- Bipolar Disorder
- Therapy Center
- When To See a Therapist
- Types of Therapy
- Best Online Therapy
- Best Couples Therapy
- Best Family Therapy
- Managing Stress
- Sleep and Dreaming
- Understanding Emotions
- Self-Improvement
- Healthy Relationships
- Student Resources
- Personality Types
- Sweepstakes
- Guided Meditations
- Verywell Mind Insights
- 2024 Verywell Mind 25
- Mental Health in the Classroom
- Editorial Process
- Meet Our Review Board
- Crisis Support
- Signs of Burnout
- Stress and Weight Gain
- Stress Reduction Tips
- Self-Care Practices
- Mindful Living

How to Recognize Burnout Symptoms
What to do if your physically and emotionally burned out at work
Burnout vs. Depression
- Take the Burnout Quiz
- Risk Factors
- Prevention and Treatment
- Next in How Stress Impacts Your Health Guide How Stress Can Cause Weight Gain
Is your job making you exhausted? Does the thought of dragging yourself to work fill you with dread? Or have you reached the point where you just don't care about your job anymore? If so, you might be experiencing burnout—a type of work-related exhaustion that can bleed over into other areas of your life.
Burnout is a type of exhaustion that can happen when you face prolonged stress that eventually results in severe physical, mental, and emotional fatigue.
Excessive workplace stress for prolonged periods can lead to burnout. However, it can also happen in other areas of life where you face too much stress for too long, such as when dealing with caregiving, relationship, parenting, or financial challenges.
So, what does burnout look like, exactly? Symptoms of burnout include feeling exhausted, empty, and unable to cope with daily life. If left unaddressed, your burnout may even make it difficult to function. Keep reading to learn more about the physical and mental symptoms of burnout, factors that may increase your risk, and a few recovery strategies .
Signs You're Burning Out
Recognizing the signs can help you better understand whether the stress you are experiencing is impacting you in a negative way. Here are a few to look for:
- Gastrointestinal problems
- High blood pressure
- Poor immune function (getting sick more often)
- Reoccurring headaches
- Sleep issues
- Concentration issues
- Depressed mood
- Feeling worthless
- Loss of interest or pleasure
- Suicidal ideation
What Does Burnout Mean?
Burnout is a reaction to prolonged or chronic job stress . It is characterized by three main dimensions:
- exhaustion,
- cynicism (less identification with the job),
- and feelings of reduced professional ability.
More simply put, if you feel exhausted, start to hate your job , and begin to feel less capable at work, you are showing signs of burnout.
Most people spend the majority of their waking hours working. So, if you hate your job, dread going to work, and don't gain any satisfaction from what you're doing, it can take a serious toll on your life. This toll shows up via burnout symptoms.
The term “burnout” is a relatively new term, first coined in 1974 by Herbert Freudenberger in his book, "Burnout: The High Cost of High Achievement." Freudenberger defined burnout as "the extinction of motivation or incentive, especially where one's devotion to a cause or relationship fails to produce the desired results."
Symptoms You Might Be Experiencing Burnout
Burnout isn’t a diagnosable psychological disorder , but that doesn't mean it shouldn't be taken seriously. Burnout symptoms can affect you both physically and mentally. Feeling burned out can contribute to mental health conditions like anxiety and depression, and the ongoing stress you are experiencing can take a massive toll on both your physical and mental health.
Physical Burnout Symptoms
When you experience burnout, your body will often display certain signs. Research indicates that some of the most common physical burnout symptoms include:
Because burnout is caused by chronic stress, it's helpful to also be aware of how this stress, in general, affects the body. Having chronic stress in your life doesn't necessarily mean that you are experiencing burnout. Unaddressed chronic stress, however, can eventually lead to burnout.
Chronic stress may be felt physically in terms of having more aches and pains, low energy levels, and changes in appetite. All of these physical signs suggest that you may be experiencing burnout.
Health Risks of Burnout
Chronic stress is associated with a wide range of negative health complications and outcomes, including heart disease, weight changes, depression, high blood pressure, and irritable bowel syndrome. Researchers have also connected stress-related disorders to an increased risk of death.
Mental Burnout Symptoms
Burnout also impacts you mentally and emotionally. Here are some of the most common mental symptoms of burnout:
If you are having suicidal thoughts, contact the National Suicide Prevention Lifeline at 988 for support and assistance from a trained counselor. If you or a loved one are in immediate danger, call 911.
For more mental health resources, see our National Helpline Database .
Burnout shares symptoms with some mental health conditions, such as depression. Depression symptoms also include a loss of interest in things, feelings of hopelessness, cognitive and physical symptoms, as well as thoughts of suicide. How can you tell if what you are feeling is burnout versus depression?
The key differences center on where and when you experience symptoms. Burnout symptoms tend to be focused on work (or the specific challenge you're dealing with), while depression tends to affect all areas of your life.
If you are depressed, you'll experience negative feelings and thoughts about all aspects of life, not just at work.
If this is how you feel, a mental health professional can help. Seeking help is important because individuals experiencing burnout may be at a higher risk of developing depression .
Are You Feeling Burnt Out? Take the Quiz
Try our fast and free burnout quiz to find out if some of the things you've been feeling may be a sign of burnout.
Factors That Put You at Risk of Burnout
People who work in certain stressful professions sometimes have a higher risk of burning out, but having a high-stress job doesn't always lead to burnout. You may not experience these ill effects if your stress is managed well.
However, some individuals (and those in certain occupations) are at a higher risk of having burnout symptoms than others. It often comes down to how you manage your stress and the support you have in your life.
For instance, a 2019 National Physician Burnout, Depression, and Suicide Report found that 44% of physicians experience burnout. Of course, it's not just physicians who are burning out. Workers in every industry at every level are at potential risk.
According to a 2018 Gallup report, there are five job factors that can contribute to employee burnout :
- Unreasonable time pressures . Employees who say they have enough time to do their work are 70% less likely to experience high burnout, while individuals who are not able to gain more time (such as paramedics and firefighters ) are at a higher risk of burnout.
- Lack of communication and support from management . Manager support offers a psychological buffer against stress. Employees who feel strongly supported by their manager are 70% less likely to experience burnout symptoms on a regular basis.
- Lack of role clarity . Only 60% of workers know what is expected of them. When expectations are like moving targets, employees may become exhausted simply by trying to figure out what they are supposed to be doing.
- Unmanageable workload . When the workload feels unmanageable, even the most optimistic employees will feel hopeless . Feeling overwhelmed can quickly lead to burnout symptoms.
- Unfair treatment . Employees who feel they are treated unfairly at work are 2.3 times more likely to experience a high level of burnout. Unfair treatment may include things such as favoritism, unfair compensation, and mistreatment from a co-worker .
The stress that contributes to burnout can come mainly from your job, but stressors from other areas of life can add to these levels as well. For instance, personality traits and thought patterns such as perfectionism , neuroticism , and pessimism can contribute to the stress you feel.
Other Causes of Burnout
Other factors that can contribute to burnout include:
- Poor communication from your employer
- Lack of clarity about your role or duties
- Intense pressure and tight deadlines
- Feeling like you have no control over your life or work
- Being mistreated by your boss or coworkers
- Excessive workloads or expectations
- Working too long without enough time to rest
- Work that is overly boring or stressful
- Not getting enough sleep
- Lack of social support
- Lack of recognition for your efforts
- Poor work-life balance
Press Play for Advice On Dealing With a Toxic Workplace
Hosted by therapist Amy Morin, LCSW, this episode of The Verywell Mind Podcast , featuring business expert Heather Monahan, shares how to survive a toxic workplace. Click below to listen now.
Subscribe Now : Apple Podcasts / Spotify / Google Podcasts
Burnout Can Have Serious Effects
Chances are, you probably have a pretty good idea of whether you are burned out or not. So what happens if you don't take steps to address those feelings of exhaustion, disconnect, and distress? If left untreated, burnout symptoms can lead to:
You Might Feel Alienated From Your Work
Individuals experiencing burnout view their jobs as increasingly stressful and frustrating. You may grow cynical about your working conditions and the people you work with. You might also emotionally distance yourself and begin to feel numb about your work.
You May Become Emotionally Exhausted
Over time, untreated burnout symptoms can cause you to feel emotionally drained and unable to cope. You might find it harder and harder to deal with problems at work and at home. When you get home from work, you may be so fatigued that you don't have the physical or mental energy to engage in other activities that are part of your home life.
Your Performance at Work Can Suffer
Burnout affects everyday tasks at work, or in the home if your main job involves caring for family members . Individuals with burnout symptoms feel negative about tasks, have difficulty concentrating, and often lack creativity. Together, this results in reduced performance.
How to Prevent and Treat Burnout
Although the term "burnout" suggests that this may be a permanent condition, it is reversible. If you are feeling burned out , you may need to make some changes to your work environment.
How to Deal With Burnout
- Discuss work problems with your company's human resources department or your supervisor.
- Explore less stressful positions or tasks within your company.
- Take regular breaks.
- Learn meditation or other mindfulness techniques.
- Eat a healthy diet.
- Get plenty of exercise.
- Practice healthy sleep habits.
- Consider taking a vacation.
Approaching human resources about problems you're having or talking to a supervisor could be helpful if the company is invested in creating a healthier work environment. In some cases, a change in position or a new job altogether may be necessary to begin to recover from burnout. If you can't switch jobs, it may help to at least switch tasks .
It can also be helpful to develop clear strategies to help you manage your stress. Self-care strategies like eating a healthy diet, getting plenty of exercise, and engaging in healthy sleep habits may help reduce some of the effects of a high-stress job.
A vacation may offer you some temporary relief too, but a week away from the office won't be enough to help you beat burnout. Regularly scheduled breaks from work, along with daily renewal exercises, can be key to helping you combat burnout.
Social support is also critical. This can come from various sources, including coworkers, friends, family, and mental health professionals. If you are struggling to find the type of support you need, consider joining an in-person or online support group where you can talk about your challenges and get encouragement from people with the same type of experience.
If you are experiencing burnout and are having difficulty finding your way out, or you suspect that you may also have a mental health condition such as depression, seek professional treatment. Talking to a mental health professional can help you discover the strategies you need to feel your best.
Tileva A. How to douse chronic workplace stress before it explodes into full burnout . Society for Human Resource Management.
Maslach C, Leiter MP. Understanding the burnout experience: Recent research and its implications for psychiatry. World Psychiatry . 2016;15(2):103–111. doi:10.1002/wps.20311
Brandstätter V, Job V, Schulze B. Motivational incongruence and well-being at the workplace: person-job fit, job burnout, and physical symptoms . Front Psychol . 2016;7:1153. doi:10.3389/fpsyg.2016.01153
Yale Medicine. Chronic stress .
American Psychological Association. Stress effects on the body .
Tian F, Shen Q, Hu Y, et al. Association of stress-related disorders with subsequent risk of all-cause and cause-specific mortality: A population-based and sibling-controlled cohort study . The Lancet Regional Health - Europe . 2022;18:100402. doi:10.1016/j.lanepe.2022.100402
Pereira H, Feher G, Tibold A, Monteiro S, Esgalhado G. Mediating effect of burnout on the association between work-related quality of life and mental health symptoms . Brain Sci . 2021;11(6):813. doi:10.3390/brainsci11060813
Bianchi R, Schonfeld IS, Laurent E. Burnout-depression overlap: a review. Clin Psychol Rev. 2015;36:28-41. doi:10.1016/j.cpr.2015.01.004
Kane L. Medscape National Physician Burnout, Depression & Suicide Report 2019 .
Wigert B, Agrawal S. Employee burnout, Part 1: The 5 main causes . Gallup.
Wekenborg MK, Von dawans B, Hill LK, Thayer JF, Penz M, Kirschbaum C. Examining reactivity patterns in burnout and other indicators of chronic stress . Psychoneuroendocrinology. 2019;106:195-205. doi:10.1016/j.psyneuen.2019.04.002
Demerouti E. Strategies used by individuals to prevent burnout. Eur J Clin Invest. 2015;45(10):1106-12. doi:10.1111/eci.12494
By Elizabeth Scott, PhD Elizabeth Scott, PhD is an author, workshop leader, educator, and award-winning blogger on stress management, positive psychology, relationships, and emotional wellbeing.
Find anything you save across the site in your account
Burnout: Modern Affliction or Human Condition?

Burnout is generally said to date to 1973; at least, that’s around when it got its name. By the nineteen-eighties, everyone was burned out. In 1990, when the Princeton scholar Robert Fagles published a new English translation of the Iliad, he had Achilles tell Agamemnon that he doesn’t want people to think he’s “a worthless, burnt-out coward.” This expression, needless to say, was not in Homer’s original Greek. Still, the notion that people who fought in the Trojan War, in the twelfth or thirteenth century B.C., suffered from burnout is a good indication of the disorder’s claim to universality: people who write about burnout tend to argue that it exists everywhere and has existed forever, even if, somehow, it’s always getting worse. One Swiss psychotherapist, in a history of burnout published in 2013 that begins with the usual invocation of immediate emergency—“Burnout is increasingly serious and of widespread concern”—insists that he found it in the Old Testament. Moses was burned out, in Numbers 11:14, when he complained to God, “I am not able to bear all this people alone, because it is too heavy for me.” And so was Elijah, in 1 Kings 19, when he “went a day’s journey into the wilderness, and came and sat down under a juniper tree: and he requested for himself that he might die; and said, It is enough.”
To be burned out is to be used up, like a battery so depleted that it can’t be recharged. In people, unlike batteries, it is said to produce the defining symptoms of “burnout syndrome”: exhaustion, cynicism, and loss of efficacy. Around the world, three out of five workers say they’re burned out. A 2020 U.S. study put that figure at three in four. A recent book claims that burnout afflicts an entire generation. In “ Can’t Even: How Millennials Became the Burnout Generation ,” the former BuzzFeed News reporter Anne Helen Petersen figures herself as a “pile of embers.” The earth itself suffers from burnout. “Burned out people are going to continue burning up the planet,” Arianna Huffington warned this spring. Burnout is widely reported to have grown worse during the pandemic, according to splashy stories that have appeared on television and radio, up and down the Internet, and in most major newspapers and magazines, including Forbes , the Guardian , Nature , and the New Scientist . The New York Times solicited testimonials from readers. “I used to be able to send perfect emails in a minute or less,” one wrote. “Now it takes me days just to get the motivation to think of a response.” When an assignment to write this essay appeared in my in-box, I thought, Oh, God, I can’t do that, I’ve got nothing left, and then I told myself to buck up. The burnout literature will tell you that this, too—the guilt, the self-scolding—is a feature of burnout. If you think you’re burned out, you’re burned out, and if you don’t think you’re burned out you’re burned out. Everyone sits under the shade of that juniper tree, weeping, and whispering, “Enough.”
But what, exactly, is burnout? The World Health Organization recognized burnout syndrome in 2019, in the eleventh revision of the International Classification of Diseases, but only as an occupational phenomenon, not as a medical condition. In Sweden, you can go on sick leave for burnout. That’s probably harder to do in the United States because burnout is not recognized as a mental disorder by the DSM-5 , published in 2013, and though there’s a chance it could one day be added, many psychologists object, citing the idea’s vagueness. A number of studies suggest that burnout can’t be distinguished from depression, which doesn’t make it less horrible but does make it, as a clinical term, imprecise, redundant, and unnecessary.
To question burnout isn’t to deny the scale of suffering, or the many ravages of the pandemic: despair, bitterness, fatigue, boredom, loneliness, alienation, and grief—especially grief. To question burnout is to wonder what meaning so baggy an idea can possibly hold, and whether it can really help anyone shoulder hardship. Burnout is a metaphor disguised as a diagnosis. It suffers from two confusions: the particular with the general, and the clinical with the vernacular. If burnout is universal and eternal, it’s meaningless. If everyone is burned out, and always has been, burnout is just . . . the hell of life. But if burnout is a problem of fairly recent vintage—if it began when it was named, in the early nineteen-seventies—then it raises a historical question. What started it?
Herbert J. Freudenberger, the man who named burnout, was born in Frankfurt in 1926. By the time he was twelve, Nazis had torched the synagogue to which his family belonged. Using his father’s passport, Freudenberger fled Germany. Eventually, he made his way to New York; for a while, in his teens, he lived on the streets. He went to Brooklyn College, then trained as a psychoanalyst and completed a doctorate in psychology at N.Y.U. In the late nineteen-sixties, he became fascinated by the “free clinic” movement. The first free clinic in the country was founded in Haight-Ashbury, in 1967. “ ‘Free’ to the free clinic movement represents a philosophical concept rather than an economic term,” one of its founders wrote, and the community-based clinics served “alienated populations in the United States including hippies, commune dwellers, drug abusers, third world minorities, and other ‘outsiders’ who have been rejected by the more dominant culture.” Free clinics were free of judgment, and, for patients, free of the risk of legal action. Mostly staffed by volunteers, the clinics specialized in drug-abuse treatment, drug crisis intervention, and what they called “detoxification.” At the time, people in Haight-Ashbury talked about being “burnt out” by drug addiction: exhausted, emptied out, used up, with nothing left but despair and desperation. Freudenberger visited the Haight-Ashbury clinic in 1967 and 1968. In 1970, he started a free clinic at St. Marks Place, in New York. It was open in the evening from six to ten. Freudenberger worked all day in his own practice, as a therapist, for ten to twelve hours, and then went to the clinic, where he worked until midnight. “You start your second job when most people go home,” he wrote in 1973, “and you put a great deal of yourself in the work. . . . You feel a total sense of commitment . . . until you finally find yourself, as I did, in a state of exhaustion.”
Burnout, as the Brazilian psychologist Flávio Fontes has pointed out, began as a self-diagnosis, with Freudenberger borrowing the metaphor that drug users invented to describe their suffering to describe his own. In 1974, Freudenberger edited a special issue of the Journal of Social Issues dedicated to the free-clinic movement, and contributed an essay on “staff burn-out” (which, as Fontes noted, contains three footnotes, all to essays written by Freudenberger). Freudenberger describes something like the burnout that drug users experienced in his experience of treating them:
Having experienced this feeling state of burn-out myself, I began to ask myself a number of questions about it. First of all, what is burn-out? What are its signs, what type of personalities are more prone than others to its onslaught? Why is it such a common phenomenon among free clinic folk?
The first staff burnout victim, he explained, was often the clinic’s charismatic leader, who, like some drug addicts, was quick to anger, cried easily, and grew suspicious, then paranoid. “The burning out person may now believe that since he has been through it all, in the clinic,” Freudenberger wrote, “he can take chances that others can’t.” The person exhibits risk-taking that “sometimes borders on the lunatic.” He, too, uses drugs. “He may resort to an excessive use of tranquilizers and barbiturates. Or get into pot and hash quite heavily. He does this with the ‘self con’ that he needs the rest and is doing it to relax himself.”
The street term spread. To be a burnout in the nineteen-seventies, as anyone who went to high school in those years remembers, was to be the kind of kid who skipped class to smoke pot behind the parking lot. Meanwhile, Freudenberger extended the notion of “staff burnout” to staffs of all sorts. His papers, at the University of Akron, include a folder each on burnout among attorneys, child-care workers, dentists, librarians, medical professionals, ministers, middle-class women, nurses, parents, pharmacists, police and the military, secretaries, social workers, athletes, teachers, veterinarians. Everywhere he looked, Freudenberger found burnouts. “It’s better to burn out than to fade away,” Neil Young sang, in 1978, at a time when Freudenberger was popularizing the idea in interviews and preparing the first of his co-written self-help books. In “ Burn-out: The High Cost of High Achievement ,” in 1980, he extended the metaphor to the entire United States. “ WHY, AS A NATION, DO WE SEEM, BOTH COLLECTIVELY AND INDIVIDUALLY, TO BE IN THE THROES OF A FAST-SPREADING PHENOMENON—BURN-OUT? ”
Somehow, suddenly, burning out wasn’t any longer what happened to you when you had nothing, bent low, on skid row; it was what happened to you when you wanted everything. This made it an American problem, a yuppie problem, a badge of success. The press lapped up this story, filling the pages of newspapers and magazines with each new category of burned-out workers (“It used to be that just about every time we heard or read the word ‘burnout’ it was preceded by ‘teacher,’ ” read a 1981 story that warned about “homemakers burnout”), anecdotes (“Pat rolls over, hits the sleep button on her alarm clock and ignores the fact that it’s morning. . . . Pat is suffering from ‘burnout’ ”), lists of symptoms (“the farther down the list you go, the closer you are to burnout!”), rules (“Stop nurturing”), and quizzes:
Are you suffering from burnout? . . . Looking back over the past six months of your life at the office, at home and in social situations. . . . 1. Do you seem to be working harder and accomplishing less? 2. Do you tire more easily? 3. Do you often get the blues without apparent reason? 4. Do you forget appointments, deadlines, personal possessions? 5. Have you become increasingly irritable? 6. Have you grown more disappointed in the people around you? 7. Do you see close friends and family members less frequently? 8. Do you suffer physical symptoms like pains, headaches and lingering colds? 9. Do you find it hard to laugh when the joke is on you? 10. Do you have little to say to others? 11. Does sex seem more trouble than it’s worth?
You could mark questions with “X”s, cut out the quiz, and stick it on the fridge, or on the wall of your “Dilbert”-era cubicle. See? See? This says I need a break, goddammit.
Link copied
Sure, there were skeptics. “The new IN thing is ‘burnout,’ ” a Times-Picayune columnist wrote. “And if you don’t come down with it, possibly you’re a bum.” Even Freudenberger said he was burned out on burnout. Still, in 1985 he published a new book, “Women’s Burnout: How to Spot It, How to Reverse It, and How to Prevent It.” In the era of anti-feminist backlash chronicled by Susan Faludi, the press loved quoting Freudenberger saying things like “You can’t have it all.”
Freudenberger died in 1999 at the age of seventy-three. His obituary in the Times noted, “He worked 14 or 15 hours a day, six days a week, until three weeks before his death.” He had run himself ragged.
“Every age has its signature afflictions,” the Korean-born, Berlin-based philosopher Byung-Chul Han writes in “ The Burnout Society, ” first published in German in 2010. Burnout, for Han, is depression and exhaustion, “the sickness of a society that suffers from excessive positivity,” an “achievement society,” a yes-we-can world in which nothing is impossible, a world that requires people to strive to the point of self-destruction. “It reflects a humanity waging war on itself.”
Lost in the misty history of burnout is a truth about the patients treated at free clinics in the early seventies: many of them were Vietnam War veterans, addicted to heroin. The Haight-Ashbury clinic managed to stay open partly because it treated so many veterans that it received funding from the federal government. Those veterans were burned out on heroin. But they also suffered from what, for decades, had been called “combat fatigue” or “battle fatigue.” In 1980, when Freudenberger first reached a popular audience with his claims about “burnout syndrome,” the battle fatigue of Vietnam veterans was recognized by the DSM-III as post-traumatic stress disorder. Meanwhile, some groups, particularly feminists and other advocates for battered women and sexually abused children, were extending this understanding to people who had never seen combat.
Burnout, like P.T.S.D., moved from military to civilian life, as if everyone were, suddenly, suffering from battle fatigue. Since the late nineteen-seventies, the empirical study of burnout has been led by Christina Maslach, a social psychologist at the University of California, Berkeley. In 1981, she developed the field’s principal diagnostic tool, the Maslach Burnout Inventory, and the following year published “ Burnout: The Cost of Caring ,” which brought her research to a popular readership. “Burnout is a syndrome of emotional exhaustion, depersonalization, and reduced personal accomplishment that can occur among individuals who do ‘people work’ of some kind,” Maslach wrote then. She emphasized burnout in the “helping professions”: teaching, nursing, and social work—professions dominated by women who are almost always very poorly paid (people who, extending the military metaphor, are lately classed as frontline workers, alongside police, firefighters, and E.M.T.s). Taking care of vulnerable people and witnessing their anguish exacts an enormous toll and produces its own suffering. Naming that pain was meant to be a step toward alleviating it. But it hasn’t worked out that way, because the conditions of doing care work—the emotional drain, the hours, the thanklessness—have not gotten better.
Burnout continued to climb the occupational ladder. “Burnout cuts across executive and managerial levels,” Harvard Business Review reported in 1981, in an article that told the tale of a knackered executive: “Not only did the long hours and the unremitting pressure of walking a tightrope among conflicting interests exhaust him; they also made it impossible for him to get at the control problems that needed attention. . . . In short, he had ‘burned out.’ ” Burnout kept spreading. “College Presidents, Coaches, Working Mothers Say They’re Exhausted,” according to a Newsweek cover in 1995. With the emergence of the Web, people started talking about “digital burnout.” “Is the Internet Killing Us?” Elle asked in 2014, in an article on “how to deal with burnout.” (“Don’t answer/write emails in the middle of the night. . . . Watch your breath come in and out of your nostrils or your stomach contracting and expanding as you breathe.”) “Work hard and go home” is the motto at Slack, a company whose product, launched in 2014, made it even harder to stop working. Slack burns you out. Social media burns you out. Gig work burns you out. In “Can’t Even,” a book that started out as a viral BuzzFeed piece, Petersen argues, “Increasingly—and increasingly among millennials—burnout isn’t just a temporary affliction. It’s our contemporary condition.” And it’s a condition of the pandemic.
In March, Maslach and a colleague published a careful article in Harvard Business Review , in which they warned against using burnout as an umbrella term and expressed regret that its measurement has been put to uses for which it was never intended. “We never designed the MBI as a tool to diagnose an individual health problem,” they explained; instead, assessing burnout was meant to encourage employers to “establish healthier workplaces.”
The louder the talk about burnout, it appears, the greater the number of people who say they’re burned out: harried, depleted, and disconsolate. What can explain the astonishing rise and spread of this affliction? Declining church membership comes to mind. In 1985, seventy-one per cent of Americans belonged to a house of worship, which is about what that percentage had been since the nineteen-forties; in 2020, only forty-seven per cent of Americans belonged to an institution of faith. Many of the recommended ways to address burnout—wellness, mindfulness, and meditation (“Take time each day, even five minutes, to sit still,” Elle advised)—are secularized versions of prayer, Sabbath-keeping, and worship. If burnout has been around since the Trojan War, prayer, worship, and the Sabbath are what humans invented to alleviate it. But this explanation goes only so far, not least because the emergence of the prosperity gospel made American Christianity a religion of achievement. Much the same appears to apply to other faiths. A Web site called productivemuslim.com offers advice on “How to Counter Workplace Burnout” (“There is barakah in earning a halal income”). Also, actually praying, honoring the Sabbath, and attending worship services don’t seem to prevent people who are religious from burning out, since religious Web sites and magazines, too, are full of warnings about burnout, including for the clergy. (“The life of a church leader involves a high level of contact with other people. Often when the church leader is suffering high stress or burnout he or she will withdraw from relationships and fear public appearances.”)
You can suffer from marriage burnout and parent burnout and pandemic burnout partly because, although burnout is supposed to be mainly about working too much, people now talk about all sorts of things that aren’t work as if they were: you have to work on your marriage, work in your garden, work out, work harder on raising your kids, work on your relationship with God. (“Are You at Risk for Christian Burnout?” one Web site asks. You’ll know you are if you’re driving yourself too hard to become “an excellent Christian.”) Even getting a massage is “bodywork.”
Burnout may be our contemporary condition, but it has very particular historical origins. In the nineteen-seventies, when Freudenberger first started looking for burnout across occupations, real wages stagnated and union membership declined. Manufacturing jobs disappeared; service jobs grew. Some of these trends have lately begun to reverse, but all the talk about burnout, beginning in the past few decades, did nothing to solve these problems; instead, it turned responsibility for enormous economic and social upheaval and changes in the labor market back onto the individual worker. Petersen argues that this burden falls especially heavily on millennials, and she offers support for this claim, but a lesson of the history of burnout is that every generation of Americans who have come of age since the nineteen-seventies have made the same claim, and they were right, too, because overwork keeps getting worse . It’s this giant mess that Joe Biden is trying to fix. In earlier eras, when companies demanded long hours for low wages, workers engaged in collective bargaining and got better contracts. Starting in the nineteen-eighties, when companies demanded long hours for low wages, workers put newspaper clippings on the doors of their fridges, burnout checklists. Do you suffer from burnout? Here’s how to tell!
Burnout is a combat metaphor. In the conditions of late capitalism, from the Reagan era forward, work, for many people, has come to feel like a battlefield, and daily life, including politics and life online, like yet more slaughter. People across all walks of life—rich and poor, young and old, caretakers and the cared for, the faithful and the faithless—really are worn down, wiped out, threadbare, on edge, battered, and battle-scarred. Lockdowns, too, are features of war, as if each one of us, amid not only the pandemic but also acts of terrorism and mass shootings and armed insurrections, were now engaged in a Hobbesian battle for existence, civil life having become a war zone. May there one day come again more peaceful metaphors for anguish, bone-aching weariness, bitter regret, and haunting loss. “You will tear your heart out, desperate, raging,” Achilles warned Agamemnon. Meanwhile, a wellness site tells me that there are “11 ways to alleviate burnout and the ‘Pandemic Wall.’ ” First, “Make a list of coping strategies.” Yeah, no. ♦

By signing up, you agree to our User Agreement and Privacy Policy & Cookie Statement . This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
- SUGGESTED TOPICS
- The Magazine
- Newsletters
- Managing Yourself
- Managing Teams
- Work-life Balance
- The Big Idea
- Data & Visuals
- Reading Lists
- Case Selections
- HBR Learning
- Topic Feeds
- Account Settings
- Email Preferences
Burnout Is About Your Workplace, Not Your People
- Jennifer Moss

Leaders create the conditions that lead to burnout — or prevent it.
We often think of burnout as an individual problem, solvable with simple-fix techniques like “learning to say no”, more yoga, better breathing, practicing resilience. Yet, evidence is mounting that personal, band-aid solutions are not enough to combat an epic and rapidly evolving workplace phenomenon. In fact, they might be harming, not helping the battle. With “burnout” now officially recognized by the World Health Organization, the responsibility for managing it has shifted away from employees and toward employers. Burnout is preventable. It requires good organizational hygiene, better data, asking more timely and relevant questions, smarter budgeting (more micro-budgeting), and ensuring that wellness offerings are included as part of your well-being strategy
We tend to think of burnout as an individual problem, solvable by “learning to say no,” more yoga, better breathing techniques, practicing resilience — the self-help list goes on. But evidence is mounting that applying personal, band-aid solutions to an epic and rapidly evolving workplace phenomenon may be harming, not helping, the battle. With “burnout” now officially recognized by the World Health Organization (WHO) , the responsibility for managing it has shifted away from the individual and towards the organization. Leaders take note: It’s now on you to build a burnout strategy.
- Jennifer Moss is a workplace expert, international public speaker, and award-winning journalist. She is the bestselling author of Unlocking Happiness at Work (Kogan Page, 2016) and The Burnout Epidemic (HBR Press, September 2021).
Partner Center
How to Prevent Burnout in the Workplace: 20 Strategies

Its impact is considerable.
Indeed, burnout among physicians, which is twice that of the general public, leads to emotional and physical withdrawal from work and can negatively impact safe, high-quality healthcare for patients (Olson et al., 2019).
The effect of burnout is widespread. The impact of increasing workload, a perceived lack of control, and job insecurity lead to high turnover, reduced productivity, and poor mental health (Kolomitro et al., 2019).
This article explores the warning signs of burnout in the workplace and what we can do to prevent it.
Before you continue, we thought you might like to download our three Stress & Burnout Prevention Exercises (PDF) for free . These science-based exercises will equip you and those you work with, with tools to manage stress better and find a healthier balance in your life.
This Article Contains:
14 warning signs of workplace burnout, 8 strategies to prevent employee burnout, 6 programs & initiatives for hr professionals, preventing burnout when working from home, positivepsychology.com’s relevant resources, a take-home message.
In increasingly busy, high-pressure working environments, employees often become the shock absorbers , taking organizational strain and working longer, more frantic hours (Kolomitro et al., 2019).
The long-term impact is burnout , identified by “lower psychological and physical wellbeing, as well as dissatisfaction, and employee turnover” (Kolomitro et al., 2019).
“Burnout occurs when an individual experiences too much stress for a prolonged period,” writes researcher Susan Bruce (2009). The employee is left feeling mentally, emotionally, and physically exhausted. Not only that, they are less productive at work, show reduced concern for others, and are more likely to miss work (Bruce, 2009).
Its effects are not only felt by the individual. In education, for example, burned-out teachers can negatively impact their students’ education (Bruce, 2009).
Organizations with burned-out staff experience low productivity, lost working days, lower profits, reduced talent, and even damage to their corporate reputation (Bruce, 2009).
So how do we recognize the warning signs of burnout?
Once we can spot early predictors and signs of burnout, we can take action.
Writing for the Harvard Business Review , Elizabeth Grace Saunders (2021) describes how, without realizing and on the verge of burnout, she was “perpetually exhausted, annoyed, and feeling unaccomplished and unappreciated.”
There are many early predictors, indicators, and manifestations of stress that contribute to burnout.
The following factors are recognized as early predictors of burnout (Maslach & Leiter, 2008):
- Job demands that exceed human limits.
- Role conflict leading to a perceived lack of control; being under pressure from several, often incompatible, demands that compete with one another.
- Insufficient reward and lack of recognition for the work performed, devaluing both the work and the worker.
- Lack of support from the manager or team, consistently associated with exhaustion.
- Work perceived as unfair or inequitable , caused by an effort–reward imbalance.
- Relationship between the individual and the environment leading to feelings of imbalance or a bad fit. Such incongruity connects with excessive job demands and unfairness at work.
The following feelings, physical complaints, and thought patterns accompany stress and manifest in the workplace (Bruce, 2009):
- Feelings : Tired, irritable, distracted, inadequate, and incompetent.
- Physical : Muscular aches and body pain, headaches, increased or reduced appetite, weight change, and nausea.
- Emotional : Feeling trapped, hopeless, and depressed.
- Mental : Poor concentration, muddled thinking, and indecisiveness.
Stress in the workplace can manifest as:
- Regularly arriving late to work
- Absenteeism
- Reduced goals, aspirations, and commitment
- Increased cynicism and apathy
- Poor treatment of others
- Relationship difficulties
- Increase in smoking and alcohol consumption
- Making careless mistakes
- Obstructive and uncooperative behavior
- Overspending
While burnout is unique for every individual, it can be spotted and avoided.

- Work satisfaction
- Organizational respect
- Employer care
- Work–life integration
Balancing all four factors is essential to overall employee wellbeing and reduces the likelihood of long-term and ultimately overwhelming pressure.
The following strategies can help find that balance and protect against burnout (Saunders, 2021; Boyes, 2021).
When workload and capacity are in balance, it is possible to get work done and find time for professional growth, development, rest, and work recovery.
Assess how you are doing in each of the following activities:
- Planning your work. Do you know what work is coming? What will you be working on next week? Do you have a shareable plan?
- Delegating tasks. Sometimes we steer away from handing over work to others, but it can be positive for both parties.
- Saying no. Saying no is necessary when you have too much work or someone else could perform it.
- Letting go of perfectionism. Sometimes producing a perfect piece of work is not required; sometimes, good enough is all that is needed.
If you are experiencing any of the symptoms of burnout, try to focus on each of the above actions. Proactive effort to reduce workload can be highly effective at removing some stressors impacting burnout.
Feeling out of control, a lack of autonomy, and inadequate resources impact your ability to succeed at what you are doing and contribute to burnout.
Do you get calls from your boss or answer emails late into the night or over the weekend?
Consider how you can regain control. Agree on a timetable for when you are available and what resources you need to do your job well. Gaining a sense of control over your environment can increase your sense of autonomy.
Community is essential to feeling supported. While you may not be able to choose who you work with, you can invest time and energy in strengthening the bonds you share with your coworkers and boss.
Positive group morale, where you can rely on one other, can make the team more robust and reduce the likelihood of burnout.
A sense of fairness at work can be helped by feeling valued and recognized for the contributions you make.
Let it be known that you would like to be mentioned as a contributor or become involved in presenting some of the team’s successes.
Value mismatch
“Burnout isn’t simply about being tired,” writes Saunders (2021). When your values cannot align with those of your organization, you may need to consider whether it is time to look for new opportunities.
Determine if you can find compatibility in your current position or whether another organization might be better suited to your values.
Task balancing
After delivering something highly demanding (cognitively, emotionally, or physically), it may be beneficial to switch to a less complex task.
Swapping between tasks of varying difficulty on a daily, weekly, or monthly basis can be an excellent way to regain balance and give yourself a break.
After putting together a complex report, presentation, or analysis, why not plan the rest of your week for organizing emails into folders?
Mental breaks
We sometimes feel unable to stop. We check emails while in line for a coffee and type up notes on the flight back from a business meeting. While it can seem essential when you are busy to keep pushing ahead, it is vital to take breaks. Use spare time to read a book, listen to music, talk to a friend, or run through breathing exercises.
Taking time out for yourself is crucial to your wellbeing and will ultimately benefit your performance.
Physical breaks
Stress and tension take their toll physically. You may notice tight shoulders or headaches. Learning to recognize times when you are most stressed or anxious can help. When you do, find a moment to take some slow breaths or go for a walk.
Download 3 Free Stress & Burnout Prevention Exercises (PDF)
These detailed, science-based exercises will equip you or your clients with tools to manage stress better and find a healthier balance in their life.
Download 3 Stress & Burnout Prevention Exercises Pack (PDF)
By filling out your name and email address below.
- Email Address *
- Your Expertise * Your expertise Therapy Coaching Education Counseling Business Healthcare Other
- Comments This field is for validation purposes and should be left unchanged.
While burnout is damaging to the employee, it is also expensive for the business. In the U.S. alone, the cost of absenteeism is $300 billion a year in insurance, reduced productivity, and staff turnover (Peart, 2021).
HR professionals have an essential role to play in reducing the effect and likelihood of burnout within the working environment (Castanheira & Chambel, 2010).
Putting in effective workplace wellness practices can help. For them to be effective, they must be at an organizational level, reducing stress at work, fostering employee wellbeing, and upping employee engagement (Peart, 2021; Chamorro-Premuzic, 2021).
According to clinical psychologist and leadership consultant Natalia Peart (2021), it is possible to create a working environment that reduces stress. To do this, we must build positive, stress-reducing environments that integrate with day-to-day working habits.
Increase psychological safety
Staff must see work as nonthreatening, allowing them to work and collaborate effectively. We can help perceptions of psychological safety by:
- Giving staff clear goals
- Making sure they feel heard by management
- Making work challenging yet non-threatening
Create a culture where it is okay to fail. Recognize and encourage people who think outside the box.
Regular workday breaks
Our attention and ability to focus are limited. After two hours (or less), our concentration reduces significantly (Peart, 2021), which could make us more likely to make mistakes, become less creative, and lose the ability to solve complex problems.
Staff must be encouraged to take breaks without feeling guilty. It is vital that they take time away from their desk regularly and as needed.
Placing entries in the calendar can help by setting aside time. And leading by example can help reduce stress and create an environment conducive to consistent performance.
World’s Largest Positive Psychology Resource
The Positive Psychology Toolkit© is a groundbreaking practitioner resource containing over 500 science-based exercises , activities, interventions, questionnaires, and assessments created by experts using the latest positive psychology research.
Updated monthly. 100% Science-based.
“The best positive psychology resource out there!” — Emiliya Zhivotovskaya , Flourishing Center CEO
Private spaces
While open offices are commonplace, they can be a cause of ongoing distraction.
Create spaces where staff can work uninterrupted and encourage them to turn off email and other messaging services at predefined times.
Set work boundaries
There will be times when working outside core hours may be necessary, but there is still a need to agree on typical workday expectations. Regularly answering emails late in the evening or over the weekend can increase employee anxiety and the sense of never leaving work.
Setting boundaries, flexible working, and providing additional time off can restore work–life balance.
Increase employee engagement
Improving the connection staff feel with their workplace and coworkers can heighten job satisfaction while reducing stress (Peart, 2021).
Engagement can be promoted through a culture of:
- Transparency It is vital to understand how work aligns with corporate goals.
- Using strengths and talents When people use their strengths, they feel more competent and engaged.
- Autonomy Staff are “43% less likely to experience high levels of burnout” when they decide on how and when they complete their work (Peart, 2021).
- Recognition Supporting and recognizing good work reduces stress while promoting a sense of belonging.
- Sense of purpose Feeling a sense of purpose in what we do adds meaning to otherwise tedious tasks. Share the company’s goals and communicate their positive effect on the community.
Hire better bosses
Good leaders must be hired or created, shielding employees from stress. However, rather than being seen as a source of calm and inspiration, managers often become the cause of stress. This is especially the case when managers make poor decisions, are abusive, or alienate their staff.
Hiring teams must take more time scrutinizing candidates who apply for leadership roles, identifying their empathy, emotional intelligence , and ability to perform under pressure.

While working from home removes commuting times and can allow us to take our children to school, it may be overshadowed by long working hours and a sense that we never leave work.
“The risk of burnout when working from home is substantial” write Laura Giurge and Vanessa Bohns (2021).
In an environment where the line between work and home life can quickly become blurred, it is crucial to our mental health that we agree upon and implement boundaries.
Even a non-urgent email sent after hours can create a sense of urgency or leave us with the weight of the action on our mind until we log on the next day. Working from home can also cause staff to feel indebted to their employer and mistakenly believe they need to work more intensely for more hours each day.
There are ways to create boundaries when working from home and reduce loneliness and burnout (Giurge & Bohns, 2021; Moss, 2021):
- Put on work clothes. Wearing something different when working from home can create a sense of performing a work activity in a separate environment.
- Commute to work. Even a walk around the block before heading to a dedicated space to work can create a feeling of separation.
- Maintain temporal boundaries. Create a work schedule that fits your needs and your organization’s, such as taking the children to school and stopping for lunch. Respect your own time and that of your colleagues. They may have different schedules for their commitments.
- Create an out-of-office reply. Create an automated email reply for when you are performing non-work activities or need time to focus uninterrupted on your tasks.
- Virtual coffee breaks. Staff should be encouraged to take time away from the desk for a walk with a friend, a casual chat, or to grab a coffee. Taking even 10 minutes will ultimately benefit concentration and focus. Finding ways to “carve out non-work time and mental space” are crucial when working from home, where boundaries are so unclear (Giurge & Bohns, 2021).
- Reducing loneliness. While working from home can be incredibly beneficial or even necessary, it may become a source of loneliness. Scheduling an in-office day once a month (as long as a time can be agreed upon and works for all remote workers) where staff can get together and have a catch-up can improve bonds between workers while creating a sense of shared goals.
15 Minutes a day to prevent burnout – Paul Koeck
We have many resources that can help with managing stress, overcoming obstacles, and dealing with difficult situations.
- 5-4-3-2-1 Stress Reduction Technique Use your five senses to ground yourself in the moment and slow down thinking.
- Coping With Stress Identifying and understanding what causes you stress can help you regain control over how you respond.
- Coping – Stressors and Resources Consider past, current, and anticipated stressors, and plan coping strategies to manage them.
- It Could Be Worse Build resilience by challenging unhelpful thought patterns and processes .
17 Stress & Burnout Prevention Exercises If you’re looking for more science-based ways to help others manage stress without spending hours on research and session prep, this collection contains 17 validated stress management tools for practitioners . Use them to help others identify signs of burnout and create more balance in their lives.
17 Exercises To Reduce Stress & Burnout
Help your clients prevent burnout, handle stressors, and achieve a healthy, sustainable work-life balance with these 17 Stress & Burnout Prevention Exercises [PDF].
Created by Experts. 100% Science-based.
Humans are curious.
We need a degree of stress to prevent boredom and frustration.
However, too much can lead to poor decision making and ineffective communication, negatively impact mental health, and ultimately cause burnout (Bruce, 2009).
Stress not only takes a toll on our physical and mental wellbeing, but also narrows our outlook, making long-term strategic thinking more difficult (Peart, 2021).
“Burnout is experienced as emotional exhaustion or depersonalization” (Olson et al., 2019) and is the ultimate destination for long-term stress. It can harm physical health, psychological wellbeing, and performance at work (Olson et al., 2019; Maslach & Leiter, 2008).
While unpleasant for the individual, it can also damage the organization, leading to failing performance, absenteeism, and disengagement.
Spotting the early warning signs, positive leadership , and protective and proactive policies can avoid or reduce burnout. A balanced work culture promotes a positive work environment and a growth mindset.
There is a proven link between job satisfaction and mental health, so finding a good balance for stress is vital. Low job satisfaction at work can predict depression, low self-esteem, and anxiety (Bruce, 2009).
Use this article’s guidance to recognize dangers or early warning signs in yourself, colleagues, or clients. Then take some steps discussed to help reduce or prevent damaging environments and invest in employees’ wellbeing and performance.
We hope you enjoyed reading this article. Don’t forget to download our three Stress & Burnout Prevention Exercises (PDF) for free .
- Boyes, A. (2021). How to get through an extremely busy time at work. In HBR guide to beating burnout (pp. 29–34). Harvard Business Review Press.
- Bruce, S. P. (2009). Recognizing stress and avoiding burnout. Currents in Pharmacy Teaching and Learning, 1 (1), 57–64.
- Castanheira, F., & Chambel, M. J. (2010). Reducing burnout in call centers through HR practices. Human Resource Management , 49 (6), 1047–1065.
- Chamorro-Premuzic, T. (2021). Just hire better bosses. In HBR guide to beating burnout (pp. 189–194). Harvard Business Review Press.
- Giurge, L. M, & Bohns, V. K. (2021). How to avoid burnout while working from home. In HBR guide to beating burnout (pp. 35–40). Harvard Business Review Press.
- Hyett, M. P., & Parker, G. B. (2015). Further examination of the properties of the Workplace Well-Being Questionnaire (WWQ). Social Indicators Research , 124 (2), 683–692.
- Kolomitro, K., Kenny, N., & Sheffield, S. L. M. (2019). A call to action: Exploring and responding to educational developers’ workplace burnout and well-being in higher education. International Journal for Academic Development , 1–14.
- Maslach, C., & Leiter, M. P. (2008). Early predictors of job burnout and engagement. Journal of Applied Psychology , 93 (3), 498–512.
- Moss, J. (2021). Helping remote workers avoid loneliness and burnout. In HBR guide to beating burnout (pp. 173–180). Harvard Business Review Press.
- Olson, K., Sinsky, C., Rinne, S. T., Long, T., Vender, R., Mukherjee, S., … Linzer, M. (2019). Cross-sectional survey of workplace stressors associated with physician burnout measured by the Mini-Z and the Maslach Burnout Inventory. Stress and Health , 35 (2), 157–175.
- Peart, N. (2021). Making work less stressful and more engaging for your employees. In HBR guide to beating burnout (pp. 139–148). Harvard Business Review Press.
- Saunders, E. G. (2021). Six causes of burnout, and how to avoid them. In HBR guide to beating burnout (pp. 23–28). Harvard Business Review Press.
Share this article:
Article feedback
What our readers think.
Wow, a very well-researched report with clearly explained content. Although the articles took the form of a generalised format which is why there was a less evidence-based approach, the author did a marvellous work.
Question: Is burnout predictive? In an education study, how would predictive burnout be validated in an evidence-based educational environment?
Thank you for your comment and your question. Burnout is most certainly predictive, and therefore also preventative. There has been a plethora of research on protective factors of burnout as well as what can actually predict burnout.
I think this article and this article might be of interest to you since they discuss predictive burnout in educational environments.
I hope this helps.
Kind regards, -Caroline | Community Manager
Let us know your thoughts Cancel reply
Your email address will not be published.
Save my name, email, and website in this browser for the next time I comment.
Related articles

Recognizing High-Functioning Anxiety & 6 Tools to Manage It
As our lives get busier and busier and more and more crises develop on the world stage, we are seeing reports of increasing incidences of [...]

Moving From Chronic Stress to Wellbeing & Resilience
Stress. It can be as minute as daily hassles, car trouble, an angry boss, to financial strain, a death or terminal illness. The ongoing stressors [...]

3 Burnout Prevention Strategies for Type A Personality
Highly driven, goal-oriented, and somewhat impatient? You may be dealing with a Type A personality. Having a Type A personality comes with a mixed bag [...]
Read other articles by their category
- Body & Brain (55)
- Coaching & Application (59)
- Compassion (26)
- Counseling (51)
- Emotional Intelligence (24)
- Gratitude (18)
- Grief & Bereavement (21)
- Happiness & SWB (40)
- Meaning & Values (27)
- Meditation (21)
- Mindfulness (44)
- Motivation & Goals (46)
- Optimism & Mindset (35)
- Positive CBT (30)
- Positive Communication (23)
- Positive Education (48)
- Positive Emotions (32)
- Positive Leadership (20)
- Positive Parenting (16)
- Positive Psychology (34)
- Positive Workplace (37)
- Productivity (18)
- Relationships (46)
- Resilience & Coping (40)
- Self Awareness (22)
- Self Esteem (38)
- Strengths & Virtues (33)
- Stress & Burnout Prevention (38)
- Theory & Books (46)
- Therapy Exercises (37)
- Types of Therapy (65)
- Email This field is for validation purposes and should be left unchanged.
3 Stress Exercises Pack

The Face of Burnout in Nursing: My Personal Story and Lessons Learned

Photo by Artem Kovalev on Unsplash
Two-and-a-half years ago, I experienced severe burnout in my role as a night shift charge nurse in a cardiovascular ICU. This blog post shares my personal story, highlighting the common ingredients of burnout and the challenges I faced. Through this experience, I learned valuable lessons that can benefit both nurses and the health care industry as a whole.
Where it All Began
Transitioning from a clinical nurse educator to a night shift charge nurse in a new cardiovascular ICU was an exciting opportunity for me. However, it soon became overwhelming due to various factors. These included a surgeon I didn’t see eye-to-eye with, moral and ethical dilemmas in patient care, staffing challenges, and a hostile work environment created by lateral violence from coworkers.
Strained to the Breaking Point
As my anxiety grew, I struggled to meet expectations each night. While prioritizing patient care and my night shift team, I feared for our patients’ well-being. Frequently, we were overloaded with acute post-cardiothoracic surgery patients. Despite my efforts to manage admissions responsibly, I faced constant pressure. Doubts crept in, and I lost trust in myself and my ability to provide safe care.
The emotional toll affected my eating, sleeping, and overall well-being. I couldn’t disconnect from work. When I was at work I feared when my surgeon rounded or if I would need to call him in the middle of the night because a patient’s condition was declining. When I was off, I was worried about how the patients were doing and if there was anything I might have done wrong. It was nothing for me to randomly start crying at any moment.
I was afraid to leave because of the financial stability this position gave me and my family. But the last thing I wanted was to be responsible for a patient’s deterioration, or worse, a patient dying. I had to get out of there. To be honest, I wasn’t even sure I wanted to be a nurse anymore.
Seeking a Solution
My story of burnout is unique to me, but it echoes stories from many other nurses. After resigning, I realized I didn’t want to be a victim of burnout. I embarked on a healing journey and learned valuable lessons about myself and the life I wanted to create. While personal shifts are important, I also believe tangible solutions within the health care environment can significantly impact patient well-being and nurse satisfaction. Instead of dwelling on problems, I embraced a mindset of seeking solutions. Here are some actionable suggestions to create a safer, healthier health care workplace.
Four Suggestions for Improvement
- Suggest an acuity-based staffing model: An acuity-based staffing model, supported by research, adjusts nurse-to-patient ratios based on patient diagnoses and acuity. This allows nurses caring for higher-acuity patients to have a reduced nurse-to-patient ratio so they can be more attentive to patients’ needs and subtle changes. A nurse with a higher nurse-to-patient ratio will have patients with stable vital signs, controlled pain, and not showing signs of distress.
- Advocate for leadership presence on night shift: Night shift nurses often face resource limitations and imbalanced skill mixes, including more novice nurses. Communicating the challenges to leadership and inviting them to experience the night shift reality can help bridge the gap between awareness and action. Trust me, leadership doesn’t always know how things really are.
- Foster accountability within the team: Encourage a culture of mutual support and self-care. Don’t just come in each day to take care of your patients. Come in each day to take care of each other. Establish a buddy system to make sure you are taking your needed breaks, using the bathroom, and staying hydrated. By caring for each other, nurses can collectively prioritize well-being.
- Provide a comprehensive orientation for new hires: Play an active role in onboarding new nurses, ensuring they feel confident, competent, and welcomed into the team. Reducing turnover is essential to improving staffing situations and maintaining the effectiveness of any new staffing model.

Jenna Colelli, MSN, BSEd, RN, CCRN-K, is director of staff development for Wellington Regional Medical Center, Wellington, FL. In this role, she works to “mentor and empower nurses to care for themselves so they can better care for the patients we serve.”
Share this:
- Click to share on Facebook (Opens in new window)
- Click to share on X (Opens in new window)
- Click to share on Twitter (Opens in new window)
- Click to share on LinkedIn (Opens in new window)
- Click to share on Reddit (Opens in new window)
- Click to share on Pinterest (Opens in new window)
- Click to email a link to a friend (Opens in new window)
- Click to print (Opens in new window)
- Click to share on WhatsApp (Opens in new window)
- Click to share on Tumblr (Opens in new window)
- Click to share on Pocket (Opens in new window)
Share This Story, Choose Your Platform!
About the author: guest author.
Thank you for this honest, thoughtful and insightful essay. Your suggested solutions are right on target. I hope the appropriate leaders heed your words and put them into practice. Good luck in your new position.
Thank you for speaking your truth. Best wishes for success in your new position. Gloria Cox MSN, BS Health Art, RN Retired Nurse Educator Vaccinator (Covid-19) 2021-2022
Thank you for this. I’m retired now but nursing can’t be like a production line, it requires attention to individuals- co-workers as well as patients. Our system is so fragmented that saving money in the hospital can seem like a win even if it increases costs elsewhere. We can do a lot to reduce burn-out and improve practice by caring for our team.
Comments are moderated before approval, but always welcome. Cancel reply
This site uses Akismet to reduce spam. Learn how your comment data is processed .
Discover more from Off the Charts
Subscribe now to keep reading and get access to the full archive.
Type your email…
Continue reading

Employers need to focus on workplace burnout: Here's why
Concrete ways to address the problem with psychological science
- Healthy Workplaces
- Mental Health

Workplace burnout can be a serious problem for individual workers and entire organizations. The good news is there are ways to get ahead of it and methods to rectify it.
What it is: “Workplace” burnout is an occupation-related syndrome resulting from chronic workplace stress that has not been successfully managed. Burnout can be measured and quantified using validated scientific tools. It involves ongoing emotional exhaustion, psychological distance or negativity, and feelings of inefficacy—all adding up to a state where the job-related stressors are not being effectively managed by the normal rest found in work breaks, weekends, and time off (World Health Organization, 2019).
What it isn’t: This isn’t “burnout” we use in casual conversation. True workplace burnout is specific to one’s job or occupation and is more concerning and detrimental than the daily irritations everyone experiences and most of us manage.
There are three dimensions to workplace burnout:
- Feelings of energy depletion or emotional exhaustion
- Increased mental distance from one’s work and negative or cynical feelings toward one’s work
- Reduced sense of efficacy at work
Mindy Shoss, PhD, professor of psychology at the University of Central Florida and associate editor of the Journal of Occupational Health Psychology , says, “There are many potential causes of burnout in today’s workplaces—excessive workloads, low levels of support, having little say or control over workplace matters, lack of recognition or rewards for one’s efforts, and interpersonally toxic and unfair work environments. Add to that the constant hum of uncertainty about a possible recession, and it’s no surprise that burnout is on the rise in many workplaces.”
[ Related: A pandemic of burnout: 4 questions for Dan Pelton ]
Why workplace burnout matters
Decades of research shows an association between workplace burnout and a host of negative organizational, psychological, and even physical consequences, including:
Organizational
- Absenteeism
- Job dissatisfaction
- Presenteeism
Psychological
- Psychological distress
- Heart disease
- Musculoskeletal pain
(Salvagioni et al., 2017).
The facts and figures
According to leading scientific research, employees who experience true workplace burnout have a:
- 57% increased risk of workplace absence greater than two weeks due to illness (Borritz et al., 2010)
- 180% increased risk of developing depressive disorders (Ahola et al., 2005)
- 84% increased risk of Type 2 diabetes (Melamed et al., 2006)
- 40% increased risk of hypertension (von Känel et al., 2020)
Additionally, workplace burnout may impair short-term memory, attention, and other cognitive processes essential for daily work activities (Gavelin et al., 2022).
Dennis P. Stolle, JD, PhD, APA’s senior director of applied psychology, points out that burnout has consequences for organizational effectiveness, not just individuals. “When workers are suffering from burnout, their productivity drops, and they may become less innovative and more likely to make errors. If this spreads throughout an organization, it can have a serious negative impact on productivity, service quality, and the bottom-line.”
What you can do
Christina Maslach , PhD, one of the leading experts on workplace burnout, has emphasized that finding solutions to the problem of burnout requires considering the workplace, the worker, and the workplace/worker fit.
“We need to reframe the basic question from who is burning out to why they are burning out. It is not enough to simply focus on the worker who is having a problem—there must be a recognition of the surrounding job conditions that are the sources of the problem. That is why the job-person relationship is so important. Is there a good match between the worker and the workplace environment, which enables the worker to thrive and do well?” Maslach says.
Employers can
- Periodically measure whether workplace burnout is happening in their organization through thoughtful and systematic surveys.
- Keep track of workloads, regularly check in with workers on how they are doing, and encourage taking advantage of time off.
- Take a hard look at their organization’s practices to ensure that they are giving workers the control, flexibility, and resources needed to manage workload and job stress.
Employees can
- Prioritize self-care, including caring for both physical and emotional well-being.
- Set appropriate boundaries, including giving themselves permission to truly unplug from work for reasonable periods of time.
- Prioritize social relationships. Healthy relationships with coworkers, friends, and family can help buffer workplace stresses.
Employers and employees can
- Constantly strive for a healthy, supportive, and inclusive workplace that fosters a sense of trust and confidence that workers have each other’s backs.
- Regularly discuss whether workloads are reasonable and appropriate to ensure work is distributed in an equitable way and, if needed, restructure accordingly.
Sometimes the solution may be to redesign job responsibilities or move the employee to a different position in the same organization. Not only might this be good for the employee, but it may help the organization retain valuable talent. A win/win.
Related podcasts

Why we’re burned out and what to do about it, with Christina Maslach, PhD

How do you build a successful team? With Eduardo Salas, PhD
Mental health in the workplace
To Curb Burnout, Design Jobs to Better Match Employees’ Needs
The Burnout Challenge: Managing People’s Relationships with Their Jobs
Burnout: A Guide to Identifying Burnout and Pathways to Recovery
Ahola, K., Honkonen, T., Isometsä, E., Kalimo, R., Nykyri, E., Aromaa, A., & Lönnqvist, J. (2005). The relationship between job-related burnout and depressive disorders—Results from the Finnish Health 2000 Study. Journal of Affective Disorders , 88 (1), 55–62. https://doi.org/10.1016/j.jad.2005.06.004
Borritz, M., Christensen, K. B., Bültmann, U., Rugulies, R., Lund, T., Andersen, I., Villadsen, E., Diderichsen, F., & Kristensen, T. S. (2010). Impact of burnout and psychosocial work characteristics on future long-term sickness absence. Prospective results of the Danish PUMA study among human service workers. Journal of Occupational and Environmental Medicine , 52 (10), 964–970. https://doi.org/10.1097/JOM.0b013e3181f12f95
Gavelin, H. M., Domellöf, M. E., Åström, E., Nelson, A., Launder, N. H., Neely, A. S., & Lampit, A. (2022). Cognitive function in clinical burnout: A systematic review and meta-analysis. Work & Stress , 36 (1), 86–104. https://doi.org/10.1080/02678373.2021.2002972
Melamed, S., Shirom, A., Toker, S., & Shapira, I. (2006). Burnout and risk of type 2 diabetes: A prospective study of apparently healthy employed persons. Psychosomatic Medicine , 68 (6), 863–869. https://doi.org/10.1097/01.psy.0000242860.24009.f0
Salvagioni, D. A. J., Melanda, F. N., Mesas, A. E., González, A. D., Gabani, F. L., & de Andrade, S. M. (2017). Physical, psychological and occupational consequences of job burnout: A systematic review of prospective studies. PLoS ONE , 12 (10), Article e0185781. https://doi.org/10.1371/journal.pone.0185781
von Känel, R., Princip, M., Holzgang, S. A., Fuchs, W. J., van Nuffel, M., Pazhenkottil, A. P., & Spiller, T. R. (2020). Relationship between job burnout and somatic diseases: A network analysis. Scientific Reports , 10 (1), Article 18438. https://doi.org/10.1038/s41598-020-75611-7
World Health Organization. (2019). QD85 Burnout. In International statistical classification of diseases and related health problems (11th ed.). https://icd.who.int/browse11/l-m/en#/http://id.who.int/icd/entity/129180281
Recommended Reading
Related topics.
- Healthy workplaces
- 5 ways to improve employee mental health
- Psychology informs Surgeon General’s healthy workplace framework
- Worker well-being is in demand as organizational culture shifts
- Women leaders make work better
You may also like
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Environ Res Public Health

Burnout: A Review of Theory and Measurement
Sergio edú-valsania.
1 Department of Social Sciences, Universidad Europea Miguel de Cervantes (UEMC), C/Padre Julio Chevalier, 2, 47012 Valladolid, Spain; se.cmeu@udes
Ana Laguía
2 Department of Social and Organizational Psychology, Faculty of Psychology, Universidad Nacional de Educación a Distancia (UNED), C/Juan del Rosal 10, 28040 Madrid, Spain; se.denu.isp@onairomaj
Juan A. Moriano
A growing body of empirical evidence shows that occupational health is now more relevant than ever due to the COVID-19 pandemic. This review focuses on burnout, an occupational phenomenon that results from chronic stress in the workplace. After analyzing how burnout occurs and its different dimensions, the following aspects are discussed: (1) Description of the factors that can trigger burnout and the individual factors that have been proposed to modulate it, (2) identification of the effects that burnout generates at both individual and organizational levels, (3) presentation of the main actions that can be used to prevent and/or reduce burnout, and (4) recapitulation of the main tools that have been developed so far to measure burnout, both from a generic perspective or applied to specific occupations. Furthermore, this review summarizes the main contributions of the papers that comprise the Special Issue on “Occupational Stress and Health: Psychological Burden and Burnout”, which represent an advance in the theoretical and practical understanding of burnout.
1. Introduction
When work and professional environments are not well organized and managed, they can have adverse consequences for workers that, far from dignifying them, exhaust them and consume their psychological resources. Burnout has become one of the most important psychosocial occupational hazards in today’s society, generating significant costs for both individuals and organizations [ 1 , 2 , 3 , 4 ]. Although burnout was initially considered to be specific to professionals working in the care of people [ 5 ], later evidence has shown that this syndrome can develop among all types of professions and occupational groups [ 6 , 7 ]. However, burnout prevalence estimates vary considerably according to the burnout definition applied. For instance, a national study of US general surgery residents found estimates varied from 3.2% to 91.4%, with 43.2% of respondents acknowledging weekly symptoms [ 8 ].
The enormous negative impact that burnout has on the work and personal lives of workers, also affecting the economy and public health of the most affected countries, has led the World Health Organization (WHO) to include this syndrome in the 11th Revision of the International Classification of Diseases (ICD-11) as a phenomenon exclusive to the occupational context. Likewise, the need to address burnout is also justified for legal reasons, such as compliance with the European Union Framework Directive on Health and Safety (89/391/EEC).
A growing body of empirical evidence shows that occupational health is now more relevant than ever due to the COVID-19 pandemic. Particularly, the pandemic has placed considerable psychological strain on healthcare workers. Since the COVID-19 outbreak, numerous studies related to burnout have been carried out with samples of frontline healthcare workers, physicians, nurses, or pharmacists across the world [ 9 , 10 , 11 , 12 ]. However, the lack of a baseline level of burnout before the pandemic makes it difficult to compare changes in prevalence for the same populations. Evidence from studies of the impact of past outbreaks (e.g., SARS, influenza, or Ebola epidemics) show long-term cognitive and mental health effects (e.g., emotional distress, post-traumatic stress disorder) [ 13 ]. This evidence can be useful to design interventions for healthcare workers. These are also hard times for workers in general. Teleworking full-time due to COVID-19 has received the attention of several empirical works, which analyze job exhaustion and burnout [ 14 , 15 , 16 , 17 ]. Teacher burnout is also the focus of an increasing number of studies [ 18 , 19 , 20 , 21 ]. Additionally, working parents may experience high levels of stress in the home environment during the COVID-19 pandemic, leading to parental burnout [ 22 , 23 ].
This review aims to understand what burnout is and its different components, how it occurs, to identify the factors that trigger burnout and the individual factors that modulate it, to identify the effects that burnout generates at both individual and organizational levels, to understand which are the main actions that can be used to prevent and/or reduce burnout, and to present the main tools that currently exist to measure burnout.
2. Burnout: Definition and Development of This Construct
Overall, burnout syndrome is an individual response to chronic work stress that develops progressively and can eventually become chronic, causing health alterations [ 24 ]. From a psychological point of view, this syndrome causes damage at a cognitive, emotional, and attitudinal level, which translates into negative behavior towards work, peers, users, and the professional role itself [ 25 ]. However, it is not a personal problem, but a consequence of certain characteristics of the work activity [ 26 ].
Historically, Graham Greene was the first author to use the term burnout in his novel “A Burnt-Out Case” when describing the story of an architect who found neither meaning in his profession nor pleasure in life. Later, the term was picked up and introduced in the psychological sphere by Freudenberger [ 27 ], where he described burnout as a state of exhaustion, fatigue, and frustration due to a professional activity that fails to produce the expected expectations. Initially, this author delimited it as something exclusively related to volunteer workers in a care center where all kinds of people with mental disorders and social problems attended. Because of their occupation, these workers experienced in crescendo a loss of energy to the point of exhaustion and demotivation, as well as aggressiveness towards the service users.
Shortly thereafter, Maslach [ 28 ] introduced burnout into the scientific literature and defined it as a gradual process of fatigue, cynicism, and reduced commitment among social care professionals. Years later and after several empirical studies, Maslach and Jackson [ 5 ] reformulated the concept and elaborated a more rigorous and operational definition of burnout as a psychological syndrome characterized by emotional exhaustion, depersonalization and a reduced sense of professional efficacy that can appear in caregivers ( Table 1 ). The turning point between the two definitions is the consideration of burnout as a syndrome, with a syndrome being understood as a picture or set of symptoms and signs that exist at the same time and clinically define a particular state distinct from others.
Burnout dimensions.
| Dimension | Definition |
|---|---|
| Emotional exhaustion | This dimension manifests in the form of feelings and sensation of being exhausted by the psychological efforts made at work. It is also described in terms of weariness, tiredness, fatigue, weakening, and the subjects who manifest this type of feelings show difficulties in adapting to the work environment since they lack sufficient emotional energy to cope with work tasks. |
| Cynicism or depersonalization | This dimension, the interpersonal component of burnout, is defined as a response of detachment, indifference and unconcern towards the work being performed and/or the people who receive it. It translates into negative or inappropriate attitudes and behaviors, irritability, loss of idealism, and interpersonal avoidance usually towards service users, patients, and/or clients. |
| Reduced personal achievement | This dimension is reflected in a negative professional self-evaluation and doubts about the ability to perform the job effectively, as well as a greater tendency to evaluate results negatively. It also translates into a decrease in productivity and capabilities, low morale, as well as lower coping skills. |
However, some authors have argued that these three dimensions are not completely independent. Thus, it is possible to find several explanations in the literature. The difference between them lies in which is the first dimension that appears in the face of job stress (emotional exhaustion or depersonalization). Although definitive evidence has not yet been obtained, longitudinal studies have shown that there is a causal order between the key dimensions of burnout. Thus, high levels of emotional exhaustion lead to high levels of cynicism or depersonalization [ 29 ]. Likewise, empirical studies indicate that exhaustion and depersonalization constitute the core or key dimensions of the syndrome of being burned out at work, while lack of professional fulfillment is considered as an antecedent of burnout or even a consequence [ 30 ].
Finally, although Maslach and Jackson’s [ 5 ] conceptualization of burnout remains the most widely accepted, other definitions or formulations are found in the scientific literature. For example, Salanova et al. [ 31 ] reformulate such approaches and propose an extended model of burnout composed of: (1) exhaustion (related to crises in the relationship between the person and work in general), (2) mental distance that includes both cynicism (distant attitudes towards work in general) and depersonalization (distant attitudes towards the people for and with whom one works) and (3) professional inefficacy (feeling of not doing tasks adequately and being incompetent at work).
2.1. Subtypes of Burnout
As an alternative to the unitary definition of burnout, Montero-Marín [ 24 ] proposes that this syndrome does not always develop in the same way and that, on the contrary, there can be three variations that depend on the dedication of workers to their work activity ( Figure 1 ). These subtypes could also be understood as stages in which there is a progressive deterioration in the levels of worker commitment to their job and have repercussions when choosing the intervention to be applied [ 32 ]. From this theoretical perspective, burnout is considered a developing condition, with a progressive reduction in levels of engagement, and evolves from enthusiasm to apathy [ 24 ]. Burnout is proposed to typically appear with the excessive involvement characteristic of the frenetic subtype. Since it is not easy to maintain this level of activity without becoming exhausted, the worker may adopt a certain protective distance. This distancing may relieve workers from overactivity, but at the cost of the frustration that emerges in the under-challenged subtype. In the long run, this leads to a reduced perception of efficacy, giving way to passive coping strategies, typically present in the worn-out subtype. The parallelism between the evolution of the syndrome and the different subtypes raises the possibility of implementing new lines of therapeutic intervention on burnout by understanding the subtypes as a succession of stages in the development of the syndrome [ 24 ]. Indeed, empirical studies suggest a progressive deterioration from the frenetic to the under-challenged and worn-out [ 33 ]. Nevertheless, more longitudinal studies are still needed to clarify the transition from one subtype to another and the evolution of the syndrome.

Profiles and subtypes of burnout.
The frenetic subtype is typical of work contexts with overload and workers who work intensely until exhaustion. It also tends to be more frequent in jobs with split shifts, temporary contracts and, in general, situations that force workers to be much more involved to keep the job. It is the subtype of burnout in which workers show greater dedication to work. At the motivational level, these workers show high involvement and need to obtain important achievements and it has been related to a coping style based on the attempt to solve problems actively, for which they use a high number of working hours per week or are involved in different jobs at the same time. For all these reasons, this profile is associated with high levels of burnout and a feeling of abandonment of personal life and health at work.
The under-challenged subtype is typical of monotonous and unstimulating professions, with repetitive, mechanical, and routine tasks that do not provide the necessary satisfaction to workers, who state that the work is not rewarding and is monotonous. Consequently, workers show indifference, boredom, and lack of personal development along with a desire to change jobs. This subtype of burnout is related to high levels of cynicism, due to a lack of identification with work tasks, and is associated with an escapist coping style, based on distraction or cognitive avoidance.
The worn-out subtype is characterized mainly by feelings of hopelessness and a sense of lack of control over the results of their work and recognition of the efforts invested, so that they finally opt for neglect and abandonment as a response to any difficulty. It is, therefore, the profile in which the worker shows less dedication. Thus, this type of profile is strongly associated with the perception of inefficiency and a passive style of coping with stress, based mainly on behavioral disconnection, which generates a strong sense of incompetence and makes them experience feelings of guilt.
2.2. Why Does Burnout Appear and How Does It Develop?
Since the appearance of the term in the scientific literature, several approaches have emerged that have attempted to answer the question of why burnout appears and how it develops. In this section, we will focus on detailing the most current and empirically supported explanatory theories of burnout considering that, instead of being antagonistic to each other, they are complementary and provide a more global view of this syndrome. Specifically, the following theories are summarized: (1) social cognitive theory; (2) social exchange theory; (3) organizational theory; (4) structural theory; (5) job demands–resources theory; (6) emotional contagion theory.
2.2.1. Social Cognitive Theory
This approach is characterized by giving a central role to individual variables such as self-efficacy, self-confidence and self-concept in the development and evolution of burnout [ 34 , 35 ]. So, this syndrome is triggered when the worker harbors doubts about their own effectiveness, or that of their group, in achieving professional goals [ 36 , 37 ]. These approaches were corroborated in a study conducted in a Spanish context with 274 secondary school teachers showing that burnout occurred after the emergence of professional efficacy crises [ 36 ].
The circumstances facilitate the development of inefficacy expectations or efficacy crises are the following [ 38 ]: (1) negative experiences of failure in the past, (2) lack of reference models who have gone through a similar experience and have overcome it, (3) lack of external reinforcement for the work, (4) lack of feedback on the work completed or excessive negative criticism, and (5) difficulties at work. In this way, crises of effectiveness would lead to low professional fulfillment which, if maintained over time, would generate emotional exhaustion and then cynicism/depersonalization as a way of coping with stress ( Figure 2 ).

Development of burnout according to the socio-cognitive theory of the self-efficacy.
2.2.2. Social Exchange Theory
This theory considers that burnout occurs when the worker perceives a lack of equity between the efforts and contributions made and the results obtained in their work [ 39 ]. This lack of reciprocity, which can occur with service users, colleagues, supervisors, and organizations, consumes the emotional resources of professionals, generating an emotional exhaustion that becomes chronic. From this approach, burnout can be triggered by the significant interpersonal demands involved in dealing with clients/users that become emotionally consuming. Thus, to avoid contact with the original source of discomfort, depersonalization or cynicism is used as a stress coping strategy, which ultimately leads to low personal fulfillment ( Figure 3 ).

Development of burnout according to social exchange theory.
2.2.3. Organizational Theory
This approach considers that burnout is a consequence of organizational and work stressors (see Section 3.1 ) combined with inadequate individual coping strategies [ 40 , 41 ]. Within this theory, there are two alternative models to explain the relationships between the dimensions of burnout. According to Golembiewski et al. [ 41 ], burnout starts because of the existence of organizational stressors or risk factors, such as work overload or role ambiguity, and before which some individuals show as a coping strategy a decrease in their organizational commitment, which is very similar to cynicism and depersonalization. Subsequently, the person will experience low personal fulfillment at work and emotional exhaustion, which triggers burnout syndrome. Thus, depersonalization would be the first phase of burnout, followed by a feeling of low self-fulfillment and, finally, emotional exhaustion. The alternative proposal is that put forward by Cox et al. [ 40 ]. For these authors, the emotional exhaustion caused by enduring work stressors is the initial dimension of this syndrome. Depersonalization is considered a coping strategy in the face of emotional exhaustion and low personal fulfillment is the result.
2.2.4. Demands–Resources Theory
This approach postulates that burnout occurs when there is an imbalance between the demands and resources derived from work [ 42 ]. Job demands are those job factors that require sustained physical or mental effort and are associated with certain physiological costs due to activation of the hypothalamic–pituitary–adrenal axis and psychological costs (e.g., subjective fatigue, reduced focus of attention, and redefinition of task requirements). Common work demands include work overload, emotional labor, time pressure, or interpersonal conflicts. When recovery in the face of such demands is insufficient or inadequate, a state of physical and mental exhaustion is triggered.
Work resources, on the other hand, refer to the physical, psychological, organizational, or social aspects of work that can reduce the demands of work and the associated physiological and psychological costs and that can be decisive in achieving work objectives. Resources at work can be organizational in nature, but also personal ( Table 2 ). When demands exceed resources, fatigue occurs; if this imbalance is maintained over time, fatigue becomes chronic and, finally, burnout appears. Therefore, job demands have a direct and positive relationship with burnout, especially emotional exhaustion, while the existence of job resources inversely influences depersonalization by minimizing or reducing its use as a coping strategy.
Summary of main demands and job resources.
| Job Demands | Job Resources |
|---|---|
| Temporary pressure Interpersonal conflicts with clients and colleagues Task complexity Job insecurity Unfavorable schedule changes Qualitative and quantitative work overload Personal occupational hazards | Technical knowledge and skills Socio-emotional skills Positive psychological capital (self-efficacy, optimism, hope and resilience) Creativity Time flexibility Job security Supervisor and peer support Material resources Autonomy Rewards |
2.2.5. Structural Theory
This approach maintains that burnout is a response to chronic job stress that appears when the coping strategies employed by the individual to manage job stressors fail. Initially, work stress will elicit a series of coping strategies. When the coping strategies initially employed are not successful, they lead to professional failure and to the development of feelings of low personal fulfillment at work and emotional exhaustion. Faced with these feelings, the subject develops depersonalization attitudes as a new form of coping. (The sequence is illustrated in Figure 4 .) In turn, burnout will have adverse consequences both for the health of individuals and for organizations. This model has been empirically contrasted with different professional groups such as teachers or nurses [ 43 ].

Development of burnout according to structural theory.
2.2.6. Theory of Emotional Contagion
Emotional contagion refers to the tendency to automatically imitate and synchronize facial expressions, vocalizations, postures, and movements with those of other people and, consequently, to converge emotionally with them [ 44 ]. When people work together, it is common for them to share situations and experience collective emotions, such as sadness, fear, or exhaustion. Therefore, from this theory it is considered that burnout occurs in work groups, since there are shared beliefs and emotions that are developed throughout social interaction [ 38 ]. This burnout contagion has been evidenced especially in teaching and health personnel [ 45 ], as well as between spouses (outside work). Thus, emotional contagion influences the development of burnout both inside and outside the workplace [ 26 , 46 ].
3. What Circumstances Trigger Burnout?
The antecedents are those aspects that are going to propitiate, trigger, and/or maintain people suffering from burnout syndrome. In general, these aspects can be classified into two broad categories: (1) organizational factors such as, for example, the workload or the emotional demands involved, and (2) individual factors such as, for example, the worker’s personality or coping strategies. It is important to emphasize that this syndrome is primarily a consequence of exposure to certain working conditions and not an individual characteristic such as a personality trait. Strictly speaking, therefore, the triggers of burnout would be factors related to the work (be it content, structure or relationships with users, clients, bosses, and/or colleagues). However, it is considered that, although organizational factors are capable per se of generating burnout, certain individual factors would act as moderating variables. Thus, personal aspects such as, for example, a lack of self-confidence or the use of stress-avoidance coping mechanisms could play a role in enhancing situational factors. On the other hand, other individual characteristics, such as optimism or active coping, can lessen or even slow down the negative effect of organizational factors on burnout and its consequences.
3.1. Organizational Factors
Regarding situational factors, reviews of the scientific literature [ 47 ] show that, in general, both the type of tasks, the way they are organized and the relationships between colleagues, bosses, and/or clients are potential burnout triggers or risk factors.
3.1.1. Work Overload
Workload, both quantitative and qualitative, when excessive, requires sustained effort, generating physiological and psychological costs. Such symptoms can trigger the experience of burnout and psychological distancing from work as a self-defense mechanism [ 48 ].
3.1.2. Emotional Labor
Emotional labor is understood as the psychological process necessary to self-regulate one’s emotions and show those emotions desired by the organization. It involves controlling or hiding negative emotions such as anger, irritation or discomfort to comply with the rules or requirements of the organization and objectives of the job, as well as the display of emotions not felt, such as sympathy towards customers or users, although the opposite is really felt, or tranquility in situations in which what is really felt is fear. Emotional labor will therefore involve a greater workload. In this sense, several studies have shown positive relationships between emotional labor and burnout in different professions, such as teachers [ 49 ] and HR department workers [ 50 ].
3.1.3. Lack of Autonomy and Influence at Work
Lack of freedom at work when performing tasks, as well as the inability to influence decisions that affect work has been positively associated with higher levels of burnout. Conversely, when workers experience autonomy and control over their work, there are lower rates of burnout and higher rates of professional fulfillment [ 48 ]. In this line, several investigations have found negative relationships between burnout and empowerment, so that the greater the empowerment perceived by workers, the lower the levels of burnout experienced [ 51 , 52 ].
3.1.4. Ambiguity and Role Conflict
When the worker does not know what is expected of them and/or does not have enough information about their mission (role ambiguity) or in their case the different tasks and demands to be fulfilled are incongruent or incompatible with each other (role conflict), burnout levels are increased [ 53 ].
3.1.5. Inadequate Supervision and Perception of Injustice
The perception of inadequate supervision (e.g., excessively directive, and unfair by only focusing on the negative aspects without valuing achievements and efforts, or at the other extreme not at all directive or non-existent) increases the risk of developing burnout. On the contrary, a fair treatment with employees favors the increase in available resources, exerting a negative effect on emotional exhaustion in such a way that workers are less likely to develop burnout symptomatology [ 54 ].
3.1.6. Lack of Perceived Social Support
Lack of social support at work, either from co-workers or supervisors, as well as internal conflicts between co-workers are considered important triggers of burnout. On the contrary, social support has been found to act as a brake on this syndrome [ 55 ].
3.1.7. Poor Working Hours
The working hours conditions that make it difficult to reconcile family and professional life are another important trigger of burnout. For instance, shift work, high rotations, night work, long working hours, or a large amount of overtime are powerful triggers of burnout. Additionally, such hourly characteristics are positively related to sleep disorders, heart problems, health complaints, job dissatisfaction, decreased attention and performance, as well as an increased risk of accidents [ 48 ].
3.2. Individual Factors Modulating Burnout
Regarding individual factors, both personality traits and sociodemographic variables and coping strategies have been analyzed as predisposing or facilitating the development of burnout in the case of the presence of some of the organizational factors explained above. Table 3 summarizes these factors and their modulating effect on burnout: positive (they amplify the effect of social factors) or negative (they reduce the effect of social factors).
Individual burnout modulators.
| Protectors of Burnout | Enhancers of Burnout |
|---|---|
| Agreeableness Conscientiousness Extraversion Openness to experience Positive psychological capital Problem-focused coping | Neuroticism External locus of control Type A Personality Alexithymia Emotion-focused coping |
Personality influences how people perceive their work environment and, therefore, how they manage and cope with work demands and resources. Several studies [ 56 , 57 , 58 ] conclude that the personality traits posited in the Big Five model (extraversion, neuroticism, agreeableness, conscientiousness, and openness to experience; [ 59 ]) are significantly but differentially associated with burnout. Thus, it has been found that there is a negative correlation between extraversion and the components of burnout. Thus, extraversion will be a protective factor against burnout. As for neuroticism or emotional instability, positive correlations have been found with burnout. Therefore, people with less emotional stability will be more likely to suffer from burnout. Agreeableness is another personality factor that has shown a protective effect on burnout, so that more-agreeable workers tend to experience less burnout than their less-agreeable colleagues. Likewise, conscientiousness, or the tendency to behave responsibly and persistently, reduces the likelihood of burnout. Finally, openness to experience that represents aspects related to breadth of interests and creativity also has protective effects on burnout as it is positively associated with professional efficacy and negatively associated with depersonalization.
Other individual characteristics that influence the development of burnout are the external locus of control, the type A behavior pattern and having high expectations. Locus of control [ 60 ] refers to the degree to which people believe they have control over events and their lives (internal locus of control) and the degree to which they believe that events occur due to external causes such as chance or the decisions of others (external locus of control). The greater the external locus of control, the greater the probability of developing burnout, especially in ambiguous or novel situations, in which the persons believe they have little or no possibility of controllability. Type A behavior pattern is characterized by competitiveness, impulsivity, impatience, and aggressiveness, and has been widely implicated as a health risk factor. This behavior pattern is positively related to the emotional exhaustion and depersonalization factors of burnout. Finally, the expectations that employees have regarding their work are related to the level of burnout, such that higher expectations and higher goal setting lead to greater efforts and thus higher levels of emotional exhaustion and depersonalization [ 47 , 48 ]. The person’s level of involvement also seems to be important. Specifically, over-involvement has also been proposed as a potent trigger, especially when it may be impossible to achieve goals. This mismatch between expectations and realities can lead to frustration and burnout in workers.
In terms of sociodemographic variables, reviews of studies [ 47 , 48 ] point to an inverse relationship between age and burnout, such that people will experience lower levels of burnout as their age increases. However, the results are not always so consistent. A systematic review of the determinants of burnout [ 61 ] found a significant relationship between increasing age and increased risk of depersonalization, although on the other hand there is also a greater sense of personal accomplishment. Regarding gender, most studies indicate that emotional exhaustion and low professional fulfillment tend to be more common among women while depersonalization is more frequent in men. In relation to marital status, workers who are single (especially men) seem to be more exposed to burnout compared to those who live with a partner. However, such findings seem to be more appropriate in men, as in the case of working women, it constitutes an additional risk factor since working women are usually responsible for household chores and, therefore, this may pose a difficulty in reconciling personal and professional life.
Coping strategies are another variable that play an important role in the development of burnout [ 62 , 63 ]. Although there are several classifications of coping strategies, the most established one is the distinction between problem-focused coping and emotion-focused coping [ 64 ]. Problem-focused coping represents an attempt to act directly on the stressful situation, whereas emotion-focused coping focuses on modifying negative emotional responses to stressful events, avoiding intervening on them. Empirical evidence suggests that, in general, avoidance and emotion-focused coping are positively related to burnout, that is, they favor it, whereas active and problem-focused coping are negatively related to burnout, that is, they reduce it. However, not all emotion-focused coping strategies increase burnout, as social support-seeking, reappraisal, and religious support, in some cases, have protective effects on burnout [ 55 ]. On the other hand, it has also been proposed that the effectiveness of problem-focused coping may depend on the control that individuals can exert over potential stressors in the work environment. Specifically, the use of problem-focused active coping strategies when there is little possibility of controlling and/or changing environmental stressors may exacerbate the undesirable effects of work stress; in such situations it is more advisable to employ coping strategies to facilitate adaptation to the situation. Therefore, one cannot be blunt in concluding that emotion-focused coping strategies are always negative since problem-focused coping only seems adaptive in controllable situations, while avoidance-oriented coping is adaptive in situations that are difficult to control [ 65 ].
3.3. Future Research
This section has focused on summarizing the main triggers of burnout. However, since burnout symptoms develop and evolve differently depending on individual characteristics (e.g., personality or coping strategies) and the work environment (e.g., job demands or leadership styles), it is necessary to continue advancing the knowledge of which are the personal factors that in combination with certain contextual triggers produce greater or lesser symptomatology. For example, when faced with the same stressor, do all personality types experience the same symptoms and consequences? Which personalities are more vulnerable to developing burnout when faced with specific triggers? Which are the most potentially harmful combinations of individual characteristics and contextual triggers? And which are the least? From a temporal perspective, it would also be necessary to carry out more longitudinal studies to study the evolution of symptomatology.
Finally, and because of the increase in home working during the COVID-19 pandemic, it would also be interesting to examine whether teleworking may cause a greater or lesser occurrence of this symptomatology, compared to face-to-face work, as well as to examine possible differences depending on the sector of activity.
4. Consequences of Burnout
Burnout results in a series of adverse consequences both for the individuals who suffer from it and for the organizations in which these professionals work. These consequences are initially of a psychological nature, but maintained over time, they translate into adverse effects on the physical/biological health and behaviors of workers, which in turn will have undesirable organizational consequences [ 66 ].
4.1. Psychological Consequences
The psychological alterations generated by the syndrome of being burned out at work occur at both cognitive and emotional levels. Different studies have associated this syndrome with concentration and memory problems, difficulty in making decisions, reduced coping capacity, anxiety, depression, dissatisfaction with life, low self-esteem, insomnia, irritability and increased alcohol and tobacco consumption [ 66 , 67 ]. Other researchers have also shown that this syndrome can pose a significant risk of suicide [ 68 ].
4.2. Health Consequences
Several reviews of studies conclude that employees with higher levels of burnout are more likely to suffer from a variety of physical health problems such as musculoskeletal pain, gastric alterations, cardiovascular disorders, headaches, increased vulnerability to infections, as well as insomnia and chronic fatigue [ 69 ]. Burnout has also been found to dangerously increase blood cortisol levels [ 70 ] and constitutes an independent risk factor for type 2 diabetes [ 71 ]. Now, the way these symptoms manifest themselves is not the same in all individuals, nor do they all have to occur.
4.3. Behavioral Consequences
In addition to physical and psychological health problems, in general, burnout is also directly related to job dissatisfaction [ 72 ], low organizational commitment [ 66 ], increased absenteeism [ 73 ], turnover intention [ 74 ], and reductions in performance [ 47 ]. On the other hand, some employees with burnout syndrome may justifiably leave their job; however, others decide to remain working [ 75 ]. This may lead to work presenteeism (i.e., individuals go to work, although they do not really fulfill their responsibilities due to health issues). In addition, burnout can lead to deviant and counterproductive behaviors in workers, aggressiveness among colleagues and towards users, alcohol and psychotropic drug use, misuse of corporate material, or even theft [ 68 , 69 , 75 , 76 ].
However, the form and evolution of these individual consequences (psychological, health, and behavioral) is not the same in all cases. In this sense, and although it is not always easy to delimit them, four levels of burnout syndrome have been described [ 77 ]:
- Mild: those affected have mild, unspecific physical symptoms (headaches, back pain, low back pain), show some fatigue, and become less operative.
- Moderate: insomnia, attention and concentration deficits appear. At this level, detachment, irritability, cynicism, fatigue, boredom, progressive loss of motivation, making the individual emotionally exhausted with feelings of frustration, incompetence, guilt, and negative self-esteem.
- Severe: increased absenteeism, task aversion and depersonalization, as well as alcohol and psychotropic drug abuse.
- Extreme: extreme behaviors of isolation, aggressiveness, existential crisis, chronic depression, and suicide attempts.
4.4. Organizational Consequences
The negative consequences experienced at the individual level by workers with burnout translate into low motivation and performance that can extend to the work unit and the organization, causing a reduction in the quality of services [ 78 ]. Likewise, employees suffering from burnout influence the rest of the organization, causing greater conflicts or interrupting work tasks, thus reducing production and increasing production times [ 67 ]. Therefore, as indicated in the emotional contagion theory, burnout can cause a “contagion effect”, generating a bad working environment [ 45 ]. This syndrome also usually generates significant economic losses as a consequence of absenteeism, loss of efficiency and counterproductive behaviors [ 76 ].
4.5. Future Research
It would be interesting to examine in depth the relationships between the psychological alterations caused by burnout and the effects on workers’ health, safety, and performance. For example, how psychological damage caused by burnout influences workers’ attitudes and behavior, and exploration of the possible modulating role of individual factors and certain organizational characteristics (i.e., leadership, organizational climate, cohesion among workers). In addition, longitudinal studies would be necessary to analyze the possible relationship between the different consequences of burnout and productivity.

5. Prevention Strategies
Now we have established what burnout is and what circumstances trigger it, in this section we will focus on how to act both to avoid and to reverse its occurrence and consequences. First, the most appropriate type of preventive intervention should be selected. Primary prevention is aimed at all workers and its purpose is to reduce or eliminate organizational risk factors to prevent the occurrence of burnout. Primary prevention is the most consistent with the principles of an occupational risk prevention management system by providing workers with adequate support, job adaptations, information, and adequate training to deal with this psychosocial risk.
Secondary prevention, on the other hand, is carried out once the first symptoms of burnout have appeared, so it is not aimed at all workers, but only at those who are already affected and its purpose in general is that such symptoms do not evolve further, improving the way in which the person responds to these stressors. These interventions are aimed more at individuals than at the organization, bringing about changes in attitudes and improving their coping resources, which does not imply that there are no organizational interventions as well. Finally, tertiary prevention focuses on employees who are already burned out at work. The aim of this type of prevention is to reduce the most severe harms (e.g., serious health problems and/or poor job performance). Since this type of intervention is aimed at trying to resolve the damage to the worker’s physical and/or psychological health, it is considered reactive and not strictly speaking prevention, but treatment.
From another perspective, we will classify the interventions considering the promoter of the intervention, that is, who organizes, decides and, if necessary, finances the actions to be carried out. In this sense, interventions can be classified as follows: (1) promoted by the organization, which in turn could be subdivided into actions directed at the organizational and job structure and actions directed at employees, and (2) promoted by individuals, which could also be subdivided into interventions directed at oneself as an individual and interventions directed at improving one’s interaction with the organization and with aspects of the job ( Table 4 ).
Summary of burnout interventions.
| Promoted by the Organization | Promoted by the Worker | ||
|---|---|---|---|
| Aimed at the Structure | Aimed at Employees | Aimed at Oneself | Aimed at Aspects of the Job |
| Improvement of contents and workstations | Training | Physical exercise | Time management |
| Humanization of work schedules and implementation of work–life balance plans | Strengths-based interventions | Mindfulness training | Job crafting |
| Managers’ leadership development | Coaching and guidance | Self-assessment | |
| Use of non-financial rewards and incentives | Creation of support groups | Psychotherapy | |
| Development of welcome programs | |||
| Burnout monitoring and design of tailor-made plans | |||
| Institutionalization of the Occupational Health and Safety Service | |||
5.1. Organizational Interventions Aimed at Work Structure
The following is a description of interventions that generally focus on reducing work stressors and increasing the organizational resources available to workers [ 79 , 80 ].
- (1) Work redesign. This measure aims to partially change the objectives and tasks of the job while improving the quality of work by eliminating structural and/or procedural elements that interfere and generate stress [ 81 ]. It could also be considered job redesign the enrichment of jobs through the incorporation of new and more stimulating tasks that make the job more motivating and rewarding.
- (2) Modification of exposure times to potential stressors. This can be completed by reducing the time in which the worker is exposed to the most stressful elements of the job (such as, for example, attention to users or patients) through job rotation, or, if necessary, by performing other tasks or activities [ 82 , 83 ].
- Humanization of schedules and implementation of work–life balance plans. This intervention involves organizing and making work schedules and shifts more flexible to allow for the reconciliation of personal and professional life [ 84 ]. In this sense, variable work shifts and long working hours exceeding 8 h should be eliminated.
- Managers’ leadership development. Supervisor support and leadership is considered an important work resource capable of reducing burnout levels in employees. However, not all supervisors employ an adequate leadership style. In this sense, several studies have shown that authentic [ 54 ], transformational [ 85 ], and servant [ 86 ] leadership styles are related to decreased burnout and have positive effects on employees’ psychological resources [ 87 ]. For this reason, these are the leadership styles that should be developed and trained to avoid the occurrence of this syndrome. Additionally, the performance of leaders and specifically leadership behaviors should also be regularly evaluated by the individuals working with them to identify potentially adverse aspects that could trigger burnout.
- Use of rewards and incentives that are not only financial. Employees can be motivated by rewards that do not always need to be of a financial nature. Recognizing work well done is a very efficient way to increase workers’ motivation levels and prevent burnout [ 48 ]. As indicated previously, one of the factors causing efficiency crises, which in turn were triggers of burnout, was the lack of reinforcement and appraisal by supervisors. In addition to recognition of accomplishment, other types of rewards such as greater time flexibility (which can facilitate work–life balance) or protected time to achieve personally meaningful work goals can enhance well-being. In contrast, employing simple financial rewards may be less effective by encouraging overwork and pressure to achieve goals, which promote burnout.
- Development of welcoming programs. Since role conflicts and ambiguities are potential triggers of burnout, it is advisable for organizations to develop welcoming processes for new workers, where the mission of the position, tasks, and objectives to be fulfilled are explained with absolute clarity and they are progressively introduced to the most stressful elements of the job, always offering support from the supervisor or other colleagues [ 88 ].
- Burnout monitoring and design of customized plans. This consists of periodically conducting surveys and measurements of workers to “monitor” the organization’s burnout levels and compare the scores of workers according to units, location, position, supervisor, etc. (e.g., [ 89 ]). The aim is basically to identify the appearance of the first symptoms, thus preventing the syndrome from becoming chronic. It is important that, in addition to the levels of burnout, the organization identifies as precisely as possible the risk factors in the work environment that may be present to eliminate or minimize them. Additionally, since the specific way in which symptoms manifest themselves and which dimension is dominant varies in each work unit, to be effective it will be necessary to design interventions specific to the causes and consequences/symptoms identified.
- (1) Delivery of psychoeducational workshops on stress and burnout that can be scheduled in the same organization or by outsourcing the service.
- (2) Counseling services for workers with work-related problems. This action can be carried out within the organization or by outsourcing the service by referring the employee to a counseling specialist.
- (3) Referral to specialized health promotion services such as psychologists and medical specialists.
5.2. Interventions Promoted by the Organization Aimed at Employees
This type of intervention basically aims to increase the personal resources of employees to manage stressors at work, which in turn helps to reduce burnout levels.
Examples of training actions promoted by organizations to prevent burnout.
| Actions |
|---|
| Self-regulation and emotional management Development of other personal resources, such as resilience, self-efficacy, hope, and optimism Conflict management Work stress management Time management Job-specific technical skills Problem solving Teamwork |
Generic phases of strengths-based interventions.
| 1. Identification of Competencies | 2. Strengths Development | 3. Utilization of Strengths |
|---|---|---|
| They usually result in a list of the most relevant strengths. Performance appraisals and other tools such as questionnaires and strengths scales can be used for this purpose. | Organizations often set up training workshops and individual development programs in which individuals are encouraged to cultivate and refine their strengths by developing a concrete action plan. | An attempt is made to match the types of tasks to be performed with the strengths of the employees. |
- Coaching and guidance. These are non-directive methods that encourage employees to regain control of their emotional state and well-being on their own, so the coach/counselor will not “prescribe” any treatment. Instead, the coach/counselor will guide the employee to come up with (or with some assistance) coping strategies on their own [ 93 ]. This type of intervention is usually typical of secondary prevention, in the early stages of the syndrome, when it is assumed that the person still has the capacity to redirect it.
- Creation of support groups. Peer and team support has always been critical in helping professionals cope with the difficulties and challenges of day-to-day life. This support encompasses a wide range of activities, including the celebration of achievements or the creation of formal support groups. In this sense, organizations should incorporate activities into work processes that are conducive to such a sense of community as dedicating time to share ideas and knowledge about how to act and deal with day-to-day professional challenges [ 88 ]. Support groups refer to any group of coworkers, whether formal (expressly created by the organization) or informal (not created by the organization but arising spontaneously) that meet regularly to exchange information, give each other emotional support and/or solve work problems. What these groups have in common is that they offer recognition for work completed (even if objectives have not been achieved), comfort, help, and companionship. The primary objective of the support groups is to reduce the professionals’ feelings of loneliness and emotional exhaustion, as well as the exchange of knowledge to develop effective ways of dealing with problems. This intervention (e.g., two hours every two weeks) is one of the most widely employed interventions for intervening on burnout and its benefits have been repeatedly demonstrated [ 73 ]. While the creation of support groups is an individual focus intervention, in many cases it is encouraged by the organization, or should be.
5.3. Individual-Focused Interventions Promoted by the Individual
These types of actions are initiated and determined by the workers themselves and are aimed at improving their emotional and physical state completely outside the work environment, including physical exercise, mindfulness, self-assessment and, where appropriate, psychotherapy.
- Physical exercise. Several studies have shown the positive effect of physical activity as a moderating variable of the effects of burnout on the health of workers [ 94 , 95 ]. Physical exercise can be used in primary, secondary and, where appropriate, tertiary prevention.
- Mindfulness training. A systematic review [ 96 ] of various specialized databases published between 2008 and 2017 concluded that mindfulness practice is effective in reducing burnout syndrome, both in its total values and in those corresponding to its dimensions, mitigating the negative psychosomatic and emotional effects of the syndrome, and increasing other positive ones such as empathy or concentration.
- Self-assessment. This intervention involves the self-observation of possible signs that could point to burnout. The way to do this is, for example, by keeping a diary of stress symptoms and related events such as specific symptoms, thoughts, feelings, and ways of coping with them. On the other hand, in addition to this type of diary, it is also important to measure the degree of burnout with a properly validated test, such as those indicated in the following section, and to compare one’s own score with that of a reference group or with oneself over time.
- (1) Cognitive techniques: these are aimed at the individual reevaluating and restructuring their appreciation and vision of stressful or problematic situations, so that they can deal with these situations more effectively. This type of technique is useful because people perceive situations subjectively and individually and, therefore, in a biased way. Cognitive techniques are aimed at identifying and modifying errors in the perception of reality to influence the emotions they provoke and the behavior they trigger.
- (2) Physiological deactivation techniques: the aim of this type of technique is to teach the person mechanisms to control, through relaxation, the increased physiological activation and anxiety caused by stressful stimuli.
- (3) Training in healthy lifestyle habits: physical exercise, a balanced diet, and restful sleep can help to reduce the symptoms of burnout.
5.4. Individually Driven, Work-Focused Interventions
These interventions are also initiated and determined by workers, but in this case, they are aimed at improving the work environment.
- Time management. Employees who are at risk of burnout often feel that they lack the time to fulfill all their responsibilities or that they work long hours with no time for personal use and rest. Self-management of time consists of correctly planning one’s time by making efficient use of the time available, organizing tasks realistically, and delegating them when appropriate, as well as dedicating daily time for personal activities and recreation [ 79 , 80 ]. Although this intervention is promoted by each worker, to facilitate proper time management, organizations as indicated above can or should provide training and coaching actions to their workers [ 97 ].
Types of adjustments made with job crafting.
| Doing what is possible to develop professional skills and learn new things on the job. | Organizing work in such a way that it does not cause too much stress, is mentally less intense, as well as avoiding emotionally complicated situations with customers and colleagues and trying not to make difficult decisions at work. | Asking, if necessary, for help and feedback about the job from the supervisor and co-workers. | When an interesting project comes up, proactively offer to work on it, when there is little to do, offer help to co-workers and ask for more responsibility from the supervisor. |
5.5. Future Research
Evaluation research on the success or failure of intervention strategies aimed at preventing or containing burnout is stilled needed. The interventions presented in this section offer a general and broad view of how to deal with burnout. However, since this syndrome depends on and develops idiosyncratically according to personal factors as well as working conditions, future lines of research should focus on analyzing which are the most efficient interventions according to individual characteristics and situational triggers. In addition, it would be optimal to establish comparisons between different interventions aimed at both the individual and the organization level. Furthermore, it is necessary to analyze the possible interaction between interventions and whether the combination of several of them is potentiating, inhibiting, or redundant. Finally, it would also be interesting to establish longitudinal studies to detect which of these interventions are more effective in the long term.
6. Assessment and Measurement
When it comes to assessing burnout, several tools (scales and questionnaires) have been developed and validated in different countries. These tools can be classified into two broad categories: (1) generic instruments (i.e., instruments aimed at assessing the syndrome, without differentiating by professional occupations; the main difference between these instruments is the burnout theoretical model they consider and what other aspects, if any, they evaluate), and (2) specific instruments aimed at evaluating burnout in specific occupations (e.g., nurses, psychologists, physicians) or even out of job (e.g., sports, school and parental relationships). Table 8 shows the main instruments currently available for assessing burnout.
Instruments for assessing burnout.
| Maslach Burnout Inventory (MBI) Questionnaire for the Evaluation of Burnout Syndrome at Work (CESQT) Copenhagen Burnout Inventory (CBI) Oldenburg Burnout Inventory Burnout Clinical Subtypes Questionnaire (BCSQ-36/12) Burnout Assessment Tool (BAT) Shirom–Melamed Burnout Questionnaire (SMBQ) | Maslach Burnout Inventory-Human Services Survey (MBI-HSS) Brief Burnout Questionnaire Revised for nursing staff Physician Burnout Questionnaire Teacher Burnout Questionnaire Psychologist’s Burnout Inventory Burnout Questionnaire for Athletes School Burnout Inventory Parental Burnout Inventory |
6.1. Generic Instruments
Maslach Burnout Inventory (MBI; [ 5 ]). The most widely used and validated tool for measuring burnout. At first, this tool was designed exclusively to measure burnout in personnel in the care sector and was called the Maslach Burnout Inventory-Human Services Survey (MBI-HSS). However, research and epidemiological studies showed that burnout can occur in any occupation and sector of activity, and for these reasons Schaufeli et al. [ 99 ] developed the definitive tool, the MBI-GS (Maslach Burnout Inventory-General Survey), based on the previous one and applicable to all occupations and jobs. This instrument has 16 items distributed in three dimensions: emotional exhaustion, cynicism, and reduced professional fulfillment. Thus, high scores on these dimensions would be indicative of burnout. This tool has subsequently been validated in different cultural and work contexts, such as Spanish [ 6 ], Italian [ 100 ], French [ 101 ], Chinese [ 102 ], and Arabic [ 103 ], among others.
Questionnaire for the Evaluation of Burnout Syndrome (CESQT; [ 104 ]). The CESQT consists of twenty items that are grouped into four dimensions: (1) enthusiasm for work: this is defined as the individual’s desire to achieve work goals because it is a source of personal pleasure. Low scores in this dimension indicate high levels of burnout; (2) psychic burnout: this is defined as the occurrence of emotional and physical exhaustion because of work; (3) indolence or the presence of negative attitudes of indifference and cynicism towards the organization’s customers; and (4) guilt: this is defined as the appearance of feelings of guilt for the behavior and negative attitudes developed at work, especially towards people with whom work relationships are established. This instrument has two different versions: the main version (CESQT), which is applied to workers who work with people (e.g., psychologists, teachers, or doctors) and the “Professional Disenchantment” version (CESQTDP), which is administered to those workers who do not work in direct contact with people. Although this tool was originally designed in a Spanish context, throughout these years the CESQT has also had a great reception and a wide development in different countries. It has been translated, adapted and validated in Germany [ 105 ], France [ 106 ], Italy [ 107 ], Portugal [ 108 ], and Poland [ 109 ]. In Anglo-Saxon literature, the use of the CESQT is regularly cited as the Spanish Burnout Inventory (SBI; e.g., [ 110 , 111 ]), and alludes to the theoretical model from which it starts, highlighting that among its strengths is the fact of collecting a broader vision of burnout than other instruments by including the dimension of guilt [ 67 ]. The wide dissemination of the instrument and its quality as a psychological assessment tool has favored the American Psychological Association (APA) to include it in its database of psychological tests.
Copenhagen Burnout Inventory (CBI; [ 112 ]). This scale allows the assessment of context-free burnout. It is composed of three main factors: (1) personal burnout, (2) work-related burnout, and (3) client-related burnout.
Oldenburg Burnout Inventory [ 113 ]. This inventory was developed to measure burnout across various occupational groups and measures two dimensions of burnout: (1) exhaustion, which is the primary symptom of burnout, and (2) disengagement from work.
Burnout Clinical Subtypes Questionnaire (BCSQ; [ 114 , 115 ]). The questionnaire consists of 36 items and measures the different properties of each clinical subtype. Each subtype consists of several facets: involvement, ambition, and overload of the frenetic type; indifference, lack of development, and boredom of the under-challenged type; and finally, neglect, lack of acknowledgement, and lack of control of the worn-out type. This questionnaire was originally developed in Spain, but recently it has been validated for other cultures such as Latvia [ 116 ] and Germany [ 117 ]. In its short version (BCSQ-12), consisting of 12 items, only one subscale of each subtype is analyzed (i.e., overload, lack of development, and neglect).
Burnout Assessment Tool (BAT; [ 118 ]). This tool is based on an alternative, comprehensive conceptualization of burnout, and includes all relevant elements that are associated with burnout. The questionnaire contains 33 items and consists of the BAT-C and BAT-S. The BAT-C assesses the four core dimensions: (1) exhaustion, (2) cognitive, (3) emotional impairment, and (4) mental distance). The BAT-S assesses two atypical secondary dimensions that often co-occur with the core symptoms: (1) psychological complaints, and (2) psychosomatic complaints.
Shirom–Melamed Burnout Questionnaire (SMBQ; [ 119 ]). The instrument comprises 22 items which consists of the following sub-scales: (1) emotional exhaustion, (2) physical fatigue, (3) cognitive weariness, (4) tension, and (5) listlessness. Later development of the instrument resulted in the Shirom–Melamed Burnout Measure (SMBM; [ 120 ]), which included 14 item divided in three subscales; (1) physical fatigue, (2) emotional exhaustion, and (3) cognitive weariness.
6.2. Specific Instruments
Maslach Burnout Inventory-Human Services Survey (MBI-HSS; [ 5 ]). This is a 22-item survey, applicable to human services jobs, for instance, clergy, police, therapists, social workers, medical professionals. The MBI-HSS (MP), adapted for medical personnel, and MBI-Educators Survey (MBI-ES), adapted for educators, are available online at https://www.mindgarden.com/117-maslach-burnout-inventory-mbi (accessed on 26 December 2022).
Brief Burnout Questionnaire Revised for nursing staff [ 121 ]. This instrument is an alternative tool to the MBI-HSS (MP). The questionnaire comprises 21 items that evaluate not only the syndrome itself, but also its antecedents and consequences. These items are gathered into four factors: (1) job dissatisfaction, comprising four items; (2) social climate, made up of three items; (3) personal impact, made up of four items, and (4) motivational exhaustion, comprising four items.
Physician Burnout Questionnaire-PhBQ [ 122 ]. This is another alternative instrument to the MBI-HSS (MP). The PhBQ contains 17 items and includes four subscales: burnout syndrome (PhBSS), antecedents (PhBAS), consequences (PhBCS), and personal resources (PPRS).
Teacher Burnout Questionnaire [ 123 ]. This questionnaire examines the burnout of teachers and is based on Maslach, Jackson and Leiter’s original instrument ([ 28 ]). The questionnaire comprises 14 items.
Psychologist’s Burnout Inventory—PBI [ 124 ]. This instrument measures four factors related to burnout among psychologist: control (three items assessing control over work activities, schedule, and decisions), overinvolvement (three items assessing feelings of responsibility for and spending time thinking about or dealing with clients), support (three items assessing emotional and instrumental support from colleagues), and negative client behaviors (six items assessing the experience of aggressive, dangerous, or threatening client behaviors). A revision of this instrument (PBI-R) was developed by Rupert et al. [ 125 ].
Athlete Burnout Questionnaire [ 126 , 127 ]. This tool is adapted to sport environments, and it is composed of 15 items organized in three dimensions: emotional/physical exhaustion, reduced sense of accomplishment and devaluation.
School Burnout Inventory-SBI [ 128 ]. This inventory comprises nine items grouped in three dimensions: (a) exhaustion at school, (b) cynicism toward the meaning of school, and (c) sense of inadequacy at school.
Parental Burnout Inventory [ 129 ]. This instrument assesses parental burnout syndrome, including exhaustion, distancing, and inefficacy.
6.3. Future Research
The main objection that could be made to the questionnaires presented above is that they are self-reported measures that focus especially on quantifying the burnout factors (emotional exhaustion, cynicism, and professional efficacy). However, since the burnout phenomenon is complex, more tools should be designed that consider both the antecedents and the physical and psychological consequences of burnout, thus offering a more global vision of this syndrome. As noted by Shirom [ 130 ], burnout measures should be analyzed within the framework of theoretical models that also consider causes and effects of burnout, as well as correlates. This type of instrument would, in turn, allow the development of more individualized and personalized interventions and treatments.
Moreover, different theoretical conceptualizations of burnout have led to the proliferation of a wide range of measurement instruments, usually comprising several dimensions. To what extent these instruments overlap or encompass different constructs remains to be seen. As a consequence, the burnout definition applied translates into considerably different burnout prevalence estimates in the literature. Furthermore, while some researchers use a unidimensional measure of burnout, others focus on one or more dimensions. Additionally, most instruments also lack a clinically validated threshold or cutoff values for burnout diagnosis.
Future lines of research could focus on examining the relationships between self-report measures of burnout and objective biological markers (i.e., salivary cortisol) to identify which questionnaires have the highest predictive capacity for these biomarkers. In addition, adaptation and validation of the main measurement instruments to different cultural contexts is still an ongoing need.
7. Special Issue on “Occupational Stress and Health: Psychological Burden and Burnout”
This Special Issue includes 21 papers which bring together recent developments and studies in this field. It aims to provide a comprehensive approach to occupational health from a broad range of perspectives. The results are of use for both researchers and practitioners. Undoubtedly, the COVID-19 pandemic has impacted organizational contexts increasing the risk of stress and burnout. Burnout and stress are analyzed from different perspectives with a focus on specific occupational groups in diverse countries from several continents. Post-Traumatic Stress Disorder (PTSD) in the Military Police of Rio de Janeiro (Brazil) is investigated as well as its correlations with socio-demographic and occupational variables [ 131 ]. Gender and age differences in personal discrimination experience, burnout, and job stress among physiotherapists and occupational therapists are examined in South Korea [ 132 ]. Nurses in South Korea are further studied with respect to emotional labor, burnout, turnover intention, and medical error levels within the previous six months [ 133 ]. Healthcare workers are also the focus of another study in Japan [ 134 ], which concludes that the number of physical symptoms perceived are positively related to burnout scores. Moreover, job strain and work–family conflict are associated with an increased risk of burnout, while being married, being a parent, and job support are associated with a decreased risk of burnout. In Spain, the relationship between burnout, compassion fatigue, and psychological flexibility is analyzed in geriatric nurses [ 135 ] as well as the prevalence of emotional exhaustion, depersonalization, and possible non-psychotic psychiatric disorders in nurses during the COVID-19 pandemic [ 136 ]. In Germany [ 137 ], teachers and social workers are surveyed following a model derived from the Job Demands–Resources theory to predict effects of strains on burnout, job satisfaction, general state of health, and life satisfaction. While some professionals working in the educational sector are burned out, other develop resilience, and thus it is important to identify antecedents and profiles (e.g., support), as evidenced by another study carried out in Spain [ 138 ]. Burnout and job satisfaction are additionally examined in a sample of music therapists in Spain [ 139 ]; a higher risk of burnout is associated with working longer hours in a palliative care setting.
Although a variety of instruments have been developed and validated in different contexts, new reliable and more specific tools are timely and highly valuable to better operationalize and understand job burnout. In this line, a new scale to gauge the balance between risks and resources ( Balance ) is developed in three French-speaking countries and then longitudinally tested in several English-speaking countries [ 140 ]. Another instrument is developed to evaluate job resources and further explore the relationship between resources and psychological detachment [ 141 ]. To assess the added value of a joint use of two tools, Leclercq et al. [ 142 ] compare the diagnostic accuracy of a structured interview guide and a self-reported questionnaire, finding differences in sensitivity and specificity with implications in diagnosis and treatment. A systematic review analyses both subjective and objective measurement methods to study fatigue, sleepiness, and sleep behavior in seafarers [ 143 ]. Related to new ways to measure and study stress, the “Study on Emergency physicians’ responses Evaluated by Karasek questionnaire” (SEEK) Protocol [ 144 ] presents the design of a study protocol to examine well-being in emergency healthcare workers in order to assess and determine Karasek scores in a large sample size of emergency healthcare workers and evaluate whether there is a change in work perception (both in the short and the long term). Additionally, this protocol will allow us to explore Karasek’s associations with some biomarkers of stress and protective factors.
The identification of mediators is another promising line of research. Mérida-López et al. [ 145 ] explore in a sample of pre-service teachers in Spain the mediator role of study engagement in the relationship between self- and other-focused emotion regulation abilities and occupational commitment. A moderated-mediation model is used in China to examine the effect of perceived overqualification on emotional exhaustion, the mediating role of emotional exhaustion in the relationship between perceived overqualification and creativity, and the moderating role of pay for performance in the perceived overqualification–emotional exhaustion relationship. Occupational stressors are studied in China as mediators in the psychological capital–family satisfaction link [ 146 ]. In Brazil, the moderating role of recovery from work stress is explored in the relationship between flexibility ideals and patterns of sustainable well-being at telework [ 147 ].
Last, a growing avenue of research is devoted to leadership. Leaders’ behaviors have important consequences for both employees and organizations. In this Special Issue, ethical leadership is investigated in South Korea with respect to emotional labor and emotional exhaustion [ 148 ]. Identity leadership, team identification, and employee burnout are examined in 28 countries within the Global Identity Leadership Development (GILD) project [ 149 ]. Security-providing leadership is proposed to be a job resource to prevent employee burnout [ 150 ].
8. Conclusions
In this review, we have analyzed what burnout is, what are its main dimensions, what models have been proposed for the description and explanation of this syndrome, what are its antecedents and consequences, what tools allow its evaluation and how it can be intervened both at the organizational and individual level. We also present our critical vision, indicating how each specific aspect should be studied today, the future lines of research on burnout, and what the future lines of intervention in organizations should be. The most recent research published in the Special Issue on “Occupational Stress and Health: Psychological Burden and Burnout”, 21 papers, is summarized according to main areas.
There is no doubt that burnout is currently a growing concern for individuals, organizations, and society. For example, among physicians, this syndrome has reached epidemic proportions around the world, accompanied by alarming levels of depression and suicidal ideation [ 151 ]. Thus, people suffering from burnout report feeling exhausted throughout the day, and not only during their working day. In fact, just thinking about work before getting up in the morning leaves them exhausted.
Work environments with excessive work schedules and high levels of demands, as well as the need to prove that one is worthy of a certain position, leave workers emotionally drained, cynical about work, and with a low sense of personal accomplishment. Moreover, the pressure does not end with the end of the workday; new technologies, mobile devices and the lack of boundaries prevent disconnection and the necessary recovery from work.
However, burnout is not an inevitable syndrome; it can be prevented before it appears and treated during its development. Nonetheless, interventions often focus on individuals rather than organizations, even though the main causes of this syndrome are organizational factors such as work overload or role ambiguity. As Shanafelt and Noseworthy [ 88 ] point out, organizations should regularly assess the well-being of their workers, both quantitatively and qualitatively, and consider it a key performance indicator. In fact, it is likely that the relationship between burnout and job performance is underestimated because burned-out workers adopt “performance protection” strategies to maintain priority tasks and neglect low-priority secondary tasks such as, for example, dealing kindly with customers, clients, or patients [ 152 ]. In this way, evidence of the syndrome is masked until critical points are reached.
Author Contributions
Conceptualization, S.E.-V. and J.A.M.; writing—original draft preparation, S.E.-V., J.A.M. and A.L.; writing—review and editing, A.L. All authors have read and agreed to the published version of the manuscript.
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Conflicts of interest.
The authors declare no conflict of interest.
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.

Is This Depression or Burnout?
Stroll along this crosswalk to learn differences between depression and burnout..
Updated July 30, 2024 | Reviewed by Margaret Foley
- What Is Depression?
- Take our Depression Test
- Find a therapist to overcome depression
- Burnout and depression are often confused and difficult to tease apart.
- Relative to depression, burnout tends to be more specific to a situation or context, such as a work setting.
- Burnout may present with a different ratio of signs and symptoms (say, more cynicism) compared to depression.
What's the difference between depression and burnout ? The two are often challenging to tease apart, and confusing them can get in the way of finding solutions. In other words, differentiating the two isn't just an academic performance; there are real-world consequences.
In this blog post, I'll define each concept before comparing them.
As an aside, I don't include any comments on burnout and depression in relation to perfectionism —the primary theme of this blog and my book, Flawed: Why Perfectionism Is a Challenge for Management.
Depression is a syndrome characterized by many distinct aspects. It’s dimensional in that you can have none or a ton of severity, with every degree in between.
When you have enough signs and symptoms of a depressive episode and they're severe enough, you’re diagnosable with something called major depressive disorder (MDD) , a mental health condition. But very few presentations of MDD look the same.
What do I mean?
Fun fact—there are precisely 227 possible ways 1 for an MDD episode to present in a person. For an episode, you need five or more depressive symptoms, but at least one of two primary features are required. Which two features? A depressive episode requires at least one of either (a) sad mood or (b) anhedonia (pronounced "anne-heh-dough-nee-uh"). 2
An-he- what?
Anhedonia means a lack of pleasure or interest. Somebody with depression may lose interest in or lack pleasure from activities (e.g., writing blogs [GASP!], video games, sex , reading, socializing) that they normally enjoy or have enjoyed in the past.
I find it fascinating that you can have a depressive disorder but have zero sadness. That is, you can present with anhedonia but not sadness. Does that blow your mind? Depression doesn't always mean sad.
By the way, in some people, especially children, sadness can look a lot like irritability, and the anhedonia can resemble profound boredom (i.e., ennui , which is a super fun word to say and therefore feels opposite of its meaning).
The other symptoms/signs that can qualify you for an MDD episode include sleep disturbance; appetite changes (often based on weight fluctuations); low energy; changes in body movements, which can take opposite forms, such as slow (i.e., psychomotor retardation) or jittery movements (i.e., psychomotor agitation); feeling guilty or worthless; worsened concentration ; and increased suicidal thoughts or thoughts of death more generally. 3
So, as you can see, MDD can present with various combinations of signs and symptoms. By the way, this is called polythetic diagnostic criteria. New Scrabble word!
In addition, for many people, MDD is episodic—that is, you have episodes of depression that last for at least two weeks and come and go over a lifetime (with at least one month in between episodes). 4 Often MDD looks different from episode to episode, even for the same person. 5
Then, what is burnout?
Burnout is an unpleasant syndrome that occurs from stress. You tend to see burnout in high-pressure scenarios, such as work settings and caretaker roles. For example, it's not uncommon to see an election attorney become burnt out with their job during election season, when their stress level is skyrocketing. Similarly, burnout is a likely state for a 40-year-old single mother (of small children) who also happens to be caretaking for her father with advanced dementia . Society even has a cutesy/flippant name for this stressful life stage—the sandwich generation .
Burnout is characterized by different but connected dimensions: exhaustion; cynicism and disconnection; and decreased achievement. 6 "Exhaustion" refers to the feeling of being emotionally and physically depleted. You're running on empty. "Cynicism" and "Disconnection" refer to the social and mission components of burnout. You stop caring about the purpose of your involvement. You develop negative attitudes and exhibit irritability. You feel compelled to avoid and escape activities related to your role. "Decreased achievement" is the behavioral results of burnout. You stop or slow down engaging in tasks, which reduces production.
These burnout characteristics feed into each other and are therefore related. For mental health experts, this may sound familiar....
Burnout and Cognitive Behavioral Therapy (CBT)
If you're a psychologist who specializes in cognitive behavioral therapy (CBT) , you may see considerable overlap with the CBT triangle and conceptualization.

The CBT triangle depicts the interconnectedness of thoughts, feelings, and behaviors in a given situation. For example, in a stressful work situation, you might think that you'll never escape your new duties (i.e., thoughts), which then leads to feelings of frustration and guilt (i.e., feelings). This cascade may then result in withdrawing from your role and snapping at others (i.e., behaviors). The point of CBT is to shatter this cycle.
This discussion of CBT isn't a self-indulgent sidebar. The CBT triangle seems to parallel the different dimensions of burnout. It's not a perfect mapping, but it's pretty darn close.
First, burnout's "Exhaustion" maps on to CBT's "Feelings." Second, the "Cynicism" and "Disconnection" coincide with "Thoughts." Third and lastly, "Decreased achievement" parallels CBT's "Behavior."
Comparing Depression and Burnout: Similarities
Based on everything I've described, it's easy to see how burnout and depression can be confused. There are a lot of similarities.
In the figure below, I've created a crosswalk that shows similarities between burnout and depression. I make no claims about it being an exhaustive list, but it's a good place to start. (And for the record, I really wanted to use the Beatle's Abbey Road crosswalk cover for the figure but didn't want to deal with pesky rights issues.)
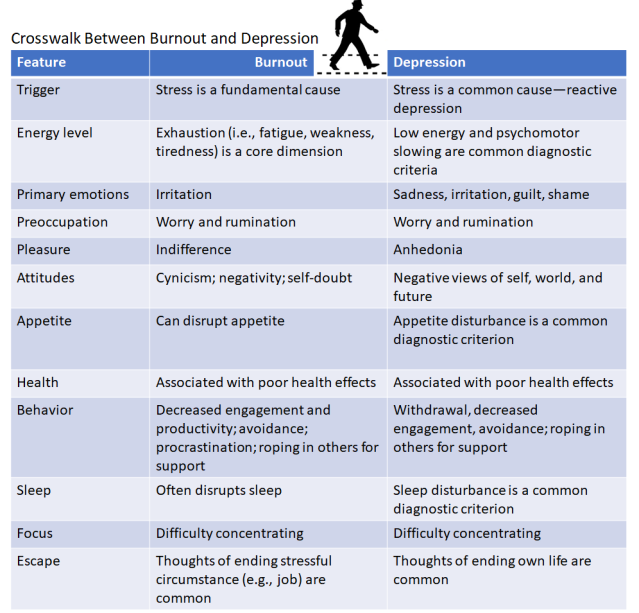
So, as you can see, there is considerable overlap between burnout and depression. Do they have any differences?
Comparing Depression and Burnout: Differences
Yes, depression can be the result of stressors—what we call reactive depression —but it can often occur in the absence of triggering stressors. When depression presents without commensurate situational stressors, we call this endogenous depression . This blog post predominantly focuses on reactive depression, as it's quite different from endogenous depression. 7
In addition, although burnout can result from multiple simultaneous stressors—and it often negatively affects multiple areas of life at the same time (such as in the workplace or at home)—its presentation is usually narrower than depression. That is, unlike with depression, the personal distress from burnout is mostly focused on one or two specific areas of life. It doesn't always generalize to other areas. For example, you might experience burnout with your job or as a caretaker, but you may feel fine at home with your family (or vice versa).
Depression doesn't respect these types of situational boundaries —it feels terrible in most situations and places.
For this reason, with burnout, many of the negative attitude components, such as self-doubt and cynicism, may be restricted to a specific setting or situation. For depression, it's more global. It sticks its tentacles in everything.
Although burnout and depression share some unpleasant emotions (e.g., irritation, sadness, and so on), predominant presentations in each seem to vary. Burnout may have a higher ratio of irritability relative to the other emotions.
Concluding Thoughts
Burnout and depression have many similarities and some differences. All told, it seems like these constructs tap into the same underlying phenomenon, perhaps one that we just haven't defined very well (yet!). This would suggest that third variables (e.g., neuroticism ) explain both.
Burnout also might be a narrow form of depression, a precursor to or cause of depression, the result of depression, or "Yes, all of the above." As with much of life and its causal dynamics, there's probably a feedback loop in which burnout and depression feed into each other. It's also worth noting that depression and burnout aren't mutually exclusive; you can have both simultaneously (fun times!).
I hope you feel more informed about burnout vs. depression. I'm burnt out on this blog post. Until next time...
1. Zimmerman M, Ellison W, Young D, Chelminski I, Dalrymple K. How many different ways do patients meet the diagnostic criteria for major depressive disorder? Compr Psychiatry. 2015 Jan;56:29-34. doi: 10.1016/j.comppsych.2014.09.007. Epub 2014 Sep 6. PMID: 25266848. ↩︎
2. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders . 5th ed., Text Revision, American Psychiatric Publishing, 2022, https://doi.org/10.1176/appi.books.9780890425787 . ↩︎
3. Ibid. ↩︎
4. Ibid. ↩︎
5. Klein DN, Shankman SA, Rose S. Ten-year prospective follow-up study of the naturalistic course of dysthymic disorder and double depression. American Journal of Psychiatry. 2006;163(5):872–880. ↩︎
6. Edú-Valsania S, Laguía A, Moriano JA. Burnout: A Review of Theory and Measurement. Int J Environ Res Public Health. 2022 Feb 4;19(3):1780. doi: 10.3390/ijerph19031780. PMID: 35162802; PMCID: PMC8834764. ↩︎
7. Shorter E. The doctrine of the two depressions in historical perspective. Acta Psychiatr Scand Suppl. 2007;(433):5-13. doi: 10.1111/j.1600-0447.2007.00957.x. PMID: 17280565; PMCID: PMC3712975.; Malki K, Keers R, Tosto MG, Lourdusamy A, Carboni L, Domenici E, Uher R, McGuffin P, Schalkwyk LC. The endogenous and reactive depression subtypes revisited: integrative animal and human studies implicate multiple distinct molecular mechanisms underlying major depressive disorder. BMC Med. 2014 May 7;12:73. doi: 10.1186/1741-7015-12-73. PMID: 24886127; PMCID: PMC4046519. ↩︎

Gregory Chasson, Ph.D., ABPP , is the author of Flawed: Why Perfectionism is a Challenge for Management , a clinical psychologist, and an Associate Professor at the University of Chicago.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Online Therapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Self Tests NEW
- Therapy Center
- Diagnosis Dictionary
- Types of Therapy

Sticking up for yourself is no easy task. But there are concrete skills you can use to hone your assertiveness and advocate for yourself.
- Emotional Intelligence
- Gaslighting
- Affective Forecasting
- Neuroscience
- Human Rights Policy
- A Constitution for the TMU newspaper “The Eyeopener”
- Board of Directors
- Stories We Broke
- Advertising
- Being an Eyeopener Source
- Volunteer With Us
- How To Pitch To Us

Toronto Metropolitan University's Independent Student Newspaper Since 1967
- Campus News
- Student Politics
- Arts & Culture
- Communities
- Business & Tech
- Fun & Satire
- Special Issues
Personal essay: The emotional burnout of being a POC hustler
For people of colour, our identities can be at odds with the world, but can also be our greatest strength, words by rhea singh, illustration by pernia jamshed.
S WE SAT in the kitchen at my friend Caitlin Mackavic’s Sweet 16 birthday party, we talked about things anyone would talk about in high school: upcoming exams, people we went to school with, overbearing parents. Eventually, we got to the topic of graduation. As a kid, I wanted to pursue a degree in fine art and by 15, I was set on graphic design. But a friend of Caitlin’s started talking about how she was going to pursue journalism at Boston University. We ended up talking about her future career for hours.
In my final two years of high school, I swapped my fine art course for a history course and piled on a French course to prepare myself. I researched how to structure features and news pieces to build my portfolio. I was going to make the switch to journalism. I eventually applied and was admitted to Ryerson’s journalism program in 2017.
Three years later, none of my art practices are in my life anymore. My canvas easel still sits in my parents’ garage, collecting dust and has been untouched since I was in Grade 9.
Once I got to Ryerson, and as time progressed, I got more overwhelmed and stressed about the degree I was pursuing, eventually feeling burnt out. I would constantly think whether or not this was the right program for me and if I was doing a good enough job compared to everyone else. For most of my first year, I felt as though I had made a mistake, and all those years of art in my life were flushed away just so I could get to Ryerson and feel lost.
I quickly learned that being a journalist of colour comes with an unspoken responsibility when reporting on marginalized communities—properly representing your community and proving you can make it through the trials and tribulations of being a person of colour (POC) in a predominately white industry.
These stressors agonize the feeling of wanting to give up. There’s an anxiousness that’s associated with how white reporters present your community and how you need to atone for the mistakes that others aren’t trained to fix. It makes you feel like you want to crash, hiding away to avoid these unspoken responsibilities.
But my burnout didn’t last forever. Eventually, I learned to take those factors that made me feel burnt out and use them to my advantage. I learned to love reporting on my community and to not only see it as a responsibility but a privilege as well. By embracing the platform that I have as a journalist, I can aim to produce a more accurate and in-depth story to be told that I wasn’t seeing in the media. This was also something I learned from Shree Paradkar.
In September 2019, Paradkar, a race and gender columnist at the Toronto Star , wrote about Maxime Bernier’s visit with The Star ’s editorial board . A photo circulated on Twitter of Bernier meeting with the national news outlet’s all-white board made up of three men and one woman. Paradkar wrote about how the few journalists of colour in The Star newsroom had to deal with being let down by their own employers’ decision.
“We didn’t have the luxury of shrugging or rolling our eyes. Many of us had deadlines, yet we had to take on the emotionally exhausting task of organizing and speaking up to explain to our management why this impacted us so viscerally.”
The first piece I ever wrote was in my first year, and it was about having Polycystic Ovarian Syndrome (PCOS) as a South Asian woman. In the Indian community, having children and a family is an integral part of the culture that is drilled into you at a young age. With PCOS comes infertility, which can clash with the communities’ underlying expectations.
As Paradkar says in her opinion piece, she as a columnist has the privilege of voicing her concerns. When my piece came out in first year, there was a sense of empowerment I felt in teaching people the realities of communities of colour. As stressful as it may seem to write about these issues, it creates a conversation that people are scared to delve into.
With these kinds of discussions, you open doors for reporters of colour to eliminate burnout and create content they can be proud of. Having this drive allows for more accurate and empathic reporting in those communities while also opening doors for newsrooms to introduce training when reporting on marginalized groups.
Identity in any given industry that is predominantly white can be anxiety-inducing due to the pressure of properly representing your community—especially when no one else does. This exists for journalists like me, but it also exists in other industries like television and film, fashion, music and any other storytelling or expressive kind of work.
WHEN IT COMES to being a POC artist, the narrative is very similar. For Rafa, her burnout doesn’t just stem from her art practices but from familial to financial responsibilities as well. This, she says, can make it hard to spend time in the art world itself.
“As an immigrant, I find myself trying to navigate between the values of community that I was taught growing up and the more western philosophy of individual growth,” she said.

But Rafa says this burnout doesn’t last forever and can be used to her advantage. For her, representing her identity through her art is her quiet revolution. As an artist, the fourth-year photography student says the most important part of making art is identifying with the land she was born in—the memories of her childhood and the stories of her people.
“I often feel unheard, unimportant [and] outnumbered in the art world, and creating a place for myself…makes me feel like I’m doing my part,” said Rafa.
In her art, there is a story of reconciliation. She said her identity will always be a part of her work, as it is a part of her existence.
“I am constantly going back and forth between my birthplace, trying to reconcile past and present me, trying to see different perspectives, how people live, what stories haven’t been told,” said Rafa.
Similarly to Paradkar, journalists across Canada are using the privilege and power they have to shift in conversation. Initiatives and groups have been created by journalists of colour themselves to combat these issues. Journalists for Human Rights (JHR) began an initiative called the North Ontario Initiative , working directly with Indigenous communities to accurately report on them. Additionally, the Asian American Journalist Association offers internship grants and scholarships to East and South Asian journalists, which can go up to USD $20,000.
Canadian Journalists of Colour —a Facebook group with over 600 members—allows for BIPOC journalists to have a supportive and safe environment to discuss story ideas and issues in the field, as well as helps young Black, Indigenous and POC journalists in navigating the industry. At Ryerson, “reporting on Indigenous issues” is a class offered for students in their third and fourth years, but the course remains optional.
Journalists of colour carry a heavy weight on their shoulders when it comes to representation, but the power we have as journalists enables us to do better by our communities and by ourselves.
Overcoming my burnout is something that took me a while to do, but once I did, I changed my whole perspective of reporting on my community. I don’t feel as though I owe it to my community to report on their struggles and achievements—I want to.

Share this:
- Click to share on Facebook (Opens in new window)
- Click to share on Twitter (Opens in new window)
- Click to share on Reddit (Opens in new window)
- Click to share on LinkedIn (Opens in new window)
- Click to share on Tumblr (Opens in new window)
TMU snaps losing skid at Winter Homecoming game
The TMU men's hockey team snapped their three game losing streak Friday at home
Second straight loss leaves Bold looking for change
The TMU men's hockey team lost its second consecutive game Saturday and are looking for change as they continue their season
Opportunity to host nationals ‘once in a lifetime’ for Bold
There’s still lots of hockey left to be played before TMU can look toward nationals in 2024
Read Next →

CopyRITE closes permanently on May 23

TMU faculty association passes motion to promote academic freedom in support of Palestine
Breaking: student alleges tmu director of community safety ‘grabbed’ and ‘pushed’ demonstrator at bog meeting, leave a reply cancel reply, read our latest issue:.

The Relationship Between Self-Determination and Burnout: Mental Health Outcomes in Medical Residents
- Find this author on Google Scholar
- Find this author on PubMed
- Search for this author on this site
- ORCID record for Hassan Moubarak
- ORCID record for Myriam El Khoury Malhame
- For correspondence: [email protected]
- Info/History
- Preview PDF
Background. Burnout is a pervasively increasing threat to personal and professional wellbeing and performance. It is yet understudied in relation to basic psychological needs (BPN), especially in at-risk population such as medical residents. This study intends to explore the differential relationship between various aspects of burnout including depersonalization (DP), emotional exhaustion (EE) and lack of personal achievement (PA) and subsets of BPN satisfaction or frustration namely autonomy, relatedness, and competence, with the framework of the Self-Determination Theory (SDT) in healthcare. Materials. A total of 110 medical residents in various Lebanese hospitals were included. Demographics and standardized scales were used to measure basic psychological need satisfaction and frustration (BPNSFS), burnout (MBI), depression and anxiety (PHQ-4). Residents were also asked about subjective evaluation of academic training and level of impact by ongoing crises (COVID-19 pandemic, Beirut port explosion and financial breakdown). Results. Result point to alarming prevalence of burnout and mental distress in our sample. It also indicates a differential correlation between gender, financial security and various subsets of burnout. It lastly points to association of DP with overall satisfaction scale (Beta=0.342, p=0.001) and PHQ-4 scores (Beta=-0.234, p=0.017), while feeling burdened to attend lectures and having been physically affected by the Beirut blast correlated with a sense of PA (Beta=0.332, p=0.010, Beta=0.187, p=0.041 respectively) and PHQ-4 (Beta=0.341, p=0.000), interacting with COVID-19 patients (Beta=0.168, p=0.020) and feeling protected in the working environment (Beta=-.231, p=0.002) showed a significant association with EE. Discussion. Within the SDT framework, this study highlights the complex interplay between collective crises, subjective evaluations or work conditions and other demographics with aspects of burnout in medical residents. It mostly points to the need address this at an individual but also an institutional level to buffer distress in future healthcare providers.
Competing Interest Statement
The authors have declared no competing interest.
Funding Statement
The author(s) received no specific funding for this work.
Author Declarations
I confirm all relevant ethical guidelines have been followed, and any necessary IRB and/or ethics committee approvals have been obtained.
The details of the IRB/oversight body that provided approval or exemption for the research described are given below:
Institutional Review Board at Lebanese American University (LAU.SOM.RC1.30/Dec/2020)
I confirm that all necessary patient/participant consent has been obtained and the appropriate institutional forms have been archived, and that any patient/participant/sample identifiers included were not known to anyone (e.g., hospital staff, patients or participants themselves) outside the research group so cannot be used to identify individuals.
I understand that all clinical trials and any other prospective interventional studies must be registered with an ICMJE-approved registry, such as ClinicalTrials.gov. I confirm that any such study reported in the manuscript has been registered and the trial registration ID is provided (note: if posting a prospective study registered retrospectively, please provide a statement in the trial ID field explaining why the study was not registered in advance).
I have followed all appropriate research reporting guidelines, such as any relevant EQUATOR Network research reporting checklist(s) and other pertinent material, if applicable.
Data Availability
The datasets used and/or analyses during the current study are available from the corresponding author on reasonable request.
View the discussion thread.
Thank you for your interest in spreading the word about medRxiv.
NOTE: Your email address is requested solely to identify you as the sender of this article.

Citation Manager Formats
- EndNote (tagged)
- EndNote 8 (xml)
- RefWorks Tagged
- Ref Manager
- Tweet Widget
- Facebook Like
- Google Plus One
Subject Area
- Psychiatry and Clinical Psychology
- Addiction Medicine (336)
- Allergy and Immunology (658)
- Anesthesia (177)
- Cardiovascular Medicine (2577)
- Dentistry and Oral Medicine (310)
- Dermatology (218)
- Emergency Medicine (390)
- Endocrinology (including Diabetes Mellitus and Metabolic Disease) (915)
- Epidemiology (12098)
- Forensic Medicine (10)
- Gastroenterology (744)
- Genetic and Genomic Medicine (4000)
- Geriatric Medicine (376)
- Health Economics (667)
- Health Informatics (2580)
- Health Policy (993)
- Health Systems and Quality Improvement (961)
- Hematology (357)
- HIV/AIDS (826)
- Infectious Diseases (except HIV/AIDS) (13579)
- Intensive Care and Critical Care Medicine (783)
- Medical Education (396)
- Medical Ethics (107)
- Nephrology (424)
- Neurology (3769)
- Nursing (207)
- Nutrition (559)
- Obstetrics and Gynecology (720)
- Occupational and Environmental Health (689)
- Oncology (1962)
- Ophthalmology (572)
- Orthopedics (233)
- Otolaryngology (301)
- Pain Medicine (248)
- Palliative Medicine (72)
- Pathology (469)
- Pediatrics (1090)
- Pharmacology and Therapeutics (453)
- Primary Care Research (442)
- Psychiatry and Clinical Psychology (3357)
- Public and Global Health (6435)
- Radiology and Imaging (1367)
- Rehabilitation Medicine and Physical Therapy (793)
- Respiratory Medicine (861)
- Rheumatology (394)
- Sexual and Reproductive Health (401)
- Sports Medicine (336)
- Surgery (434)
- Toxicology (51)
- Transplantation (185)
- Urology (164)
- Open access
- Published: 02 August 2024
Exercise, mental well-being and burnout in Thai medical students in 2020–2021: an online cross-sectional survey
- Dhachdanai Dhachpramuk 1 ,
- Suprapath Sonjaipanich 1 ,
- Supparat Theppiban 1 &
- Supinya In-iw 1
BMC Medical Education volume 24 , Article number: 837 ( 2024 ) Cite this article
126 Accesses
Metrics details
Introduction
Within the Thai medical curriculum, its rigorous education framework, demanding schedules and high academic standards can contribute to psychological distress. Regular physical activity has consistently shown positive effects on mental health. The aim of the study was to investigate the association between exercise and psychological well-being, including depression, anxiety, and burnout, in Thai medical students, and factors related to insufficient exercise and depression.
The cross-sectional study was conducted among medical students in the university hospital during 2020–2021. Participants completed self-administered questionnaires consisting of demographic data, Godin-Shephard Leisure-Time Physical Activity Questionnaire, depression screening (9Q), Thai General Health Question-28 (4 domains: somatic symptoms, anxiety and insomnia, social dysfunction, severe depression), and Maslach burnout inventory (Emotional exhaustion (EE), Depersonalization (DP), Reduced Personal Achievement (rPA).
Of the 404 participants, 50.5% were women, the mean age (SD) was 21.06 (1.8) years, and 52% were in clinical years. The prevalence of insufficient exercise was 59.6%, depression (30.2%), somatic symptoms (27.7%), anxiety (30.7%), insomnia (89.4%), social dysfunction (89.4%), high level of EE (32.4%), DP (21%), and rPA (56.7%). Insufficient exercise was associated with moderate to severe depression (OR 2.89, 95% CI 1.16–7.25), anxiety and insomnia (OR 1.56, 95% CI 1.01–2.43), social dysfunction (OR 2.51, 95% CI 1.31–4.78), burnout in part due to high rPA (OR 2.4, 95% CI 1.4–4.13), and study in clinical years (OR 1.91, 95% CI 1.28–2.87). After adjusted significant factors, only studying in the clinical year, social dysfunction, and burnout in part of rPA were related to insufficient exercise.
Conclusions
High rates of insufficient exercise, psychological challenges, and burnout were prevalent among medical students. To effectively address these issues, medical school should advise students to participate in regular exercise, promoting mental well-being and healthier lifestyles.
Peer Review reports
Mental health challenges, including depression, anxiety, and burnout syndrome, have seen an increase in prevalence on a global scale, particularly among individuals within the medical field [ 1 ]. A study highlighted that medical trainees, which encompass medical students, residents, and fellows, exhibited significantly elevated rates of mental health disorder, with occurrences being eight times for generalized anxiety disorder and five times for major depressive disorder which were higher than national averages [ 2 ]. Furthermore, the systematic review and meta-analysis focused on undergraduate medical trainees, revealing mental health problems and seeking psychiatric intervention [ 3 ]. Similarly, the previous studies among medical students demonstrated high prevalence rates of depression, mental disorders, burnout, sleep problems [ 4 ]. Among Thai medical students at a northern medical school, 11.1% had depression. Similarly, in a southern medical school, a 21.1% depression diagnosis rate was reported, with 12.5% reporting suicidality [ 5 , 6 ]. Moreover, one-third of fourth-to sixth-year medical students had poor mental health, while over half of them reported experiencing significant emotional exhaustion, despite the majority perceiving themselves as possessing a high degree of personal accomplishment [ 7 ]. These findings were consistent among six-year medical students across three medical schools [ 8 ]. It is noteworthy that both depression, mental health disorder, and burnout in medical students exceeded those within the general population [ 9 ]. The impact of these conditions on medical performance and attitude was also noted [ 10 , 11 ].
Exercise emerged as a potential avenue for enhancing mental well-being and performance [ 12 ]. The effects of exercise on mental health are attributed to its influence on neurotransmitters like noradrenaline, serotonin, and insulin-like growth factor-1 [ 13 ]. A comprehensive meta-analysis affirmed the efficacy of both aerobic and strength training exercises in alleviating depressive symptoms [ 14 ]. Medical students engaging in 30-minute fitness classes experienced diminished perceived stress and notable improvements in physical, mental, and emotional well-being compared to those who exercised individually or irregularly [ 14 ]. A study involving American obstetric residents revealed that regular exercise contributed to a reduction in health problem reporting. Of these residents, more than half had experienced mental health issues, and exercise emerged as an intervention for symptom relief [ 15 ]. Correlations were also established between self-reported mental health status among medical students and engaging in vigorous and regular physical exercise [ 16 ]. Consistent with these outcomes, two additional studies underscored the positive impact of regular exercise on medical students’ physical, mental, emotional well-being, and overall quality of life [ 16 , 17 ].
Explicitly investigating the relationship between exercise and mental well-being in Thai students is crucial due to the absence of previous research on the topic, particularly within the context of Thai medical students. Despite conducting a thorough literature review, no studies have been found that specifically examine the link between exercise, psychological well-being, and burnout among Thai medical students. Therefore, the primary objective of this study was to investigate the association between exercise and psychological well-being, including depression, anxiety, and burnout, in a Thai medical student population. The secondary objective was to study factors related to insufficient exercise and depression. The authors hypothesized that medical students who participated in regular exercise would have a lower rate of depression, anxiety, and burnout.
The institutional review board committee in Faculty of medicine Sirriaj hospital, Mahidol University, approved the study. All experiments were performed in accordance with relevant guidelines and regulations. Medical students, in the 2020–2021 academic years were invited to participate in the study. Faculty of Medicine Sirriaj hospital is one of Thailand’s oldest and largest hospitals. It has the highest number of patients and medical trainees among all medical schools in the country. Exclusion criteria were medical students with diagnoses of mental illnesses as major depressive disorder, anxiety disorder, and other psychiatric conditions. The sample size for this cross-sectional analysis was determined using a 52.8% proportion of insufficient exercise from the previous study [ 18 ], with a 95% confidence interval and a 5% margin of error. It was determined that a minimum of 383 participants was required for this study.
The electronic informed consent was obtained after explaining the study process to the participants following the hybrid lecture in the classrooms. Participants are recruited by scanning QR codes on posters or images. Prior to accessing the online questionnaires and informed consent forms within the QR codes using Google Forms, researchers provide information about the research objectives to medical students during various classroom sessions, without any academic impact. Confidentiality is maintained to ensure anonymity, and participation is voluntary. The participants were not obligated to provide their signatures, and they maintained the freedom to withdraw from the research at any point. Approximately 30% of respondents participated in the study, a proportion closely aligning with the calculated sample size.
Participants completed self-administered online questionnaires providing demographic data, Thai version of Godin-Shephard Leisure-Time Physical Activity Questionnaire (GSLTPAQ), 9 questions (9Q), Thai version of the Maslach Burnout Inventory-general survey (MBI), and Thai general health question 28 (Thai GHQ-28).
-GSLTPAQ was used to assess the level of exercise that was calculated with the intensity and frequency scores. The scores were categorized into in three levels; less than 14 units indicated insufficient exercise, 14–23 units as moderately active exercise, and more than 23 units signified active exercise [ 19 ]. Sensitivity and specificity values of Godin-Shephard Leisure-Time Physical Activity Questionnaire were 75.3 and 58.5%, respectively. Cronbach’s alpha coefficients the scale in adolescents was 0.84 [ 20 ]. Spearman correlation coefficient (r s ) between the Thai version and the English version of the GSLTPAQ was 0.95 [ 21 ].
The 9Q Thai version questionnaire consists of nine questions, each with rating scales ranging from 0 to 3 to indicate the increasing frequency of depressive symptoms. The optimal cutoff for 9Q scores is 7 or higher, with Cronbach’s alpha coefficients ranging from 0.78 to 0.82, a sensitivity of 86.15%, and a specificity of 83.12%. Scores ranging from 7 to 12 are defined as mild, 13 to 18 are classified as moderate, and scores of 19 or higher indicate severe [ 22 ].
The Thai GHQ-28 questionnaire assessed psychological well-being. This instrument displayed strong reliability and validity, with Cronbach’s alpha coefficients ranging from 0.86 to 0.95, and sensitivity and specificity ranging from 78.1 to 85.3% and 84.4–89.7%, respectively. It comprised 28 questions, categorized into four sections: somatic symptoms, anxiety and insomnia, social dysfunction, and severe depression. Each question had rating scales from 0 to 3 for the intensity of symptoms. Scores of more than 5 points for each part were interpreted as poor quality of life [ 23 ].
The Thai version of the Maslach Burnout Inventory (MBI), as translated by Sammawart S., underwent validation by experts and assessment of its reliability through the application of Cronbach’s alpha coefficient. The results of this analysis were segmented into three sections based on Cronbach’s alpha coefficients: Emotional Exhaustion (EE) 0.92, Depersonalization (DP) 0.66, and Personal Accomplishment (PA) 0.65. The questionnaire consisted of 22 questions in which the interpretation of each section employed distinct rating scales, categorizing participants into mild, moderate, and severe degrees. EE measured feelings of being emotionally overextended and exhausted by their study (Scores 0–16 are defined as mild, 17–26 as moderate, ≥ 27 as severe). DP an unfeeling and impersonal response toward patients (Scores 0–6 are defined as low, 7–12 as moderate, > 13 as high). PA measures feelings of competence and successful achievement in their work (Scores > 39 defined as low, 32–38 as moderate, and 0–31 as high) [ 24 ].
Statistical analysis
Demographic data were presented using numbers and percentage. The analytical focus included a range of variables, comprising demographic data, exercise categories, anxiety levels, depression, general health assessment, and burnout scores. The association between categorical variables was evaluated with Chi-square tests and Fisher’s exact test, where appropriate. A multivariable binary logistic regression model was used to examine factors related to insufficient exercise and to assess factors associated with depression. Results were presented in the form of odds ratios (OR) with 95% confidence intervals (95% CIs). We entered all significant results into the final model, adjusting for age and gender. P -values less than 0.05 are considered statistically significant with 80% power. We used SPSS statistical software, version 18 (SPSS, Inc., Chicago, IL, USA) for all analyses.
There were 404 participants who voluntarily participated in the study, and all completed the questionnaires. Of these, 50.5% were women. The average age was 21.06 ± 1.8 (range 17–26). Of the 404 participants, 194 (48%) were in their preclinical years, while 210 (52%) were in their clinical years. Regarding exercise, running was first rank for 44.1% of participants, followed by gym workout at 28.5%. More than half of the medical students (59.6%) did not meet recommended exercise levels. On average, participants spent 1.29 h exercising and 3.49 h using social media. (Tables 1 and 2 ) The prevalence of depression among medical students in the study was 30.2%, while burnout rates were high, with 64.3% reporting moderate to severe emotional exhaustion, and 82.4% facing moderate to severe reduced personal achievement. Social dysfunction affected 89.4%, and one third experienced anxiety and insomnia. Additionally, 59.4% reported poor sleep. (Table 3 )
The mental health problems associated with insufficient exercise were moderate to severe depression ( p = 0.018), anxiety and insomnia ( p = 0.047), social dysfunction ( p = 0.04), and burnout, in part due to reduced personal achievement ( p = 0.006). Additionally, academic year of medical students ( p = 0.001), self-reported poor quality of life ( p = 0.001) and older than 20 years ( p = 0.010) were more likely to be insufficient exercise significantly. According to mental well-being, medical students who feel depressed were more likely to burnout in all parts ( p = 0.01, p < 0.001, p = 0.032), and reported poor quality of life ( p = 0.006).
The multivariate analysis in Tables 4 and 5 shows that medical students who had insufficient exercise were more likely to have moderate to severe depression (OR = 2.89, 95%CI 1.16–7.25), anxiety and insomnia (OR = 1.56, 95%CI 1.01–2.43), social dysfunction (OR = 2.51, 95%CI 1.31–4.78), severe depression (OR = 1.91, 95%CI 1.01–3.58), high rPA (OR = 2.4, 95% CI 1.4–4.13), and study in clinical years (OR = 1.91,95%CI 1.28–2.87). After adjusting for all significant variables, social dysfunction, high rPA, and study in clinical years remained significant (OR 2.35,95% CI 1.21–4.57, OR 2.48, 95% CI 1.42–4.51,OR 1.94, 95% CI 1.28–2.94, respectively). Similar to those, depression was also related to studying in clinical years, having somatic symptoms, anxiety and insomnia, social dysfunction, and burnout except EE.
The study highlighted that medical students in the study who reported insufficient exercise demonstrated significant association with studying in clinical year, self-reported poor quality of life, moderate to severe depression, anxiety and insomnia, social dysfunction, and burnout in part of high reduced personal accomplishment. Our finding was similar to previous studies that physical exercise was inversely associated with mental health problems such as depression, anxiety, poor sleep quality, psychological distress and burnout [ 1 , 25 , 26 ]. Furthermore, a low level of exercise was associated with psychological distress such as burnout and depression among medical students [ 26 ].
In Thailand, medical schools provide a comprehensive six-year curriculum divided into two parts: the preclinical years (1st, 2nd, 3rd year) and the clinical years (4th, 5th, 6th year). In the 2nd year, the curriculum differs from the 1st and 3rd year of the preclinical years, emphasizing basic medical knowledge, laboratory classes, and frequent formative and summative assessments. Additionally, during the clinical years regarding to night shifts and the excessive workload, most medical students experience sleep deprivation, and a highly stressful environment. Consequently, they had less time available for regular exercise. More than half of the preclinical medical students managed their time on leisure activities, with the exception of 2nd -year medical students.
Insufficient exercise among medical students in the study was linked to increased levels of anxiety, insomnia, social dysfunction, and moderate to severe depression. This association can be attributed to the circumstances during the Covid-19 pandemic. Preclinical students studied from home, while clinical students faced social distancing measures and limited access to facilities, impacting their daily routines. Various studies have highlighted the pandemic’s adverse psychological effects on medical students [ 27 , 28 , 29 ]. They perceived themselves to be more stressed during clinical rotations and online education, which affected their learning and social life, ultimately leading to anxiety and depression [ 27 , 28 , 29 ]. Additionally, university students experienced reduced physical activity levels during the pandemic, coinciding with a higher prevalence of depression, anxiety, and stress [ 30 , 31 ].
The prevalence of depression in the current study was 30.2%, which was higher than the previous study but similar to the results of the systematic review and meta-analysis in earlier studies [ 3 , 4 , 32 ]. Depressed medical students reported somatic symptoms, anxiety and insomnia, social dysfunction, poor quality of life, and burnout. Moderate and severe depression were associated with insufficient exercise, consistent with earlier researches indicating that reduced physical activity related to higher rates of negative emotional conditions such as depression, anxiety, and stress [ 31 , 33 ]. Furthermore, medical students in the study experiencing depression was more likely to be studying in their clinical years and to report feelings of burnout. This result was similar to a previous study conducted in England, which stated that the majority of medical students who responded to the survey were exhausted [ 34 ]. In contrast to the previous study among medical students studying in Southern Thailand, it represented that pre-clinical year students experienced higher levels of depression and anxiety compared to clinical year students [ 32 ]. This trend may be attributed to various stressors, including the COVID-19 outbreak, online learning, virtual assessments, and reduced social interactions. During the COVID-19 pandemic, key stressors among Thai medical students included uncertainties regarding teaching modalities, concerns regarding potential system errors during exams, and the absence of clinical experience [ 35 ]. Practice during the clinical years was a significant factor related to psychological well-being, as well as over half of medical students reporting insufficient physical activity due to academic demands and shift work [ 36 ].
Burnout is a common issue among medical trainees, impacting their professional development, patient care, and personal well-being, including the occurrence of suicidal thoughts [ 37 ]. Burnout involved emotional exhaustion, depersonalization, and reduce personal accomplishment. Our study identified a significant correlation between reduced personal accomplishment and insufficient exercise, suggesting that students who felt less competent academically were less likely to engage in exercise. Furthermore, burnout in medical students were associated with unprofessional behavior, decreased patient care competence, and adverse effects on professional growth [ 37 ]. Strategies to improve burnout include increased social support, participating in recreational activities, hobbies, or exercise, to enhance coping skills. To reduce burnout and enhance mental health among medical students, it is imperative to promote healthy lifestyles that include regular exercise, adequate sleep, effective stress coping strategies, and fostering a positive learning environment.
The limitations of our study were considered. Firstly, it is important to note that our study design was cross-sectional, which means we could not establish causation or track longitudinal outcomes. Secondly, while our findings provide valuable insights into the specific group of the Thai medical students we studied, they may not represent all of the Thai medical students. Thirdly, the potential selection bias in our online survey suggests that participants who use social media might represent a specific subset of medical students, possibly seeking stress relief or having more available free time. This could impact the accuracy of mental health prevalence data in the study. As a result, we excluded individuals with mental disorders and other psychiatric conditions to reduce selection biases and provide more diverse demographic data.
Although the study possesses limitations, it contributes significantly to our understanding of the link between insufficient exercise and mental health among medical students. This underscores the importance of implementing targeted interventions. Key findings suggest the need for health guidance: monitoring quality of life, particularly during clinical years, and actively promoting healthy lifestyles characterized by regular exercise, adequate sleep, stress management skills, and a positive learning environment. Among medical students in Thailand, this study presented the association between insufficient exercise and mental well-being and burnout, enhancing our knowledge to prevent poor mental well-being or burnout with guidance not only on monitoring the quality of life, particularly among medical students in their clinical years, but also on emphasizing the fostering of healthy lifestyles. Such lifestyles are characterized by regular exercise, sufficient sleep, stress management skills, and a positive learning environment.
The recommendation for further study should include measuring the intensity of exercise, either by assessing cardiorespiratory fitness using a cardiopulmonary exercise test to measure percentages of maximal oxygen uptake (VO2max) or heart rate monitoring (HR), or by using metabolic equivalents to assess exercise intensity and estimate the energy expenditure of physical activities. Moreover, to gain a more comprehensive understanding, we advocate for the implementation of a multi-center cohort study that investigates the relationship between exercise and mental well-being, encompassing a more diverse sample. Such a study would produce more robust and widely applicable findings, ultimately contributing to the betterment of the broader medical field.
High rates of insufficient exercise, psychological challenges, and burnout prevailed among medical students. To effectively address these issues, medical schools should advise students to participate in regular exercise, which promote mental well-being and healthier lifestyles. Medical institutions must establish affirmative policies recommending active exercise to prevent burnout and encourage positive psychological outcomes. In addition, interventions to prevent burnout, such as coping strategies and self-motivation, should be integrated into the program as mandatory extracurricular activities.
Data availability
The datasets used and analyzed during the current study are available from the corresponding author upon reasonable request.
Grasdalsmoen M, Eriksen HR, Lønning KJ, Sivertsen B. Physical exercise, mental health problems, and suicide attempts in university students. BMC Psychiatry. 2020;20(1):175.
Article Google Scholar
Mousa OY, Dhamoon MS, Lander S, Dhamoon AS. The MD blues: under-recognized depression and anxiety in medical trainees. PLoS ONE. 2016;11(6):e0156554.
Rotenstein LS, Ramos MA, Torre M, Segal JB, Peluso MJ, Guille C, Sen S, Mata DA. Prevalence of Depression, depressive symptoms, and suicidal ideation among medical students: a systematic review and Meta-analysis. JAMA. 2016;316(21):2214–36.
Pacheco JP, Giacomin HT, Tam WW, Ribeiro TB, Arab C, Bezerra IM, Pinasco GC. Mental health problems among medical students in Brazil: a systematic review and meta-analysis. Braz J Psychiatry. 2017;39(4):369–78.
Phomprasith S, Karawekpanyawong N, Pinyopornpanish K, Jiraporncharoen W, Maneeton B, Phinyo P, Lawanaskol S. Prevalence and Associated factors of Depression in Medical students in a Northern Thailand University: a cross-sectional study. Healthc (Basel) 2022, 10(3).
Pitanupong J. The prevalence and Factors Associated with Mistreatment Perception among Thai Medical students in a Southern Medical School. Siriraj Med J. 2019;71:310–7.
Sathaporn K, Pitanupong J. Factors associated with the improvement of the empathy levels among clinical-year medical students in Southern Thailand: a university-based cross-sectional study. BMC Psychol. 2022;10(1):128.
Pitanupong J, Sathaporn K, Ittasakul P, Karawekpanyawong N. Relationship of mental health and burnout with empathy among medical students in Thailand: a multicenter cross-sectional study. PLoS ONE. 2023;18(1):e0279564.
Shawahna R, Hattab S, Al-Shafei R, Tab’ouni M. Prevalence and factors associated with depressive and anxiety symptoms among Palestinian medical students. BMC Psychiatry. 2020;20(1):244.
Dyrbye LN, West CP, Satele D, Boone S, Tan L, Sloan J, Shanafelt TD. Burnout among U.S. medical students, residents, and early career physicians relative to the general U.S. population. Acad Med. 2014;89(3):443–51.
Dyrbye LN, Massie FS Jr., Eacker A, Harper W, Power D, Durning SJ, Thomas MR, Moutier C, Satele D, Sloan J, et al. Relationship between burnout and professional conduct and attitudes among US medical students. JAMA. 2010;304(11):1173–80.
Singh A, Uijtdewilligen L, Twisk JW, van Mechelen W, Chinapaw MJ. Physical activity and performance at school: a systematic review of the literature including a methodological quality assessment. Arch Pediatr Adolesc Med. 2012;166(1):49–55.
Matta Mello Portugal E, Cevada T, Sobral Monteiro-Junior R, Teixeira Guimaraes T, da Cruz Rubini E, Lattari E, Blois C, Camaz Deslandes A. Neuroscience of exercise: from neurobiology mechanisms to mental health. Neuropsychobiology. 2013;68(1):1–14.
Silveira H, Moraes H, Oliveira N, Coutinho ES, Laks J, Deslandes A. Physical exercise and clinically depressed patients: a systematic review and meta-analysis. Neuropsychobiology. 2013;67(2):61–8.
Winkel AF, Woodland MB, Nguyen AT, Morgan HK. Associations between residents’ personal behaviors and Wellness: A National Survey of obstetrics and Gynecology residents. J Surg Educ. 2020;77(1):40–4.
Terebessy A, Czegledi E, Balla BC, Horvath F, Balazs P. Medical students’ health behaviour and self-reported mental health status by their country of origin: a cross-sectional study. BMC Psychiatry. 2016;16:171.
Yorks DM, Frothingham CA, Schuenke MD. Effects of Group Fitness classes on stress and quality of life of medical students. J Am Osteopath Assoc. 2017;117(11):e17–25.
Google Scholar
Al-Drees A, Abdulghani H, Irshad M, Baqays AA, Al-Zhrani AA, Alshammari SA, Alturki NI. Physical activity and academic achievement among the medical students: a cross-sectional study. Med Teach. 2016;38(Suppl 1):S66–72.
Wachirathanin P, Sriramatr S, Suporn S. Validity and reliability of questionnaires measuring leisure-time physical activity and factors of theory of planned behavior in adolescents. J Sports Sci Tech. 2014;14(2):177–85.
Shennar-Golan V, Walter O. Physical activity intensity among adolescents and Association with parent-adolescent relationship and well-being. Am J Mens Health. 2018;12(5):1530–40.
Sriramatr S, Berry T, Rodgers W. Validity and reliability of Thai versions of questionnaires measuring leisure-time physical activity, Exercise-Related Self-Efficacy, Outcome expectations and Self-Regulation. Pac Rim Int J Nurs Res. 2013;17:203–16.
Edwards WM, Coleman E. Defining sexual health: a descriptive overview. Arch Sex Behav. 2004;33(3):189–95.
Nilchaikovit T, Sukying C, Silpakit C. Reliability and validity of the Thai version of the General Health Questionaire. J PsychiatrAssoc Thai. 1996;41:2–17.
. 2560 [] (1. 2562) http://www.boe.moph.go.th/aids/Downloads/book/2560/13732_HIV_2560_for%20web.pdf
Ghrouz AK, Noohu MM, Dilshad Manzar M, Warren Spence D, BaHammam AS, Pandi-Perumal SR. Physical activity and sleep quality in relation to mental health among college students. Sleep Breath. 2019;23(2):627–34.
Wolf MR, Rosenstock JB. Inadequate sleep and Exercise Associated with Burnout and Depression among Medical Students. Acad Psychiatry. 2017;41(2):174–9.
Cao W, Fang Z, Hou G, Han M, Xu X, Dong J, Zheng J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020;287:112934.
Bachir B, Naji A, Tfayli A. The educational and psychological impact of the COVID-19 pandemic on medical students: a descriptive survey at the American University of Beirut. Med (Baltim). 2021;100(28):e26646.
Nishimura Y, Ochi K, Tokumasu K, Obika M, Hagiya H, Kataoka H, Otsuka F. Impact of the COVID-19 pandemic on the psychological distress of medical students in Japan: cross-sectional survey study. J Med Internet Res. 2021;23(2):e25232.
Gallo LA, Gallo TF, Young SL, Moritz KM, Akison LK. The impact of isolation measures due to COVID-19 on Energy Intake and physical activity levels in Australian University students. Nutrients 2020, 12(6).
Talapko J, Perić I, Vulić P, Pustijanac E, Jukić M, Bekić S, Meštrović T, Škrlec I. Mental Health and Physical Activity in Health-Related University Students during the COVID-19 pandemic. Healthc (Basel) 2021, 9(7).
Chootong R, Sono S, Choomalee K, Wiwattanaworaset P, Phusawat N, Wanghirankul N, Laojaroensuk P, Thongkhundum P, Saetang R, Euanontat S, et al. The association between physical activity and prevalence of anxiety and depression in medical students during COVID-19 pandemic: a cross-sectional study. Ann Med Surg (Lond). 2022;75:103408.
Carek PJ, Laibstain SE, Carek SM. Exercise for the treatment of depression and anxiety. Int J Psychiatry Med. 2011;41(1):15–28.
Farrell SM, Kadhum M, Lewis T, Singh G, Penzenstadler L, Molodynski A. Wellbeing and burnout amongst medical students in England. Int Rev Psychiatry. 2019;31(7–8):579–83.
Puranachaikere T, Hataiyusuk S, Anupansupsai R, In-Iw S, Saisavoey N, Techapanuwat T, Arunrodpanya F, Charonpongsuntorn C, Wiwattanaworaset P, Siripongpan A, et al. Stress and associated factors with received and needed support in medical students during COVID-19 pandemic: a multicenter study. Korean J Med Educ. 2021;33(3):203–13.
Wattanapisit A, Fungthongcharoen K, Saengow U, Vijitpongjinda S. Physical activity among medical students in Southern Thailand: a mixed methods study. BMJ Open. 2016;6(9):e013479.
Dyrbye L, Shanafelt T. A narrative review on burnout experienced by medical students and residents. Med Educ. 2016;50(1):132–49.
Download references
Acknowledgements
The authors gratefully thank all participants. We gratefully acknowledge Mr. Suthipol Udompunthurak for his assistance with the data analysis. Also, we would like to thank Dr. Mark Simmerman and Mr. Christopher Dulude for the English editing process.
Not applicable.
Open access funding provided by Mahidol University
Author information
Authors and affiliations.
Department of Pediatrics, Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok, Thailand
Dhachdanai Dhachpramuk, Suprapath Sonjaipanich, Supparat Theppiban & Supinya In-iw
You can also search for this author in PubMed Google Scholar
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by all authors. The first draft of the manuscript was written by Supinya In-iw and Dhachdanai Dhachpramuk. All authors commented on previous versions of the manuscript and approved the final manuscript.
Corresponding author
Correspondence to Supinya In-iw .
Ethics declarations
Ethics approval and consent to participate.
All methods were carried out in accordance with relevant guidelines and regulations. The informed consent was obtained from all subjects and their legal guardians.
All experimental protocols were approved by the Siriraj Institutional Review Board, Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok, Thailand. (COA No. Si 682/2020).
Consent for publication
The authors affirm that there are no individual data or images in the research study and we consent for publication.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Dhachpramuk, D., Sonjaipanich, S., Theppiban, S. et al. Exercise, mental well-being and burnout in Thai medical students in 2020–2021: an online cross-sectional survey. BMC Med Educ 24 , 837 (2024). https://doi.org/10.1186/s12909-024-05843-y
Download citation
Received : 25 September 2023
Accepted : 30 July 2024
Published : 02 August 2024
DOI : https://doi.org/10.1186/s12909-024-05843-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Medical students
- Mental well-being
BMC Medical Education
ISSN: 1472-6920
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Recommended

Inside Out 2: How new emotions mirror medical student struggles
The 2024 summer blockbuster film Inside Out 2 explores the complex emotions that first hit teenagers during puberty. Briefly, the five original emotions (from the first movie in 2015) that define the behavior of childhood Riley – Joy, Anger, Fear, Sadness, and Disgust – meet new emotions that allow Riley to grow further toward young adulthood. Unfortunately, the new emotions – Anxiety, Envy, Embarrassment, and Ennui – threaten to ruin long-standing friendships and make Riley more vulnerable to losing her sense of identity. As prehealth applicants, you likely have had to control these new emotions in preparing to become a student doctor. As health professions students, you probably experienced similar emotions when trying to impress others during your clinical rotations.
We will consider how the newer emotions contribute to your experience as a health professions student. I apologize for some plot spoilers. Throughout the article, “medical” school is meant to include other health professional education programs.
Taking control of Riley’s behavior, Anxiety helps Riley to make decisions that benefit her to avoid being a social outcast. In many cases, the decisions help her grow out of her comfort zone. However, Riley’s naive belief system (“I am a good person, I want to help people.”) becomes replaced by a belief of inadequacy (“I’ll never be good enough.”), and, at the climax, Riley experiences a panic attack that paralyzes her and endangers her health.
I’m admittedly understating the fact that anxiety dominates the mindset of most pre-health applicants (“ premed syndrome “). For years, students dread being rejected from their desired career path, and they fret about not getting the right professors for the right classes or missing out on extracurricular opportunities. They can become consumed with getting into medical school. As a result, anxiety drives students to develop a comprehensive checklist for success, anticipate every contingency for every unanticipated disaster, and look for ulterior motives in every optional secondary essay prompt.
Social concerns amplify the anxiety further: How can you fit into the culture of their new school, make the “right” friends, or get along with roommates? Can you leave positive impressions with faculty or other administrators and still be “cool” to your peers? Do people like you enough to get elected to a leadership position in a club or across your campus? Can I get into this selective organization (such as a Greek organization) despite all the initiation hoops I must jump through? Do I emulate “ effortless perfection ?” Can I find a date for the next formal? Am I exercising or meditating enough to stay calm (asked with irony)? If not, am I doomed to an eternity of regrets and failure?
Just wait until medical school ; if anything, the questions get more intense around making sure you pass your classes and avoid a remediation semester, find the “right” opportunity for a productive research record, or receive strong enough clerkship evaluations despite the brief exposure time to set up an application to a highly selective residency program (and thus get higher lifetime earnings). Other health professional programs share similar concerns as students seek employment or a post-graduate residency after graduation. First-generation health professions students or those from underrepresented communities may also bear the additional burden of wanting to succeed to represent and benefit their families or communities. Medical school is a crucible of stress that can transform or destroy you. Finally, there’s the dark cloud of student debt.
Pervasive among medical students around the world , anxiety often develops into depression, especially among vulnerable populations. Social isolation, like during the COVID-19 global pandemic lockdowns, further exacerbates feelings of isolation, anxiety, and depression . Students should take advantage of proactive strategies employed by schools, clinics, and hospitals to manage and mitigate the health challenges that could result from uncontrolled anxiety.
The adage “ comparison is the thief of joy ” summarizes the power of envy. Most who want to be doctors admire the mix of personal or community impact with altruism and selflessness shown by role models and mentors. Successful professionals lecture or mentor students, including significant benefactors who endow scholarships or new research facilities. Placing peers on pedestals for their outstanding grades, achievements, attractiveness, financial security, or offers of admission to brand/top-20 graduate programs may be additional fuel for motivation during the application process and health professions education.
But envy turns the admiration for the recognition of peers into an unhealthy obsession to place one’s needs or desire for acknowledgment above others. Sometimes, one may find satisfaction in seeing their peers fail (known as schadenfreude ). Empathy, compassion, and gratitude become victims to envy, and patient-centered care is replaced by provider/physician-centered ambition that sacrifices interprofessional teamwork and the patient’s welfare. This article lists some ways envy contributes to making decisions that are less professionally appropriate or contribute to burnout.
Embarrassment, the precursor to shame
Closely associated with “imposter syndrome” is embarrassment. Whether one is placed on the spot during a “pimping” session or misgendering a patient or peer, embarrassment humbles an individual who is exposed to making a mistake or showing their lack of complete preparation . Embarrassment may result when someone is reminded of more humble beginnings, as if they do not deserve the privilege of being a health care professional, so they suppress their connections to their home communities to “fit in” and be a perceived professional.
Keeping information private or confidential is also important in controlling embarrassment. Most do not want it known that they need or receive help because of the appearance of being impotent. One example is remediation due to failing an exam or a class; students can feel shame for having to be remediated, often something they have not experienced in their lives, and they may feel that their flaws are immutable . Those who feel such shame risk burnout or dropping out of school.
A culture rooted in dignity for others and self-care can be used to fight embarrassment . Finding constructive ways to discuss errors and correct mistakes can relieve providers’ self-doubt and build resilience and wisdom as part of their professional identity. By acknowledging that one does play a meaningful role in others’ lives and the performance of their team, students, residents, and providers can respectfully manage challenges and maintain appropriate care for their patients.
Ennui, or “the boredom”
After the excitement of orientation wears off, first-year students become mentally exhausted with the day-to-day grind. University professors are used to seeing bored students who attend their lectures only to scroll through their phones or laptops disengaged from the class, no matter how exciting the material is (or is not). Most pre-health students are used to “showing up,” “checking the boxes,” and “tapping out” to search for things they otherwise find more interesting. Tedium with experiments and data analysis often causes graduate students to question whether the Ph.D. is worth it.
Discussion of boredom in school has been ongoing for decades . Personal hobbies and habits are generally recognized as ways to fight against medical school malaise, and student affairs and organizations run programming to allow students to occasionally decompress so that their lives are not solely defined by the number of hours studying alone with flash cards. When it comes to studying things that one is not passionate about, mustering enough interest to fight ennui is challenging. Ennui comes from skepticism about the entirety of medicine and whether one truly has “the passion” to fulfill society’s call . You can enter a state of ennui when your are exhausted from processing the emotions of anxiety, envy, and embarrassment, resigning to futility and nihilism as nothing you do seems worth the effort.
Changing routines, shifting focus, or taking an extended holiday away from the daily stress of health care can lessen burnout and ennui. By reconnecting with a belief system combining self and purpose , one can appreciate the importance of living and engaging in the moment (mindfulness), especially with a caring community. These techniques help build your resilience and curiosity which will benefit your professional and personal growth.
Bringing back joy
As the mental health crisis has worsened, more schools are welcoming open discussions of these emotions to combat moral distress . When it comes to applications to medical school, disclosure of effectively managed mental health conditions (to demonstrate resiliency or overcome adversity) does not harm an applicant’s chances for a fair file review .
More physicians and administrators recognize that the health care and medical education systems drain a sense of joy from those who work long enough. With increasing concern about provider burnout since the COVID-19 pandemic, everyone wants to find ways to bring joy back into medicine/health care . Instead of rewarding health professionals for practicing kenosis (“an emptying of the self”), leaders must offer safe spaces and opportunities to discuss experiences that cause moral distress and disengagement. Patients and the public expect our health care providers to be more than just a computer AI chatbot with hands and some therapeutics to cure our ills; they expect and deserve affirmations of empathy and dignity within the natural human connection we share.
At the movie’s end, Riley finds a way to find the joy she lost. She expands her circle of friends and gains confidence that despite her mistakes, she knows her family and friends will still love and care for her. The story may not be as happy or simple for everyone, but being more aware of these complex emotions during your growth as a future professional may strengthen your resolve to achieve your goals.
Good luck to all the first-year students. May you find new ways to nurture joy and your belief in your personal and professional self.
Emil Chuck is a health professional advisor.

Surviving medical madness: a mother’s harrowing tale [PODCAST]

Medical heroes of October 7: the story of Dr. Amit Frenkel and Soroka Hospital staff

Tagged as: Medical school
More by Emil Chuck, PhD

How situational judgment tests help medical schools evaluate applicants
Related posts.

Medical ethics and medical school: a student’s perspective

From medical humanities student to physician

Who gets to succeed in medical school: Improving medical student outcomes that matter

End medical school grades

A medical student’s greatest mistake

The role of income in medical school acceptance
More in education.

Making medicine my home

Revolutionizing medical training: the power of simulation education

Music as a tool for explaining medical concepts

Skyrocketing medical school applications: the hidden costs and stress factors

The misrepresentation of the EDUCATE Act and the future of our health care system

Studying medicine in a time of deep medical distrust: Why I remain hopeful
Most popular.

Quiet firing in medicine: my journey from burnout to freedom

The unseen dangers of faulty expert witness testimony

How anxiety can be your biggest competitor and ally in achieving success

Privacy protection after death: an ongoing dilemma

Debunking schizophrenia myths [PODCAST]

Private equity’s takeover of health care: a patient’s nightmare
Past 6 months.

Struggles of navigating prestigious medical systems

Where did the physician to physician courtesy go?

Concierge medicine: exclusive access or equity dilemma?

The sham peer review: a hidden contributor to the doctor shortage

Palliative care is plagued by misunderstanding
Recent posts.

Talcum powder and female cancer: Separating myths from facts

How cultural barriers delay cancer treatment for women in Pakistan

How quality sleep can boost your weight loss journey [PODCAST]

Medicine’s struggle with genetic and social realities
Subscribe to kevinmd and never miss a story.
Get free updates delivered free to your inbox.
Find jobs at Careers by KevinMD.com
Search thousands of physician, PA, NP, and CRNA jobs now.
CME Spotlights
Leave a Comment
Comments are moderated before they are published. Please read the comment policy .
- Condition Center
I'm a Woman of Color With Psoriasis, but That Diagnosis Wasn't Easy to Get
:upscale()/2024/07/25/778/n/1922153/tmp_R7Ns6U_ca993e27203174f3_processed-8AEE9C5E-5864-40B1-AC8C-63FF4C3A2C41.jpg)
According to the National Psoriasis Foundation , around 125 million people have psoriasis — that's two to three percent of the population — including me. Psoriasis is an autoimmune disorder whereby the immune system is overactive and produces new skin cells at an abnormally rapid rate. New skin cells typically take about a month to form and shed, but for those with psoriasis, new cell development can happen in as little as three days and the shedding process doesn't take place. This results in thick, scaly patches of skin that can itch and burn, as well as crack, bleed, and peel. The cause of psoriasis isn't clear, and there is no known cure — just techniques and medications to manage the symptoms.
My psoriasis started in 2017 when I was 20 years old in college; it began with a small patch on the top of my left foot. This isn't a common area for psoriasis, which usually develops around the elbows, knees, and scalp. It started off as itchy skin, which I would scratch in my sleep, causing it to become sore and inflamed. This cycle continued and slowly spread over eight years, and I have yet to find a solution for it. Luckily, it has remained on my feet, though it does now affect both of them and my ankles. I go through phases where new patches pop up anywhere from my elbows and knees to the back of my neck, under my eyes, and even in my belly button.
One of the most frustrating parts of my psoriasis journey (beyond the condition itself) was the lack of understanding within the medical community. I was misdiagnosed multiple times over five years before I received a psoriasis diagnosis in 2022. I think one of the main reasons is that psoriasis, along with many other skin conditions, is taught to medical students on white skin, where the symptoms look completely different. My psoriasis patches do not have any redness and look completely different than most pictures I've seen online. This meant for years, I was given treatments for eczema , dermatitis , and various other conditions before it was finally identified as an autoimmune disorder.
There are many things that supposedly help with psoriasis, and so many people believe they have the answer because it worked for a friend of a friend. For several years, I struggled to wear anything that showed my feet in public because it would inevitably lead to questions and end with me being recommended a dairy-free diet, a juice cleanse, or an "all-natural" cream from an overseas homeopath, or given the sage advice that it was probably my cat that had caused it. I was embarrassed by how it looked, of my footwear choices, of the fact that I was newly married and was scratching at my feet in my sleep.
At its very worst last year, both my feet were covered in thick, scaly skin, which would constantly bleed and itch. I remember one particular weekend when I went into the city with my husband and ended up having to head home because I'd bled through my socks. We then spent the next few days indoors; I wasn't even able to walk a few minutes to the local supermarket or wear any kind of shoes without being in pain. It's tricky having an autoimmune skin disorder when you work in the beauty industry and are constantly testing and trialing products — you end up convinced that something or other will be the answer you're seeking, and the disappointment can be shattering when nothing works.
Finally, in December 2023, I connected with a brilliant dermatologist, Aadarsh Shah of the Holborn Clinic, an expert in the field who has brown skin like mine. He was a tremendous help and refreshingly honest, sharing the limited options I had for my psoriasis. Immunosuppressants (methotrexate or cyclosporine) would help slow down my overactive immune system but leave me susceptible to infections and viruses. They would also need to be factored into any family planning, as they can lead to birth defects. The other option was to live with it and use steroid treatments to calm particular flare-ups, whilst leaving enough of a gap to avoid TSW (topical steroid withdrawal) . I opted for the latter, knowing my immune system was already not very strong. Having a doctor who was able to fully understand psoriasis on skin that looked like mine was empowering. He acknowledged that due to the melanin in my skin, the scarring and pigmentation I had from healed psoriasis plaques would likely remain on my skin for years. This isn't something any other doctor or dermatologist had mentioned.
With Dr. Shah's guidance, I was able to bring the heavy inflammation on my feet down. While I have had a few bouts of TSW, which has resulted in new inflammation in previously unaffected areas, I was able to get my psoriasis back to a place that had little impact on my day-to-day life. Although it was the use of the steroid Diprosalic that helped the most, I do now try to take care of my skin without relying on steroids. If I am able to keep the area consistently hydrated, I find it itches less and is overall less aggravated. I also know that it is best to stick to ceramide -rich formulas with little to no fragrance in the inflamed areas.
We don't have a cure for psoriasis yet, so like many others I still suffer with it, and I'm concerned for what the future looks like — especially with the symptoms I am showing of early-onset psoriatic arthritis . The body positivity movement has meant there is pressure to feel confident in my skin, and I don't think I'm quite there yet — I still hesitate before wearing sandals, I still crop my feet out of pictures, and I still struggle when I see a new patch, which can lead to feelings of shame. However, I also know that when I see others with psoriasis, I feel a sense of belonging and applaud them for not hiding it. That isn't my choice, but I'm learning to accept that about myself and be more understanding that choosing to cover up my skin is just as much my decision as choosing to show it.
Sidra Imtiaz is a freelance British Pakistani Muslim beauty writer and PR expert based in London, but often in the US. She has written for Refinery29, Glamour, InStyle, Bustle, Who What Wear, and PS.
- Medical Conditions
Welcome to One More Thing by Mama Beasts, a podcast brought to you by Feast and Fettle. We invite the woman inside the mother to come out and play.
One More Thing Mama Beasts
- Society & Culture
- 5.0 • 1 Rating
- AUG 4, 2024
A Hierarchy of Her Own with Leslie Forde
In this week's episode, we are chatting with Leslie Forde, founder of Mom’s Hierarchy of Needs — a company that provides moms with products, research and community to reclaim time for their well-being. Her business also supports organizations to promote wellness for parents at greater risk for burnout with self-care research, rituals and software while teaching managers to disrupt patterns that cause fatigue.After reaching complete burnout in her own life as an exhausted mom with a demanding ...
- JUL 26, 2024
Can You Have It All? With Maggie Pearson, Founder of Feast & Fettle
From a handful of local members to thousands across the Northeast, founder Maggie Pearson grew Feast & Fettle, a fully-prepared meal service, while also becoming a mom and growing her family. In this episode, we chat with Maggie about her journey of building a thriving business and the challenges of being a working mom, plus the hard choice she had to make when it came to scaling her company. She also gives her take on the million dollar millennial mom question: can we really have it all?...
- JUL 21, 2024
Open Marriage & Wanting More with Molly Roden Winter
New York Times bestselling author Molly Roden Winter was a happily married mom of two young children when she went out for an impromptu drink to blow off steam after her husband came missed bedtime yet again. That night, she met a flirtatious younger man and this encounter marked the beginning of her journey exploring sex and relationships outside of her marriage. Described by the Washington Post as, "This book about open marriage is going to blow up your group chat," MORE delves deep i...
- JUL 14, 2024
Boundaries: Ultimate Self Care with Kimberly Solo
You can get all the facials and massages, but if you don't establish and enforce boundaries in your life, are you really taking care of yourself? Therapist Kimberly Solo says women most women struggle with setting boundaries in their lives, and this can weigh on their stress levels and ultimate health. Listen to our conversation to understand why boundaries are essential in our lives, what they can look like and what to do if you struggle to establish/maintain them. People pleasers, this one ...
- JUL 7, 2024
Perimenopause: It's Not In Your Head with Dr. Alicia Robbins
Think menopause is all hot flashes and for the 50+ crowd? Think again. Due to fluctuating hormones, the years leading up to actual menopause (when your period completely stops) can bring about an array of challenging symptoms — from fatigue and weight gain to brain fog and anxiety, impacting our health and quality of life on many levels. If you’re in your late 30’s or 40s, and haven’t been feeling quite like yourself, it’s time to get educated about perimenopause. We chat with Dr. Alicia Robb...
- JUN 30, 2024
Beneath Mom Rage with Minna Dubin and Sarah Harmon
"Rage" and "mothers" aren't supposed to mix. Yet, for many of us, quietly boiling anger rose to the surface during the pandemic, overflowing into our homes, lives and relationships. Enter writer Minna Dubin and therapist Sarah Harmon. Through different mediums, both examined and provided solutions for mom rage at a time when many women were struggling with an often misunderstood and highly judged emotion. Minna first wrote about mom rage in a 2019 personal essay and then a reported...
- © 2024 One More Thing
Customer Reviews
Top podcasts in society & culture.

IMAGES
VIDEO
COMMENTS
Burnout is a state of emotional, mental, and often physical exhaustion brought on by prolonged or repeated stress. Though it's most often caused by problems at work, it can also appear in other ...
Join us as we explore the phenomenon of burnout. Learn what it is, how it manifests, and its relationship to anxiety, depression, and stress.
Burnout is a state of physical and mental exhaustion caused by chronic stress. Learn how to recognize its symptoms, risk factors, and prevention strategies.
The word burnout has become ubiquitous—it seems to sum up the stress, exhaustion, and disaffection that many of us are feeling this year.
"Burnout is a syndrome of emotional exhaustion, depersonalization, and reduced personal accomplishment that can occur among individuals who do 'people work' of some kind," Maslach wrote then.
Her essays and reported stories have been featured in The Boston Globe, Business Insider, The New York Times, BBC, and The Christian Science Monitor.
The chicken-and-egg findings show that stress and burnout are mutually reinforcing. However, contrary to popular belief, burnout has a much greater impact on stress than vice versa. "This means ...
Burnout and stress are at all-time highs across professions, and among already strained health care workers, they are exacerbated by the politicization of mask-wearing and other unrelenting stressors.
Burnout Is About Your Workplace, Not Your People. Summary. We often think of burnout as an individual problem, solvable with simple-fix techniques like "learning to say no", more yoga, better ...
Burnout is devastating to personal relationships, wellness, and ability to provide quality care. This Whole Health tool reviews common questions about burnout, including what it is, its causes, and who experiences it.
This article explores the warning signs of burnout in the workplace and introduces 14+ strategies and programs to help you prevent it.
Discover the personal story of burnout from a nurse's perspective and the valuable lessons learned along the way. Explore tangible solutions for healthcare environments and how nurses can make a positive impact on patient well-being. This is an empowering read.
True workplace burnout is specific to one's job or occupation and is more concerning and detrimental than the daily irritations everyone experiences and most of us manage. There are three dimensions to workplace burnout: Feelings of energy depletion or emotional exhaustion. Increased mental distance from one's work and negative or cynical ...
A growing body of empirical evidence shows that occupational health is now more relevant than ever due to the COVID-19 pandemic. This review focuses on burnout, an occupational phenomenon that results from chronic stress in the workplace. After analyzing ...
That is, unlike with depression, the personal distress from burnout is mostly focused on one or two specific areas of life. It doesn't always generalize to other areas.
WHEN IT COMES to being a POC artist, the narrative is very similar. For Rafa, her burnout doesn't just stem from her art practices but from familial to financial responsibilities as well.
Background. Burnout is a pervasively increasing threat to personal and professional wellbeing and performance. It is yet understudied in relation to basic psychological needs (BPN), especially in at-risk population such as medical residents. This study intends to explore the differential relationship between various aspects of burnout including depersonalization (DP), emotional exhaustion (EE ...
The study highlighted that medical students in the study who reported insufficient exercise demonstrated significant association with studying in clinical year, self-reported poor quality of life, moderate to severe depression, anxiety and insomnia, social dysfunction, and burnout in part of high reduced personal accomplishment.
To get started on a personal statement, brainstorm your best stories and don't stunt the writing process.
"Inside Out 2" explores the complex emotions that teenagers experience during puberty. Riley's original emotions encounter new ones like Anxiety, Envy, Embarrassment, and Ennui, which challenge her sense of identity and friendships. This parallels the emotional journey of health professions students.
A writer details her experience with psoriasis as a woman of color. Read about her yearslong journey and diagnosis here.
Enter writer Minna Dubin and therapist Sarah Harmon. Through different mediums, both examined and provided solutions for mom rage at a time when many women were struggling with an often misunderstood and highly judged emotion. Minna first wrote about mom rage in a 2019 personal essay and then a reported...