confident to come forward for help.
An anonymous service user shared: “I was knocking on doors for two years before I got here, passed from service to service. I think they just didn’t believe black girls had eating disorders, so I started to think maybe it was all in my head until I got here [FREED] and got help”
The COVID-19 pandemic has affected everyone across the country but the need for support and care for young people with an eating disorder has not been forgotten.
Psychological therapies, care and support have been delivered remotely to ensure people can still access the support they need. Innovation is happening across the service with increases in access to remote treatments, comprehensive remote group programmes and workshops and seminars to ensure outreach.
Over 1200 young people have been and are being supported by FREED programmes across the country to date, it has more important than ever to ensure that those who need help, can get it.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Environ Res Public Health

Social Media, Thin-Ideal, Body Dissatisfaction and Disordered Eating Attitudes: An Exploratory Analysis
Pilar aparicio-martinez.
1 Departamento de Enfermería, Universidad de Córdoba, Campus de Menéndez Pidal, 1470 Córdoba, Spain
2 Usher Institute of Population Health Sciences and Informatics, University of Edinburgh, Edinburgh EH8 9YL, UK
3 Grupo Investigación epidemiológica en Atención primaria (GC-12) del Instituto Maimónides de Investigación Biomédica de Córdoba (IMIBIC), Hospital Universitario Reina Sofía, 14071 Córdoba, Spain; se.ocu@oreuqavm
Alberto-Jesus Perea-Moreno
4 Departamento de Física Aplicada, Universidad de Córdoba, ceiA3, Campus de Rabanales, 14071 Córdoba, Spain; se.ocu@aerepa (A.-J.P.-M.); se.ocu@pijam1af (M.P.M.-J.)
María Pilar Martinez-Jimenez
María dolores redel-macías.
5 Departamento Ingeniería Rural, Ed Leonardo da Vinci, Campus de Rabanales, Universidad de Córdoba, Campus de Excelencia Internacional Agroalimentario, ceiA3, 1470 Cordoba, Spain; se.ocu@lederdm
Claudia Pagliari
6 eHealth Research Group, Usher Institute of Population Health Sciences and Informatics, University of Edinburgh, Edinburgh EH8 9YL, UK; [email protected]
Manuel Vaquero-Abellan
Disordered eating attitudes are rapidly increasing, especially among young women in their twenties. These disordered behaviours result from the interaction of several factors, including beauty ideals. A significant factor is social media, by which the unrealistic beauty ideals are popularized and may lead to these behaviours. The objectives of this study were, first, to determine the relationship between disordered eating behaviours among female university students and sociocultural factors, such as the use of social network sites, beauty ideals, body satisfaction, body image and the body image desired to achieve and, second, to determine whether there is a sensitive relationship between disordered eating attitudes, addiction to social networks, and testosterone levels as a biological factor. The data ( N = 168) was obtained using validated surveys (EAT-26, BSQ, CIPE-a, SNSA) and indirect measures of prenatal testosterone. The data was analysed using chi-square, Student’s t-test, correlation tests and logistic regression tests. The results showed that disordered eating attitudes were linked to self-esteem ( p < 0.001), body image ( p < 0.001), body desired to achieve ( p < 0.001), the use of social media ( p < 0.001) and prenatal testosterone ( p < 0.01). The findings presented in this study suggest a relationship between body image, body concerns, body dissatisfaction, and disordered eating attitudes among college women.
1. Introduction
Mental health problems have increased, especially among young people, over the last decade [ 1 ]. The most common mental problems are behavioural, emotional, and hyperkinetic disorders. Among these illnesses, disordered eating behaviours are rapidly increasing in a short time, especially among young women [ 2 , 3 ]. These disordered attitudes are defined as afflictions in which people suffer severe disruption in their eating behaviours, thoughts and emotions. The people who suffer from these complaints are usually preoccupied with food and weight. In this sense, disordered eating is used to describe a range of irregular eating behaviours that may or may not warrant a diagnosis of a specific disordered eating attitude [ 4 ].
These disorders usually occur in women in their twenties or during adolescence [ 3 ]. People who suffer these disorders usually present altered attitudes, behaviours, weight perception and physical appearance [ 5 ]. Moreover, disordered eating behaviours or attitudes are defined as unhealthy or maladaptive eating behaviours, such as restricting or binging and/or purging [ 6 ]. These behaviours are not categorized as an eating disorder, though they are considered a phase of diagnosed eating disorders [ 7 ].
The concern from health care systems is based on the fact that these severe mental disorders usually puts in danger the well-being and health of the people who suffer them [ 5 ]. One-third of the women in the world have suffered from these mental problems at some point in their life [ 6 ]. If they are inadequately treated, they may develop severe clinical disorders [ 8 ]. Moreover, around 1% of the people with these disordered eating attitudes struggle with unhealthy and emotional problems through all their lives [ 6 ].
Out of the population with disordered eating attitudes, 16% of them present overeating, 20% purged by vomiting, and 61% food restraining [ 9 ]. These frequencies changed as people aged, with food restriction being more common in older women and vomiting during adolescence [ 10 ]. Moreover, recent data have discussed the increase of how the minimum age of the people with disorders is around 12 years of age and decreasing. Meanwhile, the prevalence of disordered eating attitudes appears to increase as young adults or adolescents grow older [ 10 ].
Although these diseases have a crucial psychobiological component, social and cultural factors have a significant influence. Among these factors, advertising has been described as an internalizing or normalizing means to spread unrealistic beauty ideals. Therefore, a higher incidence of these diseases is presented in advanced and modern societies and people with the best living conditions, mostly caused by the popularization of thin and muscular ideals [ 11 , 12 , 13 ].
Several biological factors have been linked to disordered eating attitudes, with up to 50% of disordered eating being described as familiarly transmitted [ 5 , 14 ]. Researchers have also suggested that neurotransmitters in the brain are involved in disordered eating attitudes and, therefore, eating disorders [ 15 , 16 ]. Additionally, the hormones have been linked as factors to puberty, body perception and body concerns [ 17 , 18 ]. Testosterone is included among those hormones highly studied, with blood samples providing a more precise method of examination. Nevertheless, different researchers pointed out the possibility of using indirect markers to avoid taking biological samples and creating risks for the participants. In this sense, most studies have linked testosterone and estrogenic levels via the 2D:4D digital ratio as an indirect indicator [ 19 ], which heavily dictates attractiveness [ 17 ]. This ratio, which is based on the difference in length of the phalanges of the hands (2D:4D ratio) having a lower ratio as an indicator of the existence of a higher level of testosterone, is used for the determination of intrauterine testosterone levels during gestation [ 20 ]. This ratio has reflected the relationship with self-perception, body image, body dissatisfaction, and disordered eating behaviours [ 20 , 21 ]. Based on these studies, the hormone levels, and the indirect marker, might appear to have essential roles in disordered eating attitudes [ 22 ]. Nevertheless, other authors have described how biological or genetic factors are essential, but may not determine, these disordered eating attitudes [ 23 ].
Other factors, such as ethical or familiar factors, contribute to the development of this disordered eating behaviours [ 24 ]. In this sense, previous studies have established that the probability of developing a disordered eating attitude or a diagnosis of eating disorders is higher if the mother had a disordered eating or self-esteem problems [ 25 , 26 ]. Moreover, ethnicity has been linked to the perception of beauty ideals, self-esteem and body perception [ 27 , 28 ].
Another critical factor is the media by which beauty ideals have been promoted. The media plays a vital role in formulating what is attractive in society, increasing the thin beauty ideal among females being unattainable [ 29 , 30 ]. These ideals confirmed the way young people perceived themselves and, therefore, how they value themselves [ 10 , 31 ]. This contradiction between what society portrays as a role model and the real body that many young women have has resulted in body concerns. Body concerns usually maintain over time and increase body dissatisfaction. This body dissatisfaction emerges because of the distortion on the body image, its perception and, therefore, body concern [ 32 , 33 ]. This dissatisfaction also plays an essential role in disordered eating attitudes since it provokes emotional and psychological distress [ 34 ].
In this sense, the theory of social comparison and numerous studies have studied the relationship between body dissatisfaction and disordered eating attitudes to better understand the causes of these illnesses. These previous works showed that real comparisons with other people leads to a distortion of body image and may favour disorderly feeding [ 11 , 29 , 35 ]. Additionally, Fredrickson and Roberts (1997) suggested that sexualization and self-objectification promoted via media should be considered as a risk factor for disordered eating attitudes [ 36 , 37 , 38 ]. Based on previous and recent studies it seems that the role of the media in disordered eating attitudes is noteworthy [ 1 , 11 , 39 ].
This paper presents a research study in which these objectives have been pursued: first, to determine the relationship between disordered eating attitudes in female university students and sociocultural factors, such as the use of social network sites, beauty ideals, body satisfaction, the body image and the body image desired to achieve. Second, to determine whether there is a sensitive relationship between disordered eating attitudes, addiction to social networks, and other biological factors, such as testosterone levels.
2. Background
College-aged women may be at particular risk for body dissatisfaction and disordered eating practices due to the unhealthy weight gain that often occurs during this life stage [ 3 , 31 ]. The promotion of beauty ideals in the media disseminates disordered eating [ 40 , 41 ], drive for thinness and body dissatisfaction among female college students [ 42 ]. Furthermore, the growth of social networking sites (SNS), such as Facebook or Instagram, has also increased the exposure to thin and fit ideals [ 2 , 43 , 44 ]. The social media are more used than any other media as a mean of communication. These internet-based sites pulled the users to create personal profiles and share, view, comment and ‘like’ peer-generated content [ 20 ].
Importantly, young people, almost 90% of them (ages 18–29), reported being active users and being continuously exposed to different content and images in this medium [ 14 , 45 ]. Among the most active users of these media stands out the influencers. These new media role models have a significant impact in the last tendencies, the news and the trends that young people are following [ 46 ]. In this sense, researchers have also pointed out how social media and influencers may have the key to decrease body dissatisfaction and body concerns. Nevertheless, substantial studies have shown that economic interests are linked with the promotion of dieting in social media, or even surgery [ 47 ].
The last publications concluded that the most dangerous social media was Instagram, followed by Facebook and Twitter. These conclusions were based on the instant satisfaction of reviewing and having peer views in the images posted by the users [ 48 ]. Especially on Instagram, the message is accommodated according to the image uploaded [ 47 ].
These studies concluded that the influence of the advertising and the promotion of the thin and muscular ideals might more be connected with the perception that young people has regarding body, dieting and social media [ 49 ]. Additionally, the objectification suggests that the media’s sexual objectification of women modifies their body appearance. Due to this, it could be concluded that self-perception slowly shapes attractiveness resulting in a modification in the body-image, body dissatisfaction and disordered eating attitude. That being said, the proposed hypotheses are as follows:
Among young women, self-image will be linked to body dissatisfaction, the thin-ideal and the desire to change one’s body shape.
The level of body dissatisfaction among female college students will be high and be linked to self-esteem.
The young women’s eating behaviours will be linked to the degree of body dissatisfaction and the frequency of using social media.
The young women’s body image and body description will be slightly connected to prenatal testosterone levels.
3. Methodology
3.1. design and sample.
In the first phase, a cross-sectional study was carried out focused on female college students, aged from 18 to 25 years. The sample was recruited to participate in an in-person survey from April to May 2018 from the University of Cordoba. The selection of the sample was based on non-probability convenience sampling. This method of sampling was selected based on the accessibility of the students and previous scheduling with the professors.
The final sample was constituted by 168 subjects, from biological, education, informatics and nursing degrees who agreed to participate in the study voluntarily. The initial sample was 224, though the final sample was 168 after applying the exclusion terms. The mean age of the sample was 20 ± 0.76.
3.2. Measures
All the surveys used in the study are validated in different languages, including Spanish. Moreover, these surveys are used globally among health professionals and researchers in the health field [ 50 ].
The demographic and anthropometric data were not included in this study since the objective focused on the socio-cultural and individual factors. In this sense, the perception of young people was focused on social media, self-appearance, specific social network sites and distorted eating behaviours.
The EAT-26 with the reduced version of 26 items, was used to assess the frequency of disordered eating attitudes [ 51 , 52 ]. This test measures the low, medium and high risk of having a disordered eating attitude. Moreover, three different disordered eating behaviours can be reflected depending on the answers to each item. In this sense, these three subscales are dieting (focused on questions 1, 6, 7, 10, 11, 12, 14, 16, 17, 22, 23, 24, 26), bulimia and food preoccupation (focused on questions 3, 4, 9, 18, 21, 25) and food oral control (2, 5, 8, 13, 15, 8, 20). Total scores were calculated by taking the sum of the 26 items, based on the value from 0 to 3, where higher scores, over 20 points, indicated higher levels of disordered eating behaviours. This validated survey based on screening disorder eating attitudes when the score is over 20 points [ 52 ]. Nevertheless, this survey does not provide a definite diagnosis of eating disorders; therefore, a clinical evaluation is needed. This evaluation can be carried out via individual interviews.
The body satisfaction questionnaire (BSQ) [ 53 ], whose Spanish adaptation was completed by Raich [ 54 ], was used. The stereotypes perception survey from the University of Granada was also used [ 55 ].
The questions referring to body image included illustrations of women’s bodies. These illustrations comprise seven body images that vary from underweight to obese, numbered from 1 to 7. Additionally, a specific section focused on body satisfaction, examining their satisfaction on a scale from 1 to 7, with lower scores relating to higher levels of body dissatisfaction. In this section, one of the questions examined the steps each young person would take to attain a body type that corresponded to the ideal.
The body image concerns were observed by using the BSQ, a self-report instrument evaluating weight and shape preoccupations [ 54 ]. Sample items include: “Have you been so worried about your shape that you have felt you ought to diet?”; “Have you noticed the shape of others and felt that your shape compared unfavourably?” The questions were answered on a six-point Likert scale (1 = never, five = always).
The Appearance Evaluation (AE) subscale of the Multidimensional Body-Self Relations Questionnaire-Appearance Scales (MBSRQ) was used to measure self-perception and stereotypes [ 56 ]. Participants rate the extent to which they agree with seven statements (e.g., “Most people would consider me good-looking”) on a five-point scale (1 = disagree, 5 = agree) with lower scores indicating lower self-perception and stereotypes.
Finally, self-esteem was evaluated by the Rosenberg survey (CIPE-a) composed of ten questions, which provided us with high, medium or low levels of self-esteem. The questions were given a scale on a four-point scale (1 = disagree, 4 = agree), with lower scores indicating lower self-esteem [ 57 ].
On the other hand, the survey that focused on social networks had preliminary yes/no items about having social network accounts on Twitter, Facebook, Instagram, YouTube or Snapchat. Participants indicated how often they access/check their respective accounts daily on a five-point scale: hardly ever, sometimes, usually, all most all the time and always. Additionally, the participants’ daily use (hours per day in social networks and highly visual social media, i.e., Instagram, Snapchat), number of accounts and importance given to these was rated on a 1 (strongly disagree) to 5 (strongly agree) scale.
Meanwhile, addiction to social networks was evaluated by a validated survey called the Social Networks Addiction Questionnaire (SNSA) [ 50 ]. The survey is based on the DSM-IV-TR [ 27 ], a diagnostic instrument that does not recognize psychological addictions as disorders but as a prior stage that can lead to addiction. The survey is formed by 24 items applying a five-point rating system (from 0 to 4), taking into account the frequency from “never” to “always” [ 56 ].
The study has focused on the indirect determination of intrauterine testosterone levels during the gestation, determined experimentally from the difference in length of the phalanges of the hands (2D:4D ratio). This measure was selected to determine the possible relation with sociocultural factors indirectly. The selection of this method was based on reducing the risks, vulnerability and protecting biological or genetic material from the participants. When the ratio is higher, i.e., the difference between the second and fourth finger, lower levels of testosterone are implied [ 21 ]. 2D:4D is an indicator of testosterone and oestrogen levels [ 58 ], which heavily dictate attractiveness [ 17 ]. Therefore, this digit ratio may be related to self-perception, body image, body dissatisfaction and disordered eating attitudes.
3.3. Instruments
The instruments used to obtain the image of the hands were a Canon Camera EOS700D (produced by Canon Inc., which is a Japanese company founded in Ota, Tokyo) and a Manfrotto Compact Advance tripod (produced by Manfrotto, which is an Italian company founded in, produced and distributed form the USA). Additionally, free access software GeoGebra ( https://www.geogebra.org ), which is a free access software founded in Austria and later updated and mass produced in USA, was used to analyse the indirect marker of testosterone levels (2D:4D ratio).
3.4. Procedure
Participants approved a participant information statement, consent form and questionnaires, followed by the approval of the Research Ethics Committee of Public Health System in Cordoba (Ethical Approval number 273, reference 3773).
The participants were undergraduate students with health, education, life and engineering studies. The recruitment took place in different classrooms of the University, the objective of the study, ethical indications, risks for the participants and voluntary participation in the study being previously explained. During the recruitment a teacher and a researcher were present in the classroom the entire time.
The inclusion of the participants was based on an initial survey, which was provided previously in the same classroom. In this survey, the students were asked about the previous diagnosis of conduct or emotional disorders, addiction to technologies, abuse of substances and having a social network account. Those students that had a previous diagnosis of conduct, emotional disorders, or addiction were eliminated from the sample and were not given the survey of the study. Those students that did not have an account on any social network were also excluded from the study ( Figure 1 ).

Flow chart of the recruitment and selection of the sample.
3.5. Statistical Analysis
Mean and standard deviation (SD) were calculated for the quantitative variables and frequencies in the case of qualitative variables. Firstly, we studied the normalization of the data using the Kolmogorov-Smirnov test ( p < 0.05). Moreover, Cronbach’s alpha test was used for determining the consistency among the scales and subscales and, especially, the SNS test showed acceptable value (0.77) and the EAT-26 (0.83) was excellent. In order to assess the first objective, the χ 2 test was used for the qualitative variables, such as gender and body image, and the Student’s t -test was applied to compare quantitative variables, such as the EAT-26 score and age. Additionally, correlational analyses were used to examine relations between all variables.
Moreover, the second set of analyses examined the impact of the relationship between disordered eating attitudes and the rest the factors measured. For this purpose, the crude and adjusted odds ratio (OR) values were calculated for the logistic regression. In the end, the ROC (receiver operating characteristic) curves and the validity indices were used for the diagnostic accuracy of disordered eating attitudes having body dissatisfaction and social networks addiction.
First Phase
The initial analysis of the data showed that women ( N = 168) had a range of age between 21 and 22, 96.7% of them being Caucasian ethnicity. Moreover, the body image that they had was in range between 3 and 4, which may imply a normal weight. The perception that they had of themselves was fatter (3.56 ± 1.2) when compared to the desired body image (2.99 ± 0.83) ( Table 1 ). Additionally, the most common description of body satisfaction showed low and medium-high levels of body satisfaction (48.7%). In this sense, the difference among the group with lower and higher levels of body satisfaction was related to the body image given by the women (χ 2 = 113.64, p < 0.001).
Mean, standard deviation and confidence intervals.
| Factors Studied in Women | Mean (SD) | CI 95% |
|---|---|---|
| Self-image | 3.56 (1.2) | 3.38–3.75 |
| Disordered eating | 18.34 (10.7) | 16.70–19.97 |
| Self-description | 3.99 (0.98) | 3.84–4.14 |
| Body satisfaction | 4.32 (1.48) | 4.1–4.54 |
| Desired body image | 2.99 (0.83) | 2.86–3.12 |
| Method of change | 1.98 (0.82) | 1.76–2.01 |
| Zone to change | 3.37 (1.95) | 3.08–3.67 |
| Self-perception | 2.76 (0.89) | 2.62–2.89 |
| Stereotypes | 2.59 (0.75) | 2.48–2.71 |
| Self-esteem | 31.10 (4.7) | 30.3–31.8 |
| SNS addiction | 14.69 (10.37) | 13.11–16.26 |
| Use of social media | 3.13 (0.72) | 3.02–3.24 |
| Frequency of connections | 3.46 (0.92) | 4.32–3.6 |
| Duration of the connections | 3.2 (1.17) | 3.02–3.38 |
| Importance of social media | 2.8 (0.87) | 2.67–2.94 |
Moreover, the results from the data showed that almost 93% of the women desired to change at least three zones of their body using at least two different methods (1.98 ± 0.82). The methods most used were physical activity (92%), diet (48%), surgery (24%) and beauty or alimentary products (23%). Among the zones to be modified by a surgical procedure 68% of the women indicated breast implants.
The analysis of the results from the EAT-26 test showed that most of the women had a medium probability of having disordered eating attitudes (18.34 ± 10.7). Figure 2 reflects the frequency of the scores from the EAT-26 related to body satisfaction.

Results from the EAT-26 related to body satisfaction.
The figure displays a higher frequency of scores over 20 points in disordered eating behaviours in the lower points of the body satisfaction scale. This figure implies that there were more values over 20 points when women suffered higher levels of body dissatisfaction. Additionally, the analysis between the score in the disordered eating behaviour test and level of body satisfaction showed significant differences among individuals with low and high levels of body satisfaction and scores over 20 points in the EAT-26 (χ 2 = 375.34, p < 0.001). Moreover, a more in-depth analysis of the data, based on women with more than 20 points in the EAT-26, 48 out of 168 women showed that 40.81% had food oral control, 38.77% presented bulimia and food preoccupation and 20.5% dieting.
Further study of the data was carried out in order to address the possible correlations between the body image that women perceived of themselves and the other variables analysed. In Table 2 , the correlations between the body image and the different variables have shown significant value with numerous factors, including disordered eating attitudes, self-esteem, desired body image or number of methods. These correlations were positive for a fatter body image in higher scores in the EAT-26 and more methods used to modify the body image and the current body image. Moreover, negative correlations were found for a curvier description that the women gave about their body and higher desires for a thinner body image, higher body dissatisfaction and lower levels of self-esteem.
Correlations with body image that women perceived of themselves.
| Factors Studied in Women | Correlation | -Value |
|---|---|---|
| Disordered eating attitudes | 0.29 | <0.001 |
| Self-description | 0.72 | <0.001 |
| Body satisfaction | −0.39 | <0.001 |
| Desired image | −0.46 | <0.001 |
| Method of change | 0.22 | <0.01 |
| Self-perception | −0.38 | <0.001 |
| Stereotypes | 0.38 | <0.001 |
| Self-esteem | −0.34 | <0.001 |
| 2D:4D ratio | 0.17 | <0.05 |
Another variable that determines a “fatter” body image is the level of prenatal testosterone, measured by the 2D:4D ratio. This result displayed a positive relationship implying that a higher 2D:4D ratio, lower levels of intrauterine testosterone, may lead to a fatter body image.
On the other hand, Table 3 exposed the analysis of correlations between the score obtained in EAT-26 for disordered eating attitudes and the other factors analysed. This test displayed a negative correlation between having a higher score in the test and having lower levels of body satisfaction, self-esteem, the desired of having a thinner body image and worse perception of their own body.
Correlations with having higher scores in the disordered eating attitudes test.
| Factors Studied in Women | Correlation | -Value |
|---|---|---|
| Body Image | 0.32 | <0.001 |
| Self-description | 0.34 | <0.001 |
| Body satisfaction | −0.64 | <0.001 |
| Method of change | 0.37 | <0.01 |
| Self-perception | −0.38 | <0.001 |
| Stereotypes | 0.57 | <0.001 |
| Desired image | −0.19 | <0.05 |
| Zone to change | 0.35 | <0.001 |
| Self-esteem | −0.49 | <0.001 |
| Addiction to SNS | 0.18 | <0.05 |
| 2D:4D ratio | 0.41 | <0.001 |
Moreover, the positive correlations were obtained for numerous factors studied. The most highlighting positive correlations were reflected for a higher score in the SNS addiction test, a fatter body image and a higher difference in the 2D:4D ratio. These results implied that a higher 2D:4D ratio or fatter body image may lead to a higher score in the EAT-26.
The logistic regression model was used to define a disordered eating behaviour related to having lower levels of body satisfaction, the desired to achieve a thinner body image, lower levels of self-esteem, higher score in the SNS addiction test, higher duration of connection to this media and higher difference between the second and fourth finger ( Table 4 ).
Logistic regression for disordered eating attitudes.
| Non-Adjusted | Adjusted | |||||
|---|---|---|---|---|---|---|
| Factors Studied in Women | ED (Yes) | ED (No) | OR | CI | OR | CI |
| Body Dissatisfaction | 3.35 (1.48) | 4.73 (0.21) | 0.49 | 0.38–0.64 | 0.54 | 0.33–0.87 |
| Desired image | 2.76 (0.14) | 3.19 (0.07) | 0.56 | 0.37–0.83 | 0.24 | 0.11–0.52 |
| Stereotypes | 3.15 (0.69) | 2.35 (0.98) | 5.17 | 2.95–9.06 | 2.56 | 1.16–0.65 |
| Self-esteem | 2.80 (0.53) | 3.26 (0.39) | 0.10 | 0.043–0.24 | 0.15 | 0.04–0.63 |
| Addiction to SNS | 0.96 (0.11) | 0.68 (0.57) | 1.71 | 0.56–0.74 | 0.48 | 0.23–1.01 |
| Duration of the connections | 3.43 (0.17) | 3.03 (0.09) | 1.32 | 1.4–1.76 | 1.68 | 1.05–2.69 |
| Testosterone levels (2D:4D ratio) | 1.20 (0.79) | 0.6 (0.79) | 2.49 | 1.62–3.62 | 3.13 | 1.60–6.12 |
From the analysis based on levels of self-esteem and social networks, the results showed that most women have high levels of self-esteem (31.1 ± 4.7) and low levels of addictive behaviour to social network sites (14.69 ± 10.37). Furthermore, the results of the social network sites presented a high dispersion of the results. In this sense, the confidence intervals (95%) were focused on medium levels regarding addictive behaviour to SNS (13.11–16.26).
Based on this, the correlations for the score in the SNS addition test were studied. The results indicated positive significance for the number of methods used to change their body image (<0.001), higher desired of a thinner body ( p < 0.001), lower levels of self-esteem ( p < 0.001), greater number of social media accounts ( p < 0.001), longer duration of the connections ( p < 0.001) and the importance given to the social networks ( p < 0.001). Nevertheless, the difference between the second and fourth phalange (2D:4D ratio) showed no significance with scores in the social network addiction test.
Finally, based on the results from the logistic regression, a probabilistic model was obtained. This model could diagnose 42.9% of the population with disordered eating attitudes (R 2 Cox and Snell 0.429) by knowing if the person had scored high in the SNS addiction test, body image, body dissatisfaction and high desire of having a thinner body. The specificity (90.3), sensibility (68.9) and valid index (84.6) results were optimal. Finally, the curve of the model was analysed ( Figure 3 ) obtaining an acceptable probabilistic high risk of a disordered eating attitudes (area = 0.94, p < 0.001, CI 0.88–0.97).

ROC curve from the logistic model for disordered eating.
5. Discussion
This study has reflected how different factors, such as the level of self-esteem ( Table 1 ), might play a significant role in disordered eating behaviours. Among these factors the body image that women perceived over themselves stood out as a significant element. In this sense, according to previous researchers, body image is multidimensional, being made of perceptual, behavioural and cognitive-affective domains created by the individual [ 46 ]. This perception is dependent on a variety of elements, including social media and beauty ideals. In the case of social media, the results from this study showed a relationship between the body image, body ideals and the use of social media ( Table 2 and Table 3 ). Furthermore, previous publications explained that the desire to achieve the beauty ideal emerges as the internalization of the portrayed image exposed by the media [ 59 , 60 ]. Homan (2010) discussed how, among female college students, two principal beauty ideals coexist: the athletic-ideal and thin-ideal [ 61 ]. The internalization of the athletic-ideal predicts compulsive exercise [ 61 , 62 , 63 ]. Meanwhile, the thin-ideal internalization predicts food restriction and body dissatisfaction, both leading to disordered eating attitudes and possible origins for eating disorders [ 64 , 65 , 66 ]. These results confirm the association obtained between the desire of having a thinner body image and the use of the media since this media is the primary source to promote such ideals ( Table 3 ).
The issue resides on the fact that the thin-ideal produces a worse body image with a tendency toward frustration based on a fatter body image than desired. This concern among young women results in making different choices to obtain the desired image, such as surgery [ 67 , 68 ]. In this sense, the results from this paper also showed a high frequency of women determined to undergo plastic surgery to improve their image, being focused on breast surgery.
Notwithstanding, internalization of the fit-ideal has been studied as a predictor of the use of social media content related to health and fitness [ 69 , 70 ]. In this case, the fit ideal or athletic ideal may become a replacement for the other ideals, leading to healthier behaviour [ 71 ].
The results ( Table 2 ) have established that body dissatisfaction might be a potential agent in body image and desire to change this body image. These publications also accord with our earlier observations, which showed that levels of body dissatisfaction were associated with the desire of changing the body image in order to achieve a thinner body, especially using dieting [ 72 ]. Based on this, the results appear to match with previous works about how body dissatisfaction and body concerns in young women and teenagers may be related to disordered eating attitudes [ 27 , 73 ].
Another significant outcome was the link between body concerns, body dissatisfaction and levels of self-esteem ( Table 2 ). These data are in accord with recent investigations which connected body dissatisfaction and self-esteem to mental illness and the role of emotional distress in behavioural disorders [ 48 ].
Another study found that body dissatisfaction and disordered eating attitudes could be related to a high level of intrauterine testosterone, measured by the 2D:4D ratio. The prenatal masculinization has been established as a potential intermediate phenotype for the development of these disorders in their offspring [ 74 ]. Following these studies, the results obtained in this paper seem to initially match such conclusions ( Table 3 ) [ 75 ]. These results are partially consistent with the existing literature relating to dieting, alimentary products, such as supplements, negative affect, body dissatisfaction and the tendency to thinness [ 71 ]. Nevertheless, the results obtained regarding the hormonal levels may be related to the environmental conditions during the pregnancy more than the individual level of hormones [ 76 ].
The results of the study ( Table 4 ) have shown how social network sites might play an important role in disordered eating attitudes. In the study carried out by Cohen et al. (2018), the influence of the social networks was determined by the content and the selfies that the users upload to them more than by the assiduity of the connections [ 20 ]. This is partially contradictory to the present results in which the addiction to SNS and the duration of the connections were linked to weight loss and unhealthy dieting. These results match with previous studies in the sociocultural factors, not included among biological measures [ 77 , 78 ]. Withstanding, it is important to note that the regression model obtained in this study have shown the probable role of factors, such as the degree of body satisfaction, self-esteem, use of SNS and other measures, such as the 2D:4D ratio, related to disordered eating behaviours.
Additionally, SNS addiction, which has been related to other mental disorders [ 79 ], has shown correlation with stereotypes, self-esteem, method of change, thinner body image and the desired part of the body to change. In this sense, prior investigations proved the addiction to social media as cause–effect of disordered behaviours [ 80 , 81 ].
The present study raises the possibility that disordered eating attitudes in women might be conditioned by the influence of the ideals of beauty imposed by the social environment and to a lesser extent by the exposure to intrauterine levels of testosterone extracted from the 2D:4D ratio of the phalanges. It is possible, therefore, that disordered eating attitudes are multidimensional disorders produced by the media, hormones, and factors related to body concerns. Although this study has focused on Spanish college students, the results ( Table 2 and Figure 2 ) seem to match with previous works conducted in Caucasian women [ 82 , 83 ]. These studies seem to distant themselves from publications focused on Latina or African American young women or adolescents [ 84 , 85 ]. Nevertheless, it is possible, therefore, that because the study was carried out in Spanish college students, the results might not match university women from other countries.
Nevertheless, as with all research, the current findings need to be considered in light of possible limitations of the study. Therefore, biases and possibly incorrect data may have been included, and causal inferences cannot be drawn. Additionally, as with the majority of the body image literature, the current participants were university students, based on the sample and size of the sample caution is recommended in not generalizing these results to other samples or different samples. Nevertheless, these results seem to provide essential data regarding social media, disordered eating and the perception of the young people about themselves. Another limitation present in this study is the lack of inclusion of further cultural factors, such as the mother–child relationship, and anthropometric data, such as BMI.
All being said, the results from this manuscript and the comparison with previous works suggest how the initial hypothesis has been entirely or partially confirmed, showing how disordered eating behaviours are complex eating attitudes.
6. Conclusions
This paper has argued the relationship between body image, body concerns, body dissatisfaction, and disordered eating behaviours present in college women from the south of Spain. This study has identified that women reported moderate levels of body dissatisfaction and body concerns, which were consistently and strongly associated with disordered eating attitudes. In this sense, this work has established high levels of body dissatisfaction, and the link with the desire to achieve a thinner body image. Additionally, the study has shown how body dissatisfaction and desire to achieve the thin-ideal appear to be universal among college women.
Additionally, one of the more significant findings to emerge from this study was that the thin-ideal seems to be widespread in social media. This ideal can promote unhealthy measures, such as dieting, increase body dissatisfaction and disordered eating attitudes. In this sense, the desire to change the body image and taking unhealthy measures was common, given the proliferation of the use of the social network sites where images and content encourage women to aspire to unrealistic and unattainable body ideals. In this sense, the study associated body dissatisfaction, body concerns, and general mental well-being, demonstrating that interventions to improve body perception and satisfaction are essential. Additionally, this research found that higher levels of prenatal testosterone might decrease the probability of having a disordered eating attitude among women. That said, the current study suggests a connection between disordered eating attitudes, negative impacts of exposure to thin-ideal content, addiction to social media and intrauterine testosterone levels.
Concerning practical implications, researchers have asserted that increasing body appreciation may be easier than attempting to decrease body dissatisfaction and for those disordered eating attitudes. Furthermore, the findings regarding the negative impact of exposure to social media related to women’s body satisfaction and body appreciation are notable. Despite the limitations present in this manuscript, the findings may help us to understand body concerns focused on the impact of exposure to social media.
In the end, future investigations should continue exploring differences in the levels of body dissatisfaction and disordered eating, including the differences between various ethnic groups. Given the findings regarding differences between those with higher and lower score in EAT-26, the role of social media may be essential in levels of body dissatisfaction and disordered eating attitudes within specific gender/age groups. Longitudinal research is needed to determine the direction of the association between the frequency of connections to social media and body dissatisfaction/disordered eating behaviours. Researchers may also consider culturally-relevant factors that may differentially influence such behaviours.
Acknowledgments
We would also like to thank of UCO Social Innova Project Galileo IV from the institution of OTRI of the University of Cordoba, Spain and the funding provided from “IDEP/Escuela de Doctorado” of the University of Cordoba to one of the authors. The content is the responsibility of the authors and does not necessarily represent the official views of the OTRI.
Author Contributions
Conceptualization: P.A.-M. and M.V.A.; methodology: P.A.-M. and M.P.M.-J.; validation: A.-J.P.-M.; formal analysis: P.A.-M. and A.-J.P.-M.; investigation: P.A.-M. and A.-J.P.-M.; resources: M.P.M.-J. and A.-J.P.-M.; data curation: M.D.R.-M.; writing—original draft preparation: P.A.-M., M.P.M.-J. and A.-J.P.-M.; writing—review and editing: M.V.A. and C.P.; visualization: C.P.; supervision: M.D.R.-M., C.P. and M.V.A.; project administration: M.V.A. and M.P.M.-J.; funding acquisition: M.V.A.
UCO Social Innova Project Galileo IV from the institution of OTRI of the University of Cordoba, Spain and the funding provided from “IDEP/Escuela de Doctorado” of the University of Cordoba.
Conflicts of Interest
The authors declare no conflict of interest.
- Open access
- Published: 26 August 2024
Towards collaborative care for severe and enduring Anorexia Nervosa – a mixed-method approach
- Ilona M.C. van den Eijnde-Damen 1 ,
- Joyce Maas 1 , 2 ,
- Pia Burger 1 ,
- Nynke M.G. Bodde 1 &
- Mladena Simeunovic-Ostojic 1
Journal of Eating Disorders volume 12 , Article number: 124 ( 2024 ) Cite this article
Metrics details
Severe and Enduring Eating Disorders (SEED), in particular SEED-Anorexia Nervosa (SE-AN), may represent the most difficult disorder to treat in psychiatry. Furthermore, the lack of empirical research in this patient group, and, consequently the lack of guidelines, call for an urgent increase in research and discussion within this field. Meanwhile experts concur that effective care should be structured in a collaborative manner.
To identify the challenges in providing care to patients with SE-AN in the Dutch healthcare context, and propose a collaborative care treatment model to address these issues.
A pragmatic mixed-method approach was used, structured as follows: (1) Identifying perceived barriers and treatment needs from the viewpoint of both patients and eating disorder healthcare professionals through an evaluation questionnaire; (2) Investigating current treatment practices for SEED/SE-AN via benchmarking; (3) Gaining insight into the optimal structure and content of care by interviewing network partners and experts-by-experience. Based on these findings, and drawing from literature on severe and enduring disorders, a treatment model for SE-AN was proposed and implemented.
The key challenges identified included a lack of knowledge about eating disorders among network partners, treatment ambivalence among patients and poor collaboration between professionals. The proposed model enhances self-management and collaborative relationships with healthcare providers, offers user-friendly and practical guidance, and aims at stabilization, reducing relapses, deterioration, and readmissions, thereby being cost-effective. Importantly, the model operates across levels of care (primary, secondary, tertiary).
This study, describing a collaborative care program for SE-AN, developed and implemented in a highly specialized treatment center for eating disorders, sets the stage for further explanatory/efficacy research to build on the findings in this study, with the following aims: addressing the critical gap in care for SEED/SE-AN, improving better healthcare organization, reducing relapse rates, and lowering costs for this often overlooked patient group.
Plain English summary
Severe and Enduring Eating Disorders (SEED), and particularly Severe and Enduring Anorexia Nervosa (SE-AN), present significant challenges in psychiatric treatment. This study aimed to understand the obstacles in caring for patients with SEED/SE-AN in the Dutch healthcare system and proposed a collaborative care model to address the issues. Through surveys, interviews, and benchmarking, key challenges were identified, including limited knowledge about eating disorders, patient ambivalence, and poor professional collaboration. The collaborative care model for SE-AN that was proposed in this study emphasizes structured care coordination, education for network partners, and support for eating disorder professionals, combining clinical management and psychotherapy. The study aims to bridge the gap in care for SE-AN and improve healthcare organization for this overlooked patient group.
Eating disorders (ED) are associated with great functional impairment and high mortality rates. Specifically, anorexia nervosa (AN) has the highest mortality rate of any psychiatric disorder [ 1 ]. More than 70% of patients with EDs have comorbid psychiatric disorders [ 2 ], which are linked to a worse prognosis and a higher chance of chronicity [ 3 ]. Of all patients with AN or bulimia nervosa (BN), roughly 20% develop an enduring illness [ 4 ]: a so-called ‘severe and enduring eating disorder’ (SEED) [ 5 ]. The consequences of SEED on quality of life are comparable to those experienced by patients with other severe enduring psychiatric illnesses, such as schizophrenia [ 6 ]. Daily life is constrained by chronic psychiatric symptoms, and there is usually significant psychological distress. This results in an increased need for healthcare services [ 7 ]. Furthermore, SEED, especially SEED-Anorexia Nervosa (SE-AN) has serious physical repercussions and patients often live on the edge of what their bodies are able to cope with [ 8 ]. Patients can remain stable for many years at a low BMI, but any extra stress on the body (for example due to an infection or purging behavior) that could affect weight or other clinical features, such as potassium levels, can lead to physical decompensation fast [ 6 ]. Previously, a call to action was issued, highlighting the significant lack of evidence-based treatments, insufficient research, and overall neglect within the domain of SEED [ 5 ].
Another problematic issue is the lack of consensus regarding the definition of SEED. This ambiguity leads to inconsistent participant recruitment for studies, which hinders the increase of knowledge about this group of patients, and contributes to the potential misdiagnosis of patients [ 9 ]. First, criteria for determining cut-off points for the duration of SEED vary widely, with cut-offs ranging from 5 to 10 years [ 10 , 11 ]. Second, although the SEED category implies multiple unsuccessful treatment attempts, there is no agreed-upon standard regarding the number, quality or focus of these previous interventions [ 5 ]. Other variables often taken into consideration when defining SEED are severity of illness and patient age [ 5 ]. A refined classification of the SE-AN subcategory was suggested by Hay and Touyz [ 12 ]. This classification is more aligned to definitions of other enduring psychiatric illnesses, yet it diverges from the most often mentioned cut-off points and for example mentions a duration of only > 3 years [ 12 ], although a cut-off of 7 years has also often been used for SE-AN [ 13 , 14 , 15 ]. Other criteria include a persistent state of dietary restriction, underweight, and overevaluation of weight/shape with functional impairment; exposure to at least two evidence-based treatments appropriately delivered together with a diagnostic assessment and formulation that incorporates an assessment of the person’s ED health literacy and stage of change. Robinson furthermore suggested including service utilization in the definition of SEED. These differences underline the lack of an agreed upon definition [ 16 ].
Although ED treatment usually focuses on recovering from ED symptoms and, in case of AN, weight restoration, for patients with SE-AN the emphasis lies on maximizing medical stability, quality of life, social adjustment, and vocational issues [ 5 ]. Recovery is in fact still possible for some patients if they reach a certain motivational tipping point [ 17 ]. Eddy et al. showed that around a third of patients with AN recover in the first decade of their illness, but that a second third will still recover during the second decade [ 18 ]. Several potentially beneficial treatment options for patients with SEED/SE-AN have been identified, for example, motivational treatment, (SEED-adapted) enhanced Cognitive Behavior Therapy and Specialist Supportive Clinical Management (SSCM[-SE]) [ 19 , 20 ]. SSCM combines active clinical management (including information, advice, and encouragement) with psychotherapeutic elements, marked by a supportive therapeutic style. SSCM-SE is a modified version for patients with SEED and prioritizes quality of life and harm minimization, but weight gain – unlike the standard form SSCM – is not a primary aim [ 14 ]. Other treatments that have been mentioned as potentially beneficial are pharmacological treatments and brain stimulation therapies [ 19 ].
Patients with SE-AN present a highly complex clinical picture, characterized by a mix of acute and long-term symptoms that tend to worsen over time. Managing such patients necessitates a multidisciplinary team approach, as well as collaboration with network partners across various levels of care (primary, secondary, tertiary). This collaborative effort should also involve the patients themselves and their caregivers. The importance of coordination and collaboration among all healthcare professionals involved cannot be overstated, given the likelihood of comorbid conditions and evolving treatment priorities. Moreover, this collaboration is essential to ensure that professionals remain vigilant and continuously monitor the patient’s risk.
While recognizing the necessity of a systematic approach to treating SE-AN and fostering collaboration among all stakeholders, there is a notable gap in implementing an organized treatment model for SE-AN. However, insights from literature, including literature on other complex and chronic patient groups, such as those with severe personality disorders [ 21 ], offer valuable strategies for organizing care.
The Collaborative Care Model (CCM) [ 21 ] offers valuable insights into the organization of care and a framework for collaboration. Underlying principles are shared decision making, creating effective collaborative relationships (with all parties involved), increasing self-management and enhancing problem-solving skills. It increases self-management, reduces self-destructive behavior, and improves quality and continuity of care [ 22 ]. Within this model, nurses serve as collaborative care managers, ensuring optimal continuity and coordination of care [ 5 ]. Second, the Community Outreach Partnership Program (COPP) [ 23 ] places less emphasis on diminishing ED symptoms and more on improving quality of life through fostering independence and establishing a social support network beyond the healthcare system. Key elements in the treatment plan include the so-called non-negotiable agreements, which are primarily intended to ensure medical safety.
The main aim of this study was to define a model that can improve the quality and continuity of care for patients with SE-AN within the context of Dutch mental healthcare. Our highly specialized ED treatment center offers a supra-regional treatment function and provides specialized mental health care services, as well as high-intensity and highly specialized matched care treatment programs for patients with ED, including those with severe and complex ED. The model was defined, taking the literature reviewed above into account, and by (1) identifying the perceived barriers and treatment needs from the viewpoint of patients in treatment at our center and our own ED healthcare professionals, by (2) investigating the current treatment practices with regards to SEED/SE-AN in other ED centers in the Netherlands, and by (3) gaining insight into the optimal structure and content of care for patients with SE-AN by interviewing network partners collaborating with ED centers (e.g., general practitioners [GP’s], dietitians) and experts by experience. These results led to a proposed treatment model for patients with SE-AN, which we implemented in our treatment center. We illustrated the potential efficacy of this model with two patient cases, before and after implementation.
Several steps were taken to define a proper treatment model for patients with SE-AN.
First, to address the challenges in treating patients with SE-AN, and ED more in general, individuals undergoing outpatient group treatment (regular daytime group treatment or SE-AN treatment) or inpatient care at our ED treatment center at the time of the study were contacted to complete a short evaluation, forming a convenience sample. This survey aligned with our usual treatment evaluation and consisted of five short questions (regarding the alignment of treatment with patients’ expectations; consideration of patients’ needs and wishes regarding treatment planning; and any gaps patients perceived in their current treatment) with ordinal-level responses and an option to provide additional comments. The survey was distributed over a short period of two weeks by an independent staff member who was not involved in the research, without any additional reminders. ED healthcare professionals working in inpatient as well as outpatient treatment (and some worked in both settings) from our treatment center completed a similar evaluation survey. The completed surveys were submitted voluntarily and anonymously. Insights gained from these evaluations informed the development of a topic list for further open-ended questionnaires and interviews, facilitating a deeper exploration of issues in subsequent phases of the study. Unlike the treatment evaluations that were based on both ED treatment and SE-AN treatment, subsequent phases of this study only focused on SE-AN.
Second, benchmarking was utilized to explore how various mental health care institutions design care for patients with SEED/SE-AN (see Supplement 1) [ 24 ]. Three organizations delivered Top Clinical mental healthcare, two delivered specialized mental healthcare. In the Netherlands, mental healthcare is organized according to severity. Top Clinical mental healthcare offers highly specialized treatments and includes a focus on innovative treatments and (implementation and dissemination of) disorder-specific scientific research. Another focus of Top Clinical mental healthcare is consultation and offering second opinions to other treatment centers. Specialized mental healthcare is for severe of chronical mental health problems with treatment durations up to a year, with possibility of extensions.
Third, network partners actively involved in the care of patients with SEED/SE-AN were invited via email or telephone to contribute to the study through an open-ended questionnaire (see Supplement 2). To ensure comprehensive representation from all disciplines involved in SEED/SE-AN patient care, invitations were extended to 14 general practitioners’ offices, 5 FACT (Flexible Assertive Community Treatment) team members, 2 dietitians, 2 nurse specialists, and 2 sociotherapists. Reminders were sent to improve the response rate.
Fourth, semi-structured interviews with two experts by experience from a self-help organization were conducted to gain insights into the optimal structure and content of care for patients with SEED/SE-AN. Interviews were conducted based on the topic list that resulted from the treatment evaluations by patients and ED healthcare professionals (see Supplement 3).
Treatment evaluation by patients and ED healthcare professionals
Of the 71 approached, 35 patients completed the treatment evaluation. The sample represented the diverse patient population in treatment at our ED treatment center (daytime group treatment, inpatients and outpatients), and 17.1% were patients with SE-AN. Of particular interest, patients with SEED pointed out they needed more individual treatment time, more frequent group sessions, and creative therapies.
Of the 43 staff members that were approached, 27 completed the evaluation. Several needs were mentioned: the need for more individual treatment options, supportive and structuring treatment options, as well as the need for scaling-up treatment. Staff also mentioned difficulties in the transition from inpatient to daytime treatment. Treatment should focus more on symptom reduction, acceptance of the illness, quality of life, and the treatment should convey that the patient is understood and acknowledged. Services available to patients with SEED are currently too limited, and collaboration with network partners is insufficient. Staff furthermore needs support in boosting patients’ self-management in physical, psychological, and social areas.
Benchmarking
All five ED centers participated in the benchmarking, emphasizing person-centered care. They noted that customized care is essential for patients with SEED/SE-AN, who often find standard treatments insufficient. Two institutions used SSCM, involving supportive treatment, physical monitoring, nutritional management, and psychoeducation. Other institutions’ approaches aligned with SSCM, though not explicitly named. One organization specifically employed CBT-E.
The organizations aim to enhance quality of life, focusing on rediscovering joy, maintaining social connections, and finding meaningful activities. Treatment also targets stabilization and harm reduction, minimizing the ED’s impact and preventing deterioration. Most have diverse disciplines in-house for integrated care. A robust support network, involving regular external consultations, is deemed critical, though no specific collaborative treatment model was mentioned. The collaboration’s success depends on patient needs and practitioner willingness to collaborate. Three institutions viewed SEED/SE-AN treatment as applicable to both specialized and primary mental health care. Stable patients without improvement could move to primary care, with an easy return to specialized care if needed. Two institutions argued SEED/SE-AN care belongs in specialized care due to primary care’s lack of expertise, suggesting specialized care could help enhance knowledge in primary care so that patients can be referred to specialized care more often.
Network partners
The survey received a 32% response rate from network partners. Respondents were non-ED professionals, more specifically general practice-based nurse specialists (4), nurse specialists (2) and one sociotherapist and dietitian. Points for improvement are presented in Table 1 .
Experts by experience
The experts by experience viewed the term “severe and enduring ED” negatively, suggesting it implies abandonment and a lack of potential for recovery. They argued the definition of SEED applies when recovery seems unattainable, but caution against declaring further recovery impossible, especially if correct treatment was previously unavailable. Maintaining and conveying hope is crucial; they noted recovery is possible even after many years. Patients sense when providers lose faith in improvement, potentially harming the therapeutic relationship, which they deem essential.
Respondents advocated for care tailored to individual patient needs, criticizing one-size-fits-all approaches and stressing the importance of listening to patients. They emphasized empowerment and autonomy, focusing on identifying underlying issues and aiding patients in leading as comfortable a life as possible. They interpret referrals from specialized to primary mental health care as signaling a patient has been given up on, suggesting it diminishes their worth and overlooks the root of the problem. The lack of ED expertise in primary care is problematic. However, they conceded referral to primary care might be feasible for stable individuals, provided specialized care remains vigilant due to the fluctuating nature of EDs and the risk of relapse during transitions. Improving collaboration and communication among care providers is important. They envisioned an ideal scenario where each patient has a multidisciplinary team regularly reviewing their progress, though they recognized the challenges in implementing such a model. They suggested involving experts by experience in patient groups can significantly enhance understanding and support for patients with SEED.
Development of the collaborative care treatment model
The CCM [ 22 ] model fits several needs as mentioned in the questionnaires and interviews, such as shared decision-making, increasing self-management, and actively involving all stakeholders. Collaboration between network partners across all care levels is essential. Active clinical management with psychotherapeutic elements, as incorporated in SSCM-SE is also required [ 14 ]. Finally, the COPP [ 23 ] prioritizes enhancing quality of life through independence and social support outside the healthcare system.
To integrate these elements effectively, we adopted the CCM model as our foundation and enriched it with components from SSCM-SE and the COPP. The resulting model enhances self-management and collaborative relationships with healthcare providers, offers user-friendly and practical guidance, and aims at stabilization, reducing relapses, deterioration, and readmissions, thereby being cost-effective. Importantly, our collaborative care model operates across levels of care (primary, secondary, tertiary).
The resulting model is divided into three phases, encompassing five integrated elements, see Fig. 1 . An explanation of each phase is described in the following paragraphs. After that, two cases are presented illustrating the situation before and after implementation. Both patients provided their consent for including their case description in the present paper.

Collaborative Care Program for SE-AN
Phase 1: Preparation
This phase is dedicated to establishing connections, introduction of the CCM, and setting up arrangements with the patient, their caregivers, and the network partners involved. We use the definition of Hay and Touyz [ 12 ] to determine the eligibility of patients for the program, but with the often-used cut-off of 7 years for the duration of AN [ 13 , 14 , 15 ] and at least two previous unsuccessful evidence-based treatment attempts, and additionally one treatment or second opinion at a Top Clinical mental healthcare institution. Exclusion criteria are somatic instability requiring acute medical care or inpatient treatment, and inability to set non-negotiable agreements, as treatment is voluntary. The specialized ED center takes the lead in coordinating the collaboration among all parties. During this phase, it is important to define and document the frequency and content of contacts, as well as the roles each participant will play. At our center we offer a separate group and individual treatment for patients with SE-AN (next to regular treatment for ED). Goals are set using a person-centered approach and shared decision-making; while these goals primarily reflect the patient’s values and norms, ensuring safety is paramount. Therefore, a crisis plan regarding medical and psychological safety is developed in collaboration with the patient prioritizing the least restrictive option. This plan contains non-negotiable agreements, such as specific thresholds for weight loss or critical abnormalities in lab results, early signs of a crisis, the most appropriate treatment setting (booster clinical treatment at our treatment center, admission to a general hospital or an inpatient psychiatric unit, for example) in these cases, and the corresponding interventions that will be enacted.
Phase 2: Treatment
Phase 2 focuses on monitoring the patient’s physical and mental condition, identifying potential risks, and initiating appropriate interventions. In this phase, the patient actively participates in designing a relapse prevention plan. Recognizing early signs of relapse and preparing practical coping strategies are key components of this plan, enhancing the patient’s ability to manage their condition. While the patient takes the lead in in this planning, therapists and caregivers have access to the crisis plan to ensure a coordinated response when needed. The focus of nutrition is on health and safety, not on weight gain, unless requested by the patient.
Another key objective of Phase 2 is to work gradually towards realistic treatment goals within a continuum of care at a pace comfortable to the patient. This may include our SE-AN group or individual treatment, possibly combined with food management, and treatment for any comorbid conditions. Psychotherapy for comorbid disorders and pharmaceutical treatment can be included, depending on the patient’s needs. From Phase 1, it is already determined which network partner will be involved with each specific treatment goal and in which treatment setting. Scaling-up and scaling-down of treatment for the ED (inpatient, day programs or partial hospitalization and outpatient) is possible, matching the individual level of motivation for change with goals of treatment. This enables patients with different types and degrees of severity to be included in the program. Considering the significant impact of SE-AN on patients’ quality of life, issues such as housing, occupation (employment, education), relationships (social, family), and finances require attention. Effective resocialization strategies are critical as they help diminish the influence of the ED on the patient’s life, thereby increasing stability and overall quality of life. When treatment shifts from focusing solely on reducing ED symptoms and risk management to enhancing quality of life, ED symptoms may still improve.
This person-centered approach of our treatment also stresses the importance of dignity, respect, and compassion in interaction, aiming to empower patients, and create and maintain hope. The need for treatment to embrace hope for a realistic, self-defined recovery means acknowledging that recovery might not always align with conventional or idealized, or even self-defined desirable outcomes. For some individuals with SE-AN, this could involve “attaining peace from suffering,” which may include the possibility of a “dignified death.” Discussing this topic, while maintaining hope for full recovery does not bring death closer, but paradoxically, it can open up new possibilities for life and diminish suicide risk.
Phase 3: Evaluation
Phase 3 concerns evaluation of the treatment. This evaluation should be repeated periodically, at a minimum of every three months. The criteria for evaluation, as established during Phase 1, should include input from all parties involved in the patient’s care. Routine Outcome Monitoring Data with special attention to refocusing outcomes towards quality of life is used to provide a comprehensive review of progress and outcomes. If necessary, adjustments may be made to the treatment plan based on these evaluations. The specialized ED center’s consultation liaison team (see below under ‘Overarching tasks’) assists network partners in the patients’ care, when patients are no longer in treatment at our treatment center.
Overarching tasks
In Fig. 2 , the overarching tasks regarding collaboration and key considerations related to treatment for patients with SE-AN are presented. During the whole process, the specialized ED center has an important job to educate the patient and all stakeholders on the ED, and to assist caretakers in taking care of the patient. The burden of care for ED is high and long lasting and therefore requires continued attention. The specialized ED center furthermore needs to educate network partners about SE-AN/ED. Our consultation liaison team is available daily through a telephone consultation hour to support our network partners, and the team can also be deployed on-site to support the care for patients with SEED. This support extends not only to the (somatic) care of patients with SEED but also to guidance on patient interaction. That is, dissemination of knowledge should not only focus on risk behaviors, possible complications and interventions, but also how to deal with patient’s continuous ambivalence regarding treatment. This ambivalence can cause helplessness, misunderstanding and stigmatizing attitudes in professionals. When patients are confronted with stigmatizing opinions, they may lose trust and hope in treatment, increasing the risk of relapse.
It cannot be overstated how crucial person-centered, personalized treatments, along with the consultation liaison role of the ED treatment center, are in addressing the profound complexity and scientific uncertainties surrounding SE-AN. Rather than applying a one-size-fits-all approach, this method emphasizes understanding the person living with SE-AN as a whole, while facilitating medical stabilization, harm reduction, quality of life, and the continuous maintenance of hope and engagement with treatment.
When patients are no longer in treatment at the specialized ED center, it is nevertheless important to remain accessible to the patient. This fosters trust and maintains hope. Sometimes, a brief phone call or email contact is enough for the patient to move forward and prevent further relapse. In some cases, a short booster admission may suffice.

Overarching tasks and considerations for collaborative care for SE-AN/SEED
Patient A – before the implementation of the model
Patient A, a married woman in her fifties with a long history of SE-AN, binge eating/purging subtype, was referred back to our clinic by a general hospital. Diagnosed at 16, A. has navigated through cycles of remission and relapse, with additional challenges including an anxiety disorder and post-traumatic stress disorder. Over the past three years, A. had been admitted to our clinic three times with a similar clinical picture. Unfortunately, after her most recent discharge, establishing a follow-up treatment proved challenging, leading to her relapse. This latest episode was particularly severe, with A. nearly ceasing to eat, resulting in a BMI of 14, alongside complications from excessive water intake and laxative abuse.
Post-discharge of her previous clinical admission, A. was directed to a FACT (Flexible Assertive Community Treatment) team in her area, aimed at aiding her resocialization and improving her quality of life by helping maintain treatment gains and adapt her eating habits to her home environment. Despite this plan and our efforts to collaborate with her GP for ongoing physical monitoring, the FACT-team felt unable to support A. due to perceived mismatches in their target demographic and a lack of ED expertise.
However, A.‘s recent readmission underscored the critical need for effective follow-up care. Despite the difficulties in securing a partnership for her continued treatment, the importance of collaboration among care providers, including A. herself, became increasingly apparent. The need for an ED specialist to offer guidance to those less familiar with SEED and to address stigma, feelings of helplessness, and resistance surrounding the disorder was identified. Educational efforts should extend beyond SEED to include these broader issues.
After detailed discussions about our collaborative care model and the support we could offer, the FACT-team that initially declined involvement agreed to participate in a coordinated care approach. The consensus among us, the GP, and the FACT-team, was that A. required additional support tailored to her home setting. Nevertheless, establishing this network of care encountered obstacles, with multiple rejections stemming from a cycle of referrals, highlighting the complexity of organizing collaborative care for individuals with SEED.
Patient B – an example of a proper implementation of the model
B., a single woman in her thirties, has faced SE-AN, binge eating/purging subtype, for years. Despite multiple treatments since her diagnosis at 20, lasting recovery has eluded her, complicated by comorbid post-traumatic stress disorder and borderline personality disorder. Recent years have seen her losing her job and a relationship ending, with minimal social support from her family and a friend.
Her journey encountered a significant turn during her 6th clinic admission following a severe relapse, characterized by a BMI of 14, minimal food intake, excessive hydration, vomiting, excessive exercise, and laxative misuse. It was then that a collaborative care approach was initiated, involving our clinic’s team, a FACT-team, and B.‘s GP. This approach led to a comprehensive treatment plan addressing her physical health, psychological needs, and social reintegration, including meaningful daytime activities and home supervision.
An emergency plan was crafted with B., outlining non-negotiable agreements and clear indicators for crisis intervention, which proved pivotal. B.‘s engagement in work at a care farm and supervised meals contributed to a stable weight, improved self-esteem, and reduced disordered eating thoughts and behaviors. Two years into this collaborative care, B. experienced a relapse. However, the established emergency plan enabled a swift response, ensuring a short booster admission was sufficient for her to regain stability. The immediate involvement of all network partners facilitated her quick return to societal reintegration, highlighting the effectiveness of coordinated care in managing severe ED.
Although AN boasts the highest mortality rate among psychiatric disorders, and SE-AN represents the most severe manifestation within ED, quality and continuity of care for patients with SE-AN is problematic. The lack of systematic treatment organization for SE-AN and lack of empirical evidence leaves many patients inadequately treated. This study aimed to identify treatment challenges for patients with SE-AN utilizing multiple sources of information and proposed a collaborative care treatment model.
After assessing the perceived barriers and treatment needs from the perspectives of patients and healthcare professionals from our own treatment center, analyzing the current Dutch treatment practices for SEED/SE-AN via benchmarking, and gaining insight into the optimal structure and content of care through interviews with network partners and experts by experience, we developed and implemented a treatment model for patients with SE-AN in our highly specialized treatment center. Please note that response rates to the evaluation questionnaires from patients, staff and network partners were relatively low, although similar to response rates in other studies focusing on ED health providers [ 25 , 26 , 27 , 28 , 29 ]. Notably, no GPs responded to the survey. This is partly in line with a previously noted difficulty in obtaining physicians’ participation in survey research, due to limited time, lack of interest, insufficient staffing in the office, working in non-educational settings of practice, and stigma [ 30 ]. It has been suggested that physicians might be reluctant to participate in studies on sensitive topics or areas of care where they feel their performance may fall short of expectations. Although our findings must be interpreted in the context of a low response rate, this study remains an informative initial examination using pragmatic research methodology to address key questions about how a treatment model can be applied in real-world clinical care. A strength of our study is the use of mixed methods (qualitative and quantitative). Data were collected over a short period within actual clinical care settings and their evaluation, and from multiple levels of stakeholders, providing a comprehensive perspective. Future empirical research should aim for a more in-depth analysis of the data, which would require a much larger set of primary data.
We incorporated elements from several established treatment models as found in the literature, including SSCM-SE [ 19 , 20 ], the CCM [ 21 ], and the COPP [ 23 ]. The model unfolds in three phases, each designed to optimize care for patients with SE-AN. The first phase initiates collaboration among all parties involved, sets treatment goals, and creates an emergency plan prioritizing safety. The second phase concentrates on monitoring the patient’s health, identifying potential risks, initiating timely interventions, and treatment focused on realistic goals within a continuum of care. The final phase involves evaluating the treatment efficiency.
The proposed collaborative care treatment model operates across all levels of care - primary, secondary, and tertiary - with the tertiary care center taking a leading role. Consistent with the facilitators for successful implementation of collaborative care as described earlier [ 31 ], our model designates one professional to spearhead the process. Given the high complexity and potential medical complications associated with SE-AN, a nurse specialist at the (highly) specialized ED center fills this role. In alignment with the recommendations from Wood et al., the nurse specialist also coordinates inter-professional communication through standardized care pathways and establishes clear boundaries for the role of all network partners [ 31 ].
Our collaborative care treatment model addresses the challenges mentioned by patients, staff, network partners, and experts by experience, such as lack of knowledge about ED among network partners, treatment ambivalence among patients, and poor communication/collaboration between professionals. It underscores the importance of educating network partners about ED and managing patients’ treatment ambivalence, thereby decreasing often-occurring feelings of helplessness, misunderstanding and stigmatizing attitudes in professionals [ 32 , 33 ]. The model’s structured approach, with clearly defined phases and roles for everyone involved in the patient’s care, is designed to the improve and ensure continuity of care for patients with SE-AN. This structured framework not only facilitates better care coordination, but also enhances understanding among caregivers, thereby reducing potential miscommunications and inefficiencies.
Our two case examples also illustrate the significant lack of knowledge about ED among network partners. Beyond the organization and coordination of treatment, specialized ED centers play an important role in education. This includes providing insights on handling the pervasive ambivalence towards treatment often experienced by patients. The interviews and case examples also showed that communication and collaboration between network partners is often poor. Wood et al. mention that healthcare tends to operate in silos and staff and organizational attitudes to integration are important to take into account [ 31 ]. The complexity of SE-AN exacerbates these challenges, underscoring the need for comprehensive education and support for all professionals involved in patient care.
This study, describing and implementing a collaborative care program for SE-AN, sets the stage for further research into its implementation effectiveness and cost-efficiency. It highlights the importance of directly assessing patient perspectives on collaborative care. Despite known implementation challenges, as seen in depression care, identifying and addressing barriers to collaborative care is important for expanding access [ 34 ]. Wonderlich et al. described the limited understanding of SEED as “a crisis in our field”, noting that the most severely affected patients often receive the least adequate care [ 5 ]. Given the study’s limited generalizability, there is a clear call for future research to build on our findings, aiming to address the critical gap in care for SE-AN, improve better healthcare and healthcare organization, reduced relapse rates, and lower costs for this often overlooked patient group.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
Anorexia nervosa
Bulimia nervosa
Enhanced Cognitive Behavior Therapy
Collaborative Care Model
Community Outreach Partnership Program
- Eating disorders
Flexible Assertive Community Treatment
General practitioner
Specialist Supported Clinical Management (for SEED)
Severe and enduring eating disorders
Severe and enduring anorexia nervosa
Arcelus J, Mitchell AJ, Wales J, Nielsen S. Mortality rates in patients with anorexia nervosa and other eating disorders. A meta-analysis of 36 studies. Arch Gen Psychiatry. 2011;68(7):724–31. https://doi.org/10.1001/archgenpsychiatry.2011.74 .
Article PubMed Google Scholar
Keski-Rahkonen A, Mustelin L. Epidemiology of eating disorders in Europe: prevalence, incidence, comorbidity, course, consequences, and risk factors. Curr Opin Psychiatry. 2016;29(6):340–5.
McFarlane T, MacDonald DE, Trottier K, Olmsted MP. The effectiveness of an individualized form of day hospital treatment. Eat Disord. 2015;23(3):191–205.
Steinhausen HC. Outcome of eating disorders. Child Adolesc Psychiatr Clin N Am. 2009;18(1):225–42.
Wonderlich S, Mitchell JE, Crosby RD, et al. Minimizing and treating chronicity in the eating disorders: a clinical overview. Int J Eat Disord. 2012;45(4):467–75.
Robinson P. Severe and Enduring Eating Disorder (SEED): management of Complex presentations of Anorexia and Bulimia Nervosa. Wiley; 2009.
Meije D, Hendriksen A, van Bakel M, Sinnema H. Ondersteuning bij zelfmanagement van patiënten met chronische psychiatrische aandoeningen.
Arkell J, Robinson P. A pilot case series using qualitative and quantitative methods: biological, psychological and social outcome in severe and enduring eating disorder (anorexia nervosa). Int J Eat Disord. 2008;41(7):650–6.
Broomfield C, Stedal K, Touyz S, Rhodes P. L abeling and defining severe and enduring anorexia nervosa: a systematic review and critical analysis. Int J Eat Disord. 2017;50(6):611–23.
Touyz S, Le Grange D, Lacey H, Hay P. Managing severe and Enduring Anorexia Nervosa: a clinician’s guide. Routledge; 2016.
Ciao AC, Accurso EC, Wonderlich SA. What do we know about severe and enduring anorexia nervosa? Managing severe and Enduring Anorexia Nervosa. Routledge; 2016. pp. 1–12.
Hay P, Touyz S. Classification challenges in the field of eating disorders: can severe and enduring anorexia nervosa be better defined? J Eat Disord. 2018;6:1–3.
Article Google Scholar
Ambwani S, Cardi V, Albano G, et al. A multicenter audit of outpatient care for adult anorexia nervosa: Symptom trajectory, service use, and evidence in support of early stage versus severe and enduring classification. Int J Eat Disord. 2020;53(8):1337–48. https://doi.org/10.1002/eat.23246 .
Touyz S, Le Grange D, Lacey H, et al. Treating severe and enduring anorexia nervosa: a randomized controlled trial. Psychol Med. 2013;43(12):2501–11. https://doi.org/10.1017/S0033291713000949 .
Marcolini F, Ravaglia A, Tempia Valenta S, et al. Severe enduring anorexia nervosa (SE-AN) treatment options and their effectiveness: a review of literature. J Eat Disord. 2024;12(1):48.
Article PubMed PubMed Central Google Scholar
Robinson P. Severe and enduring eating disorders: recognition and management. Adv Psychiatr Treat. 2014;20(6):392–401.
Dawson L, Rhodes P, Touyz S. Doing the impossible the process of recovery from chronic anorexia nervosa. Qual Health Res. 2014;24(4):494–505.
Eddy KT, Tabri N, Thomas JJ, et al. Recovery from anorexia nervosa and bulimia nervosa at 22-year follow-up. J Clin Psychiatry. 2017;78(2):17085.
Kotilahti E, West M, Isomaa R, Karhunen L, Rocks T, Ruusunen A. Treatment interventions for severe and enduring eating disorders: systematic review. Int J Eat Disord. 2020;53(8):1280–302.
Marcolini F, Ravaglia A, Tempia Valenta S, et al. Severe enduring anorexia nervosa (SE-AN) treatment options and their effectiveness: a review of literature. J Eat Disord. 2024;12(1):48. https://doi.org/10.1186/s40337-024-01006-y .
Stringer B, van Meijel B, Koekkoek B, Kerkhof A, Beekman A. Collaborative Care for patients with severe borderline and NOS personality disorders: a comparative multiple case study on processes and outcomes. BMC Psychiatry. 2011;11:1–10.
Stringer B, Meijel B, Karman P et al. Collaborative Care for patients with severe personality disorders: preliminary results and active ingredients from a pilot study (part I). Perspect Psychiatr Care. 2015;51(3).
Williams KD, Dobney T, Geller J. Setting the eating disorder aside: an alternative model of care. Eur Eat Disorders Review: Prof J Eat Disorders Association. 2010;18(2):90–6.
Willmington C, Belardi P, Murante AM, Vainieri M. The contribution of benchmarking to quality improvement in healthcare. A systematic literature review. BMC Health Serv Res. 2022;22(1):139.
McAlpine DE, Schroder K, Pankratz VS, Maurer M. Survey of regional health care providers on selection of treatment for bulimia nervosa. Int J Eat Disord. 2004;35(1):27–32.
Haas HL, Clopton JR. Comparing clinical and research treatments for eating disorders. Int J Eat Disord. 2003;33(4):412–20.
von Ranson KM, Robinson KE. Who is providing what type of psychotherapy to eating disorder clients? A survey. Int J Eat Disord. 2006;39(1):27–34.
Cashel ML. Child and adolescent psychological assessment: current clinical practices and the impact of managed care. Prof Psychol Res Pr. 2002;33(5):446.
Hawley KM, Cook JR, Jensen-Doss A. Do noncontingent incentives increase survey response rates among mental health providers? A randomized trial comparison. Adm Policy Mental Health Mental Health Serv Res. 2009;36:343–8.
Asch S, Connor SE, Hamilton EG, Fox SA. Problems in recruiting community-based physicians for health services research. J Gen Intern Med. 2000;15:591–9.
Wood E, Ohlsen S, Ricketts T. What are the barriers and facilitators to implementing collaborative care for depression? A systematic review. J Affect Disord. 2017;214:26–43.
Hay PJ, Touyz S, Sud R. Treatment for severe and enduring anorexia nervosa: a review. Australian New Z J Psychiatry. 2012;46(12):1136–44.
Molin M, von Hausswolff-Juhlin Y, Norring C, Hagberg L, Gustafsson SA. Case management at an outpatient unit for severe and enduring eating disorder patients at Stockholm Centre for eating Disorders–a study protocol. J Eat Disord. 2016;4:1–5.
Fu E, Carroll AJ, Rosenthal LJ, et al. Implementation barriers and experiences of eligible patients who failed to enroll in collaborative care for depression and anxiety. J Gen Intern Med. 2023;38(2):366–74.
Download references
Acknowledgements
Not applicable.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and affiliations.
Center for Eating Disorders Helmond, Mental Health Center Region Oost-Brabant, Wesselmanlaan 25a, Helmond, 5707 HA, The Netherlands
Ilona M.C. van den Eijnde-Damen, Joyce Maas, Pia Burger, Nynke M.G. Bodde & Mladena Simeunovic-Ostojic
Department of Medical and Clinical Psychology, Tilburg University, Warandelaan 2, Tilburg, 5037 AB, The Netherlands
You can also search for this author in PubMed Google Scholar
Contributions
Ilona v/d Eijnde-Damen: Data curation; Formal analysis, Investigation; Methodology; Project administration; Writing – original draft; Writing – review & editing. Joyce Maas: Writing – original draft; Writing – review & editing. Pia Burger: Writing – original draft; Writing – review & editing. Nynke Bodde: Writing – original draft; Writing – review & editing. Mladena Simeunovic-Ostojic: Conceptualization; Methodology, Supervision; Writing – original draft; Writing – review & editing.
Corresponding author
Correspondence to Joyce Maas .
Ethics declarations
Ethics approval and consent to participate.
The study was not subject to the Medical Research Involving Human Subjects Act. Participants signed informed consent before participation.
Consent for publication
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/ .
Reprints and permissions
About this article
Cite this article.
van den Eijnde-Damen, I.M., Maas, J., Burger, P. et al. Towards collaborative care for severe and enduring Anorexia Nervosa – a mixed-method approach. J Eat Disord 12 , 124 (2024). https://doi.org/10.1186/s40337-024-01091-z
Download citation
Received : 14 May 2024
Accepted : 19 August 2024
Published : 26 August 2024
DOI : https://doi.org/10.1186/s40337-024-01091-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Severe and Enduring Eating Disorders (SEED)
- Severe and Enduring Anorexia Nervosa (SE-AN)
- Collaborative care
Journal of Eating Disorders
ISSN: 2050-2974
- General enquiries: [email protected]

IMAGES
COMMENTS
Presentation of Case Dr. Lazaro V. Zayas (Psychiatry): An 11-year-old girl was seen in an outpatient clinic of this hospital because of difficulty eating solid food and associated weight loss ...
This case report illustrates an adolescent with clinical presentation of moderate anorexia nervosa with no significant co-morbidities. It highlights the management of anorexia nervosa in the outpatient setting by a multi-disciplinary health care team ...
Unfortunately, these patients and their carers often receive minimal support from eating disorders health professionals who are conflicted about terminal care, and who are hampered and limited by the paucity of literature on end-of-life care for those with anorexia nervosa. Three case studies elucidate this condition.
Abstract Anthropologists have paid much attention to food and eating practices in India, but surprisingly few scholars in any discipline have examined eating disorders. This article presents an ethnographic case study of disordered eating, based on a story of a young female pharmacist from one of the Northern Indian states.
Abstract. Anorexia nervosa is an eating disorder characterized by excessive restriction on food intake and irrational fear of gaining weight, often accompanied by a distorted body self-perception. It is clinically diagnosed more frequently in females, with type and severity varying with each case. The current report is a case of a 25-year-old ...
Emma's* journey through an eating disorder: From struggle to recovery, detailing support, therapy, and a promising future.
The story of Antonella illustrates the way in which cultural and other values impact on the presentation and treatment of eating disorders. Displaced from her European home culture to live in Canada, Antonella presents with an eating disorder and a fluctuating...
Background Eating disorders (ED), especially Anorexia Nervosa (AN), are internationally reported to have amongst the highest mortality and suicide rates in mental health. With limited evidence for current pharmacological and/or psychological treatments, there is a grave responsibility within health research to better understand outcomes for people with a lived experience of ED, factors and ...
Public Significance This study provides a comprehensive mapping and quality assessment of the current large systematic review research base regarding the effects of cognitive behavioral therapy (CBT) for eating disorders (EDs), with a focus on comparisons to other active interventions.
Primary care providers are well-positioned to iden-tify eating disorders early and initiate treatment. This case report describes an adaptation of Family-Based Treatment delivered by a primary care provider to an Asian-American male adolescent from an immigrant family with restrictive anorexia nervosa.
Toward a Biological, Psychological and Familial Approach of Eating Disorders at Onset: Case-Control ANOBAS Study Ana Rosa Sepúlveda 1* Alba Moreno-Encinas 1* José Angel Martínez-Huertas 2 Dimitra Anastasiadou 1 Esther Nova 3 Ascensión Marcos 3 Sonia Gómez-Martínez 3 José Ramón Villa-Asensi 4 Encarna Mollejo 5 Montserrat Graell 6,7
Anorexia Ner vosa is one of the eating disorders, a s classified. in the Diagnostic and Statistical Manual, the fifth edition. It is. characterised by a pathological fear of weight gain associated ...
One study of 21 adolescents that added a CBT-based perfectionism module to FBT (Hurst & Zimmer-Gembeck, 2019) reported correlations between improvements in perfectionism and improvements in eating disorder symptoms, but the limited case series data classifies this FBT treatment adaptation as Level 4 (experimental treatment).
Case Study Details. Maria is a 38-year-old divorced woman who works in a higher level administrative position for a large federal agency. She is well-established in her career and has several close friends with whom she enjoys spending time. She comes to you following years of unsuccessful attempts to get appropriate treatment for her binge eating.
The participants in our study participated in a rehabilitation programme for BED. They experienced living with BED as a challenging addiction. Low self-image and others' lack of understanding made the individuals ashamed of their eating disorders.
This clinical case involves an obese woman requesting treatment for her binge eating and obesity. The information is presented to expert clinicians who provide their thoughts regarding the case, assessment, treatment formulation, and associated clinical and research issues. Go to:
Abstract This case study involved the treatment of a young adult female, referred to as "Marie," who presented for treatment seeking help with her eating disorder. Marie evinced symptoms of dietary restriction, amenorrhea, low weight, and low body mass index (BMI); she was subsequently diagnosed with anorexia nervosa. She was treated with 20 sessions of enhanced cognitive-behavioral ...
Substantial progress has been made in the understanding of anorexia nervosa (AN) and eating disorder (ED) genetics through the efforts of large-scale collaborative consortia, yielding the first ...
Background Risk factors represent a range of complex variables associated with the onset, development, and course of eating disorders. Understanding these risk factors is vital for the refinement of aetiological models, which may inform the development of targeted, evidence-based prevention, early intervention, and treatment programs. This Rapid Review aimed to identify and summarise research ...
The First Episode Rapid Early Intervention for Eating Disorders (FREED) is an innovative service model that has offered support to over 1,200 16 to 25-year-olds who have had an eating disorder for three years or less. There are two key things that can prevent early intervention in eating disorders: difficulties spotting the illness early, and ...
Video Case Study - Eating Disorders Videos, Flashcards, High Yield Notes, & Practice Questions. Learn and reinforce your understanding of Video Case Study - Eating Disorders.
In this sense, previous studies have established that the probability of developing a disordered eating attitude or a diagnosis of eating disorders is higher if the mother had a disordered eating or self-esteem problems [ 25, 26 ]. Moreover, ethnicity has been linked to the perception of beauty ideals, self-esteem and body perception [ 27, 28 ].
Background Severe and Enduring Eating Disorders (SEED), in particular SEED-Anorexia Nervosa (SE-AN), may represent the most difficult disorder to treat in psychiatry. Furthermore, the lack of empirical research in this patient group, and, consequently the lack of guidelines, call for an urgent increase in research and discussion within this field. Meanwhile experts concur that effective care ...