Myanmar’s response to the COVID-19 pandemic
Subscribe to global connection, ashwini deshpande , ashwini deshpande associate in research at the center for policy impact in global health - duke university khaing thandar hnin , and khaing thandar hnin director - strategy, technical, policy and research unit - community partners international tom traill tom traill policy and research director - community partners international.
December 1, 2020
During the first wave of the coronavirus pandemic, from late March to early August, Myanmar recorded just 360 cases and 6 deaths. Early in the crisis, the government rapidly implemented measures to contain the virus. Just as it started easing them though, the country was hit by a major second wave in mid-August. Daily cases increased from less than 10 per day in early August to over 1,000 per day in mid-October . This wave has overwhelmed Myanmar’s inadequate and understaffed health infrastructure. By November 20, there were 76,414 confirmed cases and 1,695 deaths (Figure 1).

Figure 1 a. Cumulative active confirmed cases, discharged patients and deaths

Figure 1b. COVID-19 cases by region

Source: Ministry of Health and Sports, Myanmar . Note: Data as of November 20, 2020 .
In the November 2020 national elections, Myanmar civilian leader Aung San Suu Kyi’s party won comfortably to stay in power. The government now faces the task of stemming the rapid increase in cases. What can the country do to quickly contain COVID-19? Duke University’s Center for Policy Impact in Global Health and Community Partners International in Yangon analyzed Myanmar’s pandemic preparedness and its policy response to provide an answer to this question. Besides summarizing the current situation of the COVID-19 pandemic, our recent policy report identifies policy gaps that the new government has to plug.
Weaknesses: Testing capacity, health infrastructure, income security, and domestic stability
A day after the World Health Organization notified governments about the unexplained pneumonia cases in Wuhan in January, Myanmar set up surveillance at points of entry to the country. Since March, it has implemented domestic and international travel restrictions while issuing guidance on personal hygiene, COVID-19 symptoms, and social restrictions in public spaces (Figure 2).
Figure 2. Timeline of the policy and coordination measures by the Myanmar government

Key: blue indicates public health policies; green indicates social and economic measures; orange indicates health system respo nse
Inadequate testing capacity. Since the start of the pandemic, the government took steps to expand its testing capacity. In early October, it could conduct over 10,000 tests daily, a substantial rise from the 380 tests per day in March. But this is not enough to keep pace with the soaring second wave. Since mid-October, the rate of positive tests has been about 10 percent —implying that the confirmed cases represent only a small fraction of infected people. As of November 22, Myanmar had conducted 1,998.7 tests per 100,000 people . Limited availability of detection systems, dependence on other countries for testing kits, and shortages of human resources such as trained laboratory technicians and logistics and data managers are some of the main factors compromising laboratory testing.
Unprepared health system. According to the 2019 Global Health Security Index , Myanmar was least prepared in terms of the availability of health systems to treat the sick and protect health care workers. Myanmar had just 6.7 physicians per 10,000 people in 2018, significantly lower than the global average of 15.6 physicians per 10,000 people in 2017. Besides, it only had 10.4 hospital beds per 10,000 people. In March 2020, Myanmar reported just 0.71 intensive care unit beds and 0.46 ventilators per 100,000 population, which were insufficient to deal with even a moderate outbreak. The government has increased surge capacity by constructing makeshift hospitals, quarantine centers, and clinics; and procuring ventilators and securing funding for ICU units. But these efforts are compromised by the scarcity of medical staff . The government has called upon volunteers to work at state quarantine centers, but mandatory 14-day quarantine and increasing caseloads have stressed volunteers. In addition, some of the quarantine centers are reportedly poorly managed , increasing the transmission risk in centers; 10 percent of the total confirmed cases in the second wave are among health care workers.
Income and food shortages . Myanmar’s economy has been hurt badly by the pandemic, giving rise to income and food insecurity. The sharp decline in remittances due to the pandemic is likely to reduce household income. Eighty percent of Myanmar’s workforce is informal. Scores of day laborers have lost their jobs. Women constitute a majority of the hospitality and garment sectors, so they have been disproportionately affected by factory closures. About 4 out of 5 households reported skipping meals, and others have incurred debt to buy food. The government implemented several measures under the COVID-19 Economic Relief Plan (CERP) such as unemployment benefits to registered workers, targeted cash assistance, and a one-time food distribution to households without a regular income. It established a fund of 400 billion kyat (around $309 million) to support garment, tourism, and small and medium enterprises (SMEs) via soft loans. Soft loans were also extended to farmers, roadside vendors, and the microfinance sector. But the current cash transfer of MMK40,000 per household translates to a daily income equivalent that is below the poverty line . Besides, the CERP lacks policies that target women who have lost their livelihoods due to the pandemic.
Domestic unrest. Conflict between the government and the Ethnic Armed Organizations (EAOs) makes it hard to organize an effective pandemic response. The conflict has led to the displacement of the population as well as the disruption of transport routes and supply chains. In May, the committee that coordinates and collaborates with EAOs to control and treat COVID-19 announced a unilateral ceasefire with EAOs, but the strife between the military and the Arakan Army continues in Rakhine and Chin. As of November 20, Rakhine had the fourth-highest confirmed cases in the country, and they continue to grow. The government has supplied personal protective equipment at campsites for internally displaced persons (IDPs), but congestion and poor living conditions in IDP camps heighten transmission risk.
Solutions: More testing, better quarantine facilities, and critical care in conflict zones
Myanmar is yet to reach the peak of the COVID-19 outbreak, so the full scale of responses to tackle the pandemic is still not clear. But the current state of the pandemic, the government’s responses, and lessons from other countries point to three areas that need attention.
- Increase testing capacity. Myanmar has to build capacity and forge connections with local clinicians and businesses to make affordable testing kits and essential supplies. The state should train nongovernment health care workers to test for COVID-19 and permit nongovernment laboratories to analyze swabs.
- Improve the quarantine facility model. Myanmar might consider incorporating the Fangcang shelter model into new quarantine centers. This model has been proven to provide critical functions of isolation, triage, basic medical care, frequent monitoring, rapid referral, and essential living and social engagement to manage COVID-19 patients effectively.
- Mitigate economic impacts on vulnerable populations. The government is currently drafting the Myanmar Economic Recovery and Reform Plan (MERRP). The plan needs to consider household size, cost of living, and vulnerabilities in determining the transfer amount and frequency. To alleviate food insecurity and circumvent problems related to in-kind distribution, it should include a food allowance in the direct cash transfer. The government also needs to ensure adequate access to loans, grants, or credit to sectors that predominantly employ women.
- Ensure critical health care in conflict regions. The government needs to increase its reach in conflict regions to disseminate vital information on COVID-19. This can best be done by providing more autonomy to Ethnic Health Organizations (EHOs). It needs to improve existing processes for transporting swab samples from the conflict areas to laboratories and regularly exchanging information on testing, contact tracing, and delivery of other essential health services. The government needs to build on the existing cooperation with EHOs and other nonstate actors to plan for large scale vaccination of vulnerable populations in 2021.
- Continue provision of other essential health services. The pandemic has disrupted the provision of other essential health services, including antiretroviral therapy for HIV, the expanded program on immunization, family planning, and maternal health services. The government should seek investments for key health services from public-private partnerships, and international development organizations, increase human resources in the health sector, and consider moving appropriate health services to virtual platforms.
Related Content
Jonathan Stromseth, Thant Myint-U, Fred Dews
December 13, 2019
Massimiliano Cali
November 20, 2020
Myanmar Southeast Asia
Global Economy and Development
Asia & the Pacific Myanmar Southeast Asia
The Brookings Institution, Washington D.C.
11:30 am - 12:30 pm EDT
Sudha Ghimire
August 22, 2024
Michael E. O’Hanlon
August 15, 2024

Learn about our mission, our charter and principles, and who we are.
See what triggers an intervention and how supply and logistics allow our teams to respond quickly.
Discover our governance and what it means to be an association. Find a quick visual guide to our offices around the world.
Read through our annual financial and activity reports, and find out about where our funds come from and how they are spent.
Visit this section to get in touch with our offices around the world.
Médecins Sans Frontières brings medical humanitarian assistance to victims of conflict, natural disasters, epidemics or healthcare exclusion.

Learn about how, why, and where MSF teams respond to different diseases around the world, and the challenges we face in providing treatment.

Learn about the different contexts and situations in which MSF teams respond to provide care, including war and natural disaster settings, and how and why we adapt our activities to each.

Learn about our response and our work in depth on specific themes and events.
Where we work
In more than 70 countries, Médecins Sans Frontières provides medical humanitarian assistance to save lives and ease the suffering of people in crisis situations.
MSF Websites
- Czech Republic
- Eastern Africa
- New Zealand
- Philippines
- Russian Federation
- Southern Africa
- South Korea
- Switzerland
Our staff “own” and manage MSF, making sure that we stay true to our mission and principles, through the MSF Associations.
We set up the MSF Access Campaign in 1999 to push for access to, and the development of, life-saving and life-prolonging medicines, diagnostic tests and vaccines for people in our programmes and beyond.
Read stories from our staff as they carry out their work around the world.
Hear directly from the inspirational people we help as they talk about their experiences dealing with often neglected, life-threatening diseases.
Based in Paris, CRASH conducts and directs studies and analysis of MSF actions. They participate in internal training sessions and assessment missions in the field.
Based in Geneva, UREPH (or Research Unit) aims to improve the way MSF projects are implemented in the field and to participate in critical thinking on humanitarian and medical action.
Based in Barcelona, ARHP documents and reflects on the operational challenges and dilemmas faced by the MSF field teams.
Based in Brussels, MSF Analysis intends to stimulate reflection and debate on humanitarian topics organised around the themes of migration, refugees, aid access, health policy and the environment in which aid operates.
This logistical and supply centre in Brussels provides storage of and delivers medical equipment, logistics and drugs for international purchases for MSF missions.
This supply and logistics centre in Bordeaux, France, provides warehousing and delivery of medical equipment, logistics and drugs for international purchases for MSF missions.
This logistical centre in Amsterdam purchases, tests, and stores equipment including vehicles, communications material, power supplies, water-processing facilities and nutritional supplements.
SAMU provides strategic, clinical and implementation support to various MSF projects with medical activities related to HIV and TB. This medical unit is based in Cape Town, South Africa.
Regional logistic centre for the whole East Africa region
BRAMU specialises in neglected tropical diseases, such as dengue and Chagas, and other infectious diseases. This medical unit is based in Rio de Janeiro, Brazil.
Our medical guidelines are based on scientific data collected from MSF’s experiences, the World Health Organization (WHO), other renowned international medical institutions, and medical and scientific journals.
Find important research based on our field experience on our dedicated Field Research website.
The Manson Unit is a London, UK-based team of medical specialists who provide medical and technical support, and conduct research for MSF.
Providing epidemiological expertise to underpin our operations, conducting research and training to support our goal of providing medical aid in areas where people are affected by conflict, epidemics, disasters, or excluded from health care.
Evaluation Units have been established in Vienna, Stockholm, and Paris, assessing the potential and limitations of medical humanitarian action, thereby enhancing the effectiveness of our medical humanitarian work.
MSF works with LGBTQI+ populations in many settings over the last 25-30 years. LGBTQI+ people face healthcare disparities with limited access to care and higher disease rates than the general population.
The Luxembourg Operational Research (LuxOR) unit coordinates field research projects and operational research training, and provides support for documentation activities and routine data collection.
The Intersectional Benchmarking Unit collects and analyses data about local labour markets in all locations where MSF employs people.
To upskill and provide training to locally-hired MSF staff in several countries, MSF has created the MSF Academy for Healthcare.
This Guide explains the terms, concepts, and rules of humanitarian law in accessible and reader-friendly alphabetical entries.
The MSF Paediatric Days is an event for paediatric field staff, policy makers and academia to exchange ideas, align efforts, inspire and share frontline research to advance urgent paediatric issues of direct concern for the humanitarian field.
The MSF Foundation aims to create a fertile arena for logistics and medical knowledge-sharing to meet the needs of MSF and the humanitarian sector as a whole.
A collaborative, patients’ needs-driven, non-profit drug research and development organisation that is developing new treatments for neglected diseases, founded in 2003 by seven organisations from around the world.
View Resource Centre

- Responding to COVID-19 during political crisis in Myanmar
Political turmoil and the arrival of COVID-19 has left Myanmar's healthcare system shattered. With 2021 coming to an end, our team on the ground look back at our COVID-19 response, reflecting on what we can be proud of and what we could have done better; the dilemmas, limits and the sometimes-uncomfortable solutions.
Myanmar’s public healthcare system is in disarray. Days after the military seized power on 1 February, medical staff walked out of their jobs, spearheading the civil disobedience movement that saw government employees of all stripes go on strike. Most have not returned. Those on strike who continue to practice in underground clinics risk being attacked and detained by the authorities. At least 28 healthcare professionals have been killed since 1 February, and nearly 90 remain arrested. When Myanmar’s beleaguered public healthcare system met with the COVID-19 outbreak, hospitals were quickly overwhelmed.

Overcrowded crematoriums and empty shelves
As COVID-19 infections peaked, beds in hospitals were often impossible to come by and untold numbers of people were scrambling around towns and cities in Myanmar to source their own supplies of oxygen to administer at home. Crematoriums could not process the bodies fast enough. Routine consultations, surgeries and vaccinations were cancelled while the skeleton medical workforce responded to the outbreak. Panic buying led to empty shelves in pharmacies. Myanmar’s Ministry of Health counts nearly 20,000-recorded deaths from COVID-19 up to the end of 2021 – the fourth highest mortality rate in south-east Asia. But this figure is misleading – only counting people who died in hospitals. Countless individuals passed away in their homes while facilities were full.

How did MSF respond?
We were granted permission to open three independent COVID-19 treatment centres to receive patients with moderate to severe symptoms in Myanmar’s biggest city Yangon, and Kachin state’s Myitkyina and Hpakant townships. Remarkably, while some of us fell seriously ill with the virus, no one on the team lost their life to COVID-19, but many of our family members did. Despite this, we pulled together and looked after each other, working overtime to get the centres up-and-running for people we knew were in urgent need of its services. Although we could not save some patients admitted in very critical condition, some people made remarkable recoveries. One woman living with HIV could barely breathe when she arrived at our facility. But in five days she was off oxygen and could be discharged, making way for another patient. For others, the progress is slow and steady. One 64-year-old woman was in our Myitkyina clinic for 46 days, slowly improving her lung capacity until her oxygen levels were good enough for her to go home.

When there are no acceptable solutions
Our response could have and should have been bigger. While we had permissions to run independent COVID-19 responses in three locations, not all local health authorities were on the same page. We had begun supporting a facility in Lashio, the capital of northern Shan state, on 11 August, but one person within the Lashio healthcare structure ordered us to close it down on 15 August. Days after receiving our first patients, we were forced to transfer six people receiving treatment to the military government’s treatment centre, despite their preference to receive care from MSF.
Did we respond in time?
By the time our first treatment centre was up-and-running in early August, COVID-19 was already devastating the country. If we had been better prepared and more reactive, could we have responded sooner and saved more lives? The answer is an uncomfortable yes. The Delta variant had overwhelmed India and Bangladesh in the months before – two countries that share a 2,000-kilometre border with Myanmar. Its arrival was inevitable. We could have used that time to prepare and equip ourselves, and to have learned from the challenges our colleagues had faced in India where access to oxygen was one of the biggest issues. When the third wave hit, Myanmar was six months into the military takeover. The team was already working at full stretch to maintain existing activities and fill the gaps left in the struggling public healthcare system, in particular taking on thousands of HIV patients from the state’s National AIDS Programme . By the time we initiated our response in the middle of July, we were already on the back foot.
We did not always get it right
There was a belief that we could simply put people on oxygen and save lives. This was not the reality of treating COVID-19 patients. Those who are hospitalised with severe symptoms often have underlying conditions, exacerbating their symptoms and complicating their treatment. We needed essential drugs like insulin and basic cardiovascular medication, but they were not in our warehouse and we could not get them into the country due to convoluted internal processes and difficulties obtaining import permits. We had an emergency preparation kit for COVID-19, but what we had expected to be there was missing, such as medicine to treat blood clots, and the supplies that were included were quickly exhausted.
Committed and ready
Although internal and external constraints and challenges caused difficulties, our COVID-19 facilities are now much more than field clinics – they are excellent hospitals that have saved many lives and will save many more to come. Only around 13 million people in Myanmar are fully vaccinated – around a quarter of the population. If another wave of infections spreads, the public healthcare system risks being overwhelmed once again. With that in mind, we are maintaining our COVID-19 infrastructure and keeping medical staff on-hand should there be another outbreak. Although our supplies of essential medicines have improved, importing them remains an issue. Permissions are currently under more scrutiny than prior to the military takeover, delaying shipments. Furthermore, internal MSF processes and policies for local or regional procurement of medicines have not adapted well to the global supply crisis and often hinder emergency purchases. We have learned many lessons from the challenges we faced the first time round and remain committed and ready to respond to new and unexpected challenges to come.

Lack of a real IP waiver on COVID-19 tools is a disappointing failure for people

“Broken” humanitarian COVID-19 vaccine system delays vaccinations

Vaccinating people with comorbidities in South Africa
- News releases
- Report an incident of misconduct
- Work with us
- ICRC Supply Chain
Myanmar: ICRC strives to ensure ample COVID-19 response
- COVID-19 pandemic
- Protected persons: Internally displaced persons
- Helping detainees

In Myanmar, and many other countries where the International Committee of the Red Cross (ICRC) is present, the threat of COVID-19 is particularly acute for communities living in areas affected by armed conflict and other situations of violence, as well as for some particularly vulnerable groups such as internally displaced persons (IDP), people deprived of freedom, or migrants.
In support of the Myanmar government's actions to prevent and mitigate the risks associated with COVID-19, the ICRC, along with the Myanmar Red Cross Society (MRCS) and its other partners from the International Red Cross and Red Crescent Movement, is striving to ensure that people affected by armed conflict and other situations of violence are not left behind, and they receive the assistance and protection to which they are entitled in line with the international humanitarian law.
Between March and mid-June 2020, Myanmar's Ministry of Health and Sports has confirmed over 300 positive COVID-19 cases. Despite the low-infection rate in the country, the ICRC remains concerned for tens of thousands of families affected by armed conflict and violence, including displaced people living in temporary shelters and IDP sites.
In response to these concerns, across the country, the MRCS, as an auxiliary to the public authorities, is providing valuable support to the national COVID-19 response through its network of staff and volunteers activated in 277 townships.

Hygiene kit donation in Myitkyina, Kachin
The International Federation of Red Cross and Red Crescent Societies (IFRC) - with the mandate to scale up for disasters and pandemics - is supporting the MRCS through the international mobilization of financial, technical and logistics resources.
For the ICRC, ongoing programmes have been swiftly adapted to the new realities of the virus in order to ensure the continuity of life-saving activities such as food distributions, or the evacuations of weapon-wounded civilians in areas affected by conflict.
At the same time, in coordination with the relevant authorities and the MRCS, the ICRC rapidly developed a wide range of COVID-19-prevention activities in the areas of health care, water and habitat, or protection.
The ICRC has also engaged non-state armed groups, ethnic health organizations, religious leaders and local media to provide assistance and convey COVID-19 prevention messages to communities.

Lashio prison donation
The ICRC also considers that special attention is required for prison populations who face a higher risk of contamination when facilities are overcrowded, have poor hygiene, or lack ventilation. The ICRC supported prison authorities for prevention and infection control in detention facilities, as well as the organization of the safe return home of 2,500 detainees released following the annual presidential pardon.
ICRC COVID-19 response in Myanmar from ICRC on Vimeo .
Our teams are working to improve living conditions in existing and new IDP sites by improving basic shelter, access to safe water, and building basic latrines for better hygiene.
The ICRC plans to adjust its economic security programmes to contribute to addressing these gaps in the coming months, whether through cash programming or covering basic humanitarian needs, so that those who are most affected and exposed to the impacts of COVID-19 are less vulnerable.

"In the new context of COVID-19, it remains a top priority for the ICRC to continue protecting and assisting people affected by armed conflict and violence while reminding all parties of their obligation, under the International Humanitarian Law, to ensure access to health care to all communities," explains Stephan Sakalian, resident representative for the ICRC in Myanmar.
"It is the responsibility of everyone to act when faced with such a global and far-reaching crisis."

Sittwe prison donation
"We also need to join the efforts of the authorities, Myanmar Red Cross Society, civil society and the whole humanitarian and development community to prevent and mitigate the risks associated with COVID-19 in Myanmar. It is the responsibility of everyone to act when faced with such a global and far-reaching crisis," he added.
"It is the responsibility of everyone to act when faced with such a global and far-reaching crisis"
Myanmar: ICRC Response to COVID-19 in 2020
Related articles.

Lebanon: ICRC on the ground

Azerbaijan: Activity highlights for the first half of 2024

What does the law say about the responsibilities of the Occupying Power in the occupied Palestinian territory?
Myanmar: COVID-19 third wave has hit like a ‘tsunami’, warns WFP

Facebook Twitter Print Email
The World Food Programme ( WFP ) warned on Friday that it is facing a 70 per cent funding shortfall in Myanmar, where millions face growing food insecurity.
Amid the “triple impact of poverty, the current political unrest and economic crisis”, coupled with the rapidly spreading third wave of COVID-19 , that is “practically like a tsunami that’s hit this country”, the people of Myanmar are “experiencing the most difficult moment in their lives ”, WFP Myanmar Country Director Stephen Anderson said, from Nay Pyi Taw.
Hunger doubles
WFP needs $86 million to help fight hunger in the country over the next six months, amid turmoil since the military ousted the elected government led by Aung San Suu Kyi on 1 February.
World Food Programme
In April, the UN agency estimated that the number of people facing hunger could more than double to 6.2 million in the next six months, up from 2.8 million prior to February.
Subsequent monitoring surveys carried out by WFP have shown that since February, more and more families are being pushed to the edge, struggling to put even the most basic food on the table.
“We have seen hunger spreading further and deeper in Myanmar. Nearly 90 per cent of households living in slum-like settlements around Yangon say they have to borrow money to buy food ; incomes have been badly affected for many,” said Mr Anderson.
Tripling in support
In response, the WFP tripled its planned support to the country and starting in May, launched a new urban food response, targeting 2 million people in Yangon and Mandalay, Myanmar’s two biggest cities.
The majority of people to receive assistance are mothers, children, people with disabilities and the elderly. To date, 650,000 people have been assisted in urban areas .
At the same time, the WFP is “stepping up its operations” to reach newly displaced people affected by the clashes and insecurity in recent months. More than 220,000 people have fled violence since February, and are in urgent need of humanitarian assistance.
WFP has reached 17,500 newly displaced people and is working to assist more in August.
In total, 1.25 million people in Myanmar have received WFP food, cash and nutrition assistance in 2021 across urban and rural areas, including 360,000 food-insecure people in Rakhine, Kachin and Shan states, where there have been longstanding concerns.
Access critical
However, with $86 million more required over the next six months, it is uncertain how far these operations can go.
“It is critically important for us to be able to access to all those in need and receive the funding to provide them with humanitarian assistance,” Anderson explained. “ Now more than ever, the people of Myanmar need our support ,” he added.
Licence or Product Purchase Required
You have reached the limit of premium articles you can view for free.
Already have an account? Login here
Get expert, on-the-ground insights into the latest business and economic trends in more than 30 high-growth global markets. Produced by a dedicated team of in-country analysts, our research provides the in-depth business intelligence you need to evaluate, enter and excel in these exciting markets.
View licence options
Suitable for
- Executives and entrepreneurs
- Bankers and hedge fund managers
- Journalists and communications professionals
- Consultants and advisors of all kinds
- Academics and students
- Government and policy-research delegations
- Diplomats and expatriates

How is Covid-19 transforming Myanmar’s digital economy?

Covid-19 has shaken up the development of the digital economy in Myanmar, with the pandemic leading to a rise in demand for home broadband in this traditionally mobile-first market.

As various containment measures were imposed, companies located in the main business hubs scrambled to ensure that employees were able to work remotely .
“Household broadband demand increased because businesses were afraid that their workers would not be connected. We have very good mobile coverage in Myanmar, but this system is not designed for working from home for 10 hours per day,” Shane Thu Aung, co-founder and chairman of the Yangon-based Global Technology Group – which includes high-speed broadband service 5BB – told OBG.
In addition to simply improving internet connectivity in the home, virus-related disruptions have also seen companies look to different products to enable a smooth transition for those working remotely .
In particular, cloud services are being utilised to help cope with spikes in data demand.
“Almost all companies are now using video conferencing tools, and they have also explored cloud services so they can access their work systems from home,” Aung said. “They need to connect through the cloud due to heavy user traffic. Most government and private sector applications are also going over to the cloud.”
Aside from a shift towards home broadband in a country that has traditionally focused on developing strong mobile internet connectivity, businesses have also sought to adapt to increased demand for digital payments – further accelerating the demand for internet services.
In order to avoid cash transactions, a number of restaurants and shops have pivoted towards e-commerce platforms.
These shifts in consumer demand and behaviour have led to fresh investment in the sector, with Singapore-registered, Myanmar-focused Ascent Capital Partners committing $26m to local internet service provider Frontiir.
The funding, announced in late June, will help Frontiir expand its internet services across the country. The company currently serves 1.6m consumers across 360,000 households in four states and regions.
In addition to this investment, Ascent Capital Partners has also set aside additional financing towards mitigating the economic fallout of the virus in Myanmar.
Government-driven digital expansion
The increased uptake of digital products and platforms has also been supported by Myanmar’s post-pandemic recovery strategy.
Among the seven goals that comprise its Covid-19 Economic Relief Plan, announced in late April, the government prioritised the promotion of “innovative products and platforms”.
This includes encouraging the use of mobile payment services, bank transfers and card payments for e-commerce sales, as well as increasing the uptake of e-commerce options among businesses.
Such measures will build on previous efforts to improve the country’s ICT infrastructure and connectivity, which in recent years have focused on liberalising the industry and incentivising private investors.
In terms of internet coverage, the country’s Myanmar Digital Economy Roadmap aims to increase internet penetration from 40% in 2019 to 50% by 2025.
However, much of this coverage stems from mobile internet, with fixed broadband penetration still in the single digits, indicating significant room for further growth.
Cybersecurity in the spotlight
While the virus spurred plans to upgrade ICT infrastructure amid the increased uptake of digital platforms and services, there are nevertheless some concerns about the country’s capacity to legislate for the digital transformation.
“Many small businesses are considering how to digitalise their businesses, including trade and import procedures. However, regulations do not really reflect this, particularly for trade and Customs,” Aung told OBG. “Some government officials are responsive to the need for change, but more needs to be done. If Myanmar’s laws do not reflect these changes we will fall behind. There is a time gap and Myanmar is losing its advantage.”
One particular area of concern amid the rapid shift online is that of data protection, with fears that many companies may be unprepared to address cyber risks.
The government has been working on developing a dedicated cybersecurity law since 2018, and while there have been efforts to increase awareness through the opening of the National Cybersecurity Centre, some believe the country remains exposed to a significant level of threat.
“Suddenly everyone is worried about data security, and the government is alarmed about data classification and storage. This shows the need for a comprehensive cybersecurity law,” Aung said.
Request Reuse or Reprint of Article
Read More from OBG
Construction – and infrastructure development in particular – is expected to be a key driver of economic growth across ASEAN from 2021. The bloc, home to some of the world’s fastest-growing economies and lowest unemployment rates, faced the novel coronavirus after years of health care infrastructure improvements, with much of the group reporting Covid-19 case-fatality rates below the global mean in 2020.

Report: Oman’s digital economy and its transformative potential Oman's digital transformation is revolutionising its economy and society. With the National Programme for Digital Economy driving progress, the country is bolstering its telecommunications infrastructure, expanding e-government services, developing a competitive space industry and embracing cutting-edge technologies such as artificial intelligence (AI). This report provides insights into Oman's digital journey, highlighting advancements in connectivity, AI innovation, cybersecurity a…
Informe: Corredor Interoceánico de México como alternativa al Canal de Panamá In English El Corredor Interoceánico de México y el complejo industrial de Texistepec están emergiendo como un nodo de desarrollo clave que conecta el Océano Pacífico y el Océano Atlántico, y como un centro para el transporte y el comercio internacional. El corredor, que abarca 300 km y une dos de los principales puertos del país, ofrece importantes oportunidades para el desarrollo económico en las regiones menos desarrolladas del sur y sureste de México. Este informe, e…

Register for free Economic News Updates on Myanmar
“high-level discussions are under way to identify how we can restructure funding for health care services”, related content.
Featured Sectors in Myanmar
- Myanmar Agriculture
- Myanmar Banking
- Myanmar Construction
- Myanmar Cybersecurity
- Myanmar Digital Economy
- Myanmar Economy
- Myanmar Education
- Myanmar Energy
- Myanmar Environment
- Myanmar Financial Services
- Myanmar Health
- Myanmar ICT
- Myanmar Industry
- Myanmar Insurance
- Myanmar Legal Framework
- Myanmar Logistics
- Myanmar Media & Advertising
- Myanmar Real Estate
- Myanmar Retail
- Myanmar Safety and Security
- Myanmar Saftey and ecurity
- Myanmar Tax
- Myanmar Tourism
- Myanmar Transport
Featured Countries in ICT
Popular Sectors in Myanmar
Popular Countries in ICT
- Indonesia ICT
- The Philippines ICT
- Saudi Arabia ICT
- UAE: Abu Dhabi ICT
Featured Reports in Myanmar
Recent Reports in Myanmar
- The Report: Myanmar 2020
- The Report: Myanmar 2019
- The Report: Myanmar 2018
- The Report: Myanmar 2017
- The Report: Myanmar 2016
- The Report: Myanmar 2015
Privacy Overview
| Cookie | Duration | Description |
|---|---|---|
| cookielawinfo-checkbox-analytics | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Analytics". |
| cookielawinfo-checkbox-functional | 11 months | The cookie is set by GDPR cookie consent to record the user consent for the cookies in the category "Functional". |
| cookielawinfo-checkbox-necessary | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookies is used to store the user consent for the cookies in the category "Necessary". |
| cookielawinfo-checkbox-others | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Other. |
| cookielawinfo-checkbox-performance | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Performance". |
| viewed_cookie_policy | 11 months | The cookie is set by the GDPR Cookie Consent plugin and is used to store whether or not user has consented to the use of cookies. It does not store any personal data. |
Myanmar’s Economy Severely Impacted by COVID-19: Report
YANGON, June 25, 2020 – The global COVID-19 pandemic is dealing a severe blow to Myanmar’s economy. Economic growth in a baseline scenario is projected to drop from 6.8 percent in FY18/19 to just 0.5 percent in FY2019/20, according to the World Bank’s Myanmar Economic Monitor , released today.
If the pandemic is protracted, the economy could contract by as much as 2.5 percent in FY2019/20, with the expected recovery in 2020/21 subject to further downside risks.
The slowing economic growth threatens to partially reverse Myanmar’s recent progress in poverty reduction while reducing the incomes of households that are already poor. Under the baseline scenario, in which the domestic spread of the coronavirus is brought under control, the global economy swiftly recovers, and Myanmar’s GDP growth rate is projected to bounce back to 7.2 percent in FY2020/21, poverty rates would increase in the short term and will not return to pre-crisis levels until FY2021/22. Under the downside scenario, poverty rates would remain above their pre-crisis level until at least FY2022/23.
The report also looks at the Myanmar government’s response to the crisis through the COVID-19 fund and Economic Relief Plan (CERP), which includes measures to offer relief and initiate a resilient recovery - including tax relief, credit for businesses, food and cash to households, as well as policies to facilitate trade and investment.
“At the moment the medium-term outlook for Myanmar’s economy is positive, but there are significant downside risks due to the unpredictable evolution of the pandemic. Robust policy actions are urgently needed. It will be important for the government to boost the effectiveness of the CERP by ensuring flexibility in spending targets, extending support to smaller enterprises and ensuring all poor households can benefit from the plan,” said Mariam Sherman, World Bank Country Director for Myanmar, Cambodia and Lao PDR.
The report highlights that the effects of the crisis are not being evenly felt across sectors. Industrial production is expected to contract by 0.2 percent in FY2019/20 as lockdown measures restrict access to labor, the closure of the overland border with China disrupts the supply of industrial inputs, and consumer demand—both domestic and international—remains soft. Precautionary behavior and travel bans continue to negatively impact wholesale and retail trade, tourism-related services, and transportation. Due to the ongoing disruption of supply chains and weakening external demand, exports are expected to remain weak over the rest of the fiscal year. Tax revenues are projected to decline by 6.0 percent, year-on-year, in FY2019/20.
Meanwhile the agriculture sector has so far proven to be more resilient, and the Information and Communications Technology (ICT) sector is experiencing a surge of activity driven by a sharp increase in telecommuting and e-commerce. Falling consumer demand under COVID-19 is moderating inflation.
The Myanmar Economic Monitor is a biannual analysis of economic developments, economic prospects and policy priorities in Myanmar. The publication draws on available data reported by the Government of Myanmar and additional information collected as part of the World Bank Group’s regular economic monitoring and policy dialogue.
- Press release (Burmese)
- Key findings: Myanmar Economic Monitor June 2020
- Video: The Impact of COVID-19 on Myanmar's Economy
- Download report
- Executive summary
- Presentation (ppt)
- Myanmar COVID-19 Monitoring Platform
- Myanmar Economic Monitors
- Full launch video
Myanmar: Coronavirus Pandemic Country Profile
Research and data: Edouard Mathieu, Hannah Ritchie, Lucas Rodés-Guirao, Cameron Appel, Daniel Gavrilov, Charlie Giattino, Joe Hasell, Bobbie Macdonald, Saloni Dattani, Diana Beltekian, Esteban Ortiz-Ospina, and Max Roser
- Coronavirus
- Data explorer
- Hospitalizations
Vaccinations
- Mortality risk
- Excess mortality
- Policy responses
Build on top of our work freely
- All our code is open-source
- All our research and visualizations are free for everyone to use for all purposes
Select countries to show in all charts
Confirmed cases.
- What is the daily number of confirmed cases?
- Daily confirmed cases: how do they compare to other countries?
- What is the cumulative number of confirmed cases?
- Cumulative confirmed cases: how do they compare to other countries?
- Biweekly cases : where are confirmed cases increasing or falling?
- Global cases in comparison: how are cases changing across the world?
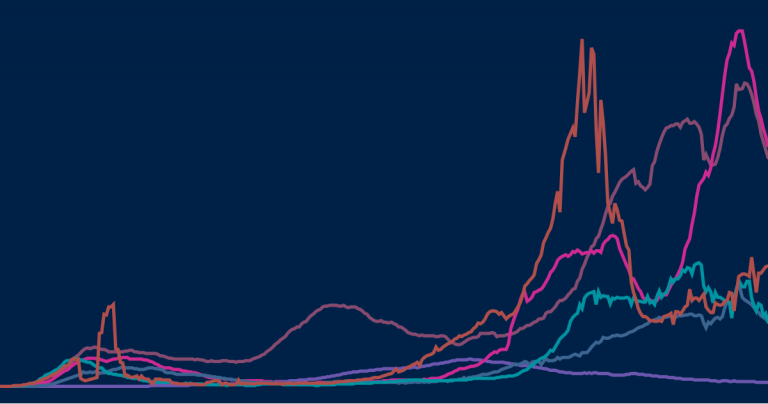
Myanmar: What is the daily number of confirmed cases?
Related charts:.
Which world regions have the most daily confirmed cases?
This chart shows the number of confirmed COVID-19 cases per day . This is shown as the seven-day rolling average.
What is important to note about these case figures?
- The reported case figures on a given date do not necessarily show the number of new cases on that day – this is due to delays in reporting.
- The number of confirmed cases is lower than the true number of infections – this is due to limited testing. In a separate post we discuss how models of COVID-19 help us estimate the true number of infections .
→ We provide more detail on these points in our page on Cases of COVID-19 .
Five quick reminders on how to interact with this chart
- By clicking on Edit countries and regions you can show and compare the data for any country in the world you are interested in.
- If you click on the title of the chart, the chart will open in a new tab. You can then copy-paste the URL and share it.
- You can switch the chart to a logarithmic axis by clicking on ‘LOG’.
- If you move both ends of the time-slider to a single point you will see a bar chart for that point in time.
- Map view: switch to a global map of confirmed cases using the ‘MAP’ tab at the bottom of the chart.
Myanmar: Daily confirmed cases: how do they compare to other countries?
Differences in the population size between different countries are often large. To compare countries, it is insightful to look at the number of confirmed cases per million people – this is what the chart shows.
Keep in mind that in countries that do very little testing the actual number of cases can be much higher than the number of confirmed cases shown here.
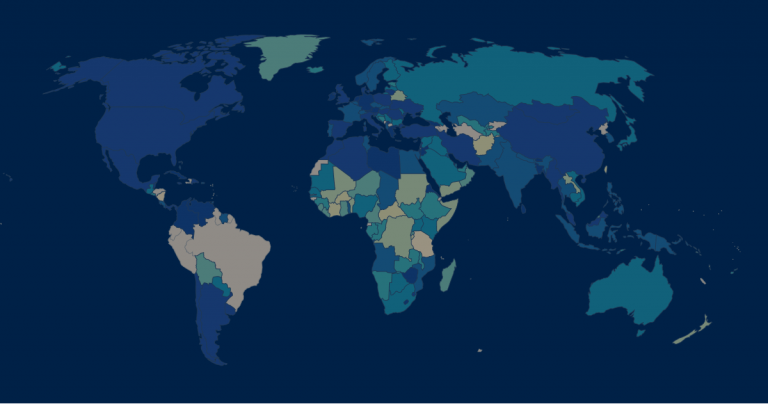
Three tips on how to interact with this map
- By clicking on any country on the map you see the change over time in this country.
- By moving the time slider (below the map) you can see how the global situation has changed over time.
- You can focus on a particular world region using the dropdown menu to the top-right of the map.
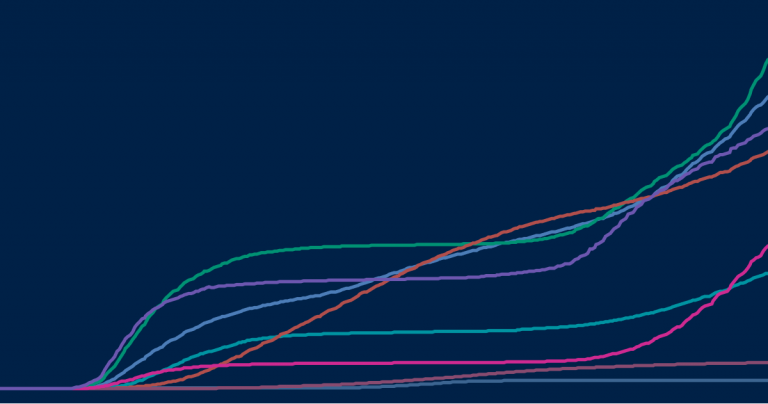
Myanmar: What is the cumulative number of confirmed cases?
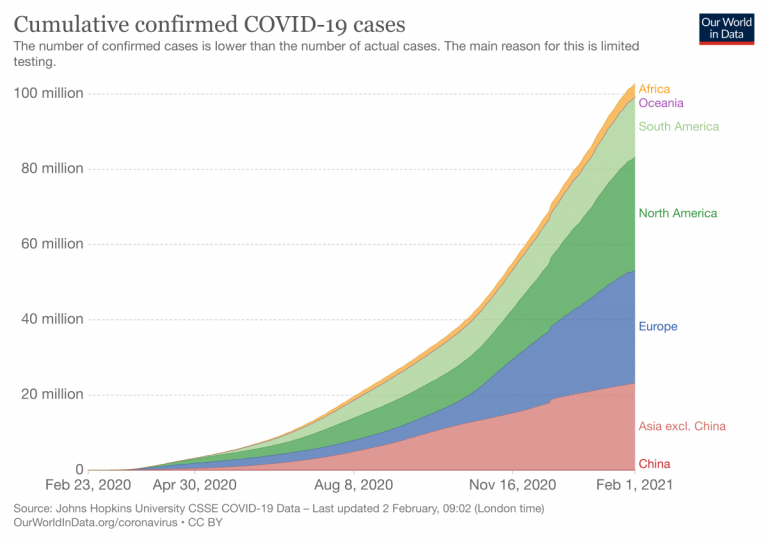
Which world regions have the most cumulative confirmed cases?
How do the number of tests compare to the number of confirmed COVID-19 cases?
The previous charts looked at the number of confirmed cases per day – this chart shows the cumulative number of confirmed cases since the beginning of the COVID-19 pandemic.
In all our charts you can download the data
We want everyone to build on top of our work and therefore we always make all our data available for download. Click on the ‘Download’-tab at the bottom of the chart to download the shown data for all countries in a .csv file.
Myanmar: Cumulative confirmed cases: how do they compare to other countries?
This chart shows the cumulative number of confirmed cases per million people.
Myanmar: Biweekly cases : where are confirmed cases increasing or falling?
Why is it useful to look at biweekly changes in confirmed cases.
For all global data sources on the pandemic, daily data does not necessarily refer to the number of new confirmed cases on that day – but to the cases reported on that day.
Since reporting can vary significantly from day to day – irrespectively of any actual variation of cases – it is helpful to look at a longer time span that is less affected by the daily variation in reporting. This provides a clearer picture of where the pandemic is accelerating, staying the same, or reducing.
The first map here provides figures on the number of confirmed cases in the last two weeks. To enable comparisons across countries it is expressed per million people of the population.
And the second map shows the percentage change (growth rate) over this period: blue are all those countries in which the case count in the last two weeks was lower than in the two weeks before. In red countries the case count has increased.
What is the weekly number of confirmed cases?
What is the weekly change (growth rate) in confirmed cases?
Myanmar: Global cases in comparison: how are cases changing across the world?
In our page on COVID-19 cases , we provide charts and maps on how the number and change in cases compare across the world.
Confirmed deaths
- What is the daily number of confirmed deaths?
- Daily confirmed deaths: how do they compare to other countries?
- What is the cumulative number of confirmed deaths?
- Cumulative confirmed deaths: how do they compare to other countries?
- Biweekly deaths : where are confirmed deaths increasing or falling?
- Global deaths in comparison: how are deaths changing across the world?
Myanmar: What is the daily number of confirmed deaths?
Which world regions have the most daily confirmed deaths?
This chart shows t he number of confirmed COVID-19 deaths per day .
Three points on confirmed death figures to keep in mind
All three points are true for all currently available international data sources on COVID-19 deaths:
- The actual death toll from COVID-19 is likely to be higher than the number of confirmed deaths – this is due to limited testing and challenges in the attribution of the cause of death. The difference between confirmed deaths and actual deaths varies by country.
- How COVID-19 deaths are determined and recorded may differ between countries.
- The death figures on a given date do not necessarily show the number of new deaths on that day, but the deaths reported on that day. Since reporting can vary significantly from day to day – irrespectively of any actual variation of deaths – it is helpful to view the seven-day rolling average of the daily figures as we do in the chart here.
→ We provide more detail on these three points in our page on Deaths from COVID-19 .
Myanmar: Daily confirmed deaths: how do they compare to other countries?
This chart shows the daily confirmed deaths per million people of a country’s population.
Why adjust for the size of the population?
Differences in the population size between countries are often large, and the COVID-19 death count in more populous countries tends to be higher . Because of this it can be insightful to know how the number of confirmed deaths in a country compares to the number of people who live there, especially when comparing across countries.
For instance, if 1,000 people died in Iceland, out of a population of about 340,000, that would have a far bigger impact than the same number dying in the United States, with its population of 331 million. 1 This difference in impact is clear when comparing deaths per million people of each country’s population – in this example it would be roughly 3 deaths/million people in the US compared to a staggering 2,941 deaths/million people in Iceland.
Myanmar: What is the cumulative number of confirmed deaths?
Which world regions have the most cumulative confirmed deaths?
The previous charts looked at the number of confirmed deaths per day – this chart shows the cumulative number of confirmed deaths since the beginning of the COVID-19 pandemic.
Myanmar: Cumulative confirmed deaths: how do they compare to other countries?
This chart shows the cumulative number of confirmed deaths per million people.
Myanmar: Biweekly deaths : where are confirmed deaths increasing or falling?
Why is it useful to look at biweekly changes in deaths.
For all global data sources on the pandemic, daily data does not necessarily refer to deaths on that day – but to the deaths reported on that day.
Since reporting can vary significantly from day to day – irrespectively of any actual variation of deaths – it is helpful to look at a longer time span that is less affected by the daily variation in reporting. This provides a clearer picture of where the pandemic is accelerating, staying the same, or reducing.
The first map here provides figures on the number of confirmed deaths in the last two weeks. To enable comparisons across countries it is expressed per million people of the population.
And the second map shows the percentage change (growth rate) over this period: blue are all those countries in which the death count in the last two weeks was lower than in the two weeks before. In red countries the death count has increased.
What is the weekly number of confirmed deaths?
What is the weekly change (growth rate) in confirmed deaths?
Myanmar: Global deaths in comparison: how are deaths changing across the world?
In our page on COVID-19 deaths , we provide charts and maps on how the number and change in deaths compare across the world.
- How many COVID-19 vaccine doses are administered daily ?
- How many COVID-19 vaccine doses have been administered in total ?
- What share of the population has received at least one dose of the COVID-19 vaccine?
- What share of the population has completed the initial vaccination protocol ?
- Global vaccinations in comparison: which countries are vaccinating most rapidly?
Myanmar: How many COVID-19 vaccine doses are administered daily ?
How many vaccine doses are administered each day (not population adjusted)?
This chart shows the daily number of COVID-19 vaccine doses administered per 100 people in a given population . This is shown as the rolling seven-day average. Note that this is counted as a single dose, and may not equal the total number of people vaccinated, depending on the specific dose regime (e.g., people receive multiple doses).
Myanmar: How many COVID-19 vaccine doses have been administered in total ?
How many vaccine doses have been administered in total (not population adjusted)?
This chart shows the total number of COVID-19 vaccine doses administered per 100 people within a given population. Note that this is counted as a single dose, and may not equal the total number of people vaccinated, depending on the specific dose regime as several available COVID vaccines require multiple doses.
Myanmar: What share of the population has received at least one dose of the COVID-19 vaccine?
How many people have received at least one vaccine dose?
This chart shows the share of the total population that has received at least one dose of the COVID-19 vaccine. This may not equal the share with a complete initial protocol if the vaccine requires two doses. If a person receives the first dose of a 2-dose vaccine, this metric goes up by 1. If they receive the second dose, the metric stays the same.
Myanmar: What share of the population has completed the initial vaccination protocol ?
How many people have completed the initial vaccination protocol?
The following chart shows the share of the total population that has completed the initial vaccination protocol. If a person receives the first dose of a 2-dose vaccine, this metric stays the same. If they receive the second dose, the metric goes up by 1.
This data is only available for countries which report the breakdown of doses administered by first and second doses.
Myanmar: Global vaccinations in comparison: which countries are vaccinating most rapidly?
In our page on COVID-19 vaccinations, we provide maps and charts on how the number of people vaccinated compares across the world.
Testing for COVID-19
- The positive rate
- The scale of testing compared to the scale of the outbreak
- How many tests are performed each day ?
- Global testing in comparison: how is testing changing across the world?
Myanmar: The positive rate
Here we show the share of reported tests returning a positive result – known as the positive rate.
The positive rate can be a good metric for how adequately countries are testing because it can indicate the level of testing relative to the size of the outbreak. To be able to properly monitor and control the spread of the virus, countries with more widespread outbreaks need to do more testing.
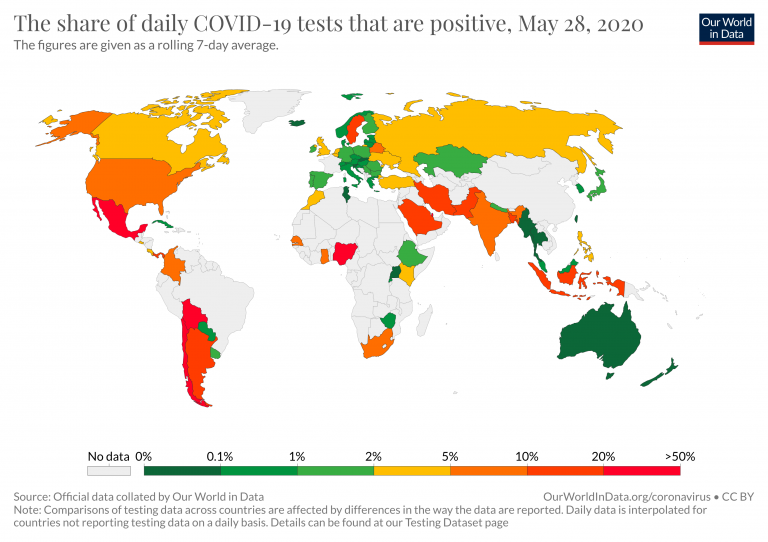
It can also be helpful to think of the positive rate the other way around:
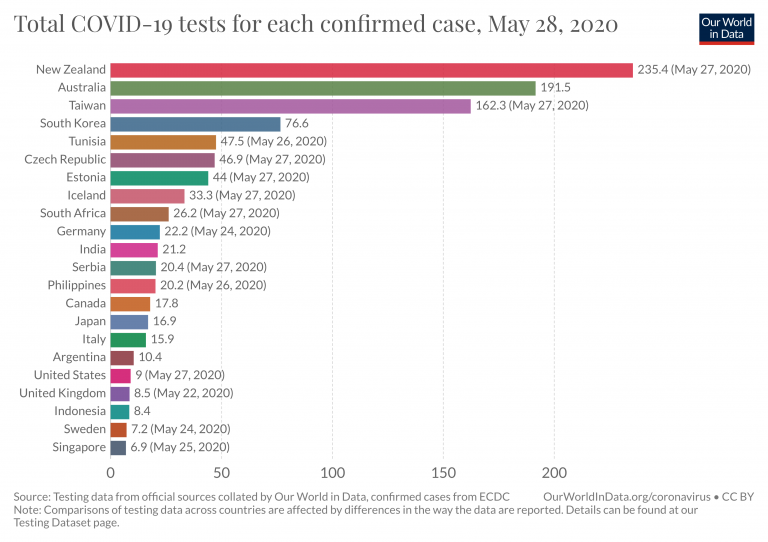
How many tests have countries done for each confirmed case in total across the outbreak?
Myanmar: The scale of testing compared to the scale of the outbreak
How do daily tests and daily new confirmed cases compare when not adjusted for population ?
This scatter chart provides another way of seeing the extent of testing relative to the scale of the outbreak in different countries.
The chart shows the daily number of tests (vertical axis) against the daily number of new confirmed cases (horizontal axis), both per million people.
Myanmar: How many tests are performed each day ?
This chart shows the number of daily tests per thousand people. Because the number of tests is often volatile from day to day, we show the figures as a seven-day rolling average.
What is counted as a test?
The number of tests does not refer to the same thing in each country – one difference is that some countries report the number of people tested, while others report the number of tests (which can be higher if the same person is tested more than once). And other countries report their testing data in a way that leaves it unclear what the test count refers to exactly.
We indicate the differences in the chart and explain them in detail in our accompanying source descriptions .
Myanmar: Global testing in comparison: how is testing changing across the world?
In our page on COVID-19 testing , we provide charts and maps on how the number and change in tests compare across the world.
Case fatality rate
- What does the data on deaths and cases tell us about the mortality risk of COVID-19?
- The case fatality rate
- Learn in more detail about the mortality risk of COVID-19
Myanmar: What does the data on deaths and cases tell us about the mortality risk of COVID-19?
To understand the risks and respond appropriately we would also want to know the mortality risk of COVID-19 – the likelihood that someone who is infected with the disease will die from it.
We look into this question in more detail on our page about the mortality risk of COVID-19 , where we explain that this requires us to know – or estimate – the number of total cases and the final number of deaths for a given infected population.
Because these are not known , we discuss what the current data on confirmed deaths and cases can and can not tell us about the risk of death. This chart shows both those metrics.
Myanmar: The case fatality rate
Related chart:.
How do the cumulative number of confirmed deaths and cases compare?
The case fatality rate is simply the ratio of the two metrics shown in the chart above.
The case fatality rate is the number of confirmed deaths divided by the number of confirmed cases.
This chart here plots the CFR calculated in just that way.
During an outbreak – and especially when the total number of cases is not known – one has to be very careful in interpreting the CFR . We wrote a detailed explainer on what can and can not be said based on current CFR figures.
Myanmar: Learn in more detail about the mortality risk of COVID-19
Learn what we know about the mortality risk of COVID-19 and explore the data used to calculate it.
Government Responses
- Government Stringency Index
To understand how governments have responded to the pandemic, we rely on data from the Oxford Coronavirus Government Response Tracker (OxCGRT), which is published and managed by researchers at the Blavatnik School of Government at the University of Oxford.
This tracker collects publicly available information on 17 indicators of government responses, spanning containment and closure policies (such as school closures and restrictions in movement); economic policies; and health system policies (such as testing regimes).
How have countries responded to the pandemic?
Travel bans, stay-at-home restrictions, school closures – how have countries responded to the pandemic? Explore the data on all policy measures.
Myanmar: Government Stringency Index
The chart here shows how governmental response has changed over time. It shows the Government Stringency Index – a composite measure of the strictness of policy responses.
The index on any given day is calculated as the mean score of nine policy measures, each taking a value between 0 and 100. See the authors’ full description of how this index is calculated.
A higher score indicates a stricter government response (i.e. 100 = strictest response).
The OxCGRT project calculates this index using nine specific measures, including:
- school and workplace closures;
- restrictions on public gatherings;
- transport restrictions;
- and stay-at-home requirements.
You can see all of these separately on our page on policy responses . There you can also compare these responses in countries across the world.
Our World in Data is free and accessible for everyone.
Help us do this work by making a donation.
- Get involved
Seven simple steps to protect yourself and others from COVID-19
March 10, 2020.
Coronavirus disease (COVID-19) is the infectious disease caused by the most recently discovered coronavirus. Most people who become infected experience mild illness and recover, but it can be more severe for others, particularly older people and those with underlying medical conditions. Here are some simple steps you can take to protect your health and the health of other people.
Everyone can follow these recommendations, but they are particularly important if you are in an area where people are known to have COVID-19.
1. Wash your hands frequently
Regularly and thoroughly clean your hands with an alcohol-based hand rub or wash them with soap and water.
Why? We frequently use our hands to touch objects and surfaces that may be contaminated. Without realizing it, we then touch our faces, transferring viruses to our eyes, nose and mouth where they can infect us. Washing your hands with soap and water or using alcohol-based hand rub kills viruses that may be on your hands — including the virus that causes COVID-19.
2. Avoid touching your eyes, nose and mouth
We often touch our faces without noticing it. Be aware of this, and avoid touching your eyes, nose and mouth.
Why? Hands touch many surfaces and can pick up viruses. Once contaminated, hands can transfer the virus to your eyes, nose or mouth and can then enter your body and make you sick.
3. Cover your cough
Make sure that you, and the people around you, follow good respiratory hygiene. This means covering your mouth and nose with the bend of your elbow or with a tissue when you cough or sneeze. Dispose of the used tissue immediately into a closed bin and wash your hands.
Why? When someone coughs or sneezes they spray small liquid droplets from their nose or mouth which may contain virus. By covering your cough or sneeze you avoid spreading viruses and other germs to other people. By using the bend of your elbow or a tissue and not your hands to cover your cough or sneeze, you avoid transferring contaminated droplets to your hands. This prevents you from contaminating a person or a surface through touching them with your hands.

4. Avoid crowded places and close contact with anyone that has fever or cough
Avoid crowded places, especially if you are over 60 or have an underlying health condition such as high blood pressure, diabetes, heart and lung diseases or cancer. Maintain at least 1 metre of distance between yourself and anyone who has a fever or cough.
Why? COVID-19 spreads mainly by respiratory droplets that come out of the mouth or nose when a person who has the disease coughs. By avoiding crowded places, you keep yourself distant (at least 1 metre) from people who may be infected with COVID-19 or any other respiratory disease.
5. Stay at home if you feel unwell
Stay at home if you feel unwell, even with a slight fever and cough.
Why? By staying home and not going to work or other places, you will recover faster and will avoid transmitting diseases to other people.
6. If you have a fever, cough and difficulty breathing, seek medical care early — but call first
If you have a fever, cough and difficulty breathing, seek medical care early — if you can, call your hospital or health centre first so that they can tell you where you should go.
Why? This will help to make sure you get the right advice, are directed to the right health facility, and will prevent you from infecting others.
7. Get information from trusted sources
Stay informed about the latest information from about about COVID-19 from trusted sources. Make sure your information comes from reliable sources — your local or national public health agency, the World Health Organization (WHO) website, or your local health professional. Everyone should know the symptoms — for most people, it starts with a fever and a dry cough.
Why? Local and national authorities will have the most up-to-date information on whether COVID-19 is spreading in your area. They are best placed to advise on what people in your area should be doing to protect themselves. For more information from WHO, visit:
- WHO COVID-19 main page
- Advice for the public
- When and how to use masks
- COVID-19 myth-busters
- Q&A videos
- Travel advice
- Training and e-learning
Related Content
Publications
Mired in uncertainty: the trend of high frequency indicators in myanmar (december 2021-january 2022).
The Myanmar military's 1 February coup d’état exacerbated the already challenging economic situation in the country that had been driven by the COVID-19 pandemic....
Impact of the twin crises on human welfare in Myanmar
The report details the impact of the COVID-19 pandemic and February 2021 coup d’état in Myanmar. It builds on the report released by UNDP in early April this year...
COVID-19, coup d'état and poverty: compounding negative shocks and their impact on human development in Myanmar
This report presents UNDP research findings and analysis of data collected prior and during the COVID-19 pandemic in Myanmar on the socioeconomic impacts of both ...
Household Vulnerability Survey 2020
The COVID 19 pandemic is having significant and, probably, lasting consequences on the Myanmar economy. The effects of the pandemic have resonated well beyond the...

The Critical Value of PPE in Myanmar’s Mon State
To cope with the situation, Mon State has been working with the UN Development Programme, to try to control the spread of the virus through an Awareness Raising a...

- Myanmar’s Crisis & the World
- Ethnic Issues
- War Against the Junta
- Junta Cronies
- Conflicts In Numbers
- Junta Watch
- Investigation
- Myanmar-China Watch
- Guest Column

Myanmar’s Third Wave of COVID-19 Spreads to Almost 90% of Townships

A charity organizing funerals for COVID-19 patients at a cemetery in Kale, Sagaing Region. / CJ
Nearly 90 percent of the country has been affected by Myanmar’s third wave of coronavirus infections, with 296 of 330 townships nationwide reporting COVID-19 cases since May.
Addressing a meeting on COVID-19 prevention and control measures on Friday, coup leader Senior General Min Aung Hlaing admitted that “the current infection [outbreak] in Myanmar is serious” and was spreading faster than the first and second waves of the coronavirus epidemic in Myanmar.
“If necessary, restrictions should be tightened so the people strictly follow the orders related to COVID-19,” he said.
The junta’s Health Ministry said in mid-June that three mutant strains of the coronavirus have been detected in Myanmar, including the Delta strain, which was first detected in India.
On Friday, Myanmar reported 64 fatalities—the highest death toll since the military coup in February—and 4,320 new COVID-19 cases, after testing 15,747 swab samples, according to the ministry.
As of Friday, Myanmar had reported a total of 184,375 COVID-19 cases with 3,685 deaths.
On Thursday, regime-controlled television announced that all schools, including private and monastic schools, will be closed until July 23. The regime reopened schools on June 1 after they had been shuttered for more than a year under the ousted civilian government due to the pandemic.
Snr-Gen Min Aung Hlaing added that the regime had an agreement with China to buy 5 million doses of vaccines, while Russia was planning to deliver the first batch of 2 million doses purchased from the country.
Additionally, the junta leader said the regime would “arrange for Myanmar Pharmaceutical Industry to manufacture the vaccines” with support from Russia, which has promised to provide technical help on vaccine production.
Myanmar reported its first cases of COVID-19 in March last year, and a second wave followed in August. In both outbreaks, public participation was huge, with healthcare professionals and volunteers at the forefront of measures to prevent and contain the disease.
After Myanmar experienced a second wave of COVID-19 in August last year, the National League for Democracy government began to implement a nationwide vaccination program on Jan. 27, days before the military coup on Feb. 1. Health-care staff and volunteer medical workers were the first to receive shots of the AstraZeneca vaccine donated by India.
In defiance of military rule, thousands of healthcare professionals are taking part in the Civil Disobedience Movement (CDM) and refusing to work for the military regime.
COVID-19 testing declined from between about 16,000 and 18,000 swab tests a day in January under the ousted NLD civilian government to fewer than 2,000 per day between February and early June. Swab testing increased again in late June, with over 8,000 tests conducted.
The military regime has imposed stay-at-home orders in 45 townships: three in Sagaing Region; five in Chin State; seven in Bago Region; eight in Mandalay Region; three in Shan State; three in Ayeyarwady Region; two in Naypyitaw; Gangaw in Magwe Region; three in Mon State; and 10 in Yangon Region.
You may also like these stories:
Related Posts

Restoring Ancient City as Regime Crumbles; Building a Mutiny; and More

Myanmar Junta to Double Electricity Rates

China Discusses Military Training with Myanmar Junta
Nearly 1,200 coronavirus-positive myanmar workers in thailand’s tak need help, groups say.
Myanmar Border Town Locked Down by KIA as New COVID-19 Infections Emerge
The Coup China Saw Coming in Myanmar—and Failed to Stop
Silence on Coup Makes Strategic Sense for Myanmar’s Wa
The irrawaddy, similar picks:.

Exodus: Tens of Thousands Flee as Myanmar Junta Troops Face Last Stand in Kokang
Myanmar National Democratic Alliance Army troops are opening roads and pathways through forests for people to flee Kokang’s capital as...

Enter the Dragon, Exit the Junta: Myanmar’s Brotherhood Alliance makes Chinese New Year Vow
Ethnic armed grouping says it will continue Operation 1027 offensive until goal of ousting the junta is achieved.

Drone Attack at Myanmar-China Border Gate Causes Over $14m in Losses
Jin San Jiao is latest northern Shan State trade hub in crosshairs of ethnic Brotherhood Alliance.

Arakan Army Captures Myanmar Junta Brigade General in Chin State Rout: Report
Rakhine-based armed group has reportedly detained the chief of 19th Military Operations Command after seizing his base in Paletwa Township.

Brotherhood Alliance Marching Towards Capital of Myanmar’s Kokang Region
Chinese embassy urges citizens to flee Laukkai Town as ethnic armies prepare to drive Myanmar junta troops from Kokang’s capital.

Myanmar Junta Arrests Thai Condo Buyers, Realtors as Currency Crashes
Monday’s arrests follow reports that Myanmar has become one of Thailand’s most lucrative markets for selling condos since the 2021...

Myanmar Suffering From Severe Shortage of Medical Oxygen as COVID-19 Cases Spike
Recommended

Wang Yi Embraced a Pariah in Myanmar: It Will Only Backfire

Increasingly Frantic Recruitment Methods Point to Myanmar Junta’s Frailty
French aircraft are abetting war crimes in myanmar: report, tnla reportedly captures two more junta bases in shan state’s nawnghkio, myanmar junta forces push back in kachin’s bhamo after losing battalion hq, get the irrawaddy’s latest news, analyses and opinion pieces on myanmar in your inbox..
Subscribe here for daily updates.
- Myanmar’s Crisis & the World
- Junta Crony
- Election 2020
- Elections in History
- Myanmar Diary
- Women & Gender
- Places in History
- On This Day
- From the Archive
- Myanmar & COVID-19
- Intelligence
- Fashion & Design
- Photo Essay
About The Irrawaddy
Founded in 1993 by a group of Myanmar journalists living in exile in Thailand, The Irrawaddy is a leading source of reliable news, information, and analysis on Burma/Myanmar and the Southeast Asian region. From its inception, The Irrawaddy has been an independent news media group, unaffiliated with any political party, organization or government. We believe that media must be free and independent and we strive to preserve press freedom.
- Code of Ethics
- Privacy Policy
© 2023 Irrawaddy Publishing Group. All Rights Reserved
Welcome Back!
Login to your account below
Remember Me
Retrieve your password
Please enter your username or email address to reset your password.
- Business Roundup
Content Search
Un country team in myanmar steps up covid-19 response efforts.
- UNCT Myanmar
Attachments

(Yangon, 19 July 2021) – The UN Country Team in Myanmar is stepping up its response efforts following an alarming spike in the reported number of COVID-19 cases in the country.
Even with very limited testing and people experiencing difficulties in accessing testing, 5497 new cases were reported on July 17 bringing the test positivity rate to 39.12 per cent compared to 22.34 per cent two weeks earlier. In addition, several COVID-19 variants have been detected, including the highly transmissible Delta variant.
Stay-at-home orders in over 70 townships across Myanmar have been imposed, as well as nationwide public holidays declared from 17-25 July in efforts to curb virus spread. Access to hospital beds and oxygen is limited due to insufficient supplies and manpower.
The UN Country Team is working to address the oxygen shortage through the procurement of oxygen concentrators and other necessary equipment through multiple channels.
The immediate scaling up of the provision of critical health services and COVID-19 vaccination efforts, remains an urgent priority.
WHO, UNICEF and partners are redoubling their efforts to accelerate COVID-19 vaccination availability through multiple channels, including through the COVAX facility. Myanmar is expected to receive enough COVID-19 vaccines through the COVAX facility during 2021 to cover 20 per cent of the population which is required to be distributed according to WHO guidelines for prioritizing vaccination. The first batch of these vaccines is expected in the current round of allocations.
Efforts are underway to re-operationalize testing and COVID-19 treatment centres are being established with available resources and capacities.
Currently, COVID-19 testing is occurring in states and regions at the rate of 12,000-15,000 tests per day. With testing at limited levels, however, many cases are expected to be unreported.
The current outbreak of COVID-19 is expected to have devastating consequences for the health of the population and for the economy. A renewed ‘whole of society’ approach is needed now more than ever, allowing all health professionals to work in safety, and both public and private providers enabled to contribute to the response.
Related Content
Myanmar – eu disaster response emergency fund for flood victims (dg echo) (echo daily flash of 28 august 2024), myanmar toolkit: observational gender review - adapted from the rapid gender assessment tool.
Myanmar + 1 more
Siete años después del desplazamiento forzoso en masa de los rohingya de Myanmar, los niños y niñas siguen sufriendo ataques mortales en el estado de Rakhine
Sept ans après le déplacement massif forcé des rohingya du myanmar, les attaques meurtrières visant les enfants se poursuivent dans l’état rakhine.
Pandemics Don’t Really End—They Echo
T he public health emergency related to the COVID-19 pandemic officially ended on May 11, 2023. It was a purely administrative step. Viruses do not answer to government decrees. Reported numbers were declining, but then started coming up again during the summer. By August, hospital admissions climbed to more than 10,000 a week. This was nowhere near the 150,000 weekly admissions recorded at the peak of the pandemic in January 2022.
The new variant is more contagious. It is not yet clear whether it is more lethal. Nor is it clear whether the recent rise is a mere uptick or foreshadows a more serious surge. More than 50,000 COVID-19 deaths have been reported in the U.S. in 2023. Somehow, this has come to be seen as almost normal.
Even while health authorities are keeping their eyes on new “variables of concern,” for much of the public COVID has been cancelled. The news media have largely moved on to other calamities. The pandemic is over. Is it?
History shows that pandemics have ragged endings. Some return again and again. The Justinian Plague that swept through the Roman Empire in the 6 th century returned in waves over the next 200 years. The Black Death that killed half the population of Europe between 1347 and 1351 came back more than 40 times over the next 400 years.
Read More: Will the New Vaccine Work Against the Latest Variant?
The effect of the COVID-19 pandemic will be felt long after the last rapid test comes back positive. Millions today are still suffering from “ long COVID ”—a range of medical conditions that can appear long after the initial infection. This concept can be applied to the whole of society.
Pandemics have always frayed the social fabric, disrupted economies, deepened social divides, and intensified prejudices, leaving behind psychological scars—all of which have lasting political repercussions.
Angered by the British crown’s attempt to restore the inequalities of the pre-pandemic feudal system, which had been weakened by the massive depopulation caused by the plague, English peasants marched on London and nearly brought down the king. Repeated waves of cholera in Europe during the 19 th century increased social tensions and contributed to growing class warfare. A sharp increase in labor strife followed the 1918 flu pandemic.
Today, society seems similarly on edge and quick to violence, an observation that was also made about medieval society following the plague. The U.S. homicide rate in 2020 and 2021 increased by nearly 40 percent. It appears to have come down in some cities, but violent crime remains above pre-pandemic levels. Mass shootings have hit an all-time high, while random unprovoked aggression has increased in public spaces. The pandemic is not entirely to blame, but it has likely been a contributing factor.
Many Americans quit their jobs after the pandemic. Others are refusing to give up working from home . The so-called great resignation appears to be ending, but the labor militancy that featured in post-pandemic societies continues.
While the COVID-19 pandemic comes nowhere near the depopulation effects of the plague, it emptied the sidewalks in many major American cities. Office buildings have fewer workers. Restaurants have lost business. It is not uncommon to see rows of boarded up retail shops. COVID does not get all the blame. The rise in crime in many city centers keeps many away. Urban geography may be permanently altered.
As it often did after past pandemics, pessimism pervades the post-pandemic moodscape. Its explanation lies beyond the pathogens. A Biblical host of natural and man-made disasters—pestilence, war, famine, floods, drought, fire, contribute to a sense of foreboding.
The 1918 flu pandemic left a legacy of distrust in institutions and each other, which was passed down to children and grandchildren, COVID may have similar long-term effects.
Americans are a cantankerous lot, increasingly suspicious of malevolent motives behind anything government does. Partisan news outlets look for conflict and stoke outrage. In past pandemics, conspiracy theories flourished, often blaming immigrants and Jews. So too, some COVID conspiracy theories suggest that the virus was designed to kill Whites or Blacks, while sparing Asians and Jews. Nothing changes.
Some believe the government created the pandemic hoax or deliberately misled the public about the seriousness of the situation. They argue that needless lockdown orders and business shutdown ruined the economy; providing financial relief to businesses and families opened the way for massive corruption and left the country with insupportable debt; mask and vaccine mandates were assaults on personal liberty for the benefit of big Pharma profits. Some still claim that the vaccines themselves rivaled the virus in their lethality. Defiance has been elevated to patriotism.
Owing to response measures, improved medications, life-saving procedures for treating critically-ill patients, and the rapid availability of a vaccine, the outbreak did not replicate the death tolls of previous pandemics.
Although it sounds perverse, saving lives ended up contributing to the controversy. Simply put: The pandemic was not deadly enough . The 2 nd century Antonine Plague killed a quarter of the Roman Empire’s population. The 6 th century Justinian plague killed half the population of Europe. According to some historians, the first wave of the plague in the 14 th century again wiped out half of Europe’s inhabitants.
COVID has killed more than a million Americans, roughly a third of one percent—or about the same percentage of the population killed in World War II. As a percentage of the total population, the 1918 flu was twice as deadly.
The demographics of the death toll are important. The 1918 flu killed many younger people—those 25-40 years old accounted for 40% of the fatalities—while COVID killed mainly older Americans, as three-quarters of the dead were 65 or older. Those under 40 accounted for just 2.5% of the fatalities.
Some questioned why the country’s well-being should be jeopardized to save the elderly, many of whom already had other afflictions anyway. Expressed in the cruelest terms, nature was culling the herd. Indeed, some of the same groups that during earlier debates about national health care expressed outrage at the prospect of death panels “pulling the plug on grandma” suggested during the pandemic that the elderly would be willing to die to save the economy.
The COVID pandemic lacked visual impact. Except for those directly affected, COVID’s toll remained abstract. There was no modern equivalent of town criers calling “Bring out your dead” accompanied by carts making the rounds to collect corpses. Had COVID led to bodies piled in the streets, shared dread might have outweighed our differences. As it turned out, we had the science to address the pandemic. What we lacked was the social accord.
Discord continues in the political arena. The tradeoffs between preserving individual rights and protecting the public are legitimate areas to explore, but rather than looking for lessons to be learned, some politicians appear determined to settle scores. Pandemic disputes will almost certainly feature in the 2024 presidential election.
Any future outbreak of disease will likely again see cable news, the internet, and social media play major roles in shaping the information individuals choose in their decision making. This will inevitably make emergency control measures more difficult to impose. COVID’s biggest political casualty may be governability itself.
We are unable to join hands to remember the more than a million Americans that have succumbed to the virus—that are succumbing still. We cannot express a nation’s gratitude to the scientists, public health officials, and heroic frontline health workers, thousands of whom died saving lives during the pandemic. Stuck in the well-worn paths of previous pandemic prejudices and conspiracy theory re-runs, we cannot come together to mourn our losses and celebrate our survival.
There will be no collective thanksgiving, no elegies, no closure. As we have seen time and time again throughout human history, pandemics do not end—they echo.
More Must-Reads from TIME
- Breaking Down the 2024 Election Calendar
- How Nayib Bukele’s ‘Iron Fist’ Has Transformed El Salvador
- What if Ultra-Processed Foods Aren’t as Bad as You Think?
- How Ukraine Beat Russia in the Battle of the Black Sea
- Long COVID Looks Different in Kids
- How Project 2025 Would Jeopardize Americans’ Health
- What a $129 Frying Pan Says About America’s Eating Habits
- The 32 Most Anticipated Books of Fall 2024
Contact us at [email protected]
We combed through thousands of Labor Day deals — these are the absolute best
- Share this —

- Watch Full Episodes
- Read With Jenna
- Inspirational
- Relationships
- TODAY Table
- Newsletters
- Start TODAY
- Shop TODAY Awards
- Citi Concert Series
- Listen All Day
Follow today
More Brands
- On The Show
- TODAY Plaza
Nearly 1 million pediatric COVID-19 cases reported last week

Nearly 1 million cases of COVID-19 were reported among children in the United States last week, the American Academy of Pediatrics said Tuesday.
The pediatric case count ending the week of Jan. 13 — 981,488 — reflects a 69% increase from the previous week’s 580,247 cases.
The new case count is likely an underestimate of the true number of pediatric COVID-19 cases, the AAP said, because many kids are either tested at home with rapid tests that are never reported to health officials, or not tested at all because of the shortage of tests.
Despite the dramatic spike, the rise is due to the increased overall spread of the omicron variant, and does not suggest that the virus has changed somehow to make kids more susceptible , said Dr. Mark Kline, the physician-in-chief at Children’s Hospital New Orleans.
Omicron is simply contagious in a way that earlier variants were not. As of Tuesday, the variant accounted for 99.5% of all COVID-19 cases in the U.S., according the Centers for Disease Control and Prevention.
“That figure of a million is really eye-popping,” Kline said. “But I don’t think that omicron has a unique propensity for children. Kids are being affected like everybody else.”
Pediatric COVID-19 cases have accounted for 20% to 25% of all U.S. cases since November. Last week, children represented 21.4% of weekly reported cases, according to the AAP.
Less than one third of kids ages 5 to 11 have received at least one dose of a COVID-19 vaccine, and no vaccines are available to kids under age 5.
“They’re the only age group left that is 100 percent unvaccinated,” Kline said. “We know that a lot of these cases are occurring in very young children.”
This story first appeared on NBCNews.com .

I’m a Paralympian. We’re not your ‘inspiration’ — we’re elite athletes

IVF success rates by age: What to know

These foods can reduce pain from period cramps
Women's health.

People tell me I don’t ‘look disabled,’ but I’m a Paralympian — and I’m going for gold

Tom Brady's TB12 diet: The pros, the cons and a shopping list
Diet & fitness.

The 5 types of friendship we all need in our life
Mind & body.

What is cycle syncing? Everything to know, from foods to workouts to fertility

6 sneaky signs you have a protein deficiency, according to dietitians

Where is deadly mosquito virus EEE spreading in US? 5 states reporting cases
How to perform pigeon pose — the perfect stretch to do after sitting all day
- Open access
- Published: 26 August 2024
Paramedics’ experiences and observations: work-related emotions and well-being resources during the initial months of the COVID-19 pandemic—a qualitative study
- Henna Myrskykari 1 , 2 &
- Hilla Nordquist 3
BMC Emergency Medicine volume 24 , Article number: 152 ( 2024 ) Cite this article
91 Accesses
1 Altmetric
Metrics details
As first responders, paramedics are an extremely important part of the care chain. COVID-19 significantly impacted their working circumstances. We examined, according to the experiences and observations of paramedics, (1) what kinds of emotions the Emergency Medical Service (EMS) personnel experienced in their new working circumstances, and (2) what work-related factors became resources for the well-being of EMS personnel during the initial months of the COVID-19 pandemic.
This qualitative study utilized reflective essay material written by experienced, advanced-level Finnish paramedics ( n = 30). The essays used in this study were written during the fall of 2020 and reflected the period when Finland had declared a state of emergency (on 17.3.2020) and the Emergency Powers Act was implemented. The data was analyzed using an inductive thematic analysis.
The emotions experienced by the EMS personnel in their new working circumstances formed three themes: (1) New concerns arose that were constantly present; (2) Surviving without proper guidance; and (3) Rapidly approaching breaking point. Three themes were formed from work-related factors that were identified as resources for the well-being of the EMS personnel. These were: (1) A high level of organizational efficiency was achieved; (2) Adaptable EMS operations; and (3) Encouraging atmosphere.
Conclusions
Crisis management practices should be more attentive to personnel needs, ensuring that managerial and psychological support is readily available in crisis situations. Preparedness that ensures effective organizational adaptation also supports personnel well-being during sudden changes in working circumstances.
Peer Review reports
At the onset of the COVID-19 pandemic, healthcare personnel across the globe faced unprecedented challenges. As initial responders in emergency healthcare, paramedics were quickly placed at the front lines of the pandemic, dealing with a range of emergencies in unpredictable conditions [ 1 ]. The pandemic greatly changed the everyday nature of work [ 2 , 3 , 4 , 5 , 6 , 7 , 8 , 9 , 10 ]. Those working on the front line were suddenly forced to adjust to personal protective equipment (PPE) requirements [ 9 , 10 ] and rapidly changing instructions that caused significant adjustments to their job description [ 11 , 12 ]. For instance, it has been reported that during the initial stages of the COVID-19 pandemic, Emergency Medical Services (EMS) personnel, including paramedics working in prehospital emergency care, experienced a significant increase in stress [ 10 , 13 ] due to several reasons, such as the lack of protection and support, increased demands, lack of personnel, fear of exposure to COVID-19 during missions, concerns of spreading the virus to family members, and frustration over quickly changing work policies [ 11 , 14 , 15 ].
With the unprecedented challenges posed by the COVID-19 pandemic, some research has been directed toward identifying available resources that help in coping with such situations. For example, Sangal et al. [ 15 ] underscored the association between effective communication and reduced work stress and burnout, and emphasized the critical need for two-way communication, consistent messaging, and the strategic consolidation of information prior to its dissemination. In parallel, Dickson et al. [ 16 ] highlight the pivotal role of leadership strategies in fostering a healthful work environment. These strategies include being relationally engaging, visibly present, open, and caring for oneself and others, while embodying core values such as compassion, empathy, courage, and authenticity. Moreover, Awais et al. [ 14 ] identify essential measures to reduce mental distress and support EMS personnel’s overall well-being in pandemic conditions, such as by providing accessible mental health and peer support, ensuring a transparent information flow, and the implementation of clear, best-practice protocols and guidelines. As a lesson learned from COVID-19, Kihlström et al. (2022) add that crisis communication, flexible working conditions, compensation, and allowing for mistakes should be part of crisis management. They also emphasize the importance of psychological support for employees. [ 12 ]
Overall, the COVID-19 pandemic had a multifaceted impact on EMS personnel, highlighting the necessity for comprehensive support and resilience strategies to safeguard their well-being [ 11 , 17 , 18 ] alongside organizational functions [ 12 , 19 ]. For example, in Finland, it has been noted in the aftermath of COVID-19 that the availability and well-being of healthcare workers are key vulnerabilities of the resilience of the Finnish health system [ 12 ]. Effective preparedness planning and organizational resilience benefit from learning from past events and gaining a deeper understanding of observations across different organizational levels [ 12 , 19 , 20 ]. For these reasons, it is important to study how the personnel experienced the changing working circumstances and to recognize the resources, even unexpected ones, that supported their well-being during the initial phase of the COVID-19 pandemic [ 12 , 19 ].
The aim of this study was to examine the emotions experienced and the resources identified as supportive of work well-being during the initial months of the COVID-19 pandemic, from the perspective of the paramedics. Our research questions were: According to the experiences and observations of paramedics, (1) what kinds of emotions did the EMS personnel experience in the new working circumstances, and (2) what work-related factors became resources for the well-being of EMS personnel during the initial months of the COVID-19 pandemic? In this study, emotions are understood as complex responses involving psychological, physiological, and behavioral components, triggered by significant events or situations [ 21 ]. Resources are understood as physical, psychological, social, or organizational aspects of the work that help achieve work goals, reduce demands and associated costs [ 22 ].
Materials and methods
This qualitative study utilized reflective essay material written in the fall of 2020 by experienced, advanced-level paramedics who worked in the Finnish EMS during the early phase of the pandemic, when Finland had declared (March 17, 2020 onward) a state of emergency and implemented the Emergency Powers Act. This allowed for new rules and guidelines from the government to ensure the security of healthcare resources. Some work rules for healthcare personnel changed, and non-urgent services were limited.
Data collection procedures
This study is part of a broader, non-project-based research initiative investigating the work well-being of paramedics from various perspectives, and the data was collected for research purposes from this standpoint. The data collection for this study was conducted at the South-Eastern Finland University of Applied Sciences as part of the Current Issues in EMS Management course. The course participants were experienced, advanced-level Finnish paramedics who were students of the master’s degree program in Development and Management of Emergency Medical Services. A similar data collection method has been utilized in other qualitative studies [for example, 23 , 24 ].
The South-Eastern Finland University of Applied Sciences granted research permission for the data collection on August 20, 2020. The learning platform “Learn” (an adapted version of Moodle [ 25 ]) was used to gather the data. A research notice, privacy statement, and essay writing instructions were published on the platform on August 21, 2020. The paramedics were asked to write about their own experiences and observations regarding how the state of emergency impacted the work well-being of EMS personnel. They were instructed not to use references but only their own reflections. Three guiding questions were asked: “What kind of workloads did EMS personnel experience during the state of emergency?” “How has this workload differed from normal conditions?” and “What effects did this workload have on the well-being of the EMS personnel?”. The assignment did not refer solely to paramedics because the EMS field community may also include individuals with other titles (such as EMS field supervisors or firefighters performing prehospital emergency care); hence the term “EMS personnel” was used.
The essay was part of the mandatory course assignments, but submitting it for research purposes was voluntary. The paramedics were informed that their participation in the study would not affect their course evaluations. They had the freedom to decline, remove parts of, or withdraw the essay before analysis. None of the paramedics exercised these options. They were also informed that the last author removes any identifying details (such as names, places, and organizational descriptions that could reveal their workplace) before sharing the data with other, at the time unnamed, researchers. The last author (female) is a senior researcher specializing in EMS and work well-being topics, a principal lecturer of the respective course, and the head of the respective master’s program, and familiar to all of them through their studies. The paramedics were aware that the essays were graded by the last author on a pass/fail scale as part of the course assessment. However, comprehensive and well-reasoned reflections positively influenced the course grade. The evaluation was not part of this study. The paramedics had the opportunity to ask further questions about the study directly from the last author during and after the essay writing process and the course.
The paramedics wrote the essays between August 23, 2020, and November 30, 2020. Thirty-two paramedics (out of 39) returned their essays using the Learn platform during this timeframe. Thus, seven of the course completions were delayed, and the essays written later were no longer appropriate to include in the data due to the time elapsed since the initial months of the COVID-19 pandemic.
All 32 gave their informed consent for their essays to be included in the study. Essays written by paramedics who had not actively participated in EMS field work during exceptional circumstances were excluded from the material ( n = 2), because they wrote the essay from a different perspective, as they could not reflect on their own experiences and observations. Thus, a total of 30 essays were included in the study. The total material was 106 pages long and comprised 32,621 words in Finnish.
Study participants
Thirty advanced-level paramedics from Finland participated in this study. They all had a bachelor’s degree in emergency care or nursing with additional emergency care specialization. At the time of the study, they were pursuing their master’s studies. Thirteen of them were women, and seventeen were men. The average age of the participants was 33.5 years among women and 35.9 years among men. Women had an average of 8.7 years of work experience, and men had 8.8 years. All the participating paramedics worked in EMS in different areas across Finland (except northern Finland) during their studies and the early phase of the pandemic.
Data analysis
The data was analyzed with a thematic analysis following the process detailed by Braun & Clarke [ 26 ]. First, the two researchers thoroughly familiarized themselves with the data, and the refined aim and research questions of the study were formulated inductively in collaboration based on the content of the data (see [ 26 ], page 84). After this, a thorough coding process was mainly carried out by the first author (female), who holds a master’s degree, is an advanced-level paramedic who worked in EMS during the pandemic, and at the time of the analysis was pursuing her doctoral studies in a different subject area related to EMS. Generating the initial codes involved making notes of interesting features of anything that stood out or seemed relevant to the research question systematically across the entire dataset. During this process, the original paragraphs and sentences were copied from the essay material into a table in Microsoft Word, with each research question in separate documents and each paragraph or sentence in its own row. The content of these data extracts was then coded in the adjacent column, carefully preserving the original content but in a more concise form. Then, the content was analyzed, and codes were combined to identify themes. After that, the authors reviewed the themes together by moving back and forth between the original material, the data in the Word documents, and the potential themes. During this process, the authors worked closely and refined the themes, allowing them to be separated and combined into new themes. For example, emotions depicting frustration and a shift to indifference formed their own theme in this kind of process. Finally, the themes were defined into main, major and minor themes and named. In the results, the main themes form the core in response to the research questions and include the most descriptions from the data. The major themes are significant but not as central as the main themes. Major themes provide additional depth and context to the results. One minor theme was formed as the analysis process progressed, and it provided valuable insights and details that deepened the response to the research question. All the coded data was utilized in the formed themes. The full content of the themes is reported in the Results section.
The emotions experienced by the EMS personnel in their new working circumstances formed three themes: New concerns arose that were constantly present (main theme); Surviving without proper guidance (major theme); and Rapidly approaching breaking point (major theme) (Fig. 1 ). Work-related factors identified as resources for the well-being of EMS personnel formed three themes: A high level of organizational efficiency was achieved (main theme); Adaptable EMS operations (major theme); and Encouraging atmosphere (minor theme) (Fig. 2 ).
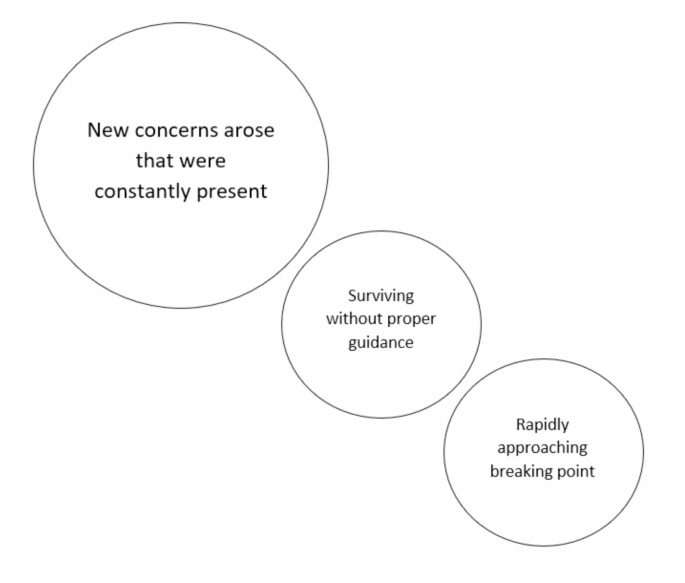
Emotions experienced by the EMS personnel in their new working circumstances
Main theme: New concerns arose that were constantly present
The main theme included several kinds of new concerns. In the beginning, the uncertainty about the virus raised concerns about work safety and the means to prevent the spread of the disease. The initial lack of training and routines led to uncertainty. In addition, the decrease in the number of EMS missions raised fears of units being reduced and unilateral decisions by the management to change the EMS personnel’s work responsibilities. The future was also a source of uncertainty in the early stages. For example, the transition to exceptional circumstances, concerns about management and the supervisors’ familiarity with national guidelines and lack of information related to sickness absence procedures, leave, personal career progression, and even the progress of vaccine development, all contributed to this feeling of uncertainty. The initial uncertainty was described as the most challenging phase, but the uncertainty was also described as long-lasting.
Being on the front line with an unknown, potentially dangerous, and easily transmissible virus caused daily concerns about the personnel’s own health, especially when some patients hid their symptoms. The thought of working without proper PPE was frightening. On the other hand, waiting for a patient’s test result was stressful, as it often resulted in many colleagues being quarantined. A constant concern for the health of loved ones and the fear of contracting the virus and unknowingly bringing it home or transmitting it to colleagues led the EMS personnel to change their behavior by limiting contact.
Being part of a high-risk group , I often wondered , in the case of coronavirus , who would protect me and other paramedics from human vanity and selfishness [of those refusing to follow the public health guidelines]? (Participant 25)
The EMS personnel felt a weight of responsibility to act correctly, especially from the perspective of keeping their skills up to date. The proper selection of PPE and aseptic procedures were significant sources of concern, as making mistakes was feared to lead to quarantine and increase their colleagues’ workloads. At the same time, concerns about the adequacy of PPE weighed on the personnel, and they felt pressure on this matter to avoid wastage of PPEs. The variability in the quality of PPE also caused concerns.
Concerns about acting correctly were also tied to ethical considerations and feelings of inadequacy when the personnel were unable to explain to patients why COVID-19 caused restrictions on healthcare services. The presence of students also provoked such ethical concerns. Recognizing patients’ symptoms correctly also felt distressing due to the immense responsibility. This concern was also closely tied to fear and even made some question their career choices. The EMS personnel were also worried about adequate treatment for the patients and sometimes felt that the patients were left alone at home to cope. A reduction in patient numbers in the early stages of the pandemic raised concerns about whether acutely ill individuals were seeking help. At the same time, the time taken to put on PPE stressed the personnel because it increased delays in providing care. In the early phase of the pandemic, the EMS personnel were stressed that patients were not protected from them.
I’m vexed in the workplace. I felt it was immediately necessary to protect patients from us paramedics as well. It wasn’t specifically called for , mostly it felt like everyone had a strong need to protect themselves. (Participant 30)
All these concerns caused a particularly heavy psychological burden on some personnel. They described feeling more fatigued and irritable than usual. They had to familiarize themselves with new guidelines even during their free time, which was exhausting. The situation felt unjust, and there was a looming fear of the entire healthcare system collapsing. COVID-19 was omnipresent. Even at the base station of the EMS services, movement was restricted and social distancing was mandated. Such segregation, even within the professional community, added to the strain and reduced opportunities for peer support. The EMS personnel felt isolated, and thoughts about changing professions increased.
It was inevitable that the segregation of the work community would affect the community spirit , and a less able work community has a significant impact on the individual level. (Participant 8)
Major theme: Surviving without proper guidance
At the onset of the pandemic, the job description of the EMS personnel underwent changes, and employers could suddenly relocate them to other work. There was not always adequate support for familiarizing oneself with the new roles, leading to a feeling of loss of control. The management was described as commanding and restricting the personnel’s actions. As opportunities to influence one’s work diminished, the sense of job satisfaction and motivation decreased.
Some felt that leadership was inadequate and neglectful, especially when the leaders switched to remote work. The management did not take the situation seriously enough, leaving the EMS personnel feeling abandoned. The lack of consistent leadership and failure to listen to the personnel caused dissatisfaction and reduced occupational endurance. In addition, the reduced contact with colleagues and close ones reduced the amount of peer support. The existing models for psychological support were found to be inadequate.
Particularly in the early stages, guidelines were seen as ambiguous and deficient, causing frustration, irritation, and fear. The guidelines also changed constantly, even daily, and it was felt that the information did not flow properly from the management to the personnel. Changes in protection recommendations also led to skepticism about the correctness of the national guidance, and the lack of consistent guidelines perplexed the personnel. Internalizing the guidelines was not supported adequately, but the necessity to grasp new information was described as immense and cognitively demanding.
At times , it felt like the work was a kind of survival in a jungle of changing instructions , one mission at a time. (Participant 11)
Major theme: Rapidly approaching breaking point
Risking one’s own health at work caused contentious feelings while concurrently feeling angry that management could work remotely. The arrogant behavior of people toward COVID-19 left them frustrated, while the EMS personnel had to limit their contacts and lost their annual leave. There were fears about forced labor.
Incomplete and constantly changing guidelines caused irritation and indifference, as the same tasks had to be performed with different levels of PPE within a short time. Some guidelines were difficult to comply with in practice, which was vexing.
Using a protective mask was described as distressing, especially on long and demanding missions. Communication and operation became more difficult. Some described frustration with cleaning PPE meant for single use.
Ensuring the proper implementation of a work pair’s aseptic and equipment maintenance was burdensome, and explaining and repeating guidelines was exhausting. A feeling of indifference was emphasized toward the end of a long shift.
After the initial stage, many began to slip with the PPE guidelines and found the instructions excessive. COVID-19 information transmitted by the emergency center lost its meaning, and instructions were left unheeded, as there was no energy to believe that the patient would have COVID-19, especially if only a few disease cases had been reported in their area.
It was disheartening to hear personnel being labeled as selfish for demanding higher pay during exceptional circumstances. This lack of recognition eroded professionalism and increased thoughts of changing professions.
However , being a doormat and a human toilet , as well as a lack of appreciation , undermines my professionalism and the prolonged situation has led me to seriously consider a different job , where values other than dedication and constant flexibility carry weight. I have heard similar thoughts from other colleagues. None of us do this for money. (Participant 9)
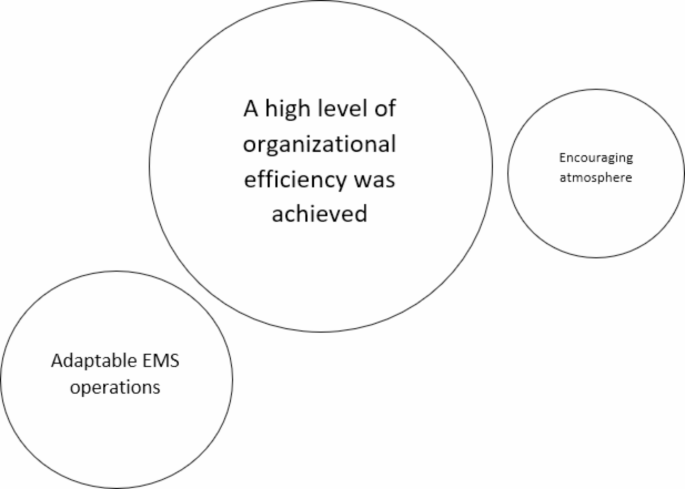
Work-related factors identified as resources for the well-being of EMS personnel
Main theme: A high level of organizational efficiency was achieved
The main theme held several different efficient functions. In the early stages of the pandemic, some felt that the information flow was active. Organizations informed the EMS personnel about the disease, its spread, and its impact on the workplace and emergency care activities.
Some felt that managers were easily accessible during the pandemic, at least remotely. Some managers worked long days to be able to support their personnel.
The response to hate and uncertainty was that one of the supervisors was always present in the morning and evening meetings. Supervisors worked long hours so as to be accessible via remote access. (Participant 26)
The organizations took effective steps to control infections. Quick access to COVID-19 tests, clear guidelines for taking sick leave, and permission to take sick leave with a low threshold were seen as positive things. The consideration of personnel belonging to risk groups by moving them to other work tasks was also perceived as positive. In addition, efforts were made to prevent the emergence of infection chains by isolating EMS personnel in their own social facilities.
Established guidelines, especially on the correct use of protective measures, made it easier to work. Some mentioned that the guidelines were available in ambulances and on phones, allowing the protection guidelines to be checked before going on a mission.
The employers took into account the need for psychological support in a diverse manner. Some organizations provided psychological support such as peer debriefing activities, talking therapy with mental health professionals, actively inquiring about their personnel’s feelings, and training them as support workers. The pandemic situation also caused organizations to create their own standard operating models to decrease mental load.
Fortunately , the problem has now been addressed actively , as a peer-to-peer defusing model was built up at our workplace during the crisis , and group defusing has started , the purpose of which is to lighten the work-related mental load. (Participant 3)
Major theme: Adaptable EMS operations
There were several different resources that clarified mission activities. The amount of protective and cleaning equipment was ramped up, and the treatment equipment was quickly updated to meet the demands brought about by the pandemic and to enable safety distances for the EMS personnel. In addition, various guidelines were amended to reduce exposure. For example, personnel on the dedicated COVID-19 ambulances were separated to work without physical contact with others, and field supervisors joined the EMS missions less often than before. Moreover, people at the scene were contacted by phone in advance to ensure that there would be no exposure risk, which also allowed other occupational safety risks to be identified. New practices resulted from the pandemic, such as cleaning communication equipment during shift changes and regularly using PPE with infected patients. All of these were seen as positive resources for efficient work.
At the end of each shift , all keys , telephones , etc., were cleaned and handed over to the next shift. This practice was not previously established in our area , but this will become a permanent practice in the future and is perceived by everyone in our work community as a positive thing. (Participant 10)
Some stated that access to PPE was sufficient, especially in areas where the number of COVID-19 infections was low. PPE was upgraded to make it easier to wear. Further, organizations acquired a variety of cleaning equipment to speed up the disinfection of ambulances.
Organizations hired more employees to enable leave and the operation of dedicated COVID-19 ambulances. The overall number of ambulances was also increased. Non-urgent missions were handled through enhanced phone services, reducing the unnecessary exposure of EMS personnel to COVID-19.
Five extra holiday substitutes were hired for EMS so that the employer could guarantee the success of agreed leave , even if the Emergency Preparedness Act had given them opportunities to cancel or postpone it. (Participant 12)
Minor theme: Encouraging atmosphere
Peer support from colleagues, a positive, comfortable, pleasant work environment, and open discussion, as well as smooth cooperation with other healthcare employees were felt to be resources for work well-being by reducing the heavy workload experienced. Due to the pandemic, the appreciation of healthcare was felt to increase slightly, which was identified as a resource.
One factor affecting resilience in the healthcare sector is certainly that in exceptional circumstances , visibility and appreciation have somewhat increased. (Participant 23)
This study examined, according to the experiences and observations of paramedics, (1) what kinds of emotions the Emergency Medical Service (EMS) personnel experienced in their new working circumstances, and (2) what work-related factors became resources for the well-being of EMS personnel during the initial months of the COVID-19 pandemic. Each research question was answered with three themes.
Previous studies have shown that the pandemic increased the workload of paramedics, prompting changes in their operating models and the function of EMS to align with new pandemic-related requirements [ 9 , 27 ]. Initially, the paramedics in the current study described facing unclear and deficient guidelines and feeling obligated to follow instructions without adequate support to internalize them. Constantly changing instructions were linked to negative emotions in various ways. Moreover, the overwhelming flood of information was heavily connected to this, although the information flow was also perceived as a resource, especially when it was timely and well-structured. The study by Sangal et al. [ 15 ] has raised similar observations and points out the importance of paying special attention to the personnel working in the frontline, as in EMS, who might be more heavily impacted by too much information and anxiety about it. They also discovered that three factors are crucial for addressing the challenges of information overload and anxiety: consolidating information before distributing it, maintaining consistent communication, and ensuring communication is two-way. McAlearney et al. [ 11 ] found that first responders, including EMS personnel, reported frustration regarding COVID-19 information because of inconsistencies between sources, misinformation on social media, and the impact of politics. A Finnish study also recognized that health systems were not sufficiently prepared for the flood of information in the current media environment [ 12 ]. Based on these previous results and our findings, it can be concluded that proper implementation of crisis communication should be an integral part of organizations’ preparedness in the future, ensuring that communication effectively supports employee actions in real-life situations. Secondly, this topic highlights the need for precise guidelines and their implementation. With better preparedness, similar chaos could be avoided in the future [ 17 ].
Many other factors also caused changes in work. The EMS mission profile changed [ 3 , 4 , 5 , 6 ], where paramedics in this study saw concerns. To prevent infection risk, the number of pre-arrival calls increased [ 7 ], the duration of EMS missions increased [ 8 , 9 ], and the continuous use of PPE and enhanced hygiene standards imposed additional burdens [ 9 , 10 ]. In Finland, there was no preparedness for the levels of PPE usage required in the early stages of the pandemic [ 12 ]. In this study, paramedics described that working with potentially inadequate PPE caused fear and frustration, which was increased by a lack of training, causing them to feel a great deal of responsibility for acting aseptically and caring for patients correctly. Conversely, providing adequate PPE, information and training has been found to increase the willingness to work [ 28 ] and the sense of safety in working in a pandemic situation [ 29 ], meaning that the role of precise training, operating instructions and leadership in the use of PPE is emphasized [ 30 ].
The paramedics in this study described many additional new concerns in their work, affecting their lives comprehensively. It has been similarly described that the pandemic adversely affected the overall well-being of healthcare personnel [ 31 ]. The restrictions implemented also impacted their leisure time [ 32 ], and the virus caused concerns for their own and their families’ health [ 11 , 28 ]. In line with this, the pandemic increased stress, burnout [ 10 , 33 ], and anxiety among EMS personnel and other healthcare personnel working on the frontline [ 11 , 14 , 34 , 35 ]. These kinds of results underscore the need for adequate guidance and support, a lack of which paramedics reported experiencing in the current study.
Personnel play a crucial role in the efficient operation of an organization and comprise the main identified resource in this study. Previous studies and summaries have highlighted that EMS personnel did not receive sufficient support during the COVID-19 pandemic [ 11 , 14 , 17 , 18 ]. Research has also brought to light elements of adequate support related to the pandemic, such as a review by Dickson et al. [ 16 ] that presents six tentative theories for healthful leadership, all of which are intertwined with genuine encounter, preparedness, and information use. In this current study, the results showed numerous factors related to these contexts that were identified as resources, specifically underlined by elements of caring, effective operational change, knowledge-based actions, and present leadership, similarly described in a study by Eaton-Williams & Williams [ 18 ]. Moreover, the paramedics in our study highlighted the importance of encouragement and identified peer support from colleagues as a resource, which is in line with studies in the UK and Finland [ 12 , 23 , 37 ].
In the early stages of the pandemic, it was noted that the EMS personnel lacked adequate training to manage their mental health, and there was a significant shortage of psychosocial support measures [ 14 ], although easy access to support would have been significant [ 18 ]. In the current study, some paramedics felt that mental health support was inadequate and delayed, while others observed an increase in mental health support during the pandemic, seeing it as an incentive for organizations to develop standard operating models for mental support, for example. This awakening was identified as a resource. This is consistent, as providing psychological support to personnel has been highlighted as a core aspect of crisis management in a Finnish study assessing health system resilience related to COVID-19 [ 12 ]. In a comprehensive recommendation commentary, Isakov et al. [ 17 ] suggest developing a national strategy to improve resilience by addressing the mental health consequences of COVID-19 and other occupational stressors for EMS personnel. This concept, applicable beyond the US, supports the view that EMS organizations are becoming increasingly aware of the need to prepare for and invest in this area.
A fundamental factor likely underlying all the described emotions was that changes in the job descriptions of the EMS personnel due to the pandemic were significant and, in part, mandated from above. In this study, paramedics described feelings of concern and frustration related to these many changes and uncertainties. According to Zamoum and Gorpe (2018), efficient crisis management emphasizes the importance of respecting emotions, recognizing rights, and making appropriate decisions. Restoring trust is a significant challenge in a crisis situation, one that cannot be resolved without complete transparency and open communication [ 38 ]. This perspective is crucial to consider in planning for future preparedness. Overall, the perspective of employee rights and obligations in exceptional circumstances has been relatively under-researched, but in Australia, grounding research on this perspective has been conducted with paramedics using various approaches [ 39 , 40 , 41 ]. The researchers conclude that there is a lack of clarity about the concept of professional obligation, specifically regarding its boundaries, and the issue urgently needs to be addressed by developing clear guidelines that outline the obligation to respond, both in normal day-to-day operations and during exceptional circumstances [ 39 ].
Complex adaptive systems (CAS) theory recognizes that in a resilient organization, different levels adapt to changing environments [ 19 , 20 ]. Barasa et al. (2018) note that planned resilience and adaptive resilience are both important [ 19 ]. Kihlström et al. (2022) note that the health system’s resilience was strengthened by a certain expectation of crisis, and they also recognized further study needs on how effectively management is responding to weak signals [ 12 ]. This could be directly related to how personnel can prepare for future changes. The results of this study revealed many negative emotions related to sudden changes, but at the same time, effective organizational adaptation was identified as a resource for the well-being of EMS personnel. Dissecting different elements of system adaptation in a crisis has been recognized as a highly necessary area for further research [ 20 ]. Kihlström et al. (2022) emphasize the importance of ensuring a healthy workforce across the entire health system. These frameworks suggest numerous potential areas for future research, which would also enhance effective preparedness [ 12 ].
Limitations of the study
In this study, we utilized essay material written in the fall of 2020, in which experienced paramedics reflected on the early stages of the COVID-19 pandemic from a work-oriented perspective. The essays were approached inductively, meaning that they were not directly written to answer our research questions, but the aim and the research questions were shaped based on the content [ 26 ]. The essays included extensive descriptions that aligned well with the aim of this study. However, it is important to remember when interpreting the results that asking specifically about this topic, for instance, in an interview, might have yielded different descriptions. It can be assessed that the study achieved a tentative descriptive level, as the detailed examination of complex phenomena such as emotions and resources would require various methods and observations.
Although the essays were mostly profound, well-thought-out, and clearly written, their credibility [ 42 ] may be affected by the fact that several months had passed between the time the essays were written and the events described. Memories may have altered, potentially influencing the content of the writings. Diary-like material from the very onset of the pandemic might have yielded more precise data, and such a data collection method could be considered in future research on exceptional circumstances.
The credibility [ 42 ] could also have been enhanced if the paramedics who wrote the essays had commented on the results and provided additional perspectives on the material and analysis through a multi-phase data collection process. This was not deemed feasible in this study, mainly because there was a 2.5-year gap between data collection and the start of the analysis. However, this also strengthened the overall trustworthiness of the study, as it allowed the first author, who had worked in prehospital emergency care during the initial phase of the pandemic, to maintain a distance from the subject, and enabled a comparison of our own findings with previously published research that investigated the same period in different contexts. The comparison was made when writing the discussion, with the analysis itself being inductive and following the thematic analysis process described by Braun & Clarke [ 26 ].
When evaluating credibility [ 42 ], it should also be noted that the participants who wrote the essays, i.e., the data for the study, were experienced paramedics but also students and one of the researchers was their principal lecturer. This could potentially limit credibility if the students, for some reason, did not want to produce truthful content for their lecturer to read. However, this risk can be considered small because the essays’ topics did not concern the students’ academic progress, the essays’ content was quite consistent, and the results aligned with other studies. As a strength, it can be considered that the students shared their experiences without holding back, as the thoughts were not for workplace use, and they could trust the data privacy statement.
To enhance transferability [ 42 ], the context of the study was described in detail, highlighting the conditions prevailing in Finnish prehospital emergency care during the early stages of the pandemic. Moreover, including a diverse range of perspectives from paramedics working in different regions of Finland (except Northern Finland) contributes to the transferability of the study, indicating that the results may be applicable and relevant to a wider context beyond a single specific region.
Dependability [ 42 ] was reinforced by the close involvement of two researchers from different backgrounds in the analysis of the material, but a limitation is that no separate analyses were conducted. However, the original data was repeatedly revisited during the analysis, which strengthened the dependability. Moreover, the first author kept detailed notes throughout the analysis process, and the last author supervised the progress while also contributing to the analysis and reporting. The research process is also reported in detail.
This study highlighted numerous, mainly negative emotions experienced by EMS personnel during the initial months of the COVID-19 pandemic due to new working circumstances. At the same time, several work-related factors were identified as resources for their well-being. The findings suggest that crisis management practices should be more attentive to personnel needs, ensuring that personnel have the necessary support, both managerial and psychological, readily available in crisis situations. Effective organizational adaptation in a crisis situation also supports personnel well-being, emphasizing the importance of effective preparedness. Future research should particularly focus on considering personnel well-being as part of organizational adaptation during exceptional circumstances and utilize these findings to enhance preparedness.
Data availability
The datasets generated and analyzed during the current study are not publicly available due to the inclusion of sensitive information and the extent of the informed consent provided by the participants.
Abbreviations
Complex Adaptive Systems (theory)
Coronavirus Disease 2019
Emergency Medical Services
Personal Protective Equipment
United Kingdom
Drennan IR, Blanchard IE, Buick JE. Opportunity for change: is it time to redefine the role of paramedics in healthcare? CJEM. 2021;23(2):139–40. https://doi.org/10.1007/s43678-021-00105-y
Boechler L, Cameron C, Smith JC, Ford-Jones P, Suthers P. Impactful approaches to Leadership on the Front lines of the COVID-19 pandemic: lived experiences of Canadian paramedics. Healthc Q. 2021;24(3):42–7. https://doi.org/10.12927/hcq.2021.26620 .
Article PubMed Google Scholar
Lerner EB, Newgard CD, Mann NC. Effect of the Coronavirus Disease 2019 (COVID-19) pandemic on the U.S. Emergency Medical Services System: a preliminary Report. Acad Emerg Med. 2020;27(8):693–9. https://doi.org/10.1111/acem.14051 .
Article PubMed PubMed Central Google Scholar
O’Connor AW, Hannah HA, Burnor EA, Fukutaki KG, Peterson T, Ballard DW, et al. Emergency Medical Service Utilization and response following COVID-19 emergency and stay-at-home policies: an interrupted time-series analysis. Cureus. 2021;21(11). https://doi.org/10.7759/cureus.19794 .
Azbel M, Heinänen M, Lääperi M, Kuisma M. Effects of the COVID-19 pandemic on trauma-related emergency medical service calls: a retrospective cohort study. BMC Emerg Med. 2021;9(1):102. https://doi.org/10.1186/s12873-021-00495-3 .
Article CAS Google Scholar
Lane DJ, Blanchard IE, Buick JE, Shaw M, McRae AD. Changes in presentation, presenting severity and disposition among patients accessing emergency services during the first months of the COVID-19 pandemic in Calgary, Alberta: a descriptive study. CMAJ Open. 2021;9(2):592–601. https://doi.org/10.9778/cmajo.20200313 .
Article Google Scholar
Shukla V, Lau CSM, Towns M, Mayer J, Kalkbrenner K, Beuerlein S, et al. COVID-19 exposure among First Responders in Arizona. J Occup Environ Med. 2020;62(12):981–5. https://doi.org/10.1097/JOM.0000000000002027 .
Article CAS PubMed Google Scholar
Andrew E, Nehme Z, Stephenson M, Walker T, Smith K. The impact of the COVID-19 pandemic on demand for emergency ambulances in Victoria, Australia. Prehosp Emerg Care. 2021;16:1–7. https://doi.org/10.1080/10903127.2021.1944409 .
Eskol JR, Zegers FD, Wittrock D, Lassen AT, Mikkelsen S. Increased ambulance on-scene times but unaffected response times during the first wave of the COVID-19 pandemic in Southern Denmark. BMC Emerg Med. 2022;9(1):61. https://doi.org/10.1186/s12873-022-00623-7 .
Schumann H, Böckelmann I, Thielmann B. Relaxation and strain among emergency medical service personnel and emergency control center dispatchers during the first two waves of the SARS-CoV-2 pandemic. Med Pr. 2023;15(5):353–62. https://doi.org/10.13075/mp.5893.01401 .
McAlearney AS, Gaughan AA, MacEwan SR, Gregory ME, Rush LJ, Volney J, et al. Pandemic experience of first responders: fear, frustration, and stress. Int J Environ Res Public Health. 2022;13(8):4693. https://doi.org/10.3390/ijerph19084693 .
Kihlström L, Huhtakangas M, Karreinen S, Viita-Aho M, Keskimäki I, Tynkkynen LK. Local cooperation has been the cornerstone: facilitators and barriers to resilience in a decentralized health system during COVID-19 in Finland. J Health Organ Manag. 2022. https://doi.org/10.1108/JHOM-02-2022-0069 .
Hendrickson RC, Slevin RA, Hoerster KD, Chang BP, Sano E, McCall CA, et al. The impact of the COVID-19 pandemic on Mental Health, Occupational Functioning, and Professional Retention among Health Care workers and First Responders. J Gen Intern Med. 2022;37(2):397–408. https://doi.org/10.1007/s11606-021-07252-z .
Awais SB, Martins RS, Khan MS. Paramedics in pandemics: protecting the mental wellness of those behind enemy lines. Br J Psychiatry. 2021;218(2):75–6. https://doi.org/10.1192/bjp.2020.193 .
Sangal RB, Bray A, Reid E, Ulrich A, Liebhardt B, Venkatesh AK, et al. Leadership communication, stress, and burnout among frontline emergency department staff amid the COVID-19 pandemic: a mixed methods approach. Healthc (Amst). 2021;9(4):100577. https://doi.org/10.1016/j.hjdsi.2021.100577 .
Dickson CAW, Davies C, McCormack B, Westcott L, Merrell J, Mcilfatrick S, et al. UK nurses’ and midwives’ experiences of healthful leadership practices during the COVID-19 pandemic: a rapid realist review. J Nurs Manag. 2022;30(8):3942–57. https://doi.org/10.1111/jonm.13790 .
Isakov A, Carr M, Munjal KG, Kumar L, Gausche-Hill MEMS. Agenda 2050 meets the COVID-19 pandemic. Health Secur. 2022;20(S1):S97–106. https://doi.org/10.1089/hs.2021.0179 .
Eaton-Williams PJ, Williams J. See us as humans. Speak to us with respect. Listen to us. A qualitative study on UK ambulance staff requirements of leadership while working during the COVID-19 pandemic. BMJ Lead. 2023;7(2):102–7. https://doi.org/10.1136/leader-2022-000622 .
Barasa E, Mbau R, Gilson L. What is resilience and how can it be nurtured? A systematic review of empirical literature on Organizational Resilience. Int J Health Policy Manag. 2018;7(6):491–503. https://doi.org/10.15171/ijhpm.2018.06 .
Coetzee C, Van Niekerk D, Raju E. Disaster resilience and complex adaptive systems theory: finding common grounds for risk reduction. Disaster Prev Manage. 2016;25(2):196–211. https://doi.org/10.1108/DPM-07-2015-0153 .
American Psychological Association. Emotion. APA Dictionary of Psychology. https://dictionary.apa.org/emotion . Accessed on 26.6.2024.
Demerouti E, Bakker AB, Nachreiner F, Schaufeli WB. The job demands-resources model of burnout. J Appl Psychol. 2001;86(3):499–512.
Ericsson CR, Lindström V, Rudman A, Nordquist H. Paramedics’ perceptions of job demands and resources in Finnish emergency medical services: a qualitative study. BMC Health Serv Res. 2022;22(1):1469. https://doi.org/10.1186/s12913-022-08856-9 .
Rinkinen T, Kinnula M, Nordquist H. Technological development roles and needs in pre-hospital emergency care from the advanced level paramedics’ perspective. Int Emerg Nurs. 2024;73:101406. https://doi.org/10.1016/j.ienj.2024.101406 .
Moodle Pty Ltd. 2020. https://moodle.org/ . Accessed on date 17.6.2024.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3:2:77–101. https://doi.org/10.1191/1478088706qp063oa .
Prezant DJ, Lancet EA, Zeig-Owens R, Lai PH, Appel D, Webber MP, et al. System impacts of the COVID-19 pandemic on New York City’s emergency medical services. J Am Coll Emerg Physicians Open. 2020;9(6):1205–13. https://doi.org/10.1002/emp2.12301 .
Alwidyan MT, Oteir AO, Trainor J. Working during pandemic disasters: views and predictors of EMS providers. Disaster Med Public Health Prep. 2022;16(1):116–22. https://doi.org/10.1017/dmp.2020.131 .
Rebmann T, Charney RL, Loux TM, Turner JA, Abbyad YS, Silvestros M. Emergency Medical Services Personnel’s pandemic influenza training received and willingness to work during a future pandemic. Prehosp Emerg Care. 2020;24(5):601–9. https://doi.org/10.1080/10903127.2019.1701158 .
Article CAS PubMed PubMed Central Google Scholar
McCann-Pineo M, Li T, Barbara P, Levinsky B, Berkowitz J. Factors influencing Use of Personal Protective Equipment among Emergency Medical services Responders during the COVID-19 pandemic: a Retrospective Chart Review. West J Emerg Med. 2022;23(3):396–407. https://doi.org/10.5811/westjem.2022.2.55217 .
Vanhaecht K, Seys D, Bruyneel L, Cox B, Kaesemans G, Cloet M, et al. COVID-19 is having a destructive impact on health-care workers’ mental well-being. Int J Qual Health Care. 2021;20(1):mzaa158. https://doi.org/10.1093/intqhc/mzaa158 .
Zolnikov TR, Furio F. First responders and social distancing during the COVID-19 pandemic. J Hum Behav Soc Environ. 2021;31(1–4):244–53. https://doi.org/10.1080/10911359.2020.1811826 .
Spychała A, Piwowarska M, Piekut A. The COVID-19 pandemic as a stress factor in the work of a paramedic. Med Pr. 2023;8(1):9–17. https://doi.org/10.13075/mp.5893.01278 .
Roberts R, Wong A, Jenkins S, Neher A, Sutton C, O’Meara P, et al. Mental health and well-being impacts of COVID-19 on rural paramedics, police, community nurses and child protection workers. Aust J Rural Health. 2021;29(5):753–67. https://doi.org/10.1111/ajr.12804 .
Chang YT, Hu YJ. Burnout and Health issues among Prehospital Personnel in Taiwan Fire Departments during a Sudden Spike in Community COVID-19 cases: a cross-sectional study. Int J Environ Res Public Health. 2022;16(4):2257. https://doi.org/10.3390/ijerph19042257 .
Mausz J, Donnelly EA, Moll S, Harms S, McConnell M. Mental disorder symptoms and the relationship with resilience among paramedics in a single Canadian site. Int J Environ Res Public Health. 2022;17(8):4879. https://doi.org/10.3390/ijerph19084879 .
Phung VH, Sanderson K, Pritchard G, Bell F, Hird K, Wankhade P, et al. The experiences and perceptions of wellbeing provision among English ambulance services staff: a multi-method qualitative study. BMC Health Serv Res. 2022;15(1):1352. https://doi.org/10.1186/s12913-022-08729-1 .
Zamoum K, Gorpe TS. Crisis Management: a historical and conceptual Approach for a better understanding of today’s crises. Crisis Manage - Theory Pract InTech. 2018. https://doi.org/10.5772/intechopen.76198 .
Anderson C, Pooley JA, Mills B, Anderson E, Smith EC. Do paramedics have a Professional Obligation to work during a pandemic? A qualitative exploration of Community Member expectations. Disaster Med Public Health Prep. 2020;14(3):406–12. https://doi.org/10.1017/dmp.2020.212 .
Smith E, Burkle FM, Gebbie K, Ford D, Bensimon C. Acceptable limitations on Paramedic Duty to treat during disaster: a qualitative exploration. Prehosp Disaster Med. 2018;33(5):466–70. https://doi.org/10.1017/S1049023X18000857 .
Smith E, Burkle F, Gebbie K, Ford D, Bensimon C. A qualitative study of paramedic duty to treat during disaster response. Disaster Med Public Health Prep. 2019;13(2):191–6. https://doi.org/10.1017/dmp.2018.15 .
Cypress BS. Rigor or reliability and validity in qualitative research: perspectives, strategies, reconceptualization, and recommendations. Dimens Crit Care Nurs. 2017;36(4):253–63. https://doi.org/10.1097/DCC.0000000000000253 .
TENK. Guidelines for the responsible conduct of research and for handling allegations of misconduct in Finland [Internet]. Helsinki: Finnish National Board on Research Integrity TENK; 2023. https://tenk.fi/sites/default/files/2023-11/RI_Guidelines_2023.pdf . Accessed 13 Jan 2024.
TENK. Ethical review in human sciences [Internet]. Helsinki: Finnish National Board on Research Integrity TENK; 2020. https://tenk.fi/sites/default/files/2021-1/Ethical_review_in_human_sciences_2020.pdf . Accessed 13 Jan 2024.
Download references
Acknowledgements
We want to sincerely thank all the paramedics who participated in this study.
Open access funded by Helsinki University Library.
Open Access funding provided by University of Helsinki (including Helsinki University Central Hospital).
Author information
Authors and affiliations.
Faculty of Medicine, University of Helsinki, Helsinki, Finland
Henna Myrskykari
Emergency Medical Services, University of Turku and Turku University Hospital, Turku, Finland
Department of Healthcare and Emergency Care, South-Eastern Finland University of Applied Sciences, Kotka, Finland
Hilla Nordquist
You can also search for this author in PubMed Google Scholar
Contributions
Study design (HM, HN). Data collection (HN). Methodology (HN). Analysis (HM, HN). Writing (HM, HN). Review and editing (HM, HN). Supervision (HN). Both authors read and approved the final manuscript.
Corresponding author
Correspondence to Henna Myrskykari .
Ethics declarations
Ethics approval and consent to participate.
The study followed the good scientific practice defined by the Finnish National Board on Research Integrity TENK [ 43 ]. The study was conducted in accordance with the Helsinki Declaration and applicable national guidelines. Adhering to the Finnish National Board on Research Integrity (TENK) guidelines on ethical principles of research with human participants and ethical review in the human sciences in Finland, an ethical review statement from a human sciences ethics committee was not required for this type of study. The participants consisted of adult students engaged in regular employment. Their involvement in the research was grounded on informed consent. The study did not involve concerns regarding the participants’ physical integrity, nor were they subjected to exceptionally strong stimuli. The potential for causing mental harm was not beyond what is typically encountered in everyday life, and their participation did not pose any safety risks [ 44 ].
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Myrskykari, H., Nordquist, H. Paramedics’ experiences and observations: work-related emotions and well-being resources during the initial months of the COVID-19 pandemic—a qualitative study. BMC Emerg Med 24 , 152 (2024). https://doi.org/10.1186/s12873-024-01072-0
Download citation
Received : 25 April 2024
Accepted : 13 August 2024
Published : 26 August 2024
DOI : https://doi.org/10.1186/s12873-024-01072-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Emergency medical services
- Health personnel
- Qualitative research
BMC Emergency Medicine
ISSN: 1471-227X
- General enquiries: [email protected]

So long, and thanks for all the fish

Before we go any further, I should note that this is my last newsletter for CJR, as I am moving on from my job as the magazine’s chief digital writer. (In case the headline doesn’t make any sense, it comes from a Douglas Adams book , in which he describes how all the dolphins suddenly vanished from the Earth, leaving behind the message: “So long, and thanks for all the fish!”) My byline may show up in CJR again on a freelance basis, but this will be my last piece as a member of staff. As I reflected on the last seven years or so of writing about the intersection of media and technology, I started to think about what (if anything) has changed since my first CJR piece was published, in October 2017— an essay headlined “The 140-character president,” about Donald Trump’s obsession with what was then known as Twitter.
Obviously, some things have changed quite a bit. Trump is no longer president (although he is trying hard to regain that position), and Twitter—now known as X—is owned by Elon Musk, the billionaire who also owns Tesla and SpaceX. Much has been written ( by me and just about everyone else) about Musk’s problem-plagued acquisition of the platform, and the changes he has made to it; it is reportedly hemorrhaging money and scrambling for both users and revenue . None of this is particularly new—the old Twitter under cofounders Jack Dorsey and Ev Williams also seemed to be continually scrambling for money and users. The reasons have changed, however: Musk, who maintains that his guiding principle is to enable free speech, has enabled many of the worst kinds of speech, including white supremacy, racism, and misogyny. This has (not surprisingly) led to an exodus of both users and advertisers.
These days, one popular conspiracy theory is that Musk is a Russian stooge who is trying to help Trump get reelected, a theory based in part on rumors about Russian troops in Ukraine using Musk’s Starlink for internet access and whispers that Putin-adjacent sources helped fund the purchase of Twitter. (The evidence for this is circumstantial —at best.) Russia’s involvement in a variety of nefarious projects (or rumors thereof) has been a consistent theme since I started writing for CJR. An early taste of that came in November 2017, when I traveled to Washington and sat in on a series of congressional hearings looking into whether Meta (then known as Facebook), Google, and Twitter had allowed Russia and Russian-aligned agents to use their services as the foundation of a gigantic disinformation campaign. Did this happen? Yes, at least in a limited way. Did it affect the outcome of the 2016 election? Opinion remains divided, but some of the smartest people in the field say no, it likely did not .
A related topic that has resurfaced again and again is whether misinformation and disinformation (Russian or otherwise) is a scourge that should be eradicated— by law if necessary —because it changes people’s behavior, or whether it is just a lot of sound and fury that doesn’t change much of anything. Disinformation experts argue that these kinds of campaigns, including what some like to call “automated propaganda,” do have a deleterious effect, but research shows that even the worst disinformation rarely changes people’s minds in any significant way (although in some cases, it can help reinforce things people already believe that are wrong or untrue). And disinformation remains, to some extent, in the eye of the beholder . Not so long ago, users who suggested that COVID-19 came from a lab might have had their Facebook accounts suspended. Now there are plenty of scientists who believe that this is a valid theory about the disease.
The broader question of whether the internet and social media are a negative influence has also been a consistent theme of my time at CJR. Multiple scientific-sounding articles have argued that cellphone and social media use have caused widespread anxiety, depression, and mental health problems among users, particularly teenage girls . This is a plausible-sounding phenomenon, and yet the majority of the research that has been done to date shows no such correlation—and, in some cases, actually shows that smartphone and social media use is a net positive for teens . I think, in general, that we should be wary of theories that tie complex human relationships to a single cause, whether it’s Instagram use or Russian troll farms engaging in what Facebook likes to refer to as “coordinated inauthentic behavior.”
As for whether the internet and social media are good for anyone at all, that question, too, has been an undercurrent of my work for CJR—and even before that. I confess that when I started writing about the social Web at the Globe and Mail , a daily newspaper in Toronto, in 2004 or so, I was convinced that it had the potential to change the world for the better. (I even cofounded a conference called Mesh that tried to explore all the ways it might do so.) I helped the Globe and Mail set up a Twitter feed and a Facebook account and do live-blogging and open itself up to reader comments; I even started a wiki to crowdsource reader insights about politics. At Gigaom , I wrote about how Twitter and Facebook helped enable the Arab Spring in Egypt, among other phenomena. Networked information seemed to have so much potential.
Unfortunately, the next decade or so—including most of my time here—would provide plenty of evidence that social media, like the internet itself, enables all of the good things about people but also all of the bad things. There was Gamergate, which in many ways helped give birth to the alt-right and its obsession with using freedom of speech to harass and abuse people via social media; then there was the rise of QAnon and conspiracy theories about Hillary Clinton and a sex-abuse ring. Facebook inadvertently helped to enable what many international observers have described as a genocide in Myanmar . To some extent, social media gave birth to the human chaos engine known as Donald Trump, a man who embodies Steve Bannon’s motto that the best route to informational success is to “flood the zone with shit.” (Unfortunately, this tactic often works on journalists and media outlets that should know better.)
Was I too naive about the positive impact of social media, and too dismissive or unaware of its negative effects? Absolutely. (In my defense, so were Dorsey and Mark Zuckerberg .) And yet what can counter these kinds of negative effects but people using those platforms and tools and technologies for good instead of evil? Perhaps that’s part of the reason I haven’t vacated Twitter (or X) despite my misgivings about Musk; if we all abandon these platforms to the bad actors and bots, how does that help? (I should note that I am also there because I enjoy the memes.) Maybe flooding the zone with positive content can counteract the effects of those who are flooding the zone with the other stuff. I’ve also been encouraged by the rise of Threads, Meta’s Twitter clone , and its experiments with the networked “fediverse,” including open-source platforms such as Mastodon and BlueSky, although none of them have really replaced Twitter as of yet.
Another major theme of my time at CJR: Google and Facebook holding themselves out as the saviors of the media multiple times and in multiple ways, something I wrote about at length in a 2018 piece called “The Platform Patrons.” Several years later, the hundreds of millions of dollars that both platforms committed to journalistic efforts—much of which consisted of training in how to use their products, which in turn exacerbated media reliance on those products—has vanished or been spent, leaving many media outlets no further ahead. Meta, in particular, killed the media- and journalism-related projects it once ran (something that I warned about in another piece, “The Facebook Armageddon ”) and is now fighting attempts to make it pay for journalism in the US and Canada. The decision on the part of many news outlets and publishers to tie so much of their business to these platforms has truly been the worst kind of Faustian bargain.
All of the topics I’ve mentioned so far, from the challenges of free speech and antitrust to journalism funding and social media moderation, were the subject of some fascinating debates that I conducted for CJR through an online platform called Galley , which we took over in 2018 after we were approached by its creators, Josh Young and Tom McGeveran. Galley was designed to be a better version of Twitter, allowing users to designate certain followers as trusted and then set up a chat open only to these users. We wound up using it for roundtable discussions with experts from the fields of law, science, sociology, and politics—an approach that I used to describe as being like a podcast, but with more typing. Unfortunately, we stopped hosting those discussions for a variety of reasons (funding being one of them), but I still believe that they added real value to those kinds of debates .
I am often asked whether there is anything worth being optimistic about in journalism and media, given the carnage we see all around us in the industry. Whether I am still naive or not remains to be seen, but I am optimistic about small, digital-native publications run by individuals like Ben Thompson (whose newsletter, Stratechery , was the inspiration for the creation of Substack) and Casey Newton ( Platformer ), or groups of writers like the teams behind 404 Media , Flaming Hydra (and its predecessor, Brick House ), and Drop Site , founded recently by former staffers at The Intercept . Hopefully at least some of them will find funding mechanisms that allow them to prosper, instead of relying on venture capital—a phenomenon that has taken down more than one promising media venture, including BuzzFeed News , Mic , and Gigaom . And, while crypto is still mostly a den of iniquity, I continue to think that Civil—a crypto-powered journalism platform that launched in 2018 and flamed out not long afterward—had some good ideas that might have worked if not for the industry’s speculative excesses.
Despite the challenges the media faces—whether it’s social algorithms, declining ad revenue, or AI-driven fakes—I still believe that there has never been a better time to be a journalist. The journalism business may be tanking, but the practice itself has never been more robust. At what other time in history could someone have started writing and within a matter of weeks reached tens or even hundreds of thousands of readers—and be making a living solely from subscriptions? I.F. Stone would have sold his soul for something like that. I am no I.F. Stone by any means, but I would like to thank all of you for reading me over these seven years, and for helping me draw attention to some of the issues that matter. I hope we can stay in touch in other ways. Onward!
Other notable stories:
- Yesterday, authorities in France charged Pavel Durov—the founder of the messaging app Telegram , who was arrested on arrival in the country over the weekend—with complicity in crimes committed on the platform and refusal to cooperate with law enforcement. (We wrote about Durov’s arrest on Tuesday .) The charges seem sure to intensify a global debate about free speech and tech leaders’ liability for users’ conduct.
- Also yesterday, a jury in Nevada convicted Robert Telles, a former local official, of murdering Jeff German, a reporter at the Las Vegas Review-Journal who had written stories about Telles, and ruled that he should get a life sentence (with the possibility of parole in twenty years). In the Review-Journal ’s newsroom, staffers hugged and wiped away tears following the verdict; the paper’s Katelyn Newberg has all the details .
- Washingtonian ’s Andrew Beaujon reports that a judge with the National Labor Relations Board will hear a complaint related to the Washington Post ’s decision to fire Felicia Sonmez, a reporter, in 2022 , after she criticized a coworker’s sexist tweet and the paper’s uneven enforcement of its social media policies. Per Beaujon, the NLRB’s general counsel will ask that Sonmez be ordered reinstated or financially compensated.
- Russia published a(nother ) list of people who it says are now barred from entering the country; ninety-two names were included, twenty-three of whom work at either the Post , the New York Times , or the Wall Street Journal . Russia blamed “editorial staff and reporters of leading liberal-globalist publications” for disseminating “fakes” and providing propaganda “cover” for the US. (We wrote about press freedom in Russia on Tuesday .)
- And the Post ’s Laura Wagner profiled Ben Rothenberg , a leading tennis journalist who has grown disillusioned with covering the sport—not least since one of the top players in the world, Alexander Zverev, sued him for covering allegations of abuse by Zverev’s ex-girlfriend. Now Racquet , a tennis magazine that published one of Rothenberg’s stories about Zverev, has stopped paying his legal bills.
The voice of journalism, since 1961
- Privacy Policy
Support CJR
- Become a Member
Advertisement
Supported by
Critic’s Notebook
When Your Child Is an Animal
The charged cultural conversation about pets and children — see “Chimp Crazy,” “childless cat ladies” and more — reveals the hidden contradictions of family life.
- Share full article

By Amanda Hess
Amanda Hess is a critic at large who writes about internet and pop culture.
“Monkey love is totally different than the way that you have love for your child,” Tonia Haddix, an exotic animal broker, says at the beginning of “Chimp Crazy,” the documentary HBO series investigating the world of chimpanzee ownership. “If it’s your natural born child, it’s just natural because you actually gave birth to that kid. But when you adopt a monkey, the bond is much, much deeper.”
“Chimp Crazy” arrives in a summer of cultural and political obsession about the place of animals in our family lives. When JD Vance became the Republican vice-presidential nominee, his 2021 comment about “childless cat ladies” resurfaced, positioning them as adversaries of the traditional family. New York magazine published a special issue questioning the ethics of pet ownership, featuring a polarizing essay from an anonymous mother who neglected her cat once her human baby arrived. In the background of these stories, you can hear the echoes of an internet-wide argument that pits companion animals against human children, pet and tot forced into a psychic battle for adult recognition.
These dynamics feel supercharged since 2020, the year when American family life — that insular institution that is expected to provide for all human care needs — became positively airtight. The coronavirus pandemic exaggerated a wider trend toward domestic isolation : pet owners spending more time with their animals, parents more time with their children, everyone less time with one another — except perhaps online, where our domestic scenes collide in a theater of grievance and stress.
When a cat, a dog or certainly a chimp scampers through a family story, it knocks it off-kilter, revealing its hypocrisies and its harms. In “Chimp Crazy,” Haddix emerges as the avatar for all the contradictions of the domestic ideal of private home care: She loves her chimp “babies” with such obsession that she traps them (and herself) in a miserable diorama of family life.
Haddix, a 50-something woman who describes herself as the “Dolly Parton of Chimps,” believes that God chose her to be a caretaker. She was a registered nurse before she became a live-in volunteer at a ramshackle chimp breeding facility in Missouri, where she speaks of a male chimp named Tonka as if she is his mother. Haddix also has two human children; she just loves them less, and says so on television.
As she appoints herself the parent to an imprisoned wild animal, she asserts an idealized form of mothering — one she describes as selfless, unending and pure. “Chimp Crazy” is the story of just how ruinous this idea of love can be, for the woman and the ape.
We are having trouble retrieving the article content.
Please enable JavaScript in your browser settings.
Thank you for your patience while we verify access. If you are in Reader mode please exit and log into your Times account, or subscribe for all of The Times.
Thank you for your patience while we verify access.
Already a subscriber? Log in .
Want all of The Times? Subscribe .
More From Forbes
The lemokey x5 is the affordable mechanical keyboard for gamers and typists.
- Share to Facebook
- Share to Twitter
- Share to Linkedin
The wired Lemokey X5 mechanical keyboard has north-facing red LEDs and 14 different lighting modes.
Are you looking for an affordable mechanical keyboard for gaming and typing? Well, I think I’ve found a bit of a bargain in the shape of the new Lemokey X5. The X5 is a 96% layout keyboard with a full numeric keypad and a row of multimedia and function keys. Because it’s a wired keyboard using a detachable USB-C cable, the X5 has a polling rate of 1,000Hz which is fast enough for even the most competitive gamer.
Although the Lemokey X5 is a budget keyboard, it has some premium features that make it great value. Built around a gasket mount structure, the X5 has shine-through, double-shot keycaps, a PC plate and acoustic foam.
The X5’s double-shot keycaps are made from ABS which makes them more durable and wear-resistant. All the keycaps have shine-through letters that are illuminated by the north-facing LEDs.
The X5 keyboard from Lemokey has shine-through ABS keycaps.
The LED backlights are a vibrant red color and there is also a range of different lighting modes to choose from, depending on your mood. The backlights can be turned off easily and the illumination level can also be adjusted from the keyboard.
The shine-through keys make the X5 ideal for use in low light levels, while the gasket mount, PC plate and foam give the keyboard a superbly solid feel. And thanks to support for QMK firmware, the Lemokey X5 can be programmed using Keychron’s web-based Launcher app with any Chrome-based browser that supports HID.
Best High-Yield Savings Accounts Of 2024
Best 5% interest savings accounts of 2024.
Using Launcher, the user can remap the entire keyboard layout and individual keys can be loaded with macros and keyboard shortcuts to speed up workflow or for specific functions for gameplay. Changes made to the keyboard’s firmware are saved in the X5's onboard memory.
The Lemokey X5 can be ordered with Red or Brown switches.
The X5 is powered by an ARM MCU with 256K of flash memory to give developers more flexibility. Meanwhile, that 1,000Hz polling rate means the X5 has no noticeable latency, even in the most demanding of games.
To ensure a comfortable typing position, the Lemokey X5 has three levels of typing angle using flip-out legs on the underside of the keyboard. You can set the typing angle to 4.5, 7 and 9 degrees. The keyboard has curved OEM-profile keycaps which work together with the adjustable typing angle to provide good ergonomic wrist support.
The Lemokey X5 is available with a choice of Linear Red or Tactile Brown pre-lubed switches. The Red switches have an operating force of 45gf, a pre-travel of 2mm and a travel distance of 4mm. The Red switches are quiet so you won’t drive your colleagues crazy with too much tapping.
The Lemokey X5 is a 97% keyboard with a numeric keypad and a full row of multimedia and function ... [+] keys.
Red switches are a great choice for gaming and general office use. And if you don’t like the switches, you can change them as the Lemokey X5 has hot-swappable switches and there’s even a switch puller included in the box.
The layout of the Lemokey X5 is ideal for Windows users but it also works fine on Macs. There are no macOS modifier keys in the box so if that’s important for you, then maybe one of Keychron’s other models might suit you better.
The typing feel of the X5 is pretty good for the money. At the price, it’s not going to be super solid, but it feels nice to type and there’s anti-ghosting NKRO support so no matter how fast you type, the X5 won’t forget what keys you press or what order you press them in.
The G1 wireless mouse from Lemokey is the perfect partner for the X5 keyboard.
Finally, every good keyboard deserves a good mouse. Fortunately, Lemokey makes the G1 wireless mouse that’s a perfect partner for the X5. Offering wired, Bluetooth and RF connectivity, the G1 is a superbly light little mouse that’s perfect for gaming. It has a built-in rechargeable battery that seems to last forever. I’d like to see the X5 bundled with the Lemokey G1 mouse as a kit. They work so well together.
Verdict: The Lemokey X5 mechanical keyboard ticks a lot of boxes. It’s a wired-only keyboard with almost no latency. The layout is almost full-sized and includes a numeric keypad, making it ideal for spreadsheets. There is also a full row of multimedia/function keys for both Windows and macOS computers. The switches are Red Linear type with red north-facing LEDs and 14 different lighting modes. The keycaps are superbly robust and the shine-through feature makes the ABS keycaps perfect for use in low light levels. When paired with the Lemokey G1 mouse, the X5 keyboard makes for one of the most affordable mechanical keyboards for gamers and office dwellers.
Pricing & Availability: The Lemokey X5 mechanical keyboard is available now and costs $49.99 while the Lemokey G1 Wireless Mouse is available in black or white and sells for $69.99.
Tech Specs:
- Dimensions (W x L): 133.7 x 380.5mm.
- Front height: 27.4mm.
- Back height: 38.6mm.
- Feet height: 2.2mm.
- Typing angles: 4.5 / 7 / 9 degrees.
- Weight: 717g.
- Body material: ABS plastic.
- Plate material : Polycarbonate.
- Polling rate: 1,000Hz.
- Keycaps: OEM profile shine-through double-shot ABS.
- MCU: WB32F3G71RCT6 (256KB Flash).
- Switches: Keychron mechanical switch (Red or Brown).
- Backlight: North-facing red LED
- N-Key Rollover (NKRO): Yes.
- Mount style: Gasket mount.
- Stabs: Plate-mounted.
- Connectivity: USB Type-C.
- Cable: Type-A to Type-C.

- Editorial Standards
- Reprints & Permissions
Join The Conversation
One Community. Many Voices. Create a free account to share your thoughts.
Forbes Community Guidelines
Our community is about connecting people through open and thoughtful conversations. We want our readers to share their views and exchange ideas and facts in a safe space.
In order to do so, please follow the posting rules in our site's Terms of Service. We've summarized some of those key rules below. Simply put, keep it civil.
Your post will be rejected if we notice that it seems to contain:
- False or intentionally out-of-context or misleading information
- Insults, profanity, incoherent, obscene or inflammatory language or threats of any kind
- Attacks on the identity of other commenters or the article's author
- Content that otherwise violates our site's terms.
User accounts will be blocked if we notice or believe that users are engaged in:
- Continuous attempts to re-post comments that have been previously moderated/rejected
- Racist, sexist, homophobic or other discriminatory comments
- Attempts or tactics that put the site security at risk
- Actions that otherwise violate our site's terms.
So, how can you be a power user?
- Stay on topic and share your insights
- Feel free to be clear and thoughtful to get your point across
- ‘Like’ or ‘Dislike’ to show your point of view.
- Protect your community.
- Use the report tool to alert us when someone breaks the rules.
Thanks for reading our community guidelines. Please read the full list of posting rules found in our site's Terms of Service.

IMAGES
VIDEO
COMMENTS
Myanmar's response to the COVID-19 pandemic. During the first wave of the coronavirus pandemic, from late March to early August, Myanmar recorded just 360 cases and 6 deaths. Early in the crisis ...
And now, a surge in coronavirus cases fuelled by the highly infectious Delta variant has dealt the country a fresh blow. ... Myanmar has so far reported more than 280,000 cases and 8,200 deaths ...
Between March 2020 and December 2020, Myanmar faced two waves of COVID-19 infections - the first wave from March to April 2020, and the second wave from August to November 2020. The cumulative number of cases in 2020 was 125 042, with 2697 deaths (3). This case study examines PHC in Myanmar in the context of the COVID-19 pandemic between ...
COVID-19 in Myanmar: Spread, actions and opportunities for peace and stability. the Philippines (Open University), Los Baños, Laguna, PhilippinesSince the declaration of pandemic on March 11, 2020, COVID-19 has been spreading to almost every country across the world, leading to a risin. tally of more than 14 million cases, and half a million ...
Myanmar's Ministry of Health counts nearly 20,000-recorded deaths from COVID-19 up to the end of 2021 - the fourth highest mortality rate in south-east Asia. But this figure is misleading ...
Between March and mid-June 2020, Myanmar's Ministry of Health and Sports has confirmed over 300 positive COVID-19 cases. Despite the low-infection rate in the country, the ICRC remains concerned for tens of thousands of families affected by armed conflict and violence, including displaced people living in temporary shelters and IDP sites.
Over the past years, Myanmar made considerable progress in attaining and sustaining high immunization coverage through various strategies. WHO-UNICEF Immunization coverage estimates 2019 for BCG, DTP3/Penta3, and OPV3 are ≥90% and ... despite the COVID-19 pandemic (Source: DHIS2 2020 data collected 31 Jan 2021, the day before the military ...
cio-Economic Impact of COVID-19 in Myanmar Understanding the socio-economic impacts of COVID-19 across sectors, population groups, gender, and geographic areas is essential for designing effective policies and measures to mitigate t. e impact of the pandemic and recover better. To contribute to an increased evidence-base and inform policymaking ...
Health workers carrying a coffin with a Covid-19 victim out of a hospital in Falam, Myanmar, in June. Chinland Herald Daily News, via Agence France-Presse — Getty Images. Three days before she ...
COVID-19 test kits arrive at Yangon airport in Myanmar in June 2020. The World Food Programme ( WFP) warned on Friday that it is facing a 70 per cent funding shortfall in Myanmar, where millions face growing food insecurity. Amid the "triple impact of poverty, the current political unrest and economic crisis", coupled with the rapidly ...
The COVID-19 pandemic in Myanmar is part of the worldwide pandemic of coronavirus disease 2019 caused by severe acute respiratory syndrome coronavirus 2 ().The virus was confirmed to have reached Myanmar on 23 March 2020. [4] On 31 March 2020, the Committee for Coronavirus Disease 19 (COVID-19), headed by First Vice President Myint Swe and made up of members from the various union ministries ...
ationMyanmarCOVID-19 Results BriefingMyanmarDecember 15, 2022This document contains summary information on. he latest projections from the IHME model on COVID-19 in Myanmar. The model. 15, 2022, with data through December 12, 2022.Current situationDaily infections in the last week increased to 238,000 pe.
First, the junta stole Myanmar's elected leaders from the people. Now, doctors say, the generals have taken the oxygen that some citizens need to breathe. As the Delta variant of the coronavirus ...
Published 30 Jun 2020. Covid-19 has shaken up the development of the digital economy in Myanmar, with the pandemic leading to a rise in demand for home broadband in this traditionally mobile-first market. As various containment measures were imposed, companies located in the main business hubs scrambled to ensure that employees were able to ...
19 July 2021. (Yangon) - The UN Country Team in Myanmar is stepping up its response efforts following an alarming spike in the reported number of COVID-19 cases in the country. Even with very limited testing and people experiencing difficulties in accessing testing, 5497 new cases were reported on July 17 bringing the test positivity rate to 39 ...
YANGON, June 25, 2020 - The global COVID-19 pandemic is dealing a severe blow to Myanmar's economy.Economic growth in a baseline scenario is projected to drop from 6.8 percent in FY18/19 to just 0.5 percent in FY2019/20, according to the World Bank's Myanmar Economic Monitor, released today.. If the pandemic is protracted, the economy could contract by as much as 2.5 percent in FY2019/20 ...
The actual death toll from COVID-19 is likely to be higher than the number of confirmed deaths - this is due to limited testing and challenges in the attribution of the cause of death. The difference between confirmed deaths and actual deaths varies by country. How COVID-19 deaths are determined and recorded may differ between countries.
9k. VIEWS. While Myanmar has been experiencing massive political and economic turmoil since the February coup, a deadly third wave of COVID-19 has hit the country, bringing with it all four known coronavirus variants. Thousands of people are dying as a direct consequence of the military regime's incompetent and negligent handling of the ...
Coronavirus disease (COVID-19) is the infectious disease caused by the most recently discovered coronavirus. Most people who become infected experience mild illness and recover, but it can be more severe for others, particularly older people and those with underlying medical conditions. Here are some simple steps you can take to protect your health and the health of other people.
Here, The Irrawaddy looks back at the Myanmar government's preparations, responses and actions over nearly five months battling the global pandemic. May 25: The government announced that Myanmar households will not need to pay for the first 150 units of electricity they use until the end of May. May 23: Myanmar's COVID-19 cases surged to ...
15.2k. Nearly 90 percent of the country has been affected by Myanmar's third wave of coronavirus infections, with 296 of 330 townships nationwide reporting COVID-19 cases since May. Addressing a meeting on COVID-19 prevention and control measures on Friday, coup leader Senior General Min Aung Hlaing admitted that "the current infection ...
Download Report (PDF | 184.35 KB) (Yangon, 19 July 2021) - The UN Country Team in Myanmar is stepping up its response efforts following an alarming spike in the reported number of COVID-19 cases ...
T he public health emergency related to the COVID-19 pandemic officially ended on May 11, 2023. It was a purely administrative step. Viruses do not answer to government decrees. Reported numbers ...
Pediatric COVID-19 cases have accounted for 20% to 25% of all U.S. cases since November. Last week, children represented 21.4% of weekly reported cases, according to the AAP.
The essays used in this study were written during the fall of 2020 and reflected the period when Finland had declared a state of emergency (on 17.3.2020) and the Emergency Powers Act was implemented. ... COVID-19 significantly impacted their working circumstances. We examined, according to the experiences and observations of paramedics, (1 ...
Not so long ago, users who suggested that COVID-19 came from a lab might have had their Facebook accounts suspended. Now there are plenty of scientists who believe that this is a valid theory about the disease. The broader question of whether the internet and social media are a negative influence has also been a consistent theme of my time at CJR.
Who has access: Members of any paid plan. The translation feature allows you to translate text directly within Grammarly. This way, you can stay focused on your current work and minimize the need to switch to external translation tools.
The charged cultural conversation about pets and children — see "Chimp Crazy," "childless cat ladies" and more — reveals the hidden contradictions of family life.
revista educación superior y sociedad, 2023, vol. 35, no. 1 2 Norberto Fernández Lamarra, Universidad Nacional de Tres de Febrero, Argentina Débora Ramos Torres, Instituto Internacional de la Unesco para la Educación Superior en América Latina y el Caribe, Venezuela Cristian Perez Centeno, Universidad Nacional de Tres de Febrero, Argentina Marisa Álvarez, Universidad Nacional de Tres de ...
The Lemokey X5 is a 97% keyboard with a numeric keypad and a full row of multimedia and function ...[+] keys. Lemokey. Red switches are a great choice for gaming and general office use.