- Case Report
- Open access
- Published: 22 November 2023

Severe-Enduring Anorexia Nervosa (SE-AN): a case series
- Federica Marcolini 1 ,
- Alessandro Ravaglia 1 ,
- Silvia Tempia Valenta 1 ,
- Giovanna Bosco 2 ,
- Giorgia Marconi 3 ,
- Federica Sanna 1 ,
- Giulia Zilli 1 ,
- Enrico Magrini 1 ,
- Flavia Picone 1 ,
- Diana De Ronchi 1 &
- Anna Rita Atti 1
Journal of Eating Disorders volume 11 , Article number: 208 ( 2023 ) Cite this article
2300 Accesses
5 Citations
4 Altmetric
Metrics details
Anorexia Nervosa (AN) poses significant therapeutic challenges, especially in cases meeting the criteria for Severe and Enduring Anorexia Nervosa (SE-AN). This subset of AN is associated with severe medical complications, frequent use of services, and the highest mortality rate among psychiatric disorders.
Case presentation
In the present case series, 14 patients were selected from those currently or previously taken care of at the Eating Disorders Outpatients Unit of the Maggiore Hospital in Bologna between January 2012 and May 2023. This case series focuses on the effects of the disease, the treatment compliance, and the description of those variables that could help understand the great complexity of the disorder.
This case series highlights the relevant issue of resistance to treatment, as well as medical and psychological complications that mark the life course of SE-AN patients. The chronicity of these disorders is determined by the overlapping of the disorder's ego-syntonic nature, the health system's difficulty in recognizing the problem in its early stages, and the presence of occupational and social impairment.
Introduction
Anorexia Nervosa (AN) constitutes a complex eating disorder (ED) characterized by low caloric intake, fear of gaining weight, dysfunctional behavior impeding weight gain, and misperceptions about one’s own body shape and weight [ 1 ]. The intricate nature of AN can lead to severe difficulties in the treatment, and patients may not necessarily benefit from conventional approaches. Most AN patients reach partial or complete remission only after several years from the development of the first symptoms [ 2 ]. Despite substantial intervention efforts, an estimated 20% of AN patients show limited improvements and, over time, become chronic [ 3 , 4 ]. Despite that, there are very few studies on chronic AN, especially in older populations, probably due to the relatively high drop out rate after a few years of treatment [ 5 , 6 ].
To delineate the domain of chronic AN, the definition of Severe and Enduring Anorexia Nervosa (SE-AN) had been proposed [ 7 ] (Table 1 ), accompanied by suggested maintenance factors [ 8 ]. This definition is useful to describe and analyze the peculiarities of chronic patients, to improve the relatively broad criteria for SE-AN definition and to better understand the clinical development of this ED. The search for a precise terminological framework has shown that the quality of the words used in the definitions, in addition to carrying the risk of stigmatizing patients, can influence the way patients and their families experience ED. Moreover, it can have a significant impact on the perspectives that clinicians have on treatment. For instance, the labels 'chronic' and 'treatment resistant' can both affect clinicians' perspective on a patient's curability or their willingness to engage cooperatively during the treatment. Other terms, such as 'severe and enduring’, 'long-lasting' and similar expressions relating to the severity and duration variation of the disease, may favor a lesser focus on the curability of an individual.
In the present case series, we aim to provide an overview of the possible associations that exist among the multiple variables, causal or consequential, peculiar to SE-AN. The search for common causal factors, although within a small population of patients with SE-AN, may facilitate a better understanding of the disorder and its main determinants in order to intercept cases that are more likely to develop a long history of illness or severe forms that would necessitate intensive treatment. It could also help to improve and personalize the therapeutic approach towards this specific population, considering that even today the available treatments do not always guarantee a positive outcome. In addition, this case series directs its focus on the effects of the disease, treatment compliance, and the description of variables that could contribute to a comprehensive understanding of the complex nature of the disorder.
Materials and methods
In the present case series, 14 patients were selected from those currently or previously taken care of at the ED Outpatients Unit of the Maggiore Hospital in Bologna between January 2012 and May 2023. To make the sample more homogeneous, we selected only adult patients (age > 18 years, by Italian law) who fully fit the eligibility criteria for SE-AN, as proposed by Hay and Touyz in 2018 [ 7 ].
Information on individual patients was obtained through data collection from several available sources: Electronic Medical Records (EMR), paper records, and other documents available in the psychiatric department.
Demographic characteristics
A total of 14 patients were enrolled, all from Bologna and its province, and all with a history of admission to Public Psychiatric Services (100%). Five patients (35.7%) were still in psychiatric service care, while four patients dropped out of services (28.6%). One patient had died. At the time of data collection, four patients (8.6%) were no longer followed within a psychiatric pathway. A summary of the main clinical and social characteristics of the patients is presented in Tables 2 and 3 .
The patients were all female (100%). The sample had an average age of 42.2 years old (ranging from 24 to 63 years old). Only four out of 14 patients (28.6%) were married and none of them had gone through a divorce. Three patients (21.4%) had at least one child, and only one had more than one. Therefore, the majority of candidates with SE-AN were not married (71.4%) and had no children (78.6%). However, 86% of the patients lived with someone: six lived with their partner/husband, and six with the family of origin.
Almost all of the patients had a job during their lifetime (78.6%), including seven employees (who carried out office work, without any specific responsibility), two hairdressers, one bartender, and one lawyer. Among those who had never worked, two were University students. Therefore, only one out of 14 patients never worked or pursued a college career. Among the 11 individuals who had had a job, however, only three people were known to be employed at the time of the analysis (27.3%). For two people, no data regarding their working life were available on their medical records.
Among the 14 patients, seven (50%) had a cigarette smoking habit, while two (14.2%) had a history of alcohol abuse. Three (21.4%) had a history of self-injury.
Clinical characteristics
The average age of onset of ED symptoms in our sample was 22.7 years (range 11–47), while the average age at which a diagnosis of AN was made in public services (Psychiatry or Dietetics) was 31.5 years (range 16–51). The patients had a mean disease duration of 17 years (range 8–31) combined, in the vast majority of cases (85.7%), with a series of unsuccessful therapeutic attempts. The latency period between the onset of the disease and its recognition by public health services was 8.79 years (range 1–34 years); in nine out of 12 cases (64.3%) the diagnosis was made after at least three years of illness, while in 6 cases (42.9%) after at least seven years.
The most frequent AN subtype in the considered sample was AN-Restrictive (85.7%), while only two patients (14.3%) suffered from the AN-Binge/Purging subtype. The most frequently reported caloric restriction methods were reduced caloric intake and intense physical exercise; this was followed by laxative use, self-induced vomiting, and diuretic use.
The average patient’s Body Mass Index (BMI) reported was 13.43 kg/m 2 (range 7.53–16.94 kg/m 2 ), highlighting the extreme severity of the cases described (according to the DSM-5 [ 1 ], AN patients with BMI < 15 kg/m 2 are classified as showing “extreme severity”). The patient with the lowest BMI included in the case series reached a value of 7.15 kg/m 2 .
Eleven patients (78.6%) had been hospitalized at least once in an internal medicine department because of their ED, due to their severe malnutrition; in addition, among the three patients who had never faced hospitalization, two had previously refused it several times despite the need expressed by their caregivers. In contrast, at least two out of 14 (14.3%) had multiple accesses and one patient was hospitalized at the time of data collection. In parallel, seven of the patients (50%) were admitted at least once to a psychiatric department to manage their disorder. In the examined clinical context, six patients (42.9%) received enteral nutrition through nasogastric tube administration on at least one occasion, while an additional six patients (42.9%) required parenteral nutrition. The purpose of the parenteral nutrition intervention was to augment daily caloric intake and provide supplementary support to oral nutrition exclusively.
Common complications of AN, such as anemia and hypokalemia, and their treatment needs, were also investigated. In 50% of the patients, the occurrence of at least one episode of anemia during the natural history of the disease was reported. Anemia was most commonly macrocytic (57%). Regarding treatment, at least 42.9% of anemia cases were of such severity that they required blood transfusion, 28.6% required only iron and vitamin supplementation. 21.4% had no history of anemia. For the 28.6% no data about the occurrence of anemia as a complication of their disorder was found examining the available clinical records, while several patients refused to take blood tests. At least one episode of hypokalemia was reported in 50% of cases. Of the seven confirmed cases of hypokalemia, 100% required treatment, and at least three were of such severity as to require intravenous infusion therapy.
Other ED complications present within the considered sample, consequences of persistent malnutrition and secondary hormonal disorders typical of AN, included osteoporosis and secondary amenorrhea. In 57.1% of the cases frank osteoporosis was shown and in 28.6% osteopenia was demonstrated. In 93% of patients there was at least one period of secondary amenorrhea during the natural history of the disease (no data regarding one individual); these included two patients taking an Estrogen-Progestin (EP) pill and two who reached menopause before having the diagnosis of AN (one of whom was in early menopause).
The presence of psychiatric comorbidities in the history of these subjects was assessed (Table 4 ), founding that 100% had at least one other psychiatric diagnosis in comorbidity to the ED (not necessarily present to date); three out of 14 patients (21.4%) had only one psychiatric comorbidity, nine (64.3%) had two, and two patients (14.2%) had up to three psychiatric disorders in addition to AN.
It was reported that 50% of patients had a history of familial psychiatric illness, and 14.2% had a parent with severe obesity.
With respect to the therapeutic approaches used for these patients, previous drug therapy attempts employed in ED treatment (in part related to the management of the various psychiatric comorbidities present in the individual cases), and the execution of ED-specific therapeutic pathways (e.g., Dietary care), were evaluated as far as possible.
Nine patients had experienced at least one ED-specific pathway, while five had never been through one; among the latter, four out of five had rejected the proposed ED treatment course, while one was considering the proposal at the time of the data collection. The setting most frequently used by those who had embarked on an ED treatment course was outpatient (100%), followed by semi-residential and residential (44.4%). Among those who started an ED pathway: six completed it, two dropped out, and one moved away.
Regarding the pharmacological therapies taken by patients during their treatment course, the use of three pharmacological classes mainly used in AN treatment (antidepressants, antipsychotics, and benzodiazepines) was analyzed, also considering the possible combined therapeutic indication with respect to the individuals' psychiatric comorbidities.
Nine out of 14 (64.3%) patients used at least one antipsychotic drug, while 28.6% never used antipsychotics; of one out of 14 patients no data were found about antipsychotic administration from the examined clinical documentations. Among users, at least three used more than one antipsychotic in their history, and the most frequently prescribed drug was olanzapine (66.7%), followed by risperidone (22%) and aripiprazole (22%).
11 of 14 patients (78.6%) used at least one antidepressant drug to manage their psychiatric disorders; two patients never used it (n = 14.3%), and one rejected the suggested treatment. Among antidepressant users, 36.4% used more than one. The most commonly prescribed antidepressant was sertraline (77.8%), followed by venlafaxine (44.4%).
Nine out of 14 individuals (64.3%) used at least one benzodiazepine during their course of treatment in psychiatric services. Four patients (28.6%) never used benzodiazepines: three had not been prescribed and one refused to take them. There was one reported case of benzodiazepine abuse, while for one patient no data was found in the available clinical records regarding sedative medications. The most commonly used benzodiazepine appears to be alprazolam (40%).
Lastly, the information obtained showed that all patients (100%) undertook individual psychotherapy during their treatment process, even though duration, frequency, and type of psychotherapeutic courses were not reported in the records.
The present work gives an insight into SE-AN, analyzing clinical features, treatment approaches, and risk factors that might contribute to the persistence of this disorder. Our patients showed a long history of illness, with an average duration of 17 years, punctuated by therapeutic failures. The majority of patients were diagnosed with the restrictive subtype of AN, characterized by caloric restriction methods, including reduced intake and intense physical exercise. The BMI average was 13.43 kg/m 2 , data highlighting the extreme severity of this clinical sample, aligning with the DSM-5 classification of extreme severity for AN patients with BMI < 15 kg/m 2 [ 1 ]. We identified a high prevalence of hospitalizations due to severe malnutrition or the occurrence of medical complications (i.e., anemia, hypokalemia, osteoporosis, amenorrhea). Moreover, the majority of the sample also suffered from psychiatric comorbidities. The presence and severity of these aspects confirms the condition of intense medical and psychological burden faced by these patients [ 9 , 10 ].
The treatment history of these individuals has often proven to be complex and ineffective, despite the multitude of approaches used, including outpatient, semi-residential, or residential treatment. In addition, this work has highlighted a difficulty on the part of the health care system in identifying the disease at the time of its presentation, leading to diagnostic delays and higher therapeutic resistance. In fact, consolidation of the symptoms and psychopathological mechanisms over time in AN patients reduces the likelihood of positive outcomes following treatments, consequently limiting the chances of recovery for these individuals [ 11 ]. There is growing bio‐behavioral evidence in EDs that the disease changes over time, with maladaptive eating and weight control behaviors becoming more automatic and entrenched [ 12 , 13 , 14 , 15 , 16 , 17 ]. Consistent with these results, many clinical studies suggest that response to treatment is more positive in the early stages of the disease (i.e., within the first three years of ED onset), and decreases the longer the condition persists [ 18 , 19 ] .
Likewise, it has been reported that, during early-stage ED, longer disease duration is associated with higher psychological distress and occupational and social impairment [ 9 , 20 ] . Therefore, the lack of—or delay in access to—treatment during the early-stage ED may facilitate chronicity, negatively impact the chances of recovery, impair social and occupational accomplishment [ 21 ]. In fact, from an environmental point of view, our sample showed relatively poor social and occupational adjustment, most of the patients not being married (71.4%), without children (78.6%), and unemployed (72.7%) at the time of data collection. These findings are in line with recent studies in the field, which characterizes individuals with SE-AN as impoverished in terms of intimacy and relationships [ 3 , 22 ], and exhibiting a propensity for economic frugality, some living below the poverty line, without well-remunerated employment behind them [ 22 , 23 ].
The duration of untreated ED (DUED) is the period of time between disease onset and the start of evidence‐based treatment. In the existing literature, the average DUED is reported to be between two and three years for anorexia nervosa (AN) [ 24 ] . However, it is noteworthy that our study yielded different findings, as we observed an average DUED of 8.79 years in our sample, with a wide-ranging variation from as short as 1 year to as long as 39 years. This significant deviation from the established averages underscores the heterogeneity and complexity of DUED across different populations, warranting further exploration to elucidate the contributing factors.
DUED can be divided into two distinct stages [ 25 ] . The initial stage is characterized by delays mostly driven by patient‐related factors, wherein individuals may experience symptoms but fail to recognize the presence of a problem or may not be prepared to seek help. In the second stage, individuals seek treatment, but they encounter service‐level delays, further prolonging the untreated illness period.
Flynn et al. [ 21 ] evaluated the role of First Episode Rapid Early Intervention for ED (FREED), finding that FREED, significantly reducing the DUED, is associated with significantly shorter wait times for both assessment and treatment, higher patients compliance to treatment, and possible distress reduction and deterioration prevention. The same results are suggested by Andrés-Pepiñá et al. [ 26 ], reporting that a substantial percentage of patients with adolescence-onset AN achieve complete remission of the disorder when they undergo specialist treatment, and an early intervention in AN may help to improve the disorder course. Also, Austin et al. [ 24 ] suggested that DUED may be a modifiable factor influencing EDs outcomes and that a shorter DUED may be related to a higher probability of remission.
Diagnostic and treatment delays appear to be partly attributable to gaps in the health system and scarce economic resources, and partly attributable to the ego-syntonic nature of the disorder itself. The treatment refractoriness, pushing the patient away from the therapeutic paths taken, if not rejected out of hand, is usually a result of an incomplete understanding of their disease state [ 25 , 27 ]. People with AN tend to hide their state of emaciation, avoiding an established relationship with primary care and resorting to emergency departments only when medical problems arise [ 28 ], leading in some cases to hospitalization. The prevalence of untreated individuals with EDs is estimated to be as high as 75% [ 29 ]. This considerable percentage may be attributed, in part, to comorbid conditions that influence motivation, scheduling constraints, or the need for clinical prioritization within general mental health services. These factors can result in delayed or hindered access to specialized ED services, particularly in cases where individuals with EDs also present with concurrent issues such as self-harm or suicidal behaviors [ 30 ].
Diagnostic-therapeutic delays thus lead to high rate of medical comorbidities due to malnutrition, the need for internal medicine/psychiatric hospitalization, as well as the substantial burden of psychiatric comorbidities [ 9 , 10 , 20 , 31 ]. Medical comorbidities and complications associated with EDs can range from mild to severe and life-threatening, potentially involving all body systems and placing people at increased risk of medical instability and death [ 32 ]. Therefore, understanding how comorbidities and co-occurring medical complications impact EDs is fundamental to treatment and recovery. In addition to the ED-associated medical comorbidities, EDs often occur together with other psychiatric conditions. Psychiatric comorbidities in people with EDs are associated with higher emergency department presentations and hospitalizations and health system costs [ 33 ]. Comorbidities may result from symptoms and behaviors associated with the ED, be co-occurring, or precede the ED onset [ 34 , 35 ]. People with an ED, their caregivers and care providers often face a complex dilemma: the individual with ED needs treatment for not only for their ED but also for their psychiatric comorbidities, and it can be hard to determine which is the clinical priority. This is further complicated because EDs and comorbidities may have a reciprocal relationship of mutual worsening, exacerbating each other's symptoms and negatively impacting treatments and outcomes.
The case series also confirms what literature shows about how the severity of SE-AN cannot be defined solely by BMI value and resistance to treatment [ 36 , 37 , 38 ], but also by the multiplicity of possible negative consequences that mark the life course of these patients, and the increasing consolidation of ED related psychopathology [ 39 ]. Repeated hospitalizations, severe complications, frequent comorbidities, a variety of unproven drug treatments are all equally present variables that indelibly mark the very long history of the disease.
This case series presented 14 cases of adult patients affected by SE-AN. It highlighted the relevant issue of resistance to treatment that marks the life course of these subjects, as well as the prospect of a variety of complications, both medical, psychological as well as social. The chronicity of this disorder is determined by the overlapping of numerous elements. First of all, the very nature of the disorder, which often makes the patient less likely to seek treatment, the difficulty of the health system in recognizing the problem in its early stages, but also the presence of an occupational and social impairment. Further studies on the topic are needed to broaden the knowledge of this disorder and its pathogenesis. This will enable us to develop more precise and effective interventions.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author following a reasonable request.
Abbreviations
- Anorexia Nervosa
Body Mass Index
Diagnostic and statistical manual of mental disorders, 5th edition
duration of untreated eating disorder
Eating Disorder
Estrogen-progestin
First episode rapid early intervention for eating disorders
Obsessive compulsive disorder
Personality disorder
Severe and Enduring Anorexia Nervosa
DSM Library [Internet]. [cited 2023 Apr 30]. Diagnostic and statistical manual of mental disorders. https://doi.org/10.1176/appi.books.9780890425787
Dobrescu SR, Dinkler L, Gillberg C, Råstam M, Gillberg C, Wentz E. Anorexia nervosa: 30-year outcome. Br J Psychiatry J Ment Sci. 2020;216(2):97–104.
Article Google Scholar
Kiely L, Conti J, Hay P. Conceptualisation of severe and enduring anorexia nervosa: a qualitative meta-synthesis. BMC Psychiatry. 2023;23(1):606.
Article PubMed PubMed Central Google Scholar
Eddy KT, Tabri N, Thomas JJ, Murray HB, Keshaviah A, Hastings E, et al. Recovery from anorexia nervosa and bulimia nervosa at 22-year follow-up. J Clin Psychiatry. 2017;78(2):184–9.
Steinhausen HC. Outcome of eating disorders. Child Adolesc Psychiatr Clin N Am. 2009;18(1):225–42.
Article PubMed Google Scholar
Fichter MM, Quadflieg N, Crosby RD, Koch S. Long-term outcome of anorexia nervosa: results from a large clinical longitudinal study. Int J Eat Disord. 2017;50(9):1018–30.
Hay P, Touyz S. Classification challenges in the field of eating disorders: can severe and enduring anorexia nervosa be better defined? J Eat Disord. 2018;6:41.
Herpertz-Dahlmann B. Serious and enduring anorexia nervosa from a developmental point of view: how to detect potential risks at an early stage and prevent chronic illness? Int J Eat Disord. 2020;53(8):1313–4.
Davidsen AH, Hoyt WT, Poulsen S, Waaddegaard M, Lau M. Eating disorder severity and functional impairment: moderating effects of illness duration in a clinical sample. Eat Weight Disord. 2017;22(3):499–507.
van Hoeken D, Hoek HW. Review of the burden of eating disorders: mortality, disability, costs, quality of life, and family burden. Curr Opin Psychiatry. 2020;33(6):521–7.
Steinhausen HC. The outcome of anorexia nervosa in the 20th century. Am J Psychiatry. 2002;159(8):1284–93.
Berner LA, Marsh R. Frontostriatal circuits and the development of bulimia nervosa. Front Behav Neurosci. 2014;8:395.
Dalton B, Foerde K, Bartholdy S, McClelland J, Kekic M, Grycuk L, et al. The effect of repetitive transcranial magnetic stimulation on food choice-related self-control in patients with severe, enduring anorexia nervosa. Int J Eat Disord. 2020;53(8):1326–36.
Fladung AK, Schulze UME, Schöll F, Bauer K, Grön G. Role of the ventral striatum in developing anorexia nervosa. Transl Psychiatry. 2013;3(10):e315.
O’Hara CB, Campbell IC, Schmidt U. A reward-centred model of anorexia nervosa: a focussed narrative review of the neurological and psychophysiological literature. Neurosci Biobehav Rev. 2015;52:131–52.
Werthmann J, Simic M, Konstantellou A, Mansfield P, Mercado D, van Ens W, et al. Same, same but different: attention bias for food cues in adults and adolescents with anorexia nervosa. Int J Eat Disord. 2019;52(6):681–90.
Steinglass JE, Walsh BT. Neurobiological model of the persistence of anorexia nervosa. J Eat Disord. 2016;4:19.
Ambwani S, Cardi V, Albano G, Cao L, Crosby RD, Macdonald P, et al. A multicenter audit of outpatient care for adult anorexia nervosa: symptom trajectory, service use, and evidence in support of “early stage” versus “severe and enduring” classification. Int J Eat Disord. 2020;53(8):1337–48.
Treasure J, Stein D, Maguire S. Has the time come for a staging model to map the course of eating disorders from high risk to severe enduring illness? An examination of the evidence. Early Interv Psychiatry. 2015;9(3):173–84.
de Vos JA, Radstaak M, Bohlmeijer ET, Westerhof GJ. Having an eating disorder and still being able to flourish? Examination of pathological symptoms and well-being as two continua of mental health in a clinical sample. Front Psychol. 2018;9:2145.
Flynn M, Austin A, Lang K, Allen K, Bassi R, Brady G, et al. Assessing the impact of first episode rapid early intervention for eating disorders on duration of untreated eating disorder: a multi-centre quasi-experimental study. Eur Eat Disord Rev J Eat Disord Assoc. 2021;29(3):458–71.
Robinson PH, Kukucska R, Guidetti G, Leavey G. Severe and enduring anorexia nervosa (SEED-AN): a qualitative study of patients with 20+ years of anorexia nervosa. Eur Eat Disord Rev J Eat Disord Assoc. 2015;23(4):318–26.
Robinson P. Severe and enduring eating disorders: concepts and management. In: Anorexia and bulimia nervosa [Internet]. IntechOpen; 2019 [cited 2023 Aug 23]. https://www.intechopen.com/chapters/68319 .
Austin A, Flynn M, Richards K, Hodsoll J, Duarte TA, Robinson P, et al. Duration of untreated eating disorder and relationship to outcomes: a systematic review of the literature. Eur Eat Disord Rev J Eat Disord Assoc. 2021;29(3):329–45.
Birchwood M, Connor C, Lester H, Patterson P, Freemantle N, Marshall M, et al. Reducing duration of untreated psychosis: care pathways to early intervention in psychosis services. Br J Psychiatry J Ment Sci. 2013;203(1):58–64.
Andrés-Pepiñá S, Plana MT, Flamarique I, Romero S, Borràs R, Julià L, et al. Long-term outcome and psychiatric comorbidity of adolescent-onset anorexia nervosa. Clin Child Psychol Psychiatry. 2020;25(1):33–44.
Starzomska M, Rosińska P, Bielecki J. Chronic anorexia nervosa: patient characteristics and treatment approaches. Psychiatr Pol. 2020;54(4):821–33.
Striegel-Moore RH, Dohm FA, Kraemer HC, Schreiber GB, Crawford PB, Daniels SR. Health services use in women with a history of bulimia nervosa or binge eating disorder. Int J Eat Disord. 2005;37(1):11–8.
Wonderlich S, Mitchell JE, Crosby RD, Myers TC, Kadlec K, Lahaise K, et al. Minimizing and treating chronicity in the eating disorders: a clinical overview. Int J Eat Disord. 2012;45(4):467–75.
Hay P, Touyz S. Treatment of patients with severe and enduring eating disorders. Curr Opin Psychiatry. 2015;28(6):473–7.
Hudson JI, Hiripi E, Pope HG, Kessler RC. The prevalence and correlates of eating disorders in the national comorbidity survey replication. Biol Psychiatry. 2007;61(3):348–58.
Mehler PS, Birmingham C, Crow S, Jahraus J. Medical complications of eating disorders. Treat Eat Disord. 2010;1(48):66–80.
Google Scholar
John A, Marchant A, Demmler J, Tan J, DelPozo-Banos M. Clinical management and mortality risk in those with eating disorders and self-harm: e-cohort study using the SAIL databank. BJPsych Open. 2021;7(2):e67.
Monteleone AM, Pellegrino F, Croatto G, Carfagno M, Hilbert A, Treasure J, et al. Treatment of eating disorders: a systematic meta-review of meta-analyses and network meta-analyses. Neurosci Biobehav Rev. 2022;142:104857.
Van Alsten SC, Duncan AE. Lifetime patterns of comorbidity in eating disorders: an approach using sequence analysis. Eur Eat Disord Rev. 2020;28(6):709–23.
Smith KE, Ellison JM, Crosby RD, Engel SG, Mitchell JE, Crow SJ, et al. The validity of DSM-5 severity specifiers for anorexia nervosa, bulimia nervosa, and binge-eating disorder. Int J Eat Disord. 2017;50(9):1109–13.
Gianini L, Roberto CA, Attia E, Walsh BT, Thomas JJ, Eddy KT, et al. Mild, moderate, meaningful? Examining the psychological and functioning correlates of DSM-5 eating disorder severity specifiers. Int J Eat Disord. 2017;50(8):906–16.
Engelhardt C, Föcker M, Bühren K, Dahmen B, Becker K, Weber L, et al. Age dependency of body mass index distribution in childhood and adolescent inpatients with anorexia nervosa with a focus on DSM-5 and ICD-11 weight criteria and severity specifiers. Eur Child Adolesc Psychiatry. 2021;30(7):1081–94.
Krug I, Binh Dang A, Granero R, Agüera Z, Sánchez I, Riesco N, et al. Drive for thinness provides an alternative, more meaningful, severity indicator than the DSM-5 severity indices for eating disorders. Eur Eat Disord Rev J Eat Disord Assoc. 2021;29(3):482–98.
Download references
Acknowledgements
Not applicable.
Author information
Authors and affiliations.
Department of Biomedical and Neuromotor Sciences, University of Bologna, Viale Pepoli 5, 40123, Bologna, Italy
Federica Marcolini, Alessandro Ravaglia, Silvia Tempia Valenta, Federica Sanna, Giulia Zilli, Enrico Magrini, Flavia Picone, Diana De Ronchi & Anna Rita Atti
Department of Clinical Nutrition, AUSL Bologna, Bologna, Italy
Giovanna Bosco
U.O. Cure Primarie, AUSL Area Vasta Romagna, ambito di Rimini, Rimini, Italy
Giorgia Marconi
You can also search for this author in PubMed Google Scholar
Contributions
Conception of the work: MF, ARA; design of the work: MF, RA; Acquisition, analysis, interpretation of data: BG, MG, SF, ZG, ME, PF; Drafted the work: MF, TVS; Revision of the work: ARA, DRD.
Corresponding author
Correspondence to Federica Marcolini .
Ethics declarations
Ethical statement and consent for publication.
Written informed consent was obtained from all participants in this study.
Competing interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Marcolini, F., Ravaglia, A., Tempia Valenta, S. et al. Severe-Enduring Anorexia Nervosa (SE-AN): a case series. J Eat Disord 11 , 208 (2023). https://doi.org/10.1186/s40337-023-00925-6
Download citation
Received : 04 July 2023
Accepted : 03 November 2023
Published : 22 November 2023
DOI : https://doi.org/10.1186/s40337-023-00925-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Eating disorders
- Severe-enduring
- Case series
Journal of Eating Disorders
ISSN: 2050-2974
- General enquiries: [email protected]
- Case report
- Open access
- Published: 05 June 2020
Case report: cognitive performance in an extreme case of anorexia nervosa with a body mass index of 7.7
- Simone Daugaard Hemmingsen ORCID: orcid.org/0000-0001-6789-7105 1 , 2 , 3 , 4 , 5 ,
- Mia Beck Lichtenstein ORCID: orcid.org/0000-0002-7885-9187 6 , 7 ,
- Alia Arif Hussain ORCID: orcid.org/0000-0002-1011-5165 8 , 9 ,
- Jan Magnus Sjögren ORCID: orcid.org/0000-0003-2060-1914 8 , 9 &
- René Klinkby Støving ORCID: orcid.org/0000-0002-4255-5544 1 , 2 , 3 , 4 , 5
BMC Psychiatry volume 20 , Article number: 284 ( 2020 ) Cite this article
4253 Accesses
7 Citations
1 Altmetric
Metrics details
Studies show that adult patients with anorexia nervosa display cognitive impairments. These impairments may be caused by illness-related circumstances such as low weight. However, the question is whether there is a cognitive adaptation to enduring undernutrition in anorexia nervosa. To our knowledge, cognitive performance has not been assessed previously in a patient with anorexia nervosa with a body mass index as low as 7.7 kg/m2.
Case presentation
We present the cognitive profile of a 35-year-old woman with severe and enduring anorexia nervosa who was diagnosed at the age of 10 years. She was assessed with a broad neuropsychological test battery three times during a year. Her body mass index was 8.4, 9.3, and 7.7 kg/m 2 , respectively. Her general memory performance was above the normal range and she performed well on verbal and design fluency tasks. Her working memory and processing speed were within the normal range. However, her results on cognitive flexibility tasks (set-shifting) were below the normal range.
Conclusions
The case study suggests that it is possible to perform normally cognitively despite extreme and chronic malnutrition though set-shifting ability may be affected. This opens for discussion whether patients with anorexia nervosa can maintain neuropsychological performance in spite of extreme underweight and starvation.
Trial registration
ClinicalTrials.gov, NCT02502617 . Registered 20 July 2015.
Peer Review reports
A growing amount of evidence indicate that anorexia nervosa (AN) is associated with impaired or inefficient neuropsychological performance in relation to healthy control subjects, regarding attention [ 1 , 2 ], memory [ 1 , 2 , 3 , 4 ], processing speed [ 4 ], and especially the executive functions [ 5 ] central coherence [ 6 ], decision-making [ 6 , 7 ], and cognitive flexibility [ 8 , 9 ]. It has been debated whether this is related to state (due to factors such as malnutrition) or trait (a premorbid trait or endophenotype of the disorder [ 10 ]). Some studies have found that patients who recovered from AN have impaired cognitive performance compared to healthy control subjects [ 11 , 12 ], supporting the trait theory of the disorder. However, longitudinal studies have found that executive functions can be normalized following weight stabilization in patients with AN [ 13 , 14 ], supporting the state theory.
Research on cognitive performance before and after re-nutrition in adult patients with extreme and chronic AN is sparse. Some studies have examined cognitive performance in patients with AN with a mean body mass index (BMI) below 15 kg/m2 (e.g. [ 10 ]), corresponding to extreme AN severity according to the Diagnostic and Statistical Manual of Mental Disorders 5 (DSM-5) [ 15 ]. However, it is unclear if patients with AN with BMI below 10 kg/m2 will display the same cognitive profile.
It has been suggested that malnutrition might affect cognitive performance since the classic Minnesota Semi-Starvation Experiment [ 16 ], where cognitive functions were studied in 36 healthy military objectors with normal weight before and after semistarvation with 25% weight-loss over a 24-week period. The men reported decline in concentration. However, the standardized tests that were administered did not confirm measurable alterations. Newer research on healthy subjects, although somewhat inconclusive, indicates affected psychomotor speed and executive functions following short-term semi-starvation [ 17 ].
However, other factors than malnutrition or weight-loss have been suggested to affect cognitive performance in patients with AN, such as long illness duration [ 18 ] and age [ 18 ]. This could explain a difference in results for children/adolescents and adults with AN mentioned in the literature [ 19 , 20 ], which cannot be explained by the trait theory.
The current case report was part of an ongoing longitudinal research project investigating the effect of re-nutrition on cognitive performance in patients with severe AN. The aim of the case study was to present the neuropsychological performance of a patient with chronic AN and extremely low BMI in order to discuss whether extremely low weight and long duration of illness are associated with cognitive impairment and if cognitive adaptation takes place. No study to our knowledge has previously reported on the cognitive profile of a patient with AN with a BMI as low as 7.7 kg/m2.
We want to introduce the idea of cognitive adaptation to severe malnutrition as a supplement to the discussion on cognitive impairment in AN. However, this idea should not be confused with Taylor’s Theory of Cognitive Adaptation [ 21 ]. The presented idea of cognitive adaptation is the idea that cognitive functions can adapt to persisting low weight in AN, i.e. cognitive performance can remain normal or regain normality in severe and enduring AN. The adaptation does not exclude specific cognitive impairment.
The current case report investigates the cognitive profile of a 35-year-old Caucasian woman with extremely severe and enduring AN who was diagnosed at the age of 10 years. The patient’s weight loss is accomplished through fasting. According to the DSM-5 [ 15 ], the patient’s symptoms are in accordance with the restricting type and the severity of AN for the patient is categorized as extreme. The patient has had low body weight since the onset of the disease 25 years ago. Consequently, she is still prepubescent.
The patient’s extreme malnutrition, the medical complications, and the refeeding treatment has previously been described in a case report [ 22 ]. Since the previous report [ 22 ], she has survived another 5 years, living in her own residence with several stabilizing hospitalizations. Her nadir BMI, defined as the lowest registered BMI, has decreased further to 7.2 kg/m2. To our knowledge, this is the lowest BMI reported in AN in the literature. During her long and severe illness course, she has participated in psychotherapy for years. However, during the past few years, she has refused to participate in psychotherapy, while she has continued the harm-reducing treatment in the nutrition department. No cognitive profile has been assessed before the current report.
She has continuously been provided supplementation with vitamins and minerals. At the present admission, she weighed 20.2 kg, including edema corresponding to at least 2 kg, and her height was 1.55 m, corresponding to a BMI of 8.41 kg/m 2 . After life-saving and stabilizing fluid and electrolyte correction, and refeeding according to guidelines [ 23 ] during 2 weeks of hospitalization, we tested her with a neuropsychological test battery (2 weeks after admission: T 0 ). After an additional 2 months of hospitalization, she could not be motivated to continue the treatment any longer. Due to years of history with rapid relapse after prolonged forced treatment, she was allowed to be discharged to outpatient follow-up. She was re-tested in the outpatient clinic 6 days following dropout from inpatient treatment and approximately 3 months after admission, (re-test: T 1 ) with a weight of 22.4 kg (BMI: 9.3 kg/m 2 ), and again at 12 months from T 0 , during a re-hospitalization, 7 days after admission (follow-up: T 2 ), with BMI 7.7 kg/m 2 . Thus, T 0 and T 2 were done at the hospital after initial stabilizing glycemic, fluid- and electrolyte correction, whereas T 1 was done in an outpatient setting, where she was in a clinically stable condition, but without the initial stabilizing treatment.
The psychopathological profile of the patient
The patient scored 21 on the Beck Depression Inventory II (BDI-II [ 24 ];) indicating moderate depression at 2 weeks after admission (T 0 ). Her scores on the Eating Disorder Inventory 3 (EDI-3 [ 25 ];) at T 0 are presented in Table 1 below. Compared to the Danish validation of EDI-3 for patients with AN ( [ 26 ]; Table 1 ), her low scores on the Drive for Thinness, the Interoceptive Deficits, the Perfectionism, and the Asceticism subscales are of interest.
Qualitative observations
During the first 2 weeks after admission, the patient was unable to participate in the neuropsychological assessment due to fatigue. Two weeks after admission, when the baseline assessment took place (T 0 ), the patient was lying down during the assessment and was noticeably tired. This was neither the case at retest (T 1 ) nor at follow-up (T 2 ) where the patient was sitting at a table. Her alertness and energy level at follow-up (T 2 ) were notable in light of her low BMI. The patient was calm during all three assessments (divided into six sessions) and expressed that the tests were fun. The aim of the study was explained to the patient before the first administration. However, only information written in the test manuals was given during each assessment.
The following validated neuropsychological tests were selected in cooperation with an experienced neuropsychologist to examine a wide range of cognitive functions: the Wechsler Memory Scale III (WMS-III) [ 27 ]; the d2-R Test of Attention – Revised [ 28 , 29 ]; the Processing Speed Index (PSI) of the Wechsler Adult Intelligence Scale IV (WAIS-IV) [ 30 ]; the Delis-Kaplan Executive Function System (D-KEFS) [ 31 ], Verbal Fluency Test, Design Fluency Test and Trail Making Test; and the Wisconsin Card Sorting Test Revised and Expanded (WCST) [ 32 ] (only administered at T 0 ). Information on each test variable, including internal consistency and test-retest reliability, are presented in Table 2 . The test battery can be administered in approximately 2 h. For all three administrations, the test battery was divided into two sessions (1 h per session) 1 day apart.
Neuropsychological findings
Table 3 gives an overview of the timeline of the patient’s raw scores and scaled scores on the test battery. Table 4 presents the patient’s norm scores and percentiles on the WMS-III, the WAIS-IV PSI, and the d2-R. Table 5 presents the patient’s WCST scores at 2 weeks after admission (T 0 ). Information on scoring are presented below each of the tables.
Memory performance on WMS-III
The patient’s scores on WMS-III indicate average to very superior auditory, visual, immediate and general memory performance (108 to 142; Mean: 100), and low average to average working memory (Table 4 ). The technical manual for WMS-III reports adequate test – retest reliability for all indexes in the age group 16–54 years, except for the Auditory Recognition Delayed Index ( [ 33 ]; Table 2 ). Estimated standard error of difference (S Diff ) scores were calculated based on Iverson and Grant ( [ 34 ]; Table 2 ). Differences between the three assessments are outlined here. Her scores on the Auditory Delayed Index decreased more than S diff : 6.70 from 132 (very superior) at 2 weeks after admission (T 0 ) to 108 (average) at re-test (T 1 ) and increased again to 132 (very superior) at follow-up (T 2 ). Her scores on the Visual Immediate Index increased slightly more than S diff : 6.70 from 118 (high average) at re-test (T 1 ) to 127 (superior) at follow-up (T 2 ). Her scores on the Visual Delayed Index decreased more than S diff : 7.65 from 125 (superior) at re-test (T 1 ) to 109 (average) at follow-up (T 2 ). Her scores on the Immediate Memory Index increased more than S diff : 3.17 from 134 (very superior) at re-test (T 1 ) to 142 (very superior) at follow-up (T 2 ). Her scores on the Working Memory Index decreased more than S diff : 8.22 from 102 (average) at 2 weeks after admission (T 0 ) to 88 (low average) at re-test (T 1 ). The scores on the rest of the indexes did not change more than the estimated S diff scores between time points.
Cognitive flexibility on D-KEFS and WCST
Overall, she performed above average on the Verbal Fluency Test (Table 3 ) at all three test times compared to the normative population for age, except for her performance at re-test (T 1 ) on the switching condition, which was decreased more than S diff : 2.42 to average, and the high number of repetition errors (7; below average) at re-test (T 1 ) and (3; average) at follow-up (T 2 ).
She performed average to above average on the Design Fluency Test at all three test sessions (Table 3 ). However, the switching condition score was lower [ 6 ] at follow-up (T 2 ) compared to 8 at 2 weeks after admission (T 0 ) and re-test (T 1 ), though still average.
During follow-up (T 2 ) on the Trail Making Test (Table 3 ), her performance on the Number-Letter Sequencing test, measuring cognitive flexibility, was below average (111 s), in spite of being average at 2 weeks after admission (T 0 ; 90 s) and re-test (T 1 ; 79 s). The numbers condition was very low at T 0 (55 s; below average), improving somewhat at re-test (T 1 ; 46 s; below average) and follow-up (T 3 ; 41 s; below average). We have no explanation for this result. On the other conditions, her performance was average at all three test times on the Trail Making Test.
Her scores on the WCST (Table 5 ) 2 weeks after admission (T 0 ) place her in the mild to moderately-to-severely range of impairment on cognitive flexibility according to this task. She completed one out of six categories (< 1st percentile). She made 52 perseverative responses (< 1st percentile; standard score 55; moderately-to-severely impaired range). She committed 50 errors (8th percentile; standard score 79: mildly impaired range), of which 36 were perseverative errors (1st percentile; standard score 55: moderately impaired range).
WAIS-IV processing speed
The scores on the Processing Speed Index (Table 4 ) were average compared to the normative population for age at all three test times. There were no relevant differences between time points. She scored 93 at admission (T 0 ) and re-test (T 1 ) and 98 at follow-up (T 2 ).
d2-R test of attention
At 2 weeks after admission (T 0 ) and re-test (T 1 ), she had a small number of processed targets (426 and 420), 18th to 21st percentile (Tables 3 and 4 ), her concentration performance was 175 and 176 corresponding to the 42nd percentile and she committed three and no errors respectively (> 90th percentile). At follow-up (T 2 ), her concentration performance was above the mean (185; 54th percentile) but not increased more than S diff : 24.89. The total processed targets score was still low (451; 34th percentile), and she committed few errors (four; 90th percentile).
Discussion and conclusions
The patient exhibited average to very superior performance on verbal fluency, design fluency, processing speed, and memory. However, her working memory performance was low average. Her attention and concentration performance were below average to average, and her performance on cognitive flexibility tasks were average to moderately-to-severely impaired.
The present case report demonstrates surprisingly good cognitive performance in a patient with severe and enduring AN with extremely low BMI varying between 7.7 and 9.3 during the study period of 1 year. However, some of her executive functions seem to be impaired. This is in line with previous research on patients with AN [ 5 , 8 ]. The present results suggest that her working memory was normal (low average) in line with previous studies [ 35 , 36 ]. However, her working memory performance was lower compared to the rest of her memory performance, which was average to very superior. The results from the D-KEFS indicate average to above-average performance with perhaps somewhat weaker cognitive flexibility (below average to average). On the other hand, the results from the WCST indicate impairment in cognitive flexibility. The overall differences in performance between the three assessments were minimal. This indicates that the minor differences in BMI between the test assessments did not significantly affect her cognitive performance, as expected.
Impaired cognitive flexibility
It could be that impaired cognitive flexibility existed prior to the illness as a premorbid trait as suggested previously [ 10 ], or that the malnutrition has affected the patient’s cognitive flexibility. Since we are missing data on her premorbid level, we cannot draw any firm conclusions.
Impaired cognitive flexibility has previously been reported in patients with AN with higher BMI [ 37 ], indicating that impairments in cognitive flexibility do not necessarily relate to undernutrition. In patients with AN who had recovered from the illness, cognitive flexibility was in the normal range in this study. However, other studies found that individuals who recovered from AN exhibited more or less impaired executive functioning [ 10 ]. Longitudinal research on the relationship between different BMI states and cognitive performance is highly needed.
Impaired cognitive flexibility may also play a role in the perpetuation of AN. Impaired cognitive flexibility has been suggested as a maintenance factor [ 38 ] and a factor related to lack of illness insight characteristic of patients with restrictive AN [ 39 ]. Lack of illness insight could be related to treatment resistance [ 40 ]. The patient’s low scores on EDI-3 subscales also reflect a discrepancy between illness severity and self-reported symptoms. This discrepancy or ambivalence is part of the nature of the disorder reflected in the low motivation for recovery and high number of dropouts from treatment alongside an expressed desire to change [ 41 ].
Cognitive adaptation in anorexia nervosa
Survival of long-term starvation is only possible due to extensive adaptive endocrine and metabolic alterations [ 42 ]. How these alterations affect cognitive functions still remains to be clarified. Well-designed longitudinal studies on severely underweight patients with a long illness duration are lacking. However, the present case report suggests that essential preservation of some cognitive functions occurs even in extreme chronic semi-starvation.
The mechanisms allowing for such preservation remains a subject of speculation. Links can be made to research on neuroplasticity and functional reorganization of cognitive functions after brain injury since patients with AN have white matter alterations [ 43 ]. Research shows that brain maturation processes of especially the prefrontal cortex continue until people are approximately 25 years old [ 44 ]. Nutritional status seems to impact this brain maturation [ 44 ]. Executive functions associated with the prefrontal cortex could therefore be affected by undernutrition during development of prefrontal connections in the brain in adolescence and young adulthood. Thus, impairment on executive functions may not arise until adulthood in patients with AN. This is in line with research that found no cognitive flexibility impairment in children and adolescents with AN but impairments in adults with AN [ 19 , 20 ]. The literature indicates that other cognitive functions associated with the prefrontal cortex, such as memory, are also impaired in adults with AN [ 3 ]. However, overall, this literature is not as explicit as the literature showing cognitive flexibility impairment in adults with AN. The ambiguity in the literature indicates differences between cognitive functions related to the prefrontal cortex in patients with AN. It might be that some prefrontal connections potentially being affected during low weight in adolescence could be reorganized or “compensated for” with time as is possible with reorganization or apparent functional recovery after brain injury [ 45 ]. In that case, cognitive performance could be regained after impairment has occurred. Some dimensions of cognitive flexibility might, however, be more difficult to compensate for. This could explain specific cognitive flexibility impairment in patients recovered from AN [ 10 ] and explain that the patient in the present case report performed normal and superior on some functions associated with prefrontal connections (memory and verbal fluency) but poorer on cognitive flexibility. We therefore suggest that reorganization of some cognitive functions can occur in spite of persisting low weight in patients with AN. In line with the possibility of cognitive reorganization in AN, Cognitive Remediation Therapy seems to improve executive functioning in patients with AN [ 46 ]. The suggested theory of cognitive adaptation may therefore not be specific to persisting low weight in AN. However, fast, substantial weight-loss could affect cognitive performance differently than persisting low weight. Therefore, studies on starving healthy subjects, including the Minnesota Semi-Starvation Experiment [ 16 ], could show different results than studies on patients with severe and enduring AN. Likewise, studies on patients with short illness duration might find different results than studies of patients with enduring AN. It is also unclear if patients developing AN in adulthood will display the same cognitive impairments. In line with these reflections, a case report of a 27-year-old Japanese woman in a coma, with BMI of 8.5 kg/m 2 at admission, describes a patient with AN where the outcome of severe malnutrition was persistent neurologic sequelae [ 47 ]. The woman developed AN at the age of 21 years where the patient in the present case report was diagnosed at the age of 10 years. The difference in age of onset, duration of illness, and/or manner of weight-loss (fast, substantial weight-loss compared to persisting low weight) may have resulted in different outcomes for the women. It is, however, also a possibility that the patient in the present case report might have an extreme phenotype which enables her to perform well in spite of her being extremely underweight.
We cannot say how high the patient’s scores on the neuropsychological test battery might be if she had not been as malnourished. We assume the patient would perform better on cognitive flexibility tasks, that her processing speed and working memory would be higher, and that she would be able to concentrate better had she not been malnourished. This is somewhat supported by previous research. Although the literature suggests impaired cognitive performance in patients with AN, the reported impairments were limited compared to healthy subjects [ 8 , 48 ]. Furthermore, it may be that severely underweight patients with AN have a higher verbal IQ [ 49 ], which does not, however, exclude the possibility of specific cognitive impairments [ 50 ]. This could explain the patient’s high memory performance (and probably global IQ) alongside specific impairment in cognitive flexibility on the WCST. This case may therefore not differ from other patients with severe AN regarding cognitive performance. It may be that the superior performance related to some cognitive functions is a trait of severely underweight patients with AN and/or that a cognitive adaptation to enduring AN increases performance to the premorbid level. In this case, (regained) superior performance of some cognitive functions (i.e. memory and verbal IQ) can exist alongside cognitive impairment in others (i.e. cognitive flexibility). This may change our view of the cognitive profile and its development in patients with severe and enduring AN.
Regardless, the fact that we were able to test the patient in the present case, raises a discussion as to whether she and others with extremely low weight may be responsive to psychotherapy as well. In the present case, the patient underwent psychotherapy for several years albeit without any impact on her weight. More research focusing on the validation of neuropsychological tests including investigation of the practice effect in this patient population is needed.
The individual scores on neuropsychological tests should always be interpreted with care. Factors other than persisting low weight may affect neuropsychological performance (e.g. dehydration, stress, depression, and anxiety). In the present case, the patient did express depressive symptoms corresponding to moderate depression, which might have influenced results on impairment in cognitive flexibility. Furthermore, the patient might experience other issues related to cognitive performance in daily life, which cannot be discovered in a neuropsychological assessment context.
Obviously, conclusions can never be drawn from one case. However, since the neuropsychological testing included a broad range of tests and was repeated three times during a year, the present case report is valid as a basis for reflecting on the affected individual’s cognitive performance at this stage. The present case report demonstrates that cognitive functions may be largely preserved under extreme chronic malnutrition or that cognitive functioning may be regained (reorganized) in spite of extreme chronic malnutrition. More research on patients with AN with extremely low BMI (< 10) is needed to determine whether cognitive performance is affected by starvation and malnutrition.
Availability of data and materials
All data analyzed during this study are included in this published article in tables or text. Raw data in a fully anonymized version is available from the corresponding author on reasonable request.
Abbreviations
- Anorexia nervosa
Intelligence quotient
Body mass index
The Beck Depression Inventory II
The Eating Disorder Inventory 3
The Wechsler Memory Scale III
The Wechsler Adult Intelligence Scale IV
The Processing Speed Index
The Delis-Kaplan Executive Function System
The Wisconsin Card Sorting Test Revised and Expanded
Seed JA, Dixon RA, McCluskey SE, Young AH. Basal activity of the hypothalamic-pituitary-adrenal axis and cognitive function in anorexia nervosa. Eur Arch Psychiatry Clin Neurosci. 2000;250(1):11–5.
Article CAS PubMed Google Scholar
Seed JA, McCue PM, Wesnes KA, Dahabra S, Young AH. Basal activity of the HPA axis and cognitive function in anorexia nervosa. Int J Neuropsychopharmacol. 2002;5(1):17–25.
Biezonski D, Cha J, Steinglass J, Posner J. Evidence for Thalamocortical circuit abnormalities and associated cognitive dysfunctions in underweight individuals with anorexia nervosa. Neuropsychopharmacology. 2016;41(6):1560–8.
Article PubMed Google Scholar
Kjaersdam Telleus G, Jepsen JR, Bentz M, Christiansen E, Jensen SO, Fagerlund B, et al. Cognitive profile of children and adolescents with anorexia nervosa. Eur Eat Disord Rev. 2015;23(1):34–42.
Roberts ME, Tchanturia K, Stahl D, Southgate L, Treasure J. A systematic review and meta-analysis of set-shifting ability in eating disorders. Psychol Med. 2007;37(8):1075–84.
Abbate-Daga G, Buzzichelli S, Marzola E, Aloi M, Amianto F, Fassino S. Does depression matter in neuropsychological performances in anorexia nervosa? A descriptive review. Int J Eat Disord. 2015;48(6):736–45.
Bodell LP, Keel PK, Brumm MC, Akubuiro A, Caballero J, Tranel D, et al. Longitudinal examination of decision-making performance in anorexia nervosa: before and after weight restoration. J Psychiatr Res. 2014;56:150–7.
Article PubMed PubMed Central Google Scholar
Hirst RB, Beard CL, Colby KA, Quittner Z, Mills BM, Lavender JM. Anorexia nervosa and bulimia nervosa: a meta-analysis of executive functioning. Neurosci Biobehav Rev. 2017;83:678–90.
Tchanturia K, Davies H, Roberts M, Harrison A, Nakazato M, Schmidt U, et al. Poor cognitive flexibility in eating disorders: examining the evidence using the Wisconsin card sorting task. PLoS One. 2012;7(1):e28331.
Article CAS PubMed PubMed Central Google Scholar
Tchanturia K, Morris RG, Anderluh MB, Collier DA, Nikolaou V, Treasure J. Set shifting in anorexia nervosa: an examination before and after weight gain, in full recovery and relationship to childhood and adult OCPD traits. J Psychiatr Res. 2004;38(5):545–52.
Danner UN, Sanders N, Smeets PA, van Meer F, Adan RA, Hoek HW, et al. Neuropsychological weaknesses in anorexia nervosa: set-shifting, central coherence, and decision making in currently ill and recovered women. Int J Eat Disord. 2012;45(5):685–94.
Wu M, Brockmeyer T, Hartmann M, Skunde M, Herzog W, Friederich H-C. Reward-related decision making in eating and weight disorders: a systematic review and meta-analysis of the evidence from neuropsychological studies. Neurosci Biobehav Rev. 2016;61:177–96.
Lozano-Serra E, Andres-Perpina S, Lazaro-Garcia L, Castro-Fornieles J. Adolescent anorexia nervosa: cognitive performance after weight recovery. J Psychosom Res. 2014;76(1):6–11.
Firk C, Mainz V, Schulte-Ruether M, Fink G, Herpertz-Dahlmann B, Konrad K. Implicit sequence learning in juvenile anorexia nervosa: neural mechanisms and the impact of starvation. J Child Psychol Psychiatry. 2015;56(11):1168–76.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Washington: Author; 2013.
Book Google Scholar
Keys A, Brozek J, Henschel A, Mickelsen O, Taylor HL. The biology of human starvation (2 volumes). Minnesota: University of Minnesota Press; 1950.
Benau EM, Orloff NC, Janke EA, Serpell L, Timko CA. A systematic review of the effects of experimental fasting on cognition. Appetite. 2014;77:52–61.
Buhren K, Mainz V, Herpertz-Dahlmann B, Schafer K, Kahraman-Lanzerath B, Lente C, et al. Cognitive flexibility in juvenile anorexia nervosa patients before and after weight recovery. J Neural Transm (Vienna). 2012;119(9):1047–57.
Article Google Scholar
Telleus GK, Fagerlund B, Jepsen JR, Bentz M, Christiansen E, Valentin JB, et al. Are weight status and cognition associated? An examination of cognitive development in children and adolescents with anorexia nervosa 1 year after first hospitalisation. Eur Eat Disord Rev. 2016;24(5):366–76.
Lang K, Stahl D, Espie J, Treasure J, Tchanturia K. Set shifting in children and adolescents with anorexia nervosa: an exploratory systematic review and meta-analysis. Int J Eat Disord. 2014;47(4):394–9.
Taylor SE. Adjustment to threatening events: a theory of cognitive adaptation. Am Psychol. 1983;38(11):1161–73.
Frolich J, Palm CV, Stoving RK. To the limit of extreme malnutrition. Nutrition. 2016;32(1):146–8.
Robinson P, Jones WR. MARSIPAN: management of really sick patients with anorexia nervosa. BJPsych Advances. 2018;24(1):20–32.
Beck AT, Steer RA, Brown GK. Manual for the Beck depression inventory-II. San Antonio: Psychological Corporation; 1996.
Google Scholar
Garner DM. Eating disorder Inventory-3. Professional manual. Lutz: Psychological Assessment Resources, Inc.; 2004.
Clausen L, Rosenvinge JH, Friborg O, Rokkedal K. Validating the eating disorder Inventory-3 (EDI-3): a comparison between 561 female eating disorders patients and 878 females from the general population. J Psychopathol Behav Assess. 2011;33(1):101–10.
Wechsler D. WAIS-III WMS-III technical manual. San Antonio: The Psychological Corporation; 2002.
Brickenkamp R, Schmidt-Atzert L, Liepmann D. The d2 test of attention – revised. A test of attention and concentration. Oxford: Hogrefe; 2016.
Brickenkamp R. d2-testen – en vurdering af opmærksomhed of koncentration. Dansk vejledning. Hogrefe Psykologisk Forlag: Frederiksberg; 2006.
Wechsler D. Wechsler adult intelligence scale—fourth edition. Technical and interpretive manual. Pearson: San Antonio; 2008.
Delis DC, Kaplan E, Kramer JH. Delis-Kaplan executive function system - technical manual. Pearson: San Antonio; 2001.
Heaton RK, Chelune GJ, Talley JL, Kay GG, Curtiss G. Wisconsin Card Sorting Test Manual Revised and Expanded. 2nd edition ed. Lutz: Psychological Assessment Resources, Inc.; 1993.
Tulsky D, Zhu J, Ledbetter M, editors. WAIS-III WMS-III technical manual (Wechsler Adult Intelligence Scale & Wechsler Memory Scale) paperback updated. USA: The Psychological Corporation; 2002.
Iverson GL. Interpreting change on the WAIS-III/WMS-III in clinical samples. Arch Clin Neuropsychol. 2001;16(2):183–91.
Bradley SJ, Taylor MJ, Rovet JF, Goldberg E, Hood J, Wachsmuth R, et al. Assessment of brain function in adolescent anorexia nervosa before and after weight gain. J Clin Exp Neuropsychol. 1997;19(1):20–33.
Lauer CJ, Gorzewski B, Gerlinghoff M, Backmund H, Zihl J. Neuropsychological assessments before and after treatment in patients with anorexia nervosa and bulimia nervosa. J Psychiatr Res. 1999;33:129–38.
Tenconi E, Santonastaso P, Degortes D, Bosello R, Titton F, Mapelli D, et al. Set-shifting abilities, central coherence, and handedness in anorexia nervosa patients, their unaffected siblings and healthy controls: exploring putative endophenotypes. World J Biol Psychiatry. 2010;11(6):813–23.
Steinglass JE, Walsh BT, Stern Y. Set shifting deficit in anorexia nervosa. J Int Neuropsychol Soc. 2006;12(3):431–5.
Konstantakopoulos G, Tchanturia K, Surguladze SA, David AS. Insight in eating disorders: clinical and cognitive correlates. Psychol Med. 2011;41(9):1951–61.
Abbate-Daga G, Amianto F, Delsedime N, De-Bacco C, Fassino S. Resistance to treatment and change in anorexia nervosa: a clinical overview. BMC Psychiatry. 2013;13(1):294.
Guarda AS. Treatment of anorexia nervosa: insights and obstacles. Physiol Behav. 2008;94(1):113–20.
Stoving RK. Mechanisms In Endocrinology: Anorexia nervosa and endocrinology: a clinical update. Eur J Endocrinol. 2019;180(1):R9–r27.
Barona M, Brown M, Clark C, Frangou S, White T, Micali N. White matter alterations in anorexia nervosa: evidence from a voxel-based meta-analysis. Neurosci Biobehav Rev. 2019;100:285–95.
Arain M, Haque M, Johal L, Mathur P, Nel W, Rais A, et al. Maturation of the adolescent brain. Neuropsychiatr Dis Treat. 2013;9:449–61.
PubMed PubMed Central Google Scholar
Mogensen J. Reorganization of the injured brain: implications for studies of the neural substrate of cognition. Front Psychol. 2011;2:7.
Tchanturia K, Lounes N, Holttum S. Cognitive remediation in anorexia nervosa and related conditions: a systematic review. Eur Eat Disord Rev. 2014;22(6):454–62.
Bando N, Watanabe K, Tomotake M, Taniguchi T, Ohmori T. Central pontine myelinolysis associated with a hypoglycemic coma in anorexia nervosa. Gen Hosp Psychiatry. 2005;27(5):372–4.
Dobson KS, Dozois DJ. Attentional biases in eating disorders: a meta-analytic review of Stroop performance. Clin Psychol Rev. 2004;23(8):1001–22.
Schilder CMT, van Elburg AA, Snellen WM, Sternheim LC, Hoek HW, Danner UN. Intellectual functioning of adolescent and adult patients with eating disorders. Int J Eat Disord. 2017;50(5):481–9.
Lena SM, Fiocco AJ, Leyenaar JK. The role of cognitive deficits in the development of eating disorders. Neuropsychol Rev. 2004;14(2):99–113.
Download references
Acknowledgements
We would like to thank Professor Jesper Mogensen at the Unit for Cognitive Neuroscience, University of Copenhagen, Denmark, for his inputs regarding neurocognitive reorganization and the possibility of extending his model to the research field of anorexia nervosa.
The study was supported by government funding: The Psychiatric Research Fund of Southern Denmark (grants for material and PhD salary) and the University of Southern Denmark (faculty scholarship). Furthermore, the study was supported with grants for material by private funds: the Jascha Foundation and the Beckett Foundation. The funding sources had no role in the design, execution, interpretation, analysis, or publication of the study.
Author information
Authors and affiliations.
Centre for Eating Disorder, Odense University Hospital, Odense, Denmark
Simone Daugaard Hemmingsen & René Klinkby Støving
Research Unit for Medical Endocrinology, Odense University Hospital, Odense, Denmark
Department of Clinical Research, University of Southern Denmark, Odense, Denmark
Open Patient data Explorative Network (OPEN), Odense, Denmark
The Research Unit, Child and Adolescent Psychiatry, Mental Health Services in the Region of Southern Denmark, Odense, Denmark
Centre for Telepsychiatry, Mental Health Services in the Region of Southern Denmark, Odense, Denmark
Mia Beck Lichtenstein
Department of Psychology, University of Southern Denmark, Odense, Denmark
Eating Disorder Unit, Mental Health Centre Ballerup, Mental Health Services in the Capital Region of Denmark, Copenhagen, Denmark
Alia Arif Hussain & Jan Magnus Sjögren
Department of Clinical Medicine, University of Copenhagen, Copenhagen, Denmark
You can also search for this author in PubMed Google Scholar
Contributions
SDH and RKS completed the data collection. RKS was the initiator of the project. SDH, RKS, and MBL all took part in the design of the study. SDH, RKS, MBL, JMS and AAH were all contributors in writing the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Simone Daugaard Hemmingsen .
Ethics declarations
Ethics approval and consent to participate.
The research project has been approved by the Regional Scientific Ethical Committee for the Region of Southern Denmark and was carried out in accordance with the 1964 Helsinki declaration and its later amendments. The authors state that the patient has given written and informed consent for participation in the study.
Consent for publication
The authors state that the patient has given written and informed consent for publication of the case report.
Competing interests
The authors declare that there are no conflicts of interest. None of the authors have received financial support or benefits from commercial sources for this study.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Hemmingsen, S.D., Lichtenstein, M.B., Hussain, A.A. et al. Case report: cognitive performance in an extreme case of anorexia nervosa with a body mass index of 7.7. BMC Psychiatry 20 , 284 (2020). https://doi.org/10.1186/s12888-020-02701-1
Download citation
Received : 13 February 2020
Accepted : 28 May 2020
Published : 05 June 2020
DOI : https://doi.org/10.1186/s12888-020-02701-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Cognitive performance
- Neuropsychology
- Undernutrition
BMC Psychiatry
ISSN: 1471-244X
- General enquiries: [email protected]

Eating Disorder Treatment and Recovery
- Bulimia Nervosa: Signs, Symptoms, and Treatment
Helping Someone with an Eating Disorder
- Orthorexia Nervosa: Signs, Symptoms, and Treatment
Binge Eating Disorder
- Body Shaming: The Effects and How to Overcome it
- Cognitive Behavioral Therapy (CBT): What it is, How it Helps
Body Dysmorphic Disorder (BDD)
- Online Therapy: Is it Right for You?
- Mental Health
- Health & Wellness
- Children & Family
- Relationships
Are you or someone you know in crisis?
- Bipolar Disorder
- Eating Disorders
- Grief & Loss
- Personality Disorders
- PTSD & Trauma
- Schizophrenia
- Therapy & Medication
- Exercise & Fitness
- Healthy Eating
- Well-being & Happiness
- Weight Loss
- Work & Career
- Illness & Disability
- Heart Health
- Learning Disabilities
- Family Caregiving
- Teen Issues
- Communication
- Emotional Intelligence
- Love & Friendship
- Domestic Abuse
- Healthy Aging
- Alzheimer’s Disease & Dementia
- End of Life
- Meet Our Team
What is anorexia nervosa?
Types of anorexia, am i anorexic, signs and symptoms of anorexia, anorexia causes and risk factors, effects of anorexia, getting help, anorexia treatment, tip 1: understand this is not really about weight or food, tip 2: learn to tolerate your feelings, tip 3: challenge damaging mindsets, tip 4: develop a healthier relationship with food, helping someone with anorexia, anorexia nervosa: symptoms, causes, and treatment.
Are you or a loved one struggling with anorexia? Explore the warning signs, symptoms, and causes of this serious eating disorder—as well as how to get the help you need.
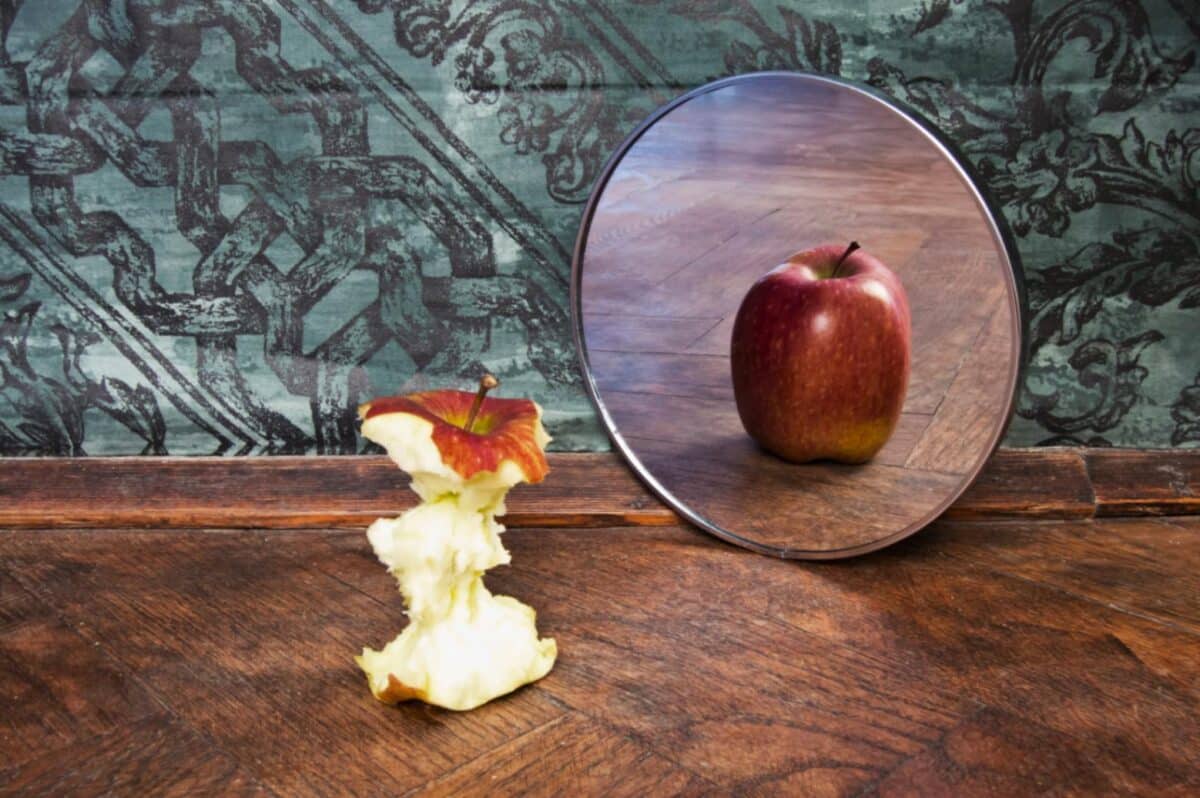
Anorexia nervosa is a serious eating disorder characterized by a refusal to maintain a healthy body weight, an intense fear of gaining weight, and a distorted body image. Anorexia can result in unhealthy, often dangerous weight loss. In fact, the desire to lose weight may become more important than anything else. You may even lose the ability to see yourself as you truly are.
While it is most common among adolescent women, anorexia can affect women and men of all ages. You may try to lose weight by starving yourself, exercising excessively, or using laxatives, vomiting, or other methods to purge yourself after eating. Thoughts about dieting, food, and your body may take up most of your day—leaving little time for friends, family, and other activities you used to enjoy. Life becomes a relentless pursuit of thinness and intense weight loss. But no matter how skinny you become, it’s never enough.
The intense dread of gaining weight or disgust with how your body looks, can make eating and mealtimes very stressful. And yet, food and what you can and can’t eat is practically all you can think about.
But no matter how ingrained this self-destructive pattern seems, there is hope. With treatment, self-help, and support, you can break the self-destructive hold anorexia has over you, develop a more realistic body image, and regain your health and self-confidence.
There are three types of anorexia:
- Restricting type of anorexia is where your weight loss is achieved by restricting calories (following drastic diets, fasting, exercising to excess).
- Purging type of anorexia is where your weight loss is achieved by vomiting or using laxatives and diuretics.
- Atypical anorexia is where you have all the symptoms and dangerous obsessions of anorexia, except you’re not underweight (often due to your genetic makeup). Even though you may still be in a healthy weight range, your dieting or exercise habits put severe stress on your body.
Ask yourself the following questions:
- Do you feel fat even though people tell you you’re not?
- Are you terrified of gaining weight?
- Do you lie about how much you eat or hide your eating habits from others?
- Are your friends or family concerned about your weight loss, eating habits, or appearance?
- Do you diet, compulsively exercise, or purge when you’re feeling overwhelmed or bad about yourself?
- Do you feel powerful or in control when you go without food, over-exercise, or purge?
- Do you base your self-worth on your weight or body size?
Speak to a Licensed Therapist
BetterHelp is an online therapy service that matches you to licensed, accredited therapists who can help with depression, anxiety, relationships, and more. Take the assessment and get matched with a therapist in as little as 48 hours.
While people with anorexia often exhibit different habits, one constant is that living with anorexia means you’re constantly hiding those habits. This can make it hard at first for friends and family to spot the warning signs. When confronted, you might try to explain away your disordered eating and wave away concerns. But as anorexia progresses, people close to you won’t be able to deny their instincts that something is wrong—and neither should you. If eating and weight control your life, you don’t have to wait until your symptoms have progressed or your health is dangerously poor before seeking help.
Food behavior symptoms
Dieting despite being thin. Following a severely restricted diet. Eating only certain low-calorie foods. Banning “bad” foods such as carbohydrates and fats.
Obsession with calories, fat grams, and nutrition. Reading food labels, measuring and weighing portions, keeping a food diary, reading diet books.
Pretending to eat or lying about eating. Hiding, playing with, or throwing away food to avoid eating. Making excuses to get out of meals (“I had a huge lunch” or “My stomach isn’t feeling good”).
Preoccupation with food. Constantly thinking about food. Cooking for others, collecting recipes, reading food magazines, or making meal plans while eating very little.
Strange or secretive food rituals. Refusing to eat around others or in public places. Eating in rigid, ritualistic ways (e.g. cutting food “just so,” chewing food and spitting it out, using a specific plate).
Appearance and body image symptoms
Dramatic weight loss. Rapid, drastic weight loss with no medical cause.
Feeling fat, despite being underweight. You may feel overweight in general or just “too fat” in certain places, such as the stomach, hips, or thighs.
Fixation on body image. Obsessed with weight, body shape, or clothing size. Frequent weigh-ins and concern over tiny fluctuations in weight.
Harshly critical of appearance. Spending a lot of time in front of the mirror checking for flaws. There’s always something to criticize. You’re never thin enough.
[Read: Body Shaming: Causes, Effects, and Improving Your Body Image]
Denial that you’re too thin. You may deny that your low body weight is a problem, while trying to conceal it (drinking a lot of water before being weighed, wearing baggy or oversized clothes).
Purging symptoms
Using diet pills, laxatives, or diuretics. Abusing water pills, herbal appetite suppressants, prescription stimulants, ipecac syrup, and other drugs for weight loss.
Throwing up after eating. Frequently disappearing after meals or going to the bathroom. May run the water to disguise sounds of vomiting or reappear smelling like mouthwash or mints.
Compulsive exercising. Following a punishing exercise regimen aimed at burning calories. Exercising through injuries, illness, and bad weather. Working out extra hard after bingeing or eating something “bad.”
There are no simple answers to the causes of anorexia. Anorexia is a complex condition that arises from a combination of many social, emotional, and biological factors. Although our culture’s idealization of thinness plays a powerful role, there are many other contributing factors, including your family environment, emotional difficulties, low self-esteem, and traumatic experiences you may have gone through in the past.
Psychological causes . People with anorexia are often perfectionists and overachievers. They tend to be the “good” daughters and sons who do what they’re told, excel in everything they do, and focus on pleasing others. But while they may appear to have it all together, inside they feel helpless, inadequate, and worthless. Through their harshly critical lens, if they’re not perfect, they’re a total failure.
Family and social pressures . In addition to the cultural pressure to be thin, there are other family and social pressures that can contribute to anorexia. These include participation in an activity that demands slenderness, such as ballet, gymnastics, or modeling. It can also include having parents who are overly controlling, put a lot of emphasis on looks, diet themselves, or criticize their children’s bodies and appearance. Stressful life events—such as the onset of puberty, a breakup, or going away to school—can also trigger anorexia.
Biological causes . Research suggests that a genetic predisposition to anorexia may run in families. If a girl has a sibling with anorexia, she is 10 to 20 times more likely than the general population to develop anorexia herself. Brain chemistry also plays a significant role. People with anorexia tend to have high levels of cortisol, the brain hormone most related to stress, and decreased levels of serotonin and norepinephrine, which are associated with feelings of well-being.
Risk factors for anorexia
- Body dissatisfaction
- Strict dieting
- Low self-esteem
- Emotional difficulties
- Perfectionism
- Troubled family relationships
- History of physical or sexual abuse
- Other traumatic experiences
- Family history of eating disorders
While the causes of anorexia are uncertain, the physical effects are clear. When your body doesn’t get the fuel it needs to function normally, it goes into starvation mode and slows down to conserve energy. Essentially, your body begins to consume itself. If self-starvation continues and more body fat is lost, medical complications pile up and your body and mind pay the price.
Source: National Women’s Health Information Center
Deciding to get help for anorexia is not an easy choice to make. It’s not uncommon to feel like anorexia is part of your identity—or even your “friend.” You may think that anorexia has such a powerful hold over you that you’ll never be able to overcome it. But while change is hard, it is possible.
Admit you have a problem. Up until now, you’ve been invested in the idea that life will improve—that you’ll finally feel good—if you lose more weight. The first step in anorexia recovery is admitting that your relentless pursuit of thinness is out of your control and acknowledging the physical and emotional damage that you’ve suffered because of it.
Talk to someone. It can be hard to talk about what you’re going through, especially if you’ve kept your anorexia a secret for a long time. You may be ashamed, ambivalent, or afraid. But it’s important to understand that you’re not alone. Find a good listener—someone who will support you as you try to heal.
Stay away from people, places, and activities that trigger your obsession with being thin. You may need to avoid looking at fashion or fitness magazines, spend less time with friends who constantly diet and talk about losing weight, and stay away from weight loss websites and “pro-ana” sites that promote anorexia.
Seek treatment from trained eating disorder professionals.
Treating anorexia involves three steps:
- Getting back to a healthy weight.
- Starting to eat more food.
- Changing how you think about yourself and food.
[Read: Eating Disorder Treatment and Recovery]
Medical treatment . The first priority in anorexia treatment is addressing and stabilizing any serious health issues. Hospitalization may be necessary if you are dangerously malnourished or so distressed that you no longer want to live. You may also need to be hospitalized until you reach a less critical weight. Outpatient treatment is an option when you’re not in immediate medical danger.
Nutritional treatment . A second component of anorexia treatment is nutritional counseling. A nutritionist or dietician will teach you about healthy eating and proper nutrition. The nutritionist will also help you develop and follow meal plans that include enough calories to reach or maintain a normal, healthy weight.
Therapy . Therapy is crucial to anorexia treatment. Its goal is to identify the negative thoughts and feelings that fuel your eating disorder and replace them with healthier, less distorted beliefs. Therapy can also help you deal with difficult emotions, relationship problems, and stress in a productive, rather than a self-destructive, way.
Along with professional treatment, the following tips can guide you on the road to recovery:
The food and weight-related issues are in fact symptoms of a deeper issue: depression, anxiety, loneliness, insecurity, pressure to be perfect, or feeling out of control. Problems that no amount of dieting or weight loss can cure.
The difference between dieting and anorexia
| Healthy Dieting | Anorexia |
|---|---|
| Healthy dieting is an attempt to control weight. | Anorexia is an attempt to control your life and emotions. |
| Your self-esteem is based on more than just weight and body image. | Your self-esteem is based entirely on how much you weigh and how thin you are. |
| You view weight loss as a way to improve your health and appearance. | You view weight loss as a way to achieve happiness. |
| Your goal is to lose weight in a healthy way. | Becoming thin is all that matters; health is not a concern. |
In order to overcome anorexia, you first need to understand that it meets a need in your life. For example, maybe you feel powerless in many parts of your life, but you can control what you eat. Saying “no” to food, getting the best of hunger, and controlling the number on the scale may make you feel strong and successful—at least for a short while. You may even come to enjoy your hunger pangs as reminders of a “special talent” that most people don’t possess.
Anorexia may also be a way of distracting yourself from difficult emotions. When you spend most of your time thinking about food, dieting, and weight loss, you don’t have to face other problems in your life or deal with complicated emotions. Restricting food may provide an emotional numbness, anesthetizing you from feelings of anxiety, sadness, or anger, perhaps even replacing those emotions with a sense of calm or safety.
Unfortunately, any boost you get from starving yourself or shedding pounds is extremely short-lived—and at some point, it will stop working for you at all. Dieting and weight loss can’t repair the negative self-image at the heart of anorexia. The only way to do that is to identify the emotional need that self-starvation fulfills and find other ways to meet it.
“I feel fat”
While your weight usually remains quite constant over the course of, say, a week, feelings of fatness can fluctuate wildly. Often, feeling fat is a mislabeling of other emotions, such as shame, boredom, frustration, or sadness. In other words, “I feel fat” really means “I feel anxious,” or “I feel lonely.” And those feelings are unlikely to ever be changed by a diet.
Identifying the underlying issues that drive your eating disorder is the first step toward recovery, but insight alone is not enough. Let’s say, for example, that following restrictive food rules makes you feel safe and powerful. When you take that coping mechanism away, you will be confronted with the feelings of fear and helplessness your anorexia helped you avoid.
Reconnecting with your feelings can be extremely uncomfortable. It’s why you may feel worse at the beginning of your recovery. But the answer isn’t to return to the destructive eating habits you previously used to distract yourself; it’s to learn how to accept and tolerate all of your feelings—even the negative ones.
Using mindfulness to cope with difficult emotions
When you start to feel overwhelmed by negativity, discomfort, or the urge to restrict food, take a moment to stop whatever you’re doing and investigate what’s going on inside.
Identify the emotion you’re feeling. Is it guilt? Shame? Helplessness? Loneliness? Anxiety? Disappointment? Fear? Insecurity?
Accept the experience you’re having. Avoidance and resistance only make negative emotions stronger. Instead, try to accept what you’re feeling without judging yourself.
Dig deeper. Where do you feel the emotion in your body? What kinds of thoughts are going through your head?
Distance yourself. Realize that you are NOT your feelings. Emotions are passing events, like clouds moving across the sky. They don’t define who you are.
Once you learn how to accept and tolerate your feelings, they’ll no longer seem so scary. You’ll realize that you’re still in control and that negative emotions are only temporary. Once you stop fighting them, they’ll quickly pass.
For a step-by-step guide to learning how to manage stress and uncomfortable emotions, check out HelpGuide’s free Emotional Intelligence Toolkit .
New ways to find emotional fulfillment
Once you understand the link between your emotions and your disordered eating patterns—and can identify your triggers—you still need to find alternatives to dieting that you can turn to for emotional fulfillment. For example:
If you’re depressed or lonely, call someone who always makes you feel better, schedule time with family or friends, watch a comedy show, or play with a dog or cat.
If you’re anxious, expend your nervous energy by dancing to your favorite music, squeezing a stress ball, or taking a brisk walk or bike ride.
If you’re exhausted, treat yourself with a hot cup of tea, go for a walk, take a bath, or light some scented candles.
If you’re bored, read a good book, explore the outdoors, visit a museum, or turn to a hobby you enjoy (playing the guitar, knitting, shooting hoops, scrapbooking, etc.).
People with anorexia are often perfectionists and overachievers. They’re the “good” daughters and sons who do what they’re told, try to excel in everything they do, and focus on pleasing others. But while they may appear to have it all together, inside they feel helpless, inadequate, and worthless.
If that sounds familiar to you, here’s the good news: these feelings don’t reflect reality. They’re fueled by irrational, self-sabotaging ways of thinking that you can learn to overcome.
Damaging mindsets that fuel anorexia
All-or-nothing thinking. Through this harshly critical lens, if you’re not perfect, you’re a total failure. You have a hard time seeing shades of gray, at least when it comes to yourself.
Emotional reasoning. You believe if you feel a certain way, it must be true. “I feel fat” means “I am fat.” “I feel hopeless” means you’ll never get better.
Musts, must-nots, and have-tos . You hold yourself to a rigid set of rules ( “I must not eat more than x number of calories , “ “I have to get straight A’s,” “ I must always be in control.” etc.) and beat yourself up if you break them.
Labeling. You call yourself names based on mistakes and perceived shortcomings. “I’m unhappy with how I look” becomes “I’m disgusting.” Slipping up becomes “I’m a “failure.”
Catastrophizing. You jump to the worst-case scenario. If you backslide in recovery, for example, you assume that there’s no hope you’ll ever get better.
Put your thoughts on the witness stand
Once you identify the destructive thoughts patterns that you default to, you can start to challenge them with questions such as:
- “What’s the evidence that this thought is true? Not true?”
- “What would I tell a friend who had this thought?”
- “Is there another way of looking at the situation or an alternate explanation?”
- “How might I look at this situation if I didn’t have anorexia?”
As you cross-examine your negative thoughts, you may be surprised at how quickly they crumble. In the process, you’ll develop a more balanced perspective.
Even though anorexia isn’t fundamentally about food, over time you’ve developed harmful food habits that can be tough to break. Developing a healthier relationship with food entails:
- Getting back to a healthy weight
- Starting to eat more food
- Changing how you think about yourself and food
Let go of rigid food rules. While following rigid rules may help you feel in control, it’s a temporary illusion. The truth is that these rules are controlling you, not the other way around. In order to get better, you’ll need to let go. This is a big change that will feel scary at first, but day by day, it will get easier.
Get back in touch with your body. If you have anorexia, you’ve learned to ignore your body’s hunger and fullness signals. You may not even recognize them anymore. The goal is to get back in touch with these internal cues, so you can eat based on your physiological needs.
Allow yourself to eat all foods. Instead of putting certain food off limits, eat whatever you want, but pay attention to how you feel physically after eating different foods. Ideally, what you eat should leave you feeling satisfied and energized.
Get rid of your scale. Instead of focusing on weight as a measurement of self-worth, focus on how you feel. Make health and vitality your goal, not a number on the scale.
Develop a healthy meal plan. If you need to gain weight, a nutritionist or dietician can help you develop a healthy meal plan that includes enough calories to get you back to a normal weight. While you can do this on your own, you’re probably out of touch with what a normal meal or serving size looks like.
Getting past your fear of gaining weight
Getting back to a normal weight is no easy task. The thought of gaining weight is probably extremely frightening, and you may be tempted to resist.
But this fear is a symptom of your anorexia. Reading about anorexia or talking to other people who have lived with it can help. It also helps to be honest about your feelings and fears. The better your family and treatment team understand what you’re going through, the better support you’ll receive.
Having anorexia can distort the way your loved one thinks—about their body, the world around them, even your motivations for trying to help. Add to that the defensiveness and denial involved in anorexia and you’ll need to tread lightly.
Waving around articles about the dire effects of anorexia or declaring, “you’ll die if you don’t eat!” probably won’t work. A better approach is to gently express your concerns and let the person know that you’re available to listen. If your loved one is willing to talk, listen without judgment, no matter how out of touch the person sounds.
[Read: Helping Someone with an Eating Disorder]
Think of yourself as an “outsider.” As someone not suffering from anorexia, there isn’t a lot you can do to “solve” your loved one’s condition. It is ultimately their choice to decide when they are ready.
Encourage your loved one to get help. The longer an eating disorder remains undiagnosed and untreated, the harder it is on the body and the more difficult it is to overcome.
Seek advice from a health professional, even if your friend or family member won’t. And you can bring others—from peers to parents—into the circle of support.
Be a role model for healthy eating, exercising, and body image. Don’t make negative comments about your own body or anyone else’s.
Don’t act like the food police. A person with anorexia needs compassion and support, not an authority figure standing over the table with a calorie counter.
Avoid threats, scare tactics, angry outbursts, and put-downs. Anorexia is often a symptom of extreme emotional distress and develops out of an attempt to manage emotional pain, stress, and/or self-hate. Negative communication will only make it worse.
Hotlines and support
National Eating Disorders Association or call 1-800-931-2237 (National Eating Disorders Association)
Beat Eating Disorders or call 0345 643 1414 (Helpfinder)
Butterfly Foundation for Eating Disorders or call 1800 33 4673 (National Eating Disorders Collaboration)
Service Provider Directory or call 1-866-633-4220 (NEDIC)
More Information
- Almost Anorexic – Is My (or My Loved One’s) Relationship with Food a Problem? - (Harvard Health Books)
- Treatment - Tips on eating disorder treatment. (National Eating Disorders Association)
- Anorexia nervosa - FAQs on anorexia and its treatment. (Office on Women’s Health)
- Anorexia Nervosa - Includes risk factors such as body image, self esteem, and perfectionism. (Eating Disorders Victoria)
- Feeding and Eating Disorders. (2013). In Diagnostic and Statistical Manual of Mental Disorders. American Psychiatric Association. Link
- Anorexia nervosa | Office on Women’s Health. (n.d.). Retrieved July 27, 2022, from Link
- Anorexia Nervosa—Psychiatric Disorders—Merck Manuals Professional Edition. (n.d.). Retrieved July 27, 2022, from Link
- Anorexia Nervosa—StatPearls—NCBI Bookshelf. (n.d.). Retrieved July 27, 2022, from Link
- Lloyd, S., Yiend, J., Schmidt, U., & Tchanturia, K. (2014). Perfectionism in Anorexia Nervosa: Novel Performance Based Evidence. PLoS ONE, 9 (10), e111697. Link
- Moskowitz, Lindsay, and Eric Weiselberg. “Anorexia Nervosa/Atypical Anorexia Nervosa.” Current Problems in Pediatric and Adolescent Health Care 47, no. 4 (April 1, 2017): 70–84. Link
- Harrington, Brian C., Michelle Jimerson, Christina Haxton, and David C. Jimerson. “Initial Evaluation, Diagnosis, and Treatment of Anorexia Nervosa and Bulimia Nervosa.” American Family Physician 91, no. 1 (January 1, 2015): 46–52. Link
- National Eating Disorders Association. “Anorexia Nervosa,” March 31, 2023. Link
- Tozzi, Federica, Patrick F. Sullivan, Jennifer L. Fear, Jan McKenzie, and Cynthia M. Bulik. “Causes and Recovery in Anorexia Nervosa: The Patient’s Perspective.” International Journal of Eating Disorders 33, no. 2 (2003): 143–54. Link
- Woerwag-Mehta, Sabine, and Janet Treasure. “Causes of Anorexia Nervosa.” Psychiatry , Eating disorders, 7, no. 4 (April 1, 2008): 147–51. Link
- Fairburn, C. G., Z. Cooper, H. A. Doll, and S. L. Welch. “Risk Factors for Anorexia Nervosa: Three Integrated Case-Control Comparisons.” Archives of General Psychiatry 56, no. 5 (May 1999): 468–76. Link
- Zipfel, Stephan, Katrin E Giel, Cynthia M Bulik, Phillipa Hay, and Ulrike Schmidt. “Anorexia Nervosa: Aetiology, Assessment, and Treatment.” The Lancet Psychiatry 2, no. 12 (December 1, 2015): 1099–1111. Link
More in Eating Disorders
How to overcome your eating disorder and gain true self-confidence

Bulimia Nervosa
Signs, symptoms, treatment and self-help tips

Advice for parents, family members and friends offering support

Orthorexia Nervosa
How to recognize if your healthy eating has gone too far

Symptoms, treatment and help for compulsive overeating

Body Shaming
Improving your body image and achieving body acceptance

Cognitive Behavioral Therapy (CBT)
How it can help with anxiety, depression, PTSD, substance abuse, and more

Always focusing on your physical flaws? You may have BDD.

Professional therapy, done online
BetterHelp makes starting therapy easy. Take the assessment and get matched with a professional, licensed therapist.
Help us help others
Millions of readers rely on HelpGuide.org for free, evidence-based resources to understand and navigate mental health challenges. Please donate today to help us save, support, and change lives.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Case study: anorexia nervosa and autistic disorder in an adolescent girl
Affiliation.
- 1 Division of Child and Adolescent Psychiatry, Children's Hospital of Western Ontario, London, Canada.
- PMID: 8768355
- DOI: 10.1097/00004583-199607000-00021
The development of anorexia nervosa in a high-functioning, early adolescent, autistic female is described. This case raises the issue of co-occurrence of childhood-onset disorders sharing the phenomena of obsessions and compulsions. The role of dysregulation of the serotonergic neurotransmitter system as a common underlying mechanism in these disorders is suggested. Psychoactive agents affecting the serotonin system and in particular the atypical neuroleptic risperidone may be of value in these disorders. There is added benefit to the combined use of biological and behavioral therapies.
PubMed Disclaimer
Similar articles
- Is anorexia nervosa a neuropsychiatric developmental disorder? An illustrative case report. Kerbeshian J, Burd L. Kerbeshian J, et al. World J Biol Psychiatry. 2009;10(4 Pt 2):648-57. doi: 10.1080/15622970802043117. World J Biol Psychiatry. 2009. PMID: 18609437
- [Anorexia nervosa and depression--a case study]. Herpertz-Dahlmann B. Herpertz-Dahlmann B. Z Kinder Jugendpsychiatr. 1987;15(3):198-207. Z Kinder Jugendpsychiatr. 1987. PMID: 3687240 German.
- Risperidone in anorexia nervosa. Newman-Toker J. Newman-Toker J. J Am Acad Child Adolesc Psychiatry. 2000 Aug;39(8):941-2. doi: 10.1097/00004583-200008000-00002. J Am Acad Child Adolesc Psychiatry. 2000. PMID: 10939220 No abstract available.
- Psychopharmacology in the treatment of anorexia nervosa and bulimia nervosa. Hoffman L, Halmi K. Hoffman L, et al. Psychiatr Clin North Am. 1993 Dec;16(4):767-78. Psychiatr Clin North Am. 1993. PMID: 7906029 Review.
- [Adolescent eating disorders]. Herpertz-Dahlmann B, Hagenah U, Vloet T, Holtkamp K. Herpertz-Dahlmann B, et al. Prax Kinderpsychol Kinderpsychiatr. 2005 Apr;54(4):248-67. Prax Kinderpsychol Kinderpsychiatr. 2005. PMID: 15918539 Review. German.
- Antipsychotics in the Treatment of Children and Adolescents with Anorexia Nervosa: A Systematic Review. Pruccoli J, Bergonzini L, La Tempa A, Parmeggiani A. Pruccoli J, et al. Biomedicines. 2022 Dec 7;10(12):3167. doi: 10.3390/biomedicines10123167. Biomedicines. 2022. PMID: 36551922 Free PMC article. Review.
- Canadian practice guidelines for the treatment of children and adolescents with eating disorders. Couturier J, Isserlin L, Norris M, Spettigue W, Brouwers M, Kimber M, McVey G, Webb C, Findlay S, Bhatnagar N, Snelgrove N, Ritsma A, Preskow W, Miller C, Coelho J, Boachie A, Steinegger C, Loewen R, Loewen T, Waite E, Ford C, Bourret K, Gusella J, Geller J, LaFrance A, LeClerc A, Scarborough J, Grewal S, Jericho M, Dimitropoulos G, Pilon D. Couturier J, et al. J Eat Disord. 2020 Feb 1;8:4. doi: 10.1186/s40337-020-0277-8. eCollection 2020. J Eat Disord. 2020. PMID: 32021688 Free PMC article. Review.
- Autism Spectrum Disorder in Anorexia Nervosa: An Updated Literature Review. Westwood H, Tchanturia K. Westwood H, et al. Curr Psychiatry Rep. 2017 Jul;19(7):41. doi: 10.1007/s11920-017-0791-9. Curr Psychiatry Rep. 2017. PMID: 28540593 Free PMC article. Review.
- Early-onset anorexia nervosa in girls with Asperger syndrome. Dudova I, Kocourkova J, Koutek J. Dudova I, et al. Neuropsychiatr Dis Treat. 2015 Jul 2;11:1639-43. doi: 10.2147/NDT.S83831. eCollection 2015. Neuropsychiatr Dis Treat. 2015. PMID: 26170676 Free PMC article.
- Potential therapeutic use of the ketogenic diet in autism spectrum disorders. Napoli E, Dueñas N, Giulivi C. Napoli E, et al. Front Pediatr. 2014 Jun 30;2:69. doi: 10.3389/fped.2014.00069. eCollection 2014. Front Pediatr. 2014. PMID: 25072037 Free PMC article. Review.
Publication types
- Search in MeSH
Related information
- Cited in Books
- PubChem Compound (MeSH Keyword)
LinkOut - more resources
Full text sources.
- Elsevier Science
- Ovid Technologies, Inc.
Other Literature Sources
- The Lens - Patent Citations
- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Lippincott Open Access
Incidence, prevalence and mortality of anorexia nervosa and bulimia nervosa
Annelies e. van eeden.
a Parnassia Psychiatric Institute, The Hague, The Netherlands
b University of Groningen, University Medical Center Groningen, Department of Psychiatry, Groningen, The Netherlands
Daphne van Hoeken
Hans w. hoek.
c Columbia University, Mailman School of Public Health, Department of Epidemiology, New York, New York, USA
Purpose of review
To review the recent literature on the epidemiology of anorexia nervosa and bulimia nervosa in terms of incidence, prevalence and mortality.
Recent findings
Although the overall incidence rate of anorexia nervosa is considerably stable over the past decades, the incidence among younger persons (aged <15 years) has increased. It is unclear whether this reflects earlier detection or earlier age of onset. Nevertheless, it has implications for future research into risk factors and for prevention programs. For bulimia nervosa, there has been a decline in overall incidence rate over time. The lifetime prevalence rates of anorexia nervosa might be up to 4% among females and 0.3% among males. Regarding bulimia nervosa, up to 3% of females and more than 1% of males suffer from this disorder during their lifetime. While epidemiological studies in the past mainly focused on young females from Western countries, anorexia nervosa and bulimia nervosa are reported worldwide among males and females from all ages. Both eating disorders may carry a five or more times increased mortality risk.
Anorexia nervosa and bulimia nervosa occur worldwide among females and males of all age groups and are associated with an increased mortality risk.
INTRODUCTION
This review aims to provide an overview of the recently published studies on the epidemiology of anorexia nervosa and bulimia nervosa. It is an update of previous reviews on this subject in this journal [ 1 – 3 ]. For a review of the epidemiology of binge eating disorder, see Keski-Rahkonen in this issue [ 4 ].

no caption available
Epidemiological studies provide information about the distribution (who, when and where) of disorders in a defined population and its trends over time. For eating disorders, there are some methodological problems regarding epidemiological research. Eating disorders are relatively rare in the community and help seeking is often avoided or delayed, for example for reasons of denial (particularly in anorexia nervosa) or stigma and shame (particularly in bulimia nervosa). These factors make general population studies on eating disorders costly and ineffective. Several strategies have been used to beat this problem, in particular the use of psychiatric case registers and other medical record-based studies. We must bear in mind that the results of these studies are an underestimation of the occurrence of eating disorders in the community, because not all patients will seek help, will be detected by their general practitioner or be referred to healthcare services. Moreover, different rates over time could be due to different case detection systems and diagnostic criteria, increased awareness leading to earlier detection and referral, and broader availability of treatment facilities, instead of a true increase in occurrence [ 1 , 5 ].
To review the literature, we searched for articles published in English using Medline/PubMed , Embase, PsycINFO and Google Scholar, using several key terms relating to epidemiology, anorexia nervosa and bulimia nervosa. We also checked the reference lists of the articles that we found for any additional articles missed by the database search.
Incidence is the number of new cases of a disorder in a population over a specified period of time (usually 1 year). The incidence rate of eating disorders is commonly expressed per 100 000 persons per year (100 000 person-years). The study of newly developed cases of an eating disorder provides clues to unravel its etiology [ 6 ]. It is noteworthy that healthcare register-based incidence rates represent the situation at the moment of detection, which is likely to be later than the moment of disorder onset.
Incidence of anorexia nervosa
Martinez-Gonzalez et al. [ 7 ▪ ] conducted a systematic review and meta-analysis of 31 published studies from 1980 to 2019 on the incidence of anorexia nervosa in females, mainly from Western countries. The incidence rates varied widely depending on the methodology, population and diagnostic criteria used. They reported on the incidence rates of only three population-based studies: 120 per 100 000 person-years among Swedish females aged 20–32 years [ 8 ], 200 per 100 000 person-years among Spanish females between the age of 12 and 22 years [ 9 ] and 270 per 100 000 person-years in Finnish twin females aged 15–19 years [ 10 ]. The pooled incidence rate of studies based on outpatient healthcare services (8.8 per 100 000 person-years; 95% confidence interval, CI: 7.8–9.8) was higher than that of hospital admissions (5.0; 95% CI 4.9–5.1) [ 7 ▪ ]. Compared to these all-age rates, the pooled incidence rates were higher for females aged 10–29 years, both in outpatient healthcare services [63.7 per 100 000 person-years (95% CI 61.2–66.1)] and in hospital admissions [8.1 (95% CI 7.6–8.5)] [ 7 ▪ ]. Furthermore, for healthcare register-based studies the incidence rates of anorexia nervosa showed a significant increase over time, especially in outpatient healthcare services. This does not necessarily mean a true increase in the occurrence of anorexia nervosa, as it could represent improved public awareness, detection and treatment rates over time.
Few studies have examined the incidence of anorexia nervosa in the general population; a limitation also encountered in the systematic review by Martinez-Gonzalez et al. [ 7 ▪ ]. The most recent study by Silen et al. [ 11 ▪ ] assessed the incidence rate of anorexia nervosa between the ages of 10 and 20 years according to the Diagnostic and Statistical Manual of Mental Disorders 5th Ed. (DSM-5) criteria in Finnish twins born between 1983 and 1987, yielding an incidence rate of anorexia nervosa of 320 (95% CI 230–440) per 100 000 person-years in the total group, 580 (95% CI 430–810) per 100 000 person-years among females and 30 (95% CI 10–310) per 100 000 person-years among males. These rates are higher than the rates in females described by Martinez-Gonzalez et al. [ 7 ▪ ]. This might be due to the use of the ‘broader’ DSM-5 criteria for anorexia nervosa by Silen et al. [ 11 ▪ ], and to the fact that twins may share genetic and environmental risk factors for anorexia nervosa, leading to a potential overestimation.
Population-based incidence rates are much higher than those derived from primary care and healthcare facilities, reflecting the selection filters on the pathways to (psychiatric) care [ 5 ]. Studies in general practices present incidence rates at the earliest stage of detection within the healthcare system. There have been no recent publications on all age groups in primary care since the previous review in this journal [ 1 ], that included a Dutch primary care study [ 12 ] which examined new cases with anorexia nervosa in a large representative sample of the Dutch population. The overall incidence rate of anorexia nervosa in Dutch females and males of all ages in primary care was fairly constant during three decades: in 1985–1989 it was 7.4 (95% CI 5.6–9.7) per 100 000 person-years, in 1995–1999 7.8 (95% CI 6.0–10.1) and in 2005–2009 6.0 (95% CI 4.3–8.1) [ 12 ]. Although no new studies have been published on incidence rates of anorexia nervosa in the total primary care population, Wood et al. [ 13 ▪ ] investigated 11- to 24-year-olds in England and found stable incidence rates between 2004 and 2014 (27.4 per 100 000 person-years; 95% CI 26.0–29.0). Demmler et al. [ 14 ] studied the incidence rate of eating disorders (all combined) in general practices in the UK since 2008, and reported a slight decline. The authors ascribe this finding to a decreasing trend in incidence of bulimia nervosa and a stable level of anorexia nervosa incidence, but they did not report rates per eating disorder diagnosis. Another primary care study among 10- to 19-year-olds in the UK reported an increased incidence rate in the age group of 13–16 years for all eating disorders combined, comparing 2018 rates to those in 2003 [ 15 ]. It is unclear whether this reflects a true increase in incidence or a shifting in age at detection.
The study of Reas and Ro [ 16 ▪ ], which was included in the meta-analysis by Martinez-Gonzalez et al. [ 7 ▪ ], described recent time trends in the incidence of anorexia nervosa in persons aged 10–49 years, using secondary care data of the Norwegian National Patient Register. The overall incidence rates for males and females combined were stable (differences nonsignificant) from 2010 to 2016, both for narrowly defined anorexia nervosa (18.8–20.4 per 100 000 person-years) and for broadly defined anorexia nervosa (33.2–39.5 per 100 000 person-years). They were also stable per sex for narrowly defined anorexia nervosa: in females 36.3–42.3 per 100 000 person-years, and in males 2.2–4.0 per 100 000 person-years; and for broadly defined anorexia nervosa: in females 63.3–79.1 per 100 000 person-years, and in males 4.4–5.9 per 100 000 person-years. The male to female ratio was found to be 1 : 13 for narrowly defined anorexia nervosa and 1 : 14 for broadly defined anorexia nervosa. This is in accordance with other studies showing considerably lower incidence rates for males, usually by more than a factor of 10, in comparison to females [ 11 ▪ , 12 ]. The incidence of anorexia nervosa according to DSM-5 criteria in 8- to 17-year-olds was examined in secondary care services in the UK and Ireland [ 17 ]. The overall incidence rate was 13.7 (95% CI 12.9–14.5) per 100 000 person-years; in females it was 25.7 (95% CI 24.1–27.3) and in males 2.3 (95% CI 1.8–2.8).
In females, the highest incidence rate of anorexia nervosa is around the age of 15 [ 11 ▪ , 12 , 17 ]. Several studies report a remarkable increase in the incidence of anorexia nervosa among girls aged 10–14 years [ 16 ▪ , 17 ]. Although most research has been performed in young females, some studies report incident anorexia nervosa cases in later life as well [ 12 , 16 ▪ ]. It is noteworthy that the peri-menopausal period has been suggested as another high-risk period in female life for the onset or recurrence of eating disorders [ 18 , 19 ]. In males, findings regarding the peak period of anorexia nervosa onset are less clear. While some studies have shown comparable [ 11 ▪ ] or a somewhat higher (age 16) peak age of onset [ 17 ], others found lower peak ages of 12–13 years [ 20 ] in comparison to females.
In summary, recent studies on time trends show fairly stable incidence rates for anorexia nervosa in the last decades [ 12 , 16 ▪ ], although some healthcare register-based studies suggest an increase in the incidence of anorexia nervosa [ 7 ▪ ], which might be explained by greater public awareness, better detection and the use of broader diagnostic criteria. Incidence rates in males are found to be lower, usually by more than a factor 10, in comparison to females [ 11 ▪ , 16 ▪ ]. The rates in males should be interpreted as an underestimation because of underdetection due to a double stigma: the stigma of having a psychiatric disorder, and an additional stigma of suffering from a ‘female-specific’ disorder [ 21 ]. Finally, the finding that the incidence of anorexia nervosa is increasing in younger girls (<15 years) has important implications for future research into risk factors [ 22 ], the development of prevention programs for younger subjects, and the planning of healthcare services.
Incidence of bulimia nervosa
Few studies have investigated the incidence of bulimia nervosa. In the population cohort study of Finnish twins born in the 1980 s, the incidence rate of DSM-5 bulimia nervosa between 10 and 20 years of age was 100 (95% CI 60–190) per 100 000 person-years overall, and 180 (95% CI 110–340) per 100 000 person-years in females [ 11 ▪ ]. These population-based DSM-5 rates of bulimia nervosa are higher than DSM-IV rates for females aged 10–19 years identified in Dutch primary care (range 20.5–22.0 per 100 000 person-years) [ 12 ], partly because of the use of broader DSM-5 criteria in the Finnish study [ 11 ▪ ], but moreover because of the fact that only a small proportion of community ‘cases’ present to (primary) care [ 3 , 5 ]. It is of note that the Finnish study [ 11 ▪ ] investigated the incidence rate between 10 and 20 years of age, which only partly covers the peak age period of 15 to 29 years suggested by other studies [ 12 , 16 ▪ ].
The Dutch primary care study showed a significant decrease in the all-age incidence rate of bulimia nervosa according to DSM-IV criteria over three decades: in 1985–1989 it was 8.6 (95% CI 6.7–11.0), in 1995–1999 6.1 (95% CI 4.5–8.2) and in 2005–2009 3.2 (95% CI 2.0–4.9) per 100 000 person-years [ 12 ]. The English primary care study in 11- to 24-year-olds also showed a significant decline in the incidence rate of bulimia nervosa between 2004 and 2014 (incidence rate ratio: 0.5; 95% CI 0.3–0.7) [ 13 ▪ ]. Also, Demmler et al. [ 14 ] explained their all-age finding of a slight decrease in the incidence rate of all eating disorders combined in primary care to a declining trend in incidence of bulimia nervosa.
Findings of the Norwegian National Patient Register study [ 16 ▪ ] support a significant decline in overall incidence rates of bulimia nervosa in secondary care between 2010 and 2016, both in narrowly defined bulimia nervosa [2010: 18.5 per 100 000 person-years (95% CI 16.9–20.2); 2016: 16.1 (95% CI 14.6–17.2)] and in broadly defined bulimia nervosa (2010: 29.4 per 100 000 person-years (95% CI 27.4–31.5); 2016: 26.9 (95% CI 24.9–28.8). A significant decrease in incidence rates was found in all age groups, except for a trend of an increase among girls aged 10–14 years, suggesting a shift to earlier ages of onset or detection. The peak incidence was among females aged 20–29 years. In males, the incidence rates were low and stable over time, ranging between 0.9 and 1.6 for narrowly defined bulimia nervosa, and ranging between 1.7 and 2.5 for broadly defined bulimia nervosa. The male to female ratio was found to be 1 : 24 for narrowly defined bulimia nervosa and 1 : 26 for broadly defined bulimia nervosa. Incident cases of bulimia nervosa also occur in later life [ 12 , 16 ▪ ].
In conclusion, there is a decline in incidence rates of bulimia nervosa over time. The peak age of incidence ranged between 15 and 29 years. Studies of incidence in males are scarce, but the rates are found to be much lower than in females.
Incidence of anorexia nervosa and bulimia nervosa in non-Western countries
Most epidemiological studies on eating disorders have been conducted in Western countries. Although studies assessing the epidemiology of eating disorders in non-Western countries are still scarce, we will highlight the most recent findings. Two Taiwanese studies [ 23 ▪ , 24 ] used national health insurance claim data to investigate the epidemiology of eating disorders between 2001 and 2013 in 10- to 49-year-old persons. In comparison to Western countries, the overall anorexia nervosa incidence rate in Taiwan is very low (1.1–1.3 per 100 000 person-years), but stable over time. Regarding bulimia nervosa, the incidence rates in Taiwan among females increased in the years up to 2009 [21.6 (95% CI 17.8–25.4) per 100 000 person-years] and then decreased [16.3 (95% CI 12.8–19.8) per 100 000 person-years] [ 24 ], following the trend in changes in incidence of Western countries, although a decade later. The incidence in Taiwan differs from that in Western countries in terms of older age at detection of anorexia nervosa and bulimia nervosa (20–29 years) and an increase in incidence among adults rather than adolescents [ 23 ▪ , 24 ]. This last finding aligns with findings of increasing numbers of persons in midlife with incident eating disorders in Western countries [ 19 ].
A study using data and methodology from the Global Burden of Disease (GBD) Study 2017 [ 25 ] reported increasing incidence rates of anorexia nervosa and bulimia nervosa from 1990 to 2017 in China, which is in contrast with the stable (anorexia nervosa) and decreasing (bulimia nervosa) rates in Western countries, but in line with the general trend of an increase in rates in all psychiatric diagnoses in China. Because of methodological issues related to the low prevalence and lack of global coverage of epidemiological studies for eating disorders, GBD calculations on these data must be interpreted with caution [ 26 , 27 ]. In this case [ 25 ], study results were difficult to check because 15 of the 39 publications from which data were included had been published in Chinese. From the abstracts of the included studies it would appear that in at least 26 of the 39 publications no formal eating disorder diagnosis had been applied, and that none of the studies addressed incidence. This casts doubts on the validity of the findings.
Prevalence is the proportion of cases in a population present at a certain point or interval in time. The point prevalence is the prevalence at a specific date (point) in time. The 12-month prevalence is the prevalence over an interval of a year. The lifetime prevalence is the proportion of the population that has had the disorder at any moment in life up to the moment of registration. In general, lifetime prevalence rates are higher than point and 12-month prevalence rates, especially when assessed in older populations. Prevalence indicates the demand for care and is therefore useful in the planning of healthcare facilities. Many studies have assessed the prevalence of anorexia nervosa and bulimia nervosa. In this review, we focus on recently published systematic reviews and meta-analyses, supplemented by recently published population-based studies that have not been included in the described reviews and meta-analyses.
Prevalence of anorexia nervosa
Galmiche et al. [ 28 ] have performed an extensive systematic review of 94 studies published between 2000 and 2018 that addressed the prevalence of formally diagnosed eating disorders in the general population. They explained the high variability of prevalence rates by the use of different diagnostic instruments [most commonly used: Structured Clinical Interview for DSM (13%), Composite International Diagnostic Interview (12%) and Eating Disorder Examination (11%)], diagnostic criteria [DSM-IV (78%), DSM-5 (14%) and DSM-III-R (4%)] and clinical investigation methods [face-to-face interview (51%), paper-and-pencil questionnaire (27%) or online or by telephone (22%)]. Weighted means were constructed from the prevalence rates and the population size of each study included, but were most likely not stratified for age. No confidence intervals were provided, only minimum-maximum ranges of the prevalence rates. The authors themselves conclude that the small number of studies makes it difficult to estimate weighted mean sex ratios. These limitations hamper the interpretation of some findings that are at odds with previous literature, in particular for point prevalence and 12-month prevalence rates. We therefore reproduce only the ranges of lifetime prevalence rates of anorexia nervosa, which were 0.1% to 3.6% in females and 0% to 0.3% in males.
Another systematic review and meta-analysis by Qian et al. [ 29 ] included 33 studies published between 1990 and 2020 on the prevalence of anorexia nervosa in the population. All studies combined, an overall lifetime prevalence rate of 0.2% (95% CI 0.06–0.3) was found. In studies applying DSM-5 criteria (18%; all in Western countries) a higher overall lifetime prevalence rate was found [0.9% (95% CI 0.7–1.1)]. This is in line with previous research showing an increase in anorexia nervosa prevalence rates when applying DSM-5 criteria, in comparison to rates according to DSM-IV criteria [ 30 , 31 ]. Lifetime prevalence rates in males and females (Table (Table1) 1 ) were in the lower range of the rates described in the review of Galmiche et al. [ 28 ]. This could be explained by a large proportion of studies that had been conducted in Asia (40%) with very large sample sizes and much lower rates compared to Western countries, and the broader period studied (1984–2017) with especially lower prevalence rates before 2000 [ 29 ]. That is in contrast to findings described in a previous review in this journal [ 1 ] and to the notion that anorexia nervosa rates in Asian countries have been increasing in recent years and that they currently appear to be comparable to, or even higher than, those in Western countries [ 32 – 34 ]. In the review by Qian et al. [ 29 ], 6 of the 33 studies included had been published in Chinese and so the results were difficult to evaluate. However, there seems to be a lack of population-based studies using formal diagnostic interviews and applying DSM (-III-R, -IV, or -5) or International Classification of Diseases 10th Ed. (ICD-10) criteria. In Asia ‘non fat-phobic’ presentations of anorexia nervosa are common. In the DSM-5 the possibility of ‘persistent behaviour that interferes with weight gain’, which would apply to nonfat phobic presentations, is added to the DSM-IV B-criterium ‘intense fear of gaining weight or becoming fat’. Thus, the replacement of DSM-IV by DSM-5 criteria for anorexia nervosa will ultimately lead to higher rates among Asian people.
Overview of recently published studies on prevalence rates. Studies are grouped by design and listed in chronological order
| Study | Country | Study time | Age | Type of study | Criteria | Prevalence | Anorexia Nervosa | Bulimia Nervosa | |
| Lindvall Dahlgren ., 2017 [ ] | Worldwide | 2012-2017 | 19 studies Range 496–22,397 | 11 and older | Two-stage design studies | DSM-5 | Lifetime | ♀ 1.7–3.6% ♂ 0.1% (1 study) | NR |
| Point | ♀ 0.7–1.2% ♂ 0.1% (1 study) | ♀ 0.6% (2 studies) | |||||||
| Interview-based studies | DSM-5 | Lifetime | ♀ 0.8–1.9% | ♀ 2.6% (1 study) | |||||
| Self-report studies | DSM-5 | Point | ♀ 0.06–1.2% | ♀ 0.5–8.7% | |||||
| Galmiche 2019 [ ] | Worldwide | 2000-2018 | 94 studies Range 111–248,558 | 8 and older | Systematic review | DSM-III-R DSM-IV DSM-5 | Lifetime | ♀ 0.1–3.6% ♂ 0–0.3% | ♀ 0.3–4.6% ♂ 0.1–1.3% |
| Qian ., 2021 [ ] | Worldwide | 1984-2017 | 33 studies 315,877 | 15 and older | Systematic review and meta-analysis | DSM-III DSM-III-R DSM-IV DSM-5 ICD-10 | Lifetime | ♀ 0.6% (95% CI 0.3–1.1) ♂ 0.04% (95%CI 0.01–0.1) | ♀ 1.2% (95% CI 0.7–1.9) ♂ 0.4% (95%CI 0.2–0.7) |
| DSM-5 | Lifetime | 0.9% (95%CI 0.7–1.1) | 1.4% (95%CI 0.0–6.3) | ||||||
| DSM-III DSM-III-R DSM-IV DSM-5 ICD-10 | 12-month | ♀ 0.03% (95%CI 0.0–0.06) ♂ 0.01% (95%CI 0.0–0.02) | ♀ 0.3% (95%CI 0.1–0.6) ♂ 0.09% (95%CI 0.02–0.2) | ||||||
| DSM-5 | 12-month | 0.04% (95%CI 0.02–0.06) | 0.1% (1 study) | ||||||
| Micali ., 2017 [ ] | UK | 2009-2012 | 5,658 | Mean: 47.8 (SD 4.5) | Two-stage design | DSM-5 | Lifetime | ♀ 3.6% (95%CI 2.8–4.7) | ♀ 2.2% (95%CI 1.7–2.7) |
| 12-month | ♀ 0.2% (95%CI 0.2–0.5) | ♀ 0.4% (95%CI 0.2–0.7) | |||||||
| Hay ., 2017 [ ] | Australia | 2014-2015 | 5,737 | 15 and older | Interview-based | DSM-5 | 3-month | 0.4–0.5% | 1.1–1.2% |
| Udo and Grilo, 2018 [ ] | USA | 2012-2013 | 36,306 | 18 and older | Interview-based | DSM-5 | Lifetime | ♀ 1.4% (SE 0.1) ♂ 0.1% (SE 0.04) | ♀ 0.5% (SE 0.06) ♂ 0.08% (SE 0.03) |
| 12-month | ♀ 0.08% (SE 0.03) ♂ 0.01% (SE 0.01) | ♀ 0.2% (SE 0.05) ♂ 0.05% (SE 0.02) | |||||||
| Chen ., 2019 [ ] | Taiwan | 2015-2017 | 4,816 | 7-14 | Interview-based | DSM-5 | Lifetime | 0.2% (95%CI 0.0–0.4) | NR |
| 6-month | 0.2% (95%CI 0.0–0.4) | NR | |||||||
| Mohammadi ., 2020 [ ] | Iran | 2016-2018 | 27,111 | 6-18 | Interview-based | DSM-5 | Lifetime | ♀ 0.1% (95%CI 0.06–0.2) | ♀ 0.1% (95%CI 0.07–0.2) ♂ 0.02% (95%CI 0.01–0.08) |
| Silen 2020 [ ] | Finland | 2006-2009 | 1,347 | Mean 22.4 (SD 0.7) | Interview-based | DSM-5 | Lifetime | ♀ 6.2% (95%CI 4.6–8.3) ♂ 0.3% (95%CI 0.08–1.3) | ♀ 2.4% (95%CI 1.5–3.9) ♂ 0.2% (95%CI 0.02–1.1) |
| Bagaric ., 2020 [ ] | Australia | 2017 | 2,977 | Mean 53.9 (SD 19.1) | Interview-based | DSM-5 | Lifetime | NR | ♀ 2.6% (95%CI 2.1–3.2) ♂ 1.2% (95%CI 0.9–1.7) |
| Point | NR | ♀ 0.8% (95%CI 0.5–1.2) ♂ 0.4% (95%CI 0.2–0.7) | |||||||
| Ernst ., 2017 [ ] | Germany | 2009 | 1,654 | Mean: 13.4 (SD 5.8) | Self-report | DSM-5 | Point | 0.3% (95%CI 0.1–0.7) | 0.4% (95%CI 0.2–0.8) |
| Glazer ., 2019 [ ] | USA | 1996-2013 | 9,031 | Mean at baseline: 11.6 (SD 1.6) | Self-report | DSM-5 | Lifetime | ♀ 1.6% | ♀ 2.1% |
| Mitchison ., 2020 [ ] | Australia | 2017 | 5,191 | 11-19 | Self-report | DSM-5 | Point | ♀ 1.3% ♂ 0.0% | ♀ 7.7% ♂ 1.8% |
CI, confidence interval; NR, not reported; SD, standard deviation; SE, standard error.
In their systematic review, Lindvall Dahlgren, Wisting and Ro [ 35 ] focused specifically on the prevalence of DSM-5 defined anorexia nervosa in the general population. Nineteen studies published until 2017 were included. Lifetime prevalence rates for anorexia nervosa in females differed according to the study method; 1.7–3.6% in studies with two-stage design and 0.8–1.9% in interview-based studies. Point prevalence rates in females ranged from 0.06% to 1.2%, predominantly assessed with self-reports.
Since this systematic review [ 35 ], several studies [ 11 ▪ , 36 ▪▪ , 37 , 38 ▪ , 39 – 43 ] have been published that investigated prevalence according to DSM-5 criteria. The prevalence rates reported in these recent studies are shown in Table Table1 1 and are largely in line with those reported in the review. However, the population-based study of Finnish twins born in the 1980 s [ 11 ▪ ], in which the whole sample was diagnostically interviewed, found higher lifetime prevalence rates for anorexia nervosa: 6.2% (95% CI 4.6–8.3) in females and 0.3% (95% CI 0.08–1.3) in males. Suggested explanations for the higher rate found among females were the twin nature of the study, the thorough anorexia nervosa assessment and Finnish socio-cultural characteristics favouring a drive for thinness. Only 55% of the females identified with anorexia nervosa in the study reported that they had been diagnosed in real life by a healthcare professional.
Although epidemiological studies have mainly focused on the traditionally known high-risk group of young females, it has been shown in recent years that anorexia nervosa is prevalent among older persons as well [ 18 , 19 ]. The highest lifetime prevalence rates are found in adults, because of the accumulation of anorexia nervosa first emerging in the peak age period of adolescence [ 44 ] combined with incidence later in adulthood. A longitudinal, population-based study among Polish males showed that anorexia nervosa was prevalent in all age groups (10–80 + years) [ 45 ]. Although a decrease in point prevalence among females over a 30-year follow-up period was found, with no anorexia nervosa cases by age 50 [ 46 ▪ ], the 12-month prevalence rate in 40- to 50-year-old females was still 0.2% in another study [ 36 ▪▪ ].
Prevalence of bulimia nervosa
The three previously discussed systematic reviews and meta-analyses [ 28 , 29 , 35 ] also reported prevalence rates for bulimia nervosa. The lifetime prevalence rates for bulimia nervosa ranged from 0.3% to 4.6% in females and from 0.1% to 1.3% in males in the extensive systematic review by Galmiche et al. [ 28 ]. As discussed previously, we refrain from reproducing the 12-month and point prevalence rates they report for methodological reasons.
Qian et al. [ 29 ] reported an overall lifetime prevalence rate for bulimia nervosa of 0.6% (95% CI 0.3–1.0). This review included a relatively large (40%) proportion of Asian studies. For bulimia nervosa the lifetime prevalence in Western countries was 7.3 times higher than that in Asian countries. The lifetime prevalence rates in females and males (Table (Table1) 1 ) were close to the rates described by Galmiche et al. [ 28 ]. The pooled overall lifetime prevalence rate rose up to 1.4% (95% CI 0.0–6.3), when using only studies that applied DSM-5 criteria (18%; all in Western countries) [ 29 ]. Other studies supported this increase [ 30 , 31 ], which could be explained by the lower required frequency of binge eating and compensatory behaviour in DSM-5 compared to DSM-IV.
Lindvall Dahlgren et al. included only studies that had applied DSM-5 criteria and found few studies on bulimia nervosa, but the authors reported preliminary evidence for an increase in bulimia nervosa prevalence [ 35 ]. Two two-stage studies reported a point prevalence rate of 0.6% in females [ 30 , 48 ]. The lifetime prevalence rate was found to be 2.6% among females in one interview-based study [ 49 ]. In self-report studies, point prevalence rates ranged from 0.5% to 8.7% in females.
Since these systematic reviews, several studies on the prevalence of DSM-5 defined bulimia nervosa [ 11 ▪ , 36 ▪▪ , 37 , 38 ▪ , 40 – 43 , 47 ▪▪ ] have been published in recent years. Among females, lifetime prevalence rates around 2.3% (range 2.1–2.6%) were consistently found [ 11 ▪ , 36 ▪▪ , 42 , 47 ▪▪ ], which gives further support for an increase in bulimia nervosa prevalence since the introduction of DSM-5 criteria. Only one study in a large population-based sample of US adults [ 38 ▪ ] reported a substantially lower lifetime prevalence rate [0.5% (Standard Error 0.06)] in females. Possible explanations for this low rate are the use of lay interviewers rather than clinicians and the use of a questionnaire that has not been validated for eating disorder diagnoses. The combination of these factors could lead to underreporting, especially in the case of bulimia nervosa where stigma and shame around bingeing and purging play an important role.
Few recent studies reported on prevalence in males. The results were in the same order as found in the systematic reviews [ 28 , 29 ], with lifetime prevalence rates ranging between 0.1% and 1.2% [ 11 ▪ , 38 ▪ , 47 ▪▪ ]. In males like in females [ 36 ▪▪ , 46 ▪ ], bulimia nervosa does occur in all age groups up to the age of 80, although the prevalence declines after age 30 [ 45 ].
The preliminary evidence for an increase in prevalence of bulimia nervosa in population-based studies is noteworthy in the face of decreasing incidence rates in primary and secondary care. One possible explanation is that people who have a lower frequency of binge eating and compensatory behaviour (meeting DSM-5 but not DSM-IV criteria, i.e. once a week) seek help less often than those who have this behaviour more often, and thus are less often included in care-based studies. Future research is needed to clarify this apparent discrepancy.
Mortality could be described as an incidence rate in which the event being measured is death. The crude mortality rate (CMR) is the number of deaths within the study population over a specified period. The standardized mortality ratio (SMR) is the ratio of observed deaths in the study population versus that of expected deaths in the population of origin. For comparison reasons the SMR is preferred, because the CMR is not standardized for age and sex. Mortality is often used as an indicator of the severity of a disorder.
In a previous review in this journal [ 27 ], it has been reported that both anorexia nervosa and bulimia nervosa were associated with significantly increased mortality rates. In comparison to age-matched and sex-matched people in the general population, the mortality risk was around two times higher in people followed up after outpatient treatment for anorexia nervosa, or after any treatment for bulimia nervosa. In people followed up after inpatient treatment for anorexia nervosa, the mortality risk was even over five times higher. Since this previous review, a few new studies have been published.
In a landmark meta-analysis of worldwide eating disorder mortality rates by Arcelus et al. [ 50 ] the CMR of anorexia nervosa patients was 5.1 deaths per 1000 person-years (95% CI 4.0–6.1). The SMR was 5.9 (95% CI 4.2–8.3), i.e. an almost 6 times increased risk. In a recent study, after 5 years follow-up the SMR of anorexia nervosa inpatients with (complications of) severe malnutrition was found to be as high as 15.9 (95% CI 11.6–21.4) [ 51 ]. This study population was probably more severely affected than most of the study populations included in the meta-analysis [ 50 ]. For bulimia nervosa, Arcelus et al. reported a CMR of 1.7 per 1000 person-years (95% CI 1.1–2.4) and a SMR of 1.9 (95% CI 1.4–2.6) [ 50 ]. Recently, in a large 12-year follow-up study a higher mortality risk was found in females after inpatient treatment for bulimia nervosa compared to similar-age females hospitalized for pregnancy-related events [adjusted hazard ratio 4.7 (95% CI 2.1–10.8)] [ 52 ]. This difference could be even larger when compared to the general population. Iwajomo et al. investigated mortality after hospitalization for an eating disorder (anorexia nervosa, bulimia nervosa or eating disorder not otherwise specified) in a Canadian population-based cohort [ 53 ▪ ]. Although results were not presented for each eating disorder separately, the total SMR was five times higher compared to the general population [SMR 5.1 (95% CI 4.8–5.3)]. Rates were higher for males [SMR 7.2 (95% CI 6.6–8.0)] compared to females [SMR 4.6 (95% CI 4.3–4.9)]. This is in line with other recent studies that also found higher mortality rates among males: in people treated for bulimia nervosa in secondary mental healthcare services an overall SMR of 2.5 (95% CI 1.5–4.0) was reported, with significantly higher rates among males compared to females [crude hazard ratio 5.4 (95% CI 1.8–16.5)] [ 54 ]. In another study on hospitalization for anorexia nervosa, in-hospital mortality in males was more than twice that for females [odds ratio 2.4 (95% CI 1.5–3.8)] [ 55 ]. However, in a study directly comparing males and females from the same hospital, from the same treatment period and for the same follow-up period, no significant differences in SMR were found for anorexia nervosa or for bulimia nervosa [ 56 ▪ ], which might be due to the relatively small sample size of males. The SMRs for each sex-group [ 57 , 58 ] have already been described in the previous review [ 27 ]. While there were no significant differences in mortality rates, males with anorexia nervosa or bulimia nervosa did die sooner in comparison to females with anorexia nervosa or bulimia nervosa [ 56 ▪ ].
In summary, recent findings accentuate high mortality rates for anorexia nervosa and bulimia nervosa, with highest rates among those who received inpatient treatment for anorexia nervosa. Although results are still inconclusive, the suggestion that males have a probably higher mortality risk than females underscores the clinical relevance of detecting and treating anorexia nervosa and bulimia nervosa in males.
Anorexia nervosa and bulimia nervosa occur among females and males of all age groups worldwide and are associated with an increased mortality risk. The trend of a decreasing peak age at incidence has implications for future research into risk factors, the development of earlier prevention programs and planning of treatment services. Besides the well-known risk group of young females from Western countries, the occurrence of anorexia nervosa and bulimia nervosa in males, older persons and non-Western countries highlights the need for further research in these groups. Moreover, improved awareness will lead to earlier detection and treatment in these groups that suffer from an extra stigma of a ‘young, Western, female-specific’ psychiatric disorder.
Acknowledgements
The authors would like to thank Judith Offringa for her editorial assistance.
Financial support and sponsorship
Conflicts of interest.
There are no conflicts of interest.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
- ▪ of special interest
- ▪▪ of outstanding interest

IMAGES
COMMENTS
Anorexia nervosa is a chronic eating disorder which primarily affects adolescent girls and young women. 1 The prevalence of anorexia nervosa varies between 0.1-1%. 1 Although the prevalence is low, the morbidity is high and the mortality varies between 0.1-25%. 2 Relapse is common and chances of recovery are less than 50% in 10 years while 25% ...
Abstract. Anorexia nervosa is an eating disorder characterized by excessive restriction on food intake and irrational fear of gaining weight, often accompanied by a distorted body self-perception. It is clinically diagnosed more frequently in females, with type and severity varying with each case. The current report is a case of a 25-year-old ...
Anorexia specific - for me, a big issue that caused most ethical debate was whether my case of anorexia nervosa was "reversible." Many physicians misunderstand SEAN (not even an official DSM diagnosis) and that while anorexia nervosa is a psychiatric illness, it comes with severe medical complications that ultimately are the reason for death.
There are limited community-based studies worldwide and all available published reports agree on the rare incidence of anorexia nervosa. 2 Most of the existing epidemiological studies on anorexia were conducted in Western countries. 7 In Africa including Ethiopia studies assessing anorexia nervosa are scarce. 7, 14 This case reflects a 23-year ...
In some young patients with anorexia nervosa, ... On the basis of previous case studies that suggested a benefit from gradual exposure to feared foods in patients with a choking phobia, 19,20 I ...
Anorexia Nervosa (AN) poses significant therapeutic challenges, especially in cases meeting the criteria for Severe and Enduring Anorexia Nervosa (SE-AN). This subset of AN is associated with severe medical complications, frequent use of services, and the highest mortality rate among psychiatric disorders. In the present case series, 14 patients were selected from those currently or previously ...
1. Introduction. Anorexia nervosa (AN) is a complex psychiatric disorder with a high rate of mortality and a relatively low rate of remission [].Using DSM-V criteria, the lifetime prevalence of AN in females is estimated to be as high as 4% [].The lifetime prevalence in males has been estimated to be between 0.1% and 0.3%, although this is likely an underestimate [].
The Clinical Problem. Anorexia nervosa is a severe psychiatric disorder that is characterized by starvation and malnutrition, a high incidence of coexisting psychiatric conditions, treatment ...
The case study suggests that it is possible to perform normally cognitively despite extreme and chronic malnutrition though set-shifting ability may be affected. This opens for discussion whether patients with anorexia nervosa can maintain neuropsychological performance in spite of extreme underweight and starvation. ClinicalTrials.gov ...
Abstract. Anorexia nervosa is an eating disorder characterized by excessive restriction on food intake and irrational fear of gaining weight, often accompanied by a distorted body self-perception. It is clinically diagnosed more frequently in females, with type and severity varying with each case. The current report is a case of a 25-year-old ...
A total of 119 study series covering 5,590 patients suffering from anorexia nervosa that were published in the English and German literature were analyzed with regard to mortality, global outcome ...
Epidemiology and prognosis. The peak age of onset of anorexia nervosa in both men and women is 15-19 years (Micali et al, 2013).A surveillance study of young people aged 8-17 years in the UK and Ireland found incidence rates of 13.68 per 100 000 population (95% confidence interval 12.88-14.52), with rates of 25.66 (95% confidence interval 24.09-27.30) for young women and 2.28 (95% ...
Background: Prospective, longitudinal studies of risk factors for anorexia nervosa (AN) are lacking and existing cross-sectional studies are generally narrow in focus and lack methodological rigor. Building on two studies that used the Oxford Risk Factor Interview (RFI) to establish time precedence and comprehensively assess potential risk correlates for AN, the present study advances this ...
Objective. The definition and assessment of remission in anorexia nervosa (AN) needs greater consensus. Particularly in adolescents, the use of patient-reported composite indices (such as the Eating Disorder Examination [EDE] Global Score) as the sole measure of psychological remission has the potential to obscure patients' true clinical status, given developmental factors and the propensity ...
Abstract. D.R., a single 19-year-old female experiencing anorexia nervosa, was admitted to a mental health center inpatient unit weighing 64 lb, approximately 54 lb underweight, with liver, kidney, and pancreas damage. D.R. was hospitalized for 59 days. Treatment consisted of utilizing a hierarchy of reinforcements in the form of privileges ...
The maudsley outpatient study of treatments for anorexia nervosa and related conditions (MOSAIC): comparison of the maudsley model of anorexia nervosa treatment for adults ... in the bed nucleus of the stria terminalis and medial forebrain bundle in a patient with major depressive disorder and anorexia nervosa. Clin Case Rep 2017; 5:679-684.
1. Introduction. Anorexia nervosa (AN) is a syndrome that is more prevalent in industrialized and western cultures; it is more prevalent among females than males and has a peak age of onset during adolescence [].AN appears to have gained more popularity and professional attention over recent decades during a cultural period that idealizes thinness, with magazines publishing significantly more ...
This case study involved the treatment of a young adult female, referred to as "Marie," who presented for treatment seeking help with her eating disorder. Marie evinced symptoms of dietary restriction, amenorrhea, low weight, and low body mass index (BMI); she was subsequently diagnosed with anorexia nervosa.
Case Study. At the time of hospitalization, D.R. was a 19-year-old, single, Caucasian female admit- ted with diagnoses of anorexia nervosa and phobic neuroses. The patient, although ambula-. tory, was extremely emaciated. D.R. 's weight was approximately 64 lb at the time of. admission, her height 5 ft 7 in. The patient had lost a total of 54 ...
MR, Durgoji S. Case report on anorexia nervosa. Indian J Psychol Med . 2015;37:236-8. ... up to 4% of females and up to 0.3% of males suffer from anorexia nervosa. Studies assessing AN in Africa ...
Anorexia nervosa is characterised by a significant loss of weight and a pathological desire to be thin. It is a difficult disorder to treat, which commonly lasts several years and in which constant relapses occur in a high percentage of cases [7,8]. This paper examines the treatment of a case of anorexia nervosa in an adolescent girl with CBT ...
CASE STuDY #130 ANOREXIA NERVOSA SCENARIO: You are a nurse on an inpatient psychiatric unit. J., a 23-year-old woman, was admitted to the psychiatric unit last night after assessment and treatment at a local hospital emergency department (ED) for "blacking out at school." She has been given a preliminary diagnosis of anorexia nervosa.
Anorexia nervosa is a serious eating disorder characterized by a refusal to maintain a healthy body weight, an intense fear of gaining weight, and a distorted body image. ... Fairburn, C. G., Z. Cooper, H. A. Doll, and S. L. Welch. "Risk Factors for Anorexia Nervosa: Three Integrated Case-Control Comparisons." Archives of General Psychiatry ...
Abstract. The development of anorexia nervosa in a high-functioning, early adolescent, autistic female is described. This case raises the issue of co-occurrence of childhood-onset disorders sharing the phenomena of obsessions and compulsions. The role of dysregulation of the serotonergic neurotransmitter system as a common underlying mechanism ...
Although most research has been performed in young females, some studies report incident anorexia nervosa cases in later life as well [12,16 ]. It is noteworthy that the peri-menopausal period has been suggested as another high-risk period in female life for the onset or recurrence of eating disorders [18,19]. In males, findings regarding the ...
Atypical anorexia nervosa is an eating disorder in which individuals meet all the qualifications for anorexia nervosa, ... than that of anorexia nervosa. [4] One study looked at the length of duration of individual episodes seen in patients and found atypical anorexia nervosa had an 11.2 month duration as compared to anorexia nervosa with an 8 ...