
- My presentations

Auth with social network:
Download presentation
We think you have liked this presentation. If you wish to download it, please recommend it to your friends in any social system. Share buttons are a little bit lower. Thank you!
Presentation is loading. Please wait.
Basics of Medication Safety
Published by Priscilla Jenkins Modified over 9 years ago
Similar presentations
Presentation on theme: "Basics of Medication Safety"— Presentation transcript:

Partners in Crime: Your Pharmacist Sarah A. Spinler, PharmD, FCCP,FAHA, FASHP, BCPS (AQ Cardiology) Professor of Clinical Pharmacy Philadelphia College.
Medication Administration for Resource Parents
Welcome to Medicines in My Home.

The Pharmacy Guild of Australia NSW Branch Medicines for Consumers Best Practice at Home.
MEDICATIONS IN SCHOOLS: SECTION VI
Obtaining THE BEST POSSIBLE MEDICATION HISTORY Medication Reconciliation Initiative Winnipeg Regional Health Authority.
Introduction Medication safety is a critical aspect in improving the health of individuals and increasing their quality of life. When used in the proper.
The Law The law covers only non-injectable medication.
Medication Administration
Drug Use, Misuse and Abuse Health Coach McLure/Anno.

Medication Reconciliation in Long Term Care. Medication Reconciliation, or “Med Rec”, is a formal process of creating a Best Possible Medication History.
Information for adults on using over-the-counter medicines safely By: Chaltu Wakjira,PhamD August 30, 2014.

Attention Seniors: STAMP Out Prescription Drug Misuse & Abuse

January 16, 2010 Monica Robinson Green, PharmD, BCPS.

Be An Active Member Of Your Health Care Team Be An Active Member Of Your Health Care Team.
Preventing Medication Errors Chapter 9. 2 Safe Medication Administration Prescription –Licensed providers must have authority within their state to write.
Health Grade 6 Understanding Drugs Mr. Vargas. Drugs and Your Health What advice would you give to a friend about how to use medicine safely?
What BISD Staff Need to Know About: Medication Administration
Obtaining THE BEST POSSIBLE MEDICATION HISTORY

Your Medicine: Play it Safe. Your Health Care Team Doctors, nurse practitioners, and other medical professionals Nurses Pharmacists Use the link below.
About project
© 2024 SlidePlayer.com Inc. All rights reserved.
- Medication including labelling
- Remember me Not recommended on shared computers
Forgot your password?
5 Moments for Medication Safety poster
- PUBLISHED 19 July, 2021
- TYPE Infographics
- CONTENT TYPE Pre-existing
- COPYRIGHT STATUS Public domain
- PAYWALLED No
- ORIGINAL AUTHOR World Health Organization (WHO)
- ORIGINAL PUBLICATION DATE 29/03/17
- SUGGESTED AUDIENCE Everyone
- Patient safety strategy
This poster, published by the World Health Organization (WHO) in 2017, summarises in a visual way the '5 Moments for Medication Safety', which are the key moments where action by the patient or caregiver can greatly reduce the risk of harm associated with the use of their medication/s. It is part of the 'Medication without harm' global patient safety challenge.
Recommended Comments
There are no comments to display.
Create an account or sign in to comment
You need to be a member in order to leave a comment
Create an account
Sign up for a new account in our community. It's easy!
Already have an account? Sign in here.
Related hub content
- Diabetes - What the tech? poster (June 2024) Latest comment by Patient-Safety-Learning
- WHO: Your 5 moments for hand hygiene care in a maternity unit (2020) Latest comment by Patient Safety Learning
- Natural Care Forum: Medication safety in care homes Latest comment by Patient Safety Learning
Useful external links
World Health Organization
- Existing user? Sign In
- Communities
- Patient Safety Learning and the hub
- Become a member
- Join a private community
- Topic leaders
- How to share content
- Guide to writing a blog
- Moderation of content
- Acceptable use policy
- How the hub is being used
- Top tips for personalising your hub
- User feedback survey
- All content
- All community
- Create New...
Internet Explorer Alert
It appears you are using Internet Explorer as your web browser. Please note, Internet Explorer is no longer up-to-date and can cause problems in how this website functions This site functions best using the latest versions of any of the following browsers: Edge, Firefox, Chrome, Opera, or Safari . You can find the latest versions of these browsers at https://browsehappy.com
- Publications
- HealthyChildren.org
Shopping cart
Order Subtotal
Your cart is empty.
Looks like you haven't added anything to your cart.
- Career Resources
- Philanthropy
- About the AAP
- The Pediatrician's Role in Preventing Child Maltreatment
- AAP Report: Pediatric Practices Play Vital Role in Preventing Child Maltreatment
- Child Abuse and Neglect: What Parents Should Know
- AAP - Child Maltreatment can be Prevented
- News Releases
- Policy Collections
- The State of Children in 2020
- Healthy Children
- Secure Families
- Strong Communities
- A Leading Nation for Youth
- Transition Plan: Advancing Child Health in the Biden-Harris Administration
- Health Care Access & Coverage
- Immigrant Child Health
- Gun Violence Prevention
- Tobacco & E-Cigarettes
- Child Nutrition
- Assault Weapons Bans
- Childhood Immunizations
- E-Cigarette and Tobacco Products
- Children’s Health Care Coverage Fact Sheets
- Opioid Fact Sheets
- Advocacy Training Modules
- Subspecialty Advocacy Report
- AAP Washington Office Internship
- Online Courses
- Live and Virtual Activities
- National Conference and Exhibition
- Prep®- Pediatric Review and Education Programs
- Journals and Publications
- NRP LMS Login
- Patient Care
- Practice Management
- AAP Committees
- AAP Councils
- AAP Sections
- Volunteer Network
- Join a Chapter
- Chapter Websites
- Chapter Executive Directors
- District Map
- Create Account
- Early Relational Health
- Early Childhood Health & Development
- Safe Storage of Firearms
- Promoting Firearm Injury Prevention
- Mental Health Education & Training
- Practice Tools & Resources
- Policies on Mental Health
- Mental Health Resources for Families
Poster on Safe Storage and Disposal of Medications
Thank you for taking part in educating families about the importance of safe storage and disposal of medications. This poster has been designed specifically so you can add local resources. This poster is also available in Spanish . Please consider using the available space on the poster for adding phone numbers or websites of local take back programs and resources in your area. Here are some websites to get you started:
- Safe Disposal of Medicines (FDA)
- Controlled Substance Public Disposal Locations Search (US Dept of Justice)
- National Prescription Drug Take Back Day (US Drug Enforcement Administration)
- Drug Disposal Information (US DEA)
In addition, check out some other resources to support you in preventing, identifying, and treating opioid use disorder:
- Training to treat opioid use disorder
- AAP resources to address the opioid epidemic
AAP Public Service Announcement on Medication In this public service announcement from the AAP, Dr Shelly Flais explains how to protect children by safely storing medicine at home. Physicians can share the PSA on practice websites or social media by using this code:
<iframe width="854" height="480" src="https://www.youtube.com/embed/bUal9CbiKts" frameborder="0" allow="autoplay; encrypted-media" allowfullscreen></iframe>
Last Updated
American Academy of Pediatrics
- Understand the Issue
- Safe Storage and Disposal
- Helping Others
- Learn at Home
- Goals & Outcomes
- Enroll in Ambassadors
- Older Adult
- Resources & Downloads
- Discussion Board
- Request a Speaker
Share Your Story

How do you advocate prescription drug safety? Help our community by sharing your personal tips and stories here.
Teen Resources
Educate Teens About Using M edications Safely

“My Generation Rx” includes resources designed to educate teens about the importance of using medications safely, as well as teaching teens key skills to turn down invitations to misuse and positive alternatives to cope with the demands of life. These materials could be delivered in formal classroom settings, after-school programming, youth organization meetings, or any other venue with teen audiences.
- 1 Getting Started
- 2 Activities for In-person Programming
- 3 Activities for Virtual Programming
- 4 Other Resources
- 5 Generation Rx Teen en Español
Getting Started
This section provides facilitators with a comprehensive guide that contains information to successfully present all of the teen resources. In addition, we’ve included a “Tips & Advice” handout for teens. Facilitators may elect to distribute this handout following an educational program or at an informational booth.
This comprehensive facilitator guide contains information to successfully present “My Generation Rx”, including a Getting Started guide, Activity Snapshots, and a Q&A session guide.
Pass out this informational handout to educate teens on safe medication practices.
A letter designed to assist facilitators in introducing the purpose of your educational program and the importance of presenting this information.
Teen Presentation Trips and Tricks
The following video was created to help presenters prepare to present the Teen Toolkit. It includes tips and tricks on everything from talking to teens about safe medication practices, to finding an organization to partner with to playing the games and activities outlined in this toolkit. It is a great resource for first-time presenters!
Teen Presentation Videos
The following videos were created to capture a real-life Teens Toolkit presentation, so viewers can understand how to play certain games and activities while teaching the Generation Rx messages and interacting with teens.
Activities for In-person Programming
Each activity listed in this section is designed to serve as a stand-alone resource. Along with each activity, we’ve included specific talking points for facilitators. Before implementing any activity, we encourage you to review the “Getting Started” and “Activity Snapshot” from the facilitator guide (see above).
Activity 1: “Medication Safety for Teens” Presentation
An interactive PowerPoint presentation that teaches teens how to safely use medication.
Activity 2: “Champions of Rx” Game
A competitive game that provides a broad overview of the problem, as well as emphasizes how to safely use medication and teaches approaches for turning down invitations to misuse.
Activity 3: “Lead the Scene” Skit-based Activity
A skit-based activity that includes first viewing a theatrical performance, then identifying different choices select characters could have made to ensure more positive outcomes. This activity emphasizes approaches for turning down invitations to misuse, as well as positive alternatives to prescription drug misuse.
Activity 4: “Plot Twists” Skit-based Activity
A skit-based activity that requires teens to identify and perform approaches for turning down invitations to misuse, as well as identify positive alternatives to cope with the pressures of life.
Activity 5: “Minute Activities”
A collection of short, hands-on activities designed for small groups (e.g. icebreakers or resetting a group’s attention during a longer presentation) or for individuals (e.g. engaging teens at an informational booth).
Activities for Virtual Programming
Out of the five activities listed above, we’ve provided suggestions for adapting four of the activities for virtual use. Below are resources to support delivering the Generation Rx Teen Toolkit within a virtual environment.
Below are the four activities available for virtual programming. The facilitator guides provide recommendations for online adaptations through comments posted as yellow speech bubbles. We have also included the accompanying activity, although no edits have been made to these files (i.e. they are identical to the activity files listed above).
How To Videos
The first video provides guidance on how to adapt the identified activities from the Teen Toolkit for virtual use, along with suggestions for facilitating virtual engagement. The second video puts forth questions to consider when planning your virtual program, including tips from others in the field.
Medication Safety for Teens
Champions of rx, lead the scene, minute activities with online adaptations.
A collection of short, virtual, hands-on activities designed for small groups (e.g. icebreakers or resetting a group’s attention during a longer presentation) or for individuals.
Other Resources
“The Party” InterACT Video Ohio State’s INTERACT drama troupe invites high school students to direct actors who portray college kids contemplating the use of prescription drugs at a party. This innovative project was organized by The Ohio State University College of Pharmacy’s Generation Rx. Participants: Interact’s Robin Post and Nicole Kwiek, PhD, The Ohio State University College of Pharmacy.
Smart Moves, Smart Choices The Smart Moves, Smart Choices website is provided by the National Association of School Nurses with the support of Janssen Pharmaceuticals. It provides sections entitled Get Facts, Take Action, Watch Videos,and Quick Links for parents, teens, and educators. The program also offers a tool kit that enables educators to hold school assemblies about teen prescription drug abuse in their communities.
“Talking to Your Kids About Prescription Drug Abuse” This brochure was produced by the National Council on Patient Information and Education (NCPIE) and the Substance Abuse and Mental Health Services Administration (SAMHSA). It provides advice for parents regarding the rising abuse of prescription medications by teens and resources for addressing this phenomenon.
Maximizing Your Role as a Teen Influencer This program aims to protect teens by reducing prescription drug abuse. The initiative encourages educators, healthcare providers, parents and other “teen influencers” to talk to teens about prescription drug abuse. The program provides easy-to-use materials to help mentors reach out to teens..
PEERx The National Institute on Drug Abuse (NIDA), part of the National Institutes of Health, offers an online initiative called PEERx to educate 13-15 year olds on the dangers of prescription drug abuse. The centerpiece of the initiative is “Choose Your Path,” an innovative video tool that empowers teens to assume the role of the main character and select which path to take at certain points in the drama and then watch the consequences play out onscreen. Other free PEERx resources include: an Activity Guide with step-by-step instructions to help teens organize peers in their school or community group; Peer Into Your Path, a twist on Choose Your Path that invites teens to write their own decision tree-based stories weaving in facts about the effects of prescription drugs; free downloads that can be made into iron-on decals for T-shirts, or posters, wallpaper or stickers; relevant posts from NIDA’s Sara Bellum Blog; and fact sheets.
Generation Rx Teen en Español
Generation Rx Teen en Español (.zip)
Rate Our Materials
We value your feedback to help us assess the impact of this work and continually improve Generation Rx materials.
Take the Survey
Toolkit Access
Please complete the following information for access to our toolkit materials
Quick Links
Brought to you by:.
Generation Rx 217 Lloyd M. Parks Hall 500 W. 12th Ave. Columbus, OH 43210
614.292.2266 [email protected]
©2007-2021. The Ohio State University. All Rights Reserved.
- A-Z Poison Index
- Poison Center Blog
- Education Requests
- Education Staff
- Self-Poisoning Prevention Toolkit for Providers
- Self-Harm Prevention: Parent Resources
- Poison Perils with Frank & Louise
- Medication Safety at Home
- Teen Medication Safety
- E-Cigarettes for School Nurses
- Marijuana Webinar
- Opioids Webinar
- Synthetic Drugs EMS Webinar
- Synthetic Drugs Law Enforcement Webinar
- Synthetic Drugs School Nurse Webinar
- Poison Prevention in Other Languages
- Spike Education Program
- R U Prepared?
- Middle/High School Lessons
- Data Requests
- Self-Harm Prevention: Health Care Provider Toolkit
- Antidote Management & Antidote Chart
- Choosing Wisely: Toxicology
- Fentanyl Exposures in First Responders
- Pediatric Marijuana Exposures
- Physical Materials
- Lessons/Activities
- Medication Safety
- Health Care Provider Materials
Join Our Email List
Poison Perils with Frank & Louise: Beetle Battles
It was Saturday morning in the Wilmot house and Frank and Louise were enjoying their coffee on the back patio. Louise was flipping through photos of weed-free flower beds in … Continue reading →
Medication Safety Poster (Multiple Languages)
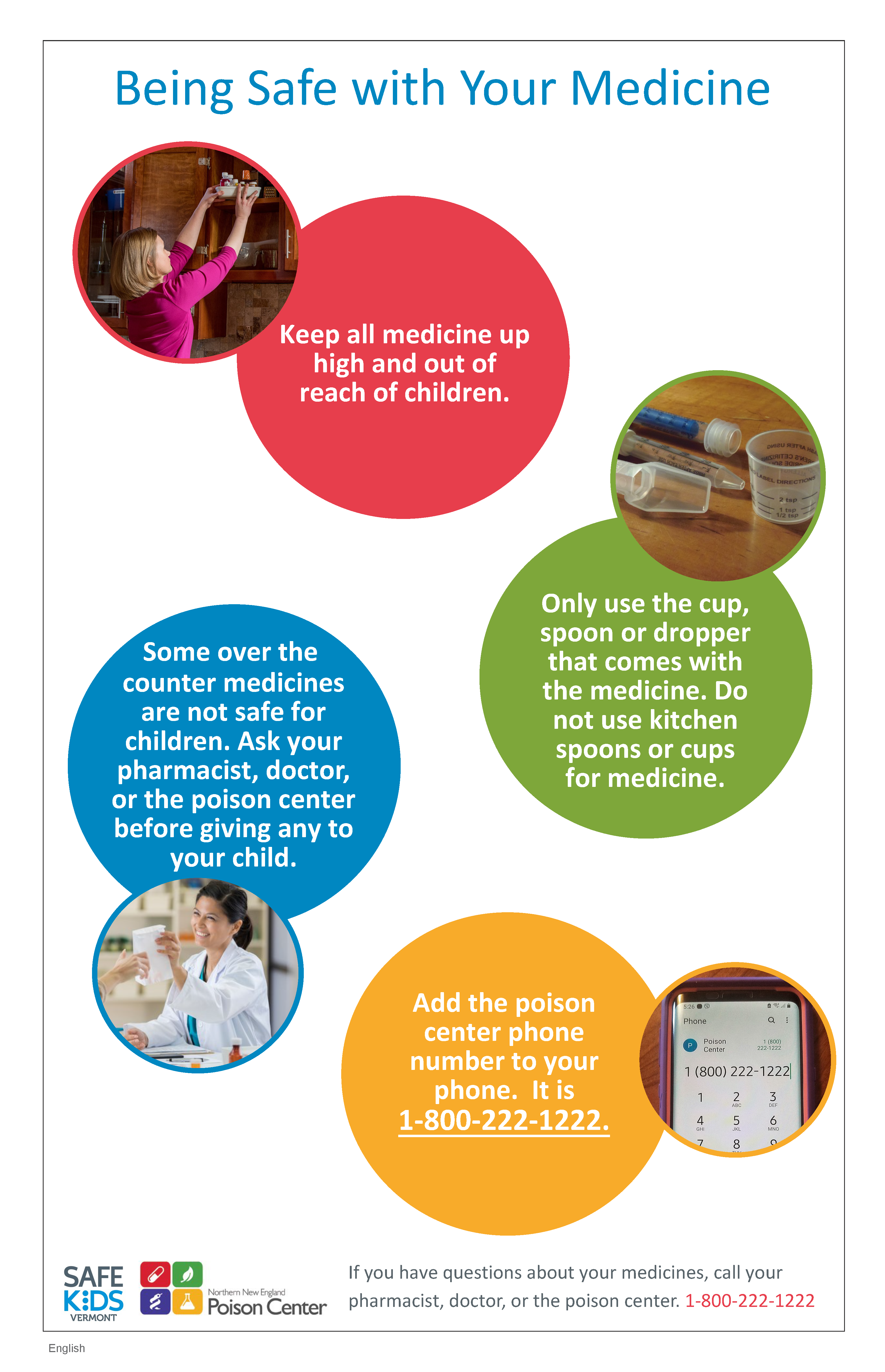
This poster comes in nine languages and conveys four key medication safety messages:
- Keep medication up high, out of reach of children
- Talk to your doctor before giving medication to your child
- Only use the measuring tool that came with your child’s medication
- Keep the poison center number in your phone: 1-800-222-1222
The languages included in this download are:
Thank you for your interest in our materials. Please enter your zip code to continue.
If you'd like to sign up for our monthly newsletter, you can enter your email address as well.
- 5 Digit Zip Code *
- Add me to your mailing list

- Poison Information
- Resources for Providers
- Legal Disclaimer
- Design & Development by Flyte
A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Tips for Medication Safety
- Facts and Stats
- Medication Safety Resources
- PROTECT Initiative
Related Topics:
- Healthcare-Associated Infections (HAIs)
Medication Safety and Your Health
- Medicines are safe when used as prescribed or as directed on the label. There are risks in taking any medicine, vitamin or other supplement.
- An adverse drug event (ADE) is when a medication causes harm to someone. ADEs include allergic reactions, side effects, overmedication and medication errors. They are a serious public health threat.
- ADEs are a preventable patient safety problem.
Why it's important
The number of ADEs can increase due to:
- Development and use of new medicines.
- Discovery of new uses for older medicines.
- The aging American population.
- Increased use of medicines for disease treatment and prevention.
Learning about medication safety can reduce the risk of harm for you and your loved ones.
More than 1.5 million emergency visits
Practice medication safety at home
Tips for adults
- Keep a list . Keep a list of your medicines, vitamins, and other supplements. Make sure your doctor knows about all the medicines, vitamins and other supplements you take.
- Follow label directions . Take medicines as directed on the label or as instructed by a doctor or pharmacist.
- Take medicine on time . Some medicines should be taken with meals or during a certain time of day (e.g., bedtime). Set timers or reminders to help you remember to take your medicines. You might try a reminder app.
- Turn a light on . Turn on a light when taking medicines so you don't misread the label and make a mistake. If you wear eyeglasses, put them on as well.
- Ask questions : If you do not understand label instructions, talk to your pharmacist or doctor before taking the medicine.
- Get the tests you need : Keep up with any blood testing suggested by your doctor.
Tips for children
- Read the label.
- Follow directions.
- Measure your child's dose using the dosing device (oral syringe, dosing cup) that comes with the medicine. Do not give a child more medicine than stated on the package.
- Check the label . Check the active ingredients in prescription and over-the-counter medicines. Make sure that you do not give your child two medicines that have the same active ingredient. If you have questions, ask your doctor or pharmacist.
- Use the right tool . If you do not have a dosing device, ask your pharmacist for one. Do not use household spoons to give medicines to children.
- Get questions answered . If you do not understand the instructions, talk to your pharmacist or doctor before giving the medicine.
- Teach children . Teach your children what medicine is and why you or a trusted adult must give it to them.
- Lock the safety cap . Always check that the cap on a medicine bottle is locked.
- Put Medicines Away . After locking the safety cap, always put medicines back in their safe storage location. Keep medicines in a place young children cannot reach or see.
What CDC is doing
- Monitoring ADEs across the country and using these data to improve medication safety through key partnerships and enhanced policies.
- Reducing ADEs by focusing on specific medications and high-risk groups.
- Promoting ADE awareness through nationwide educational campaigns.
- Drug Information for Consumers , Food and Drug Administration (FDA)
- Buying & Using Medicine Safely , Food and Drug Administration (FDA)
- Disposal of Unused Medicines: What You Should Know, Food and Drug Administration (FDA)
- Taking Medicines, Agency for Healthcare Research and Quality (AHRQ)
- Drug Safety , National Institutes of Health (NIH)
- Medication Without Harm, World Health Organization (WHO )
- Safe Medication , American Society of Health-System Pharmacists (ASHP)
- ConsumerMedSafety.org , Institute for Medication Safety Practices (ISMP)
- Consumer Information for Safe Mediation Use , National Coordinating Council for Medication Error Reporting and Prevention (NCC MERP)
- Health In Hand, CHPA Educational Foundation
Medication Safety
This website provides information, initiatives, programs, and resources to patients and caregivers about preventing adverse drug events caused by medications.
Medication Safety
Jul 23, 2014
980 likes | 3.3k Views
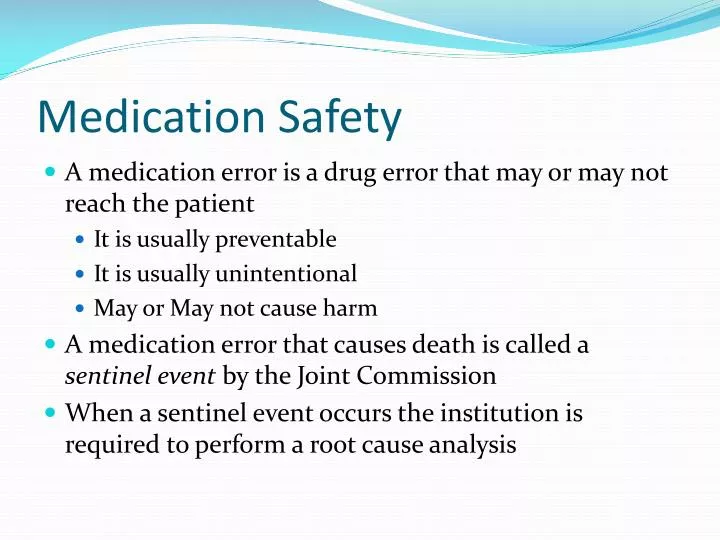
Medication Safety. A medication error is a drug error that may or may not reach the patient It is usually preventable It is usually unintentional May or May not cause harm A medication error that causes death is called a sentinel event by the Joint Commission
Share Presentation
- medication error
- pharmacy personnel
- ismp org tools errorproneabbreviations
- do crush list
Presentation Transcript
Medication Safety • A medication error is a drug error that may or may not reach the patient • It is usually preventable • It is usually unintentional • May or May not cause harm • A medication error that causes death is called a sentinel event by the Joint Commission • When a sentinel event occurs the institution is required to perform a root cause analysis
Type of Medication Errors • Prescribing Errors • Involves wrong dose, illegible sigs, wrong frequencies • Incorrectly transcribing verbal orders from MD • Dispensing Errors • Results from mistakes made during dispensing • Physically preparing medications incorrectly (i.e. using 23.4% saline instead 0.9% saline for an IV admixture) • Transcribing sig instructions incorrectly • i.e. Methothexate 12.5 mg tablet TIW as 12.5 mg TID • Error is dosing calculations • Administration Errors • Involves nursing • Incorrect route of administration • Giving KCL 40 meq IVP instead of KCL 40 meq IVPB over 60 minutes (FATAL) • Giving Vincristineintrathecally instead of intravenously (Fatal) • Giving Penicillin G Benzathine IV instead of IM (can be fatal)
Causes of Medication Errors • Performance problems • Procedure(s) not followed • Knowledge deficits • Pharmacists/Pharmacy Technicians that may be intoxicated by alcohol or drugs • Social or Family problems • Noise level at work • Distractions
Medication Error Reduction Strategies • Joint Commission “Do not use” list • ISMP (Institute for Safe Medication Practices) error prone do not use list • See Lesson 3 “Medical and Pharmacy Terminology” • Also see www.ismp.org/tools/errorproneabbreviations.pdf • ISMP also publishes a list of confused drug names • Example concludes Celebrex-Celexa • List can be found at www.ismp.org/tools/confuseddrugnames.pdf
Tall Man Lettering • Tall Man lettering is a strategy implemented by healthcare institutions in the US under the advise of the Joint Commission , FDA and ISMP • Involves drug names that can be confused with one and other, see ISMP confused name’s list • Drugs with similar sounding names or spelling are called LASA drugs-Look Alike Sound Alike drugs • Tall man lettering involves the use of mixed case lettering to distinguish between these drugs • Examples: • buPROPion VS busPIRone • glyBURide VS glipiZIDE • hydrALAZINE VS hydrOXYzine • Tall man strategies involves: labeling of these medications, ADC cabinet display, separating these drugs on pharmacy shelves
High Alert Medications • Medications that when used in error can result in serious patient harm including death • ISMP has collected a list of such drugs
High Alert Medication Strategies • US hospitals and healthcare institutions have published their own lists that mirrors the ISMP list with some additions. • Strategies include: • Specialized color code labeling for these medications • Segregating the medications in the pharmacy inventory • Restricting access to these drugs in the ADC (non overrideable) • Specialized alerts in the CPOE and the pharmacy systems • Use of standardized preparations of these drugs • i.e. Heparin USP 25,000 units/250 ml D5W
Do Not Crush List • ISMP publishes a do not crush list • These drugs should never be crushed • Typically patients that can’t swallow or have feeding tubes, NG tubes and PEG tubes have their oral dose forms crushed and administer in about 30 ml of liquid • Crushing some drugs alters their time course of activity, stability, or exposure potential to pharmacy personnel • Drugs that are long acting • Effexor XR, Cardizem CD, Detrol LA, KDUR, Paxil CR, Seroquel XR • Drugs that are enteric coated • Ecotrin • Depakote • Nexium • Powerful GI irritant • Actonel® • Teratogenic (exposure to female pharmacy personnel) • Isotretinoin • Sublingual Dose Forms • Nitroglycerin
How to report med errors and adverse drug events • FDA Medwatch • ISMP MERP database • Institute of Medicine (IOM) • TJC (Joint commission) • USP Medmarx • FDA and CDC VAERS system for vaccines
- More by User

Standard 4: Medication Safety
Standard 4: Medication Safety. Advice Centre Network Meeting Margaret Duguid Pharmaceutical Advisor February 2013. Standard 4 Medication Safety. Intent of Standard 4 – Medication Safety.
647 views • 18 slides
Medication Safety. Dr . Kanar Hidayat 2016-2017. Medication Safety Programme.
1.48k views • 16 slides
Medication Safety Medication Errors Part I PHCL 311
Topics to be covered today. IntroductionThe evidence that medication error is a problemDefinitionsThe relationship between medication error, ADE
1.69k views • 80 slides

Medication Safety: Anticoagulation Management
Medication Safety: Anticoagulation Management. Carla S. Huber, ARNP MS Community Anticoagulation Therapy (CAT) Clinic Cedar Rapids, IA 52401 515-558-4046 [email protected] www.crhealthcarealliance.org. Objectives.
839 views • 39 slides
Objectives. Identify the challenges and barriers to implementing medication safety toolsExplain the importance of utilizing evidence-based guidelines for managing warfarin therapyExplain the importance of education for patients taking warfarinList the advantages of a dedicated anticoagulation cli
576 views • 40 slides
Medication Safety and You
Introduction1 . Adverse drug events are the sixth leading cause of death in hospitals and are responsible for 7% of all admissions. Health
524 views • 36 slides
Medication Safety and You. Insert Speaker Information here. Insert your logo here. Introduction 1. Adverse drug events are the sixth leading cause of death in hospitals and are responsible for 7% of all admissions.
546 views • 36 slides
Medication Safety. The Role of Medication Reconciliation & Medicine Lists. Presenter Name & Organization. Objectives. Be familiar with Washington Patient Safety Coalition
1.23k views • 31 slides

Basics of Medication Safety
Basics of Medication Safety. Welcome and Introductions. Presentation Goals. To raise your awareness of: how you can help improve patient safety safe medication use practices the value of working with your pharmacist. Topics. Overview of medication safety Engage in patient safety!
1.56k views • 47 slides
Medication Safety 2013
Medication Safety 2013. Safe Storage, Safe Dosing, Safe Kids Erin Donaldson, Safe Kids Kenosha-Racine.
321 views • 12 slides

Medication Safety. Help for Grandparents. Bluegrass Prevention Center Elizabeth Anderson-Hoagland Fall 2011. Medications = Drugs. Change how the body works Treats or prevents a disease or symptom. Over the Counter Medications. Do NOT need to see a doctor
549 views • 30 slides
Medication Safety Part 1
Medication Safety Part 1. Outline. Medication safety terminology Relationship between medication errors, adverse drug events & adverse drug reactions Medication error classification Factors contributing to medication errors. Medication Misadventure.
1.66k views • 31 slides

Medication Safety / Device Safety Update
Medication Safety / Device Safety Update. Dr David Cousins Senior Head Safe Medication Practice and Medical Devices. Outline. New style Patient Safety Alerts from NHS England Recent Alerts New Alerts Improving reporting and learning of medication / device incidents The future.
692 views • 35 slides
Medication Safety. The Good Hospital Practice Training Series 2009 The Medical City. In this presentation…. The roles of the Medical City staff in ensuring the safe use of medications Prescription writing Verbal and phone orders High risk medication monitoring Medication reconciliation
6.31k views • 43 slides
MEDICATION SAFETY
MEDICATION SAFETY. Meeting HFAP Accreditation Standards for Pharmacy Services and Medication Use. Part Two: Procurement, Preparation and Dispensing. HFAP Chapter 25 keeps you in compliance with the Medicare Conditions of Participation. Medication Safety Series. Prescribing challenges
949 views • 50 slides

MEDICATION SAFETY. Rola Hammoud.MD Medical Quality Director. COUNT ONLY ONCE How many “f’s”. COUNT ONLY ONCE How many “f’s ”. Finished files are the result of years of scientific study combined with the experience of years. COUNT ONLY ONCE How many “f’s”.
1.6k views • 61 slides
Medication safety
Medication safety. Group 2B Supervised By: Dr. Tareef Alaama. Introduction. The safety of medicines is an essential part of patient safety . Harmful, unintended reactions to medicines are among the leading causes of death in many countries. M edication error.
1.65k views • 39 slides
Medication Safety Part 2
Medication Safety Part 2. Outline. Recommendations to prevent medication errors Actions upon error detection Definition and assessment of ADRs Role of pharmacist in medication safety Role of Saudi FDA in medication safety. Recommendations for Preventing Medication Errors.
1.62k views • 27 slides

Monthly Medication Safety Webinar :
Monthly Medication Safety Webinar :.
786 views • 68 slides

Medication Safety and Administration
Medication Safety and Administration. Medication administration for nursing students in clinical at Seattle Children’s. Update June 2011 – Kristi Klee, DNP, RN, CPN Update February 2014 – Carol Shade, MS, RN, CPHIMS Adrian Harden, BSN, RN Leslie R. Harder, MN, RN-BC. Objectives.
896 views • 33 slides
Medication Safety Patrol
Medication Safety Patrol. Good Choice or Bad Choice ?. Instructions. When taking medicine, what is a good choice? A bad choice? For each scenario, indicate if the person made a:. OR. Good Choice. Bad Choice. Cindy takes MORE medicine than instructed. Good Choice or Bad Choice ?.
301 views • 21 slides

Introduction to medication safety
Introduction to medication safety. Rationale. medication use has become increasingly complex in recent times medication error is a major cause of preventable patient harm as future pharmacist, you will have an important role in making medication use safe. Learning objectives.
572 views • 27 slides
- Person-centred care
- Therapeutic communication
- Cultural Competence
- Teamwork and collaborative practice
- Clinical Reasoning
- Evidenced-based practice
- Preventing, minimising and responding to adverse events
- Infection prevention and control
- Medication safety
Medication Safety: Resources
Interprofessional education for quality use of medicines (ipe for qum).
The four videos below profiles authentic situations in which poor interprofessional communication and teamwork resulted in adverse medication events outcomes.
1. Vanessa Anderson
This module portrays Vanessa’s story and is based upon the findings from the Coroner’s report into her death in 2005. Although Vanessa’s death resulted from a combination of human and systems errors, this module will focus primarily on the communication and medication safety issues that occurred during Vanessa’s hospitalisation. As you undertake this module carefully consider how the poor communication between the health professionals involved impacted upon medication safety and how this could have been prevented. At the same time reflect on how your learning will impact your future practice.
2. Mark Green
This module was adapted from an actual clinical case in which a serious clinical error occurred and this resulted in a person’s death. The coroner’s report following the inquest identified communication between staff and during handover, documentation and clear identification of decisions, and use of appropriate guidelines and protocols as key areas for improvement.
3. Gavin Sinclair
This module introduces 23 year-old Gavin Sinclair, who presents to the emergency department at a regional hospital after a minor car accident. A physical examination has cleared him of any physical injuries but Gavin’s mental state is of concern to staff. Undiagnosed and inadequately treated schizophrenia has a high burden of illness in the Australian community. Evidenced-based treatment for schizophrenia includes antipsychotic medications and ongoing monitoring. However, non-adherence to medication is common and stigma associated with schizophrenia is a major issue among patients, carers, and health professionals.
4. Young-Min Lee
On the day in which the module begins, Young-Min Lee was seen by a paediatrician in his rooms and was diagnosed with a urinary tract infection. Young-Min was sent with his Korean mother to the local hospital to be admitted for treatment. An error occurred in the administration of Gentamicin to the child, which is detected before it causes any harm. The module explores the communication that occurs within the healthcare team in detecting and correcting the problem, as well as the issues associated with communicating with a patient from a culturally and linguistically diverse background, and the correct procedures for open disclosure.
Acknowledgment: Tracy Levett-Jones, Conor Gilligan (and Team) University of Newcastle. Funded by the Australian Learning and Teaching Council, Office for Learning and Teaching.
WIIMALI VIRTUAL COMMUNITY
Wiimali was designed to transform understandings of healthcare, and to challenge traditional views of culture and community. It provides insights into the interactions between peoples’ lived realties and their healthcare experiences. Eileen Poole’s’ story is one of these resources.
1. Eileen Poole’s story
Eileen Poole’s journey from her home to the GP and pharmacy, through to admission to hospital because of a medication error illustrates the importance of quality use of medicines, interprofessional communication and collaboration, person-centred care, and therapeutic communication. The series of digital stories takes place in three settings:
- Eileen Poole’s home
- GP Super Clinic
- Wiimali Pharmacy
- Wiimali Hospital
EP1: Meet Eileen Poole
SAFE ADMINISTRATION OF MEDICATIONS: MANAGING INTERRUPTIONS DURING MEDICATION ADMINISTRATION
Three systematic reviews have demonstrated that interruptions (externally initiated events e.g., question from patient, telephone call, infusion pump alarm that suspends or diverts attention) during medication administration seriously compromise patient safety. A recent Australian study reported that interruptions occurred in 53% of medication administrations and that the risk and severity of medication errors double when the number of interruptions increasing from 0 to 4
This video can be used to highlight the issues associated with medication interruptions and how to prevent and manage them.
Acknowledgment: Marie Johnson, Tracy Levett-Jones, Elizabeth Manias, Bronwyn Everett and Gabrielle Weidemann. Funded by NSW Health Nursing & Midwifery Strategy Reserve Initiative Funding (SWSLHD)
MEDICATION SAFETY: A PATIENT’S STORY
In this video Helen Haskell, the founder and president of Mothers against Medical Error, shares the story of her son, Lewis Blackman, and the factors that led to his death.
Acknowledgment: Presented at the ‘Improving Medication Safety through Effective Communication and Teamwork’ conference.
NPS MEDICINEWISE – CPD FOR NURSES
This website provides a range of evidence-based education resources for nurses about safe and quality use of medicines.
https://www.nps.org.au/cpd/professions/nurses
Acknowledgment: Lynn Weekes (and team). Funded by the Australian Government department of Health
- Graphic Design
Medication Safety _ Poster Presentation For WPD23 of R. P. Shaha University
- September 2023

- R. P. Shaha University
- This person is not on ResearchGate, or hasn't claimed this research yet.
Discover the world's research
- 25+ million members
- 160+ million publication pages
- 2.3+ billion citations
- Recruit researchers
- Join for free
- Login Email Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google Welcome back! Please log in. Email · Hint Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google No account? Sign up
Warning: The NCBI web site requires JavaScript to function. more...
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Hughes RG, editor. Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Rockville (MD): Agency for Healthcare Research and Quality (US); 2008 Apr.

Patient Safety and Quality: An Evidence-Based Handbook for Nurses.
Chapter 37 medication administration safety.
Ronda G. Hughes ; Mary A. Blegen .
Affiliations
The Institute of Medicine’s (IOM) first Quality Chasm report, To Err Is Human: Building a Safer Health System , 1 stated that medication-related errors (a subset of medical error) were a significant cause of morbidity and mortality; they accounted “for one out of every 131 outpatient deaths, and one out of 854 inpatient deaths” 1 (p. 27). Medication errors were estimated to account for more than 7,000 deaths annually. 1 Building on this work and previous IOM reports, the IOM put forth a report in 2007 on medication safety, Preventing Medication Errors . 2 This report emphasized the importance of severely reducing medication errors, improving communication with patients, continually monitoring for errors, providing clinicians with decision-support and information tools, and improving and standardizing medication labeling and drug-related information.
With the growing reliance on medication therapy as the primary intervention for most illnesses, patients receiving medication interventions are exposed to potential harm as well as benefits. Benefits are effective management of the illness/disease, slowed progression of the disease, and improved patient outcomes with few if any errors. Harm from medications can arise from unintended consequences as well as medication error (wrong medication, wrong time, wrong dose, etc.). With inadequate nursing education about patient safety and quality, excessive workloads, staffing inadequacies, fatigue, illegible provider handwriting, flawed dispensing systems, and problems with the labeling of drugs, nurses are continually challenged to ensure that their patients receive the right medication at the right time. The purpose of this chapter is to review the research regarding medication safety in relation to nursing care. We will show that while we have an adequate and consistent knowledge base of medication error reporting and distribution across phases of the medication process, the knowledge base to inform interventions is very weak.
- Defining Medication Errors
Shared definitions of several key terms are important to understanding this chapter. Drugs are defined as “a substance intended for use in the diagnosis, cure, mitigation, treatment or prevention of disease; a substance (other than food) intended to affect the structure or any function of the body; and a substance intended for use as a component of a medicine but not a device or a component, part or accessory of a device.” 3 Medications include, but are not limited to, any product considered a drug by the Food and Drug Administration (FDA). 3 Given the number and variety of definitions for medication errors, the IOM has recommended that international definitions be adopted for medication error, adverse drug events, and near misses. 2
Medication Errors
One commonly used definition for a medication error is:
Any preventable event that may cause or lead to inappropriate medication use or patient harm while the medication is in the control of the health care professional, patient, or consumer. Such events may be related to professional practice, health care products, procedures, and systems, including prescribing; order communication; product labeling, packaging, and nomenclature; compounding; dispensing; distribution; administration; education; monitoring; and use. 4
Some of the factors associated with medication errors include the following:
- Medications with similar names or similar packaging
- Medications that are not commonly used or prescribed
- Commonly used medications to which many patients are allergic (e.g., antibiotics, opiates, and nonsteroidal anti-inflammatory drugs)
- Medications that require testing to ensure proper (i.e., nontoxic) therapeutic levels are maintained (e.g., lithium, warfarin, theophylline, and digoxin)
Look-alike/sound-alike medication names can result in medication errors. Misreading medication names that look similar is a common mistake. These look-alike medication names may also sound alike and can lead to errors associated with verbal prescriptions. The Joint Commission publishes a list of look-alike/sound-alike drugs that are considered the most problematic medication names across settings. (This list is available at www.jointcommission.org/NR/rdonlyres/C92AAB3F-A9BD-431C-8628-11DD2D1D53CC/0/lasa.pdf .)
Medication errors occur in all settings 5 and may or may not cause an adverse drug event (ADE). Medications with complex dosing regimens and those given in specialty areas (e.g., intensive care units, emergency departments, and diagnostic and interventional areas) are associated with increased risk of ADEs. 6 Phillips and colleagues 7 found that deaths (the most severe ADE) associated with medication errors involved central nervous system agents, antineoplastics, and cardiovascular drugs. Most of the common types of errors resulting in patient death involved the wrong dose (40.9 percent), the wrong drug (16 percent), and the wrong route of administration (9.5 percent). The causes of these deaths were categorized as oral and written miscommunication, name confusion (e.g., names that look or sound alike), similar or misleading container labeling, performance or knowledge deficits, and inappropriate packaging or device design.
Adverse Drug Events and Adverse Drug Reactions
Adverse drug events are defined as injuries that result from medication use, although the causality of this relationship may not be proven. 8 Some ADEs are caused by preventable errors. ADEs that are not preventable are often the result of adverse drug reactions (ADRs), which are defined as “any response to a drug which is noxious and unintended and which occurs at doses normally used for prophylaxis, diagnosis or therapy of disease, or the modification of physiological function, given that this noxious response is not due to medication error.” 9 Potential ADEs or near misses/close calls are medication errors that do not cause any harm to the patient because they are intercepted before they reach the patient or because the patient is able to physiologically absorb the error without any harm.
An adverse drug reaction is defined as “an undesirable response associated with use of a drug that either compromises therapeutic efficacy, enhances toxicity, or both.” 10 ADRs can be manifested as diarrhea or constipation, rash, headache, or other nonspecific symptoms. One of the challenges presented by ADRs is that prescribers may attribute the adverse effects to the patient’s underlying condition and fail to recognize the patient’s age or number of medications as a contributing factor. 11 According to Bates and colleagues, 12 more attention needs to be directed to ADEs—including both ADRs and preventable ADEs—which range in severity from insignificant to fatal.
Black Box Warnings and High-Alert Medications
In 1995, the FDA established the black box warning (BBW) system to alert prescribers to drugs with increased risks for patients. These warnings are intended to be the strongest labeling requirement for drugs or drug products that can have serious adverse reactions or potential safety hazards, especially those that may result in death or serious injury. 13 While the FDA does not issue a comprehensive list of drugs with BBWs, 14 some of the BBW drugs are celecoxib (Celebrex), warfarin, rosiglitazone (Avandia), methylphenidate (Ritalin), estrogen-containing contraceptives, and most antidepressants. 15 One study funded by the Agency for Healthcare Research and Quality found 40 percent of patients were taking a medication with a BBW and that many of those patients did not receive the recommended laboratory monitoring. The authors concluded that BBWs did not prevent the inappropriate use of high-risk medications. 16
Medication errors can be considered a sentinel event when they are associated with high-alert medications. According to the Institute for Safe Medication Practices (ISMP), “High-alert medications are those likely to cause significant harm when used in error.” The top five high-alert medications are “insulin, opiates and narcotics, injectable potassium chloride (or phosphate) concentrate, intravenous anticoagulants (heparin), and sodium chloride solutions above 0.9 percent” 17 (p. 339). ISMP’s list of high-alert medications is available at: www.ismp.org/tools/highalertmedications.pdf .
The Prevalence and Impact of Medication Errors
In the Harvard Medical Practice Study, Leape and colleagues 18 , 19 examined more than 30,000 hospital discharges selected at random from 51 hospitals in the State of New York in 1984. The researchers found that 3.7 percent of hospitalizations involved adverse events that prolonged hospital stay or were manifested as a new disability at the time of discharge. About one in four of these adverse events were judged to be attributable to negligence, and 58 percent were judged to be preventable.
It is difficult to reduce or eliminate medication errors when information on their prevalence is absent, inaccurate, or contradictory. Bates 20 put forth the notion that for every medication error that harms a patient, there are 100, mostly undetected, errors that do not. Most medication errors cause no patient harm or remain undetected by the clinician. 20 , 21 The low rate of detected errors makes assessing the effectiveness of strategies to prevent medication errors challenging.
Rates of medication errors vary, depending on the detection method used. For example, among hospitalized patients, studies have shown that errors may be occurring as frequently as one per patient per day. 5 , 22 In pediatric intensive care unit (ICU) studies, reported medication error rates have ranged from 5.7 23 and 14.6 per 100 orders 24 to as high as 26 per 100 orders. 25
The impact of medication errors on morbidity and mortality were assessed in a case-control analysis of ADEs in hospitalized patients during a 3-year period. 26 The investigators found significant increases in (a) the cost of hospitalization from increased length of stay, ranging from $677 to $9,022; (b) patient mortality (odds ratio = 1.88 with a 95% confidence interval); and (c) postdischarge disability. The impact was less in male patients, younger patients, and patients with less severe illnesses and in certain diagnosis-related groups.
Without an infrastructure to capture and assess all medication errors and near misses, the real number is not known. These rates could be expected to be higher once patient safety organizations begin to collect nationwide errors and health care clinicians become more comfortable and skilled in recognizing and reporting all medication errors. The concern raised in To Err Is Human 1 about the potential prevalence and impact of ADEs—2 out of every 100 hospitalized patients—was just the beginning of our understanding of the potential magnitude of the rates of medication errors. The concern continues, as is seen in the most recent IOM report, Preventing Medication Errors, 2 which states that “a hospital patient is subject to at least one medication error per day, with considerable variation in error rates across facilities” (pp. 1–2). Yet, despite numerous research findings, we cannot estimate the actual rates because they vary by site, organization, and clinician; because not all medication errors are detected; and because not all detected errors are reported.
Error-Prone Processes
There are five stages of the medication process: (a) ordering/prescribing, (b) transcribing and verifying, (c) dispensing and delivering, (d) administering, and (e) monitoring and reporting. 2 Monitoring and reporting is a newly identified stage about which there is little research. Some of the most noted and early work on medication safety found hospitalized patients suffer preventable injury or even death as a result of ADEs associated with errors made during the prescribing, dispensing, and administering of medications to patients, 12 , 27–29 although the rates of error in the stages of the medication process vary. A few studies have indicated that one of every three medication errors could be attributed to either a lack of knowledge about the medication or a lack of knowledge about the patient. 30
Prescribing/ordering
Of the five stages, ordering/prescribing most often initiates a series of errors resulting in a patient receiving the wrong dose or wrong medication. In this stage, the wrong drug, dose, or route can be ordered, as can drugs to which the patient has known allergies. Workload, knowledge about the prescribed drug, and attitude of the prescriber—especially if there is a low perceived importance of prescribing compared with other responsibilities—are significantly associated with ADEs. 31 , 32 Furthermore, if nurses or pharmacists question a prescriber about an order, they can be confronted with aggressive behavior, which may inhibit future questioning and seeking clarification. 33 The proportion of medication errors attributable to the ordering/prescribing stage range from 79 percent 29 to 3 percent. 34 Examples of the types of errors committed in this stage include illegible and/or incomplete orders, orders for contraindicated medications, and inappropriate doses. Similar results have been found in mandatory adverse event reporting systems. An analysis of 108 reports associated with significant harm or death reported to the State of New York noted that, when the error occurred during the prescribing stage, written prescriptions accounted for 74 percent of the errors, and verbal orders accounted for 15 percent. 6
While the preponderance of the research focuses on physician prescribing, there is a brief discussion about the role of advanced practice nurses in prescribing to ensure safety. One investigation of the occurrence of ADRs in outpatient veterans found no difference in ADR events between physicians and nurse practitioners. 11 Prescribers may make changes in medication therapy (e.g., change the dosage or discontinue the medication) in response to ADRs (e.g., constipation, rash) or other indications communicated to them by nurses or patients.
Transcribing, dispensing, and delivering
In some settings, medication orders are transcribed, dispensed, and then delivered for nurse administration. In certain circumstances and settings, both nurses and pharmacists are involved in transcribing, verifying, dispensing, and delivering medications. Yet errors of these two stages (transcribing and verifying, dispensing and delivering) have been predominately studied for pharmacists. Pharmacists can have an important role in intercepting and preventing prescribing/ordering errors. 35 One study found that while dispensing errors were 14 percent of the total ADEs, pharmacists intercepted 70 percent of all physician ordering errors. 27 Pharmacy dispensing errors have been found to range from 4 percent to 42 percent of errors. 36 Examples of errors that can be initiated at the transcribing, dispensing, and delivering stages include failure to transcribe the order, incorrectly filling the order, and failure to deliver the correct medication for the correct patient.
Medication administration
Nurses are primarily involved in the administration of medications across settings. Nurses can also be involved in both the dispensing and preparation of medications (in a similar role to pharmacists), such as crushing pills and drawing up a measured amount for injections. Early research on medication administration errors (MAEs) reported an error rate of 60 percent, 34 mainly in the form of wrong time, wrong rate, or wrong dose. In other studies, approximately one out of every three ADEs were attributable to nurses administering medications to patients. 21 , 28 In a study of deaths caused by medication errors reported to the FDA from 1993 to 1998, injectable drugs were most often the problem; 7 the most common type of error was a drug overdose, and the second most common type of error was administering the wrong drug to a patient. The 583 causes of the 469 deaths were categorized as miscommunication, name confusion, similar or misleading labeling, human factors (e.g., knowledge or performance deficits), and inappropriate packaging or device design. The most common causes were human factors (65.2 percent), followed by miscommunication (15.8 percent).
Nurses are not the only ones to administer medications. Physicians, certified medication technicians, and patients and family members also administer medications. Part of the challenge in understanding the impact of nursing in medication administration is the need for research that clearly differentiates the administrators of medications. Several studies have reported medication administration errors that have included nonnurses. 37 , 38 Among many reasons for the prevalence of nurse involvement in medication errors is that nurses may spend as much as 40 percent of their time in medication administration. 39
A large-scale study by the U.S. National Council of State Boards of Nursing assessed whether there were any identifiable characteristics common to those nurses who committed medication administration errors. The most significant finding was that “the age, educational preparation and employment setting of RNs disciplined for medication administration errors are similar to those of the entire RN population” 40 (p. 12).
The “rights” of medication administration include right patient, right drug, right time, right route, and right dose. These rights are critical for nurses. A survey of patients discharged from the hospital found that about 20 percent were concerned about an error with their medications, and 15 percent of them were concerned about being harmed from mistakes by nurses compared to 10 percent who were concerned about mistakes by physicians. 41 However, the complexity of the medication process has led to the formulation of the rights of nurses in the area of medication administration. The essential environmental conditions conducive to safe medication practices include (a) the right to complete and clearly written orders that clearly specify the drug, dose, route, and frequency; (b) the right to have the correct drug route and dose dispensed from pharmacies; (c) the right to have access to drug information; (d) the right to have policies on safe medication administration; (e) the right to administer medications safely and to identify problems in the system; and (f) the right to stop, think, and be vigilant when administering medications. 42
Types of Medication Errors
Leape and colleagues 27 reported more than 15 types of medication errors: wrong dose, wrong choice, wrong drug, known allergy, missed dose, wrong time, wrong frequency, wrong technique, drug-drug interaction, wrong route, extra dose, failure to act on test, equipment failure, inadequate monitoring, preparation error, and other. Of the 130 errors for physicians, the majority were wrong dose, wrong choice of drug, and known allergy. Among the 126 nursing administration errors, the majority were associated with wrong dose, wrong technique, and wrong drug. Each type of error was found to occur at various stages, though some more often during the ordering and administration stages.
Since the study by Leape and colleagues, research has captured some of the types of error identified by Leape and added yet others (e.g., omission due to late transcription, 43 wrong administration technique, 24 , 44 , 45 and infiltration/extravasation. 46 Reporting incidences by type of error, rather than the stage it was associated with, leads to equivocal implications for nursing practice. The categorization approach used determines whether the implication can be targeted to stage, and therefore discipline, or to types of error. For example, 11 studies reported rates of types of medication errors using institution-specific and national databases, yet not specifying whether the error occurred during the prescribing, dispensing, or administration stage of the medication process or not clearly specifying administration errors associated with nurse administration. One of these studies analyzed deaths associated with medication errors, finding that the majority of deaths were related to overdose and wrong drug 7 —again, not specified by stage. Yet among these, it may be possible to see that wrong dose, dose omission, wrong drug, and wrong time are the most frequent type of medication error. Even then, comparisons and practice implications are challenging due to the lack of standardization among the types of categories used in research.
Working Conditions Can Facilitate Medication Errors
Following the release of To Err Is Human , 1 the focus on deaths caused by medication errors targeted system issues, such as high noise levels and excessive workloads, 47 and system interventions, such as the need for computerized order entry, unit dose (e.g., single-dose packaging), and 24-hour pharmacy coverage. 48 The IOM’s report, Crossing the Quality Chasm , 49 put forth the concept that poor designs set the workforce up to fail, regardless of how hard they try. Thus, if health care institutions want to ensure safer, higher-quality care, they will need to, among other things, redesign systems of care using information technology to support clinical and administrative processes.
We are at the beginning stage of assessing and understanding the potential association between working conditions/environment and medication errors. Early research in this area found a relationship between characteristics of the work environment for nurses and medication errors. 30 , 50 , 51 For example, Leape and colleagues 27 found an association between the occurrence of medication errors and the inability to access information and failure to follow policies and guidelines. Also, research has found that health care clinicians should be aware of the repeated patterns of medication errors and near misses to provide insight on how to avoid future errors. 52
The system approach to safety emphasizes the human condition of fallibility and anticipates that errors will occur, even in the best organizations with the best people working in them. This approach focuses on identifying predisposing factors within the working environment or systems that lead to errors. 53 Reason’s 53 model of accident causation describes three conditions that predicate an error:
- Latent conditions —Organizational processes, management decisions, and elements in the system, such as staffing shortages, turnover, and medication administration protocols.
- Error-producing conditions —Environmental, team, individual, or task factors that affect performance, such as distractions and interruptions (e.g., delivering and receiving food trays), transporting patients, and performing ancillary services (e.g., delivery of medical supplies, blood products). 49
- Active failures —errors involving slips (actions in which there are recognition or selection failures), lapses (failure of memory or attention), and mistakes (incorrect choice of objective, or choice of an incorrect path to achieve it), compared to violation, where rules of correct behavior are consciously ignored.
Threats to medication safety include miscommunication among health care providers, drug information that is not accessible or up to date, confusing directions, poor technique, inadequate patient information, lack of drug knowledge, incomplete patient medication history, lack of redundant safety checks, lack of evidence-based protocols, and staff assuming roles for which they are not prepared. An additional risk is a hospital without 24-hour pharmacy coverage, especially when procedural barriers to offset the risk of accessing high-risk drugs are absent. 6
Recognizing and Reporting Medication Administration Errors
Error reporting strategies are critical to the implementation of effective system-level approaches to reduce medication errors and ADEs. 54 However, the usefulness of many reporting strategies depends directly on the level of response. 55 To be effective, medication error reporting needs to be ongoing and part of a continuous quality improvement process. 56 , 57
Previous research has found that when nurses voluntarily report medication administration errors, as few as 10 to 25 percent of errors are reported. 28 As discussed in the chapter on error reporting, there were numerous surveys of hospital nurses’ perceptions of what constitutes an MAE, why these types of errors occur, 58–61 and what the barriers to reporting are. 58–72 The three most significant barriers to reporting were (a) a hierarchical hospital culture/structure where the nursing staff disagreed about the definition of reportable errors, (b) fear of the response and reaction of hospital management/administrators and peers to a reported error, and (c) the amount of time and effort involved in documenting and reporting an error. Together these studies indicate that the medication errors that are reported do not represent the actual incidence of medication errors.
Without reporting, many errors may not be known. Based on a survey of nurses on barriers to reporting, Wakefield and colleagues 62 suggested several strategies to increase the reporting of MAEs: agreement on the definition of error; supporting and simplifying reporting of errors; institutionalizing a culture that rewards and learns from error reporting (i.e., a culture of safety, where learning is encouraged and blaming discouraged); capitalizing on feedback reports to determine system factors contributing to error; and ensuring positive incentives for MAE reporting.
Incident reports, retrospective chart reviews, and direct observation are methods that have been used to detect errors. Incident reports, which capture information on recognized errors, can vary by type of unit and management activities; 73 they represent only a few of the actual medication errors, particularly when compared to a patient record review. 74 Chart reviews have been found to be most useful in detecting errors in ordering/prescribing, but not administration. 75 , 76 Direct observation of administration with comparison to the medication administration record detects most administration errors; however, it cannot detect ordering errors and, in some systems, transcribing and dispensing errors. There were two studies that compared detection methods. One of these studies of medication administration in 36 hospitals and skilled nursing facilities found 373 errors made on 2,556 doses. 77 The comparison of three detection methods found that chart review detected 7 percent of the observed errors, and incident reports detected only 1 percent. Direct observation was able to detect 80 percent of true administration errors, far more than detected through other means. A second study compared detection methods and found that more administration errors were detected by observation (a 31.1 percent error rate) than were documented in the patients’ medical records (a 23.5 percent error rate). 78 Therefore, no one method will do it all. When automated systems that use triggers are not in place, multiple approaches such as incident reports, observation, patient record reviews, and surveillance by pharmacist may be more successful. 79
The wide variation in reported prevalence and etiology of medication errors is in part attributable to the lack of a national reporting system or systems that collect both errors and near misses. State-based and nationally focused efforts to better determine the incidence of medication errors are also available and expanding (Patient Safety and Quality Improvement Act of 2005). The FDA’s Adverse Event Reporting System (AERS), which is part of the FDAs’ MedWatch program ( www.fda.gov/medwatch ), U.S. Pharmacopeia’s (USP’s) MEDMARX ® database ( www.medmarx.com ), and the USP’s Medication Errors Reporting Program (MERP; www.ismp.org/orderforms/reporterrortoISMP.asp ), in cooperation with the ISMP, collect voluntary reports on actual and potential medication errors, analyze the information, and publish information on their findings.
Research reported to date clearly reveals that medication errors are a major threat to patient safety, and that these errors can be attributed to all involved disciplines and to all stages of the medication process. Unfortunately, the research also reveals that we have only weak knowledge of the actual incidence of errors. Our information about ADEs (those detected, reported, and treated) is better, but far from complete. With this knowledge of the strengths and limitations of the research, this chapter will consider the evidence regarding nurses’ medication administration.
Research Evidence—Medication Administration by Nurses
The research review targeted studies involving medication administration by nurses. This excluded several studies that assessed medication administration errors without differentiating whether the errors were associated with physicians, assistants, or nurses. None of these studies included interventions.
Rates and Types of Medication Administration Errors
Thirteen studies explicitly reported types of MAEs associated with nurses. The incidence of MAEs was detected either formally through incident reports, chart reviews, or direct observation, or informally through anonymous surveys. Two studies conducted retrospective assessments, one using medical records 43 and the other malpractice claims. 80 Seven studies assessed self-reported MAEs from a nationally representative database 44 , 81–83 or self-reported errors using a nationally representative sample. 84–86 None of these self-reported MAEs were verified. Eight studies assessed MAEs using direct observation of the medication administration process. 24 , 37 , 78 , 87–91
The incidence of MAEs varied widely with the different research designs and samples. Using chart reviews, Grasso and colleagues 43 found that 4.7 percent of doses were administered incorrectly. Direct observation studies placed the estimate of total incorrect doses between 19 percent and 27 percent, 87 and when an extra review was done to separate the errors into stages of the medication process, between 6 percent and 8 percent of doses were in error because of administration. The majority of types of MAEs reported were wrong dose, wrong rate, wrong time, and omission. All of the studies reviewed here reported wrong drug and dose, but varied across the other types of MAE categories (see Evidence Table 1 ); this was dependent upon the study methodology.
Evidence Table 1
Types of Reported and Observed Medication Administration Errors (MAEs)
Five studies evaluated self-reported MAEs, involving incident reports and informal reports. 38 , 44 , 81 , 82 The most common types of reported errors were wrong dose, omission, and wrong time. Four of these studies 38 , 81–83 assessed a large secondary, nationally representative database containing MAEs reported to the MEDMARX database over five years. 38 , 81 , 82 , 44 found in the error reports submitted by nursing students that the majority of MAEs were associated with omission, wrong dose, wrong time, and extra dose. Of the reported contributing factors, 78 percent were due to the inexperience of the nurse. The Beyea and Hicks 81 , 82 studies looked at errors associated with the operating room, same-day surgery, and postanesthesia; they found the majority of errors attributable to administration but did not classify them by error type. The other study reviewed 88 incident reports from a long-term care facility submitted during a 21-month period. It found that the majority of MAEs were associated with errors involving interpreting or updating the medication administration record, delayed dose, wrong dose, or wrong drug. 92 A separate component of this study surveyed administrative and clinical nurses and found that they believed the majority of medication errors occurred at either the administration or dispensing stage.
Two other studies assessed the type of MAEs reported by nurses in nationwide surveys. 84 , 85 While the majority (57 percent) of errors reported by critical care nurses involved MAEs, an additional 28 percent of reported errors involved near misses. Medication administration errors involving wrong time, omission, and wrong dose accounted for 77.3 percent of errors, while wrong drug and wrong patient accounted for 77.8 percent of near misses. The most frequent types of medication errors were wrong time (33.6 percent), wrong dose (24.1 percent), and wrong drug (17.2 percent), and the three most frequent types of near misses were wrong drug (29.3 percent), wrong dose (21.6 percent), and wrong patient (19.0 percent). 85 Many of the reported MAEs in ICUs involved intravenous medications and fluids. 84 In these surveys, the nurses who reported making errors described between two and five errors during a 14-day period.
At the more advanced stage of incident reports, one study reviewed 68 malpractice cases involving MAEs in Sweden. 80 Among the cases reviewed, the majority of MAEs made by nurses involved wrong dose. When the nurses delegated the drug administration to subordinate staff, the majority of MAEs involved wrong drug or wrong concentration of a drug. Errors, which were reported to the immediate supervisor, were also reported to the physician in 65 percent of cases. The reported causes of MAEs were lack of administration protocols, failure to check orders, ineffective nurse supervision when delegating administration, and inadequate documentation.
One study assessed medication errors using 31 medical records of patients discharged from a psychiatric hospital and found a total of 2,194 errors. 43 Of these, 997 were classified as MAEs (4.7 percent of all doses, and 66 percent of all errors). Of these, 61.9 percent were due to scheduled doses not documented as administered, 29.1 percent as drugs administered without an order, 8 percent as missed doses because of late transcription, and 3 percent resulting from orders not being correctly entered in the pharmacy computer.
Comparison of the Incidence of Medication Administration Errors by Type Categories
The number of studies using direct observation of medication administration is increasing in response to the concern about the accuracy of other sources of data. Ten studies were found, only three of which were done in the United States. While we attempt to summarize across these studies, it is difficult to determine consistency across studies as each focused on different sets of errors (some only intravenous errors, some included gastrointestinal tube technique) and were conducted in different settings. In many of the non-U.S. studies, nurses dispensed drugs from ward stock and prepared many of the intravenous solutions for administration.
Three observational studies were conducted in pediatric units—one in France, 78 one in Switzerland, 25 and one in the United States. 24 Buckley 24 reported 52 of the 263 doses (19 percent) observed to be in error, but only 15 (6 percent) of those were in the administration stage. Those 15 were nearly evenly divided among wrong dose, wrong time, wrong technique, and extra dose categories. Prot 78 reported nearly 50 percent more MAEs. Of the 1,719 observed doses, 467 (27 percent) were in error, including wrong time; excluding wrong-time errors, the error rate was 13 percent of doses. The categories with the most MAEs in Prot’s study were wrong time, wrong route (GI tube versus oral), wrong dose, unordered drug, wrong form, and omissions. Schneider and colleagues 25 reported an overall 26.9 percent error rate with wrong-time errors, and an 18.2 percent rate excluding wrong-time errors. Common errors in addition to wrong time were wrong dose preparation and wrong administration technique.
The incidence of intravenous drug errors was observed in three studies, one in England, 89 one in Germany, 90 and one in both countries. 37 About 50 percent of the doses were determined to contain at least one error. Compared to other studies, this rate is surprisingly high, and it included preparation technique errors (selection of diluent/solvent) as well as administration errors (rate of bolus injection and infusion rate). Part of the explanation may come from institutional (type of pharmacy support available) and professional training factors. (German nurses are not trained to do intravenous medications.)
Three studies focused on medication administration in ICUs in the United States, 45 in France, 91 and in the Netherlands. 94 Kopp and colleagues 45 looked at all medication errors and report that 27 percent of doses were in error; of these 32 percent could be attributed to the administration stage. Within the MAEs, most were omitted medications; the rest were evenly distributed among wrong dose, extra dose, and wrong technique. Few wrong-time errors were noted. Tissot 91 and van den Bernt 94 examined only administration stage errors and reported very different rates. Tissot reported 6.6 percent of the 2,009 observed doses were in error, most from wrong dose, wrong rate, and wrong preparation technique. Excluding wrong-time errors, van den Bernt reported a 33 percent error rate that included preparation errors with diluent/solvent issues, infusion-rate errors, and chemical incompatibility of intravenous drugs. It is likely that the differences in rates across these studies are due to the range of error types observed in each study as well as the varying responsibilities of nurses in the three countries.
The most extensive observation study, by Barker and colleagues, 87 conducted observations of medication administration in 36 randomly selected health care facilities (acute and long-term care) in two States in the United States. Of the 3,216 doses observed, 605 (19 percent) contained at least one error. Nearly half of those errors were wrong-time errors. Other common types of errors included omission, wrong dose, and unauthorized (unordered) drug. In a much smaller study conducted in the Netherlands, Colen, Neef, and Schuring 88 found an MAE rate of 27 percent, with most of these wrong-time errors. The rate of MAEs without wrong time was approximately 7 percent, and most of those were omissions.
Information from these research studies forms a consistent picture of the most common types of MAEs. These are wrong time, omissions, and wrong dose (including extra dose). Rates of error derived from direct observation studies ranged narrowly between 20 and 27 percent including wrong-time errors, and between 6 and 18 percent excluding wrong-time errors. The alarming exception to this was the nearly 50 percent error rate in observation of intravenous medication in ICUs in Europe.
Impact of Working Conditions on Medication Errors
Medication safety for patients is dependent upon systems, process, and human factors, which can vary significantly across health care settings. A review of the literature found 34 studies that investigated some aspect of working conditions in relation to medication safety.
Systems factors
Systems factors that can influence medication administration include staffing levels and RN skill mix (proportion of care given by RNs), shift length, patient acuity, and organizational climate. There were 13 articles presenting research findings and three literature reviews. The major systems/organizational factors included nurse staffing, workload, organizational climate/favorable working conditions, policies and procedures, and technologies enabling safety or contributing to MAEs.
Nurse staffing
Medication administration is a key responsibility of nurses in many settings, and three studies assessed the relationship between nurse staffing, hours of nursing care in hospitals, RN skill mix, and medication errors. Two studies associated the total hours of care and the RN skill mix at a patient care unit to reported medication error rates in those units; one study used 42 units in a large Midwestern hospital 95 and the other used 39 units in 11 small hospitals. 96 Rates of MAEs, when the number of doses was the denominator, were highest in medical-surgical and obstetric units; when patient days were the denominator, the highest rate was in ICUs. In both studies the type of unit was controlled and the rate of reported medication errors declined as the RN skill mix increased up to an 87 percent mix. A third study of nurses in ICUs in 10 hospitals found an inverse relationship between rates of medication errors and staffing work hours per patient day in specific settings (e.g., cardiac ICUs and noncardiac intermediate care settings). A little over 30 percent of the variance in medication error rates resulted from the variance in staffing work hours per patient day. 97
Other studies conducted prior to 1998 did not find a relationship between staffing and medication errors. Three literature reviews, 30 , 39 , 98 concluded that the direct evidence for a relationship between staffing and MAE rates was inconsistent. Nurses’ perceptions of the impact of staffing or workload on medication errors, however, is quite consistent.
These findings are consistent with three studies and two literature reviews on the impact of heavy workloads, a component of nurse staffing, on errors. In one survey of nurses in 11 hospitals, both pediatric and adult nurses reported staffing ratios and the number of medications being administered as being the major reasons why medication errors occur. 58 A second survey found that nurses from Taiwan also indicated that workload was a major factor in medication errors. 93 Beyea, Hicks, and Becker 81 , 82 and Hicks and colleagues 38 analyzed MEDMARX data for medication errors in the operating room, postanesthesia, and in same-day-surgery units. Most of these errors involved nurses (64–76 percent) and medication administration (59–68 percent). In all three sets of error reports, workload increases and insufficient staffing were noted to be causes of errors.
The effect of heavy workloads and inadequate numbers of nurses can also be manifested as long workdays, providing patient care beyond the point of effective performance. In a national survey by Rogers and colleagues, 99 self-reported errors by nurses found that the likelihood of a medication error increased by three times once the nurse worked more than 12.5 hours providing direct patient care. Among nurses working more than 12.5 hours, the reported errors, 58 percent of actual errors and 56 percent of near misses were associated with medication administration.
Other findings support the importance of adequate nurse staffing and understanding the impact of shift work in decreasing medication errors. A review of incident reports found that the major contributing factors to errors were inexperienced staff, followed by insufficient staffing, agency/temporary staffing, lack of access to patient information, emergency situation, poor lighting, patient transfers, floating staff, no 24-hour pharmacy, and code situations. 44 Certain aspects of shift work can also impact medication safety, as shown in a review of research conducted in the 1980s and early 1990s that indicated that there was a difference in the number of errors by shift, but no difference in the number of hours worked (8 versus 12 hours). However, there were more errors with nurses working rotating shifts. 30
Organizational climate
Other systems/organizational issues include the presence of favorable working conditions, effective systems, policies and procedures, and technologies that enable safety or contribute to MAEs. An assessment of medication administration behaviors of 176 nurses in rural Australia, using structural equation modeling to test the association between organizational climate and the administration behaviors of nurses, found that the variable “violations” was the only variable with a direct contribution to MAEs, but there was no direct linkage to actual errors. While it was not possible to determine the effect of organizational climate on violations, distress was positively associated with violations, while quality of working life, morale, and organizational climate had a negative association. The organizational climate was found to be linked with safety behavior. 100 Hofmann and Mark 101 did find that the safety climate on patient care units was linked to the rate of harm-producing medication errors in a study using data collected from 82 units in 41 hospitals. Higher overall safety climate was related to lower rates of medication errors and urinary tract infections.
Policies, procedures, and protocols
Lack of appropriate policies, procedures, and protocols can impact medication safety, as seen in a few small studies. In a study of malpractice cases, medication errors were associated with lack of administration protocols and ineffective nurse supervision in delegating administration. 80 However, even when policies are in place, they may not necessarily improve safety. For example, a review of two studies in the literature found that medication errors did not necessarily decrease with two nurses administering medications (e.g., double-checking). 30 In addition, appropriate policies may not be followed. Double-checking policies are commonly used as a strategy to ensure medication safety. When errors occurred under such policies, failure to double-check doses by both pediatric and adult nurses 58 and nurses in a Veterans Affairs (VA) hospital 102 were reported. However, research presented in two literature reviews offers somewhat conflicting information. In the first review of three studies, following double-checking policies did not necessarily prevent errors. 39 Yet in the other review, failure to adhere to policies and procedures was associated with errors. 30
Process factors
Process factors that influence medication administration include latent failures that can instigate events resulting in errors, such as administrative processes, technological processes, clinical processes, and factors such as interruptions and distractions. These factors reflect the nature of the work, including “competing tasks and interruptions, individual vs. teamwork, physical/cognitive requirements, treatment complexity, workflow.” 103 A review of the literature found 18 studies and 2 literature reviews that contained process factors and their association to medication errors by nurses.
Distractions and interruptions
Factors such as distractions and interruptions, during the process of delivering care can have a significant impact on medication safety. Nine studies, four with nationwide samples, and two literature reviews present information on the association between MAEs and distractions and interruptions. One survey of nurses in three hospitals in Taiwan found that they perceived distractions and interruptions as causes of errors. 93 In three other surveys in the United States, nurses ranked distractions as major causes for the majority of medication errors. 58 , 61 , 102 In a small, five-site observational study of medication administration among 39 RNs, licensed practical nurses (LPNs) and certified medical technicians/assistants (CMT/As), Scott-Cawiezell and colleagues 104 found an increase in medication errors attributable in part to interruptions, and when wrong-time errors were excluded, the error rate actually increased during medication administration.
These finding are furthered by research concerning self-reported errors from a nationwide sample of nurses. 84 The nurses believed the cause of their reported medication errors and near errors were interruptions and distractions. In a secondary analysis of the MEDMARX ® data base, distractions and interruptions were prominent contributing factors to medication errors. 81–83 Furthermore, these findings are supported by three reviews of the literature: one found that distractions and interruptions interfered with preparing and administering medication, potentially causing errors; 30 interruptions were perceived as causing medication errors in the second review; 98 and the third indicated that rapid turnover and changes as well as distractions and interruptions contributed to errors. 39
Documentation of the medication administration process
One small study investigated nurse adherence to a hospital policy to document medications administered and their effects on patients. From a sample of 12 nurses in one hospital, one-third of progress notes were found to contain information about administered medications, yet only 30 percent of those progress notes included medication name, dose, and time of administration, and only 10 percent documented information about desired or adverse effects of medications. Medication education, outcomes of administered medication, and assessment prior to administering were not documented in any progress note. Only half of withheld medications were documented. 105 In a review of records to detect medication errors, Grasso and colleagues 43 found that 62 percent did not document doses as administered.
Communication
Five studies and one literature review assessed the relationship between communication failures and medication errors. A small observational study of 12 nurses found that they communicated with other nurses about information resources on medications, how to troubleshoot equipment problems, clarification in medication orders, changes in medication regimens, and patient assessment parameters when handing over patients. 106 Nurses communicated with physicians informally to exchange information, about the absence of other physicians, and in both unstructured and structured ward rounds. Nurses also communicated with pharmacists about information on medication administration and organizing medications for patient discharge. Another direct observational study of medication administration found opportunities for errors associated with incomplete or illegible prescriptions. 91 This finding was supported by two related literature reviews that indicated that illegible and poorly written drug prescriptions and breakdowns in communication led to errors. 30 , 39 Another survey found that nurses ranked difficult/illegible physician handwriting as a cause of the majority of medication errors, but did not consider withholding a dose because a lab report was late or omitting a medication while the patient was sleeping as something that should have been communicated to physicians or others. 61
A small survey of 39 nurses in three hospitals in Nova Scotia about communication failures during patient transfers found that more than two-thirds of nurses reported difficulty in obtaining an accurate medication history from patients when they were admitted; 82 percent reported patients were unable to provide accurate medication histories. When patients were transferred from across units, 85 percent of nurses reported that medication orders were rewritten at transfer, 92 percent that medication orders were checked against electronic medical records, 62 percent that it was time consuming to clarify medication orders, 66 percent that the reasons for medication changes were made at transfer, and 20 percent that blanket orders are often written as transfer orders. 107
Three studies investigated the impact of complexity on medication safety. In a small, five site observational study of medication administration of 39 RNs, LPNs and CMT/As in long-term care settings, Scott-Cawiezell and colleagues 104 found that even though RNs administered fewer medications they had more MAEs, compared to LPNs and CMT/As. The suggested explanation was that the mediations RN must administer in long-term care are those with more complexity. Another survey of 284 RNs in 11 hospitals found that pediatric and adult nurses reported numbers of medications being administered as a major reason on why medication errors occur. 58 Also, another survey of nurses found that they perceived that complicated doctor-initiated orders (24 percent) and complicated prescription were the major causes of MAEs related to the medication administration process. 93
Equipment failure while administering medication
Three studies found that systems and process factors can interfere with medication administration when equipment used in administration does not perform properly, exposing the nurse and patient to safety risks. In two ICU studies, infusion pump problems were involved in 6.7 percent of 58 MAEs in one study 24 and 12 percent of the 42 MAEs in the other sutdy. 45 Another investigation of smart pumps with integrated decision-support software found that half of the ADEs were considered preventable (2.12 of 100 patient-pump days), and 72 percent of preventable ADEs were serious or life-threatening. 108 Given the number of ADEs, the fact that the drug library was bypassed in 24 percent of the infusions, and the frequency of overriding alerts, the investigators concluded that use of the smart pumps did not reduce the rate of serious medication errors—but possibly could if certain process factors could be modified, such as not allowing overrides.
Monitoring and assessing
An essential component of the medication process related to the administration of medications is monitoring and assessing the patient by the nurse. Only two studies provided information in this area, offering scant evidence. In the first, based on a small sample of nurses in one unit in one hospital, a qualitative analysis of observed medication administration found that participants monitored patients before, during, and after medication administration. 109 Nurses assessed vital signs, lab values, ability to swallow, and patients’ self- report of health. They also felt responsible for timing medication administration and providing as-needed (e.g., PRN) medications. In the second study, where ICU nurses were surveyed, no administration errors were found to be associated with inadequate monitoring or lack of patient information. 24
Effects of Human Factors on Medication Administration Errors
There are a wide range of system-related human factors that can impact medication administration. These factors include characteristics of individual providers (e.g., training, fatigue levels), the nature of the clinical work (e.g., need for attention to detail, time pressures), equipment and technology interfaces (e.g., confusing or straight-forward to operate), the design of the physical environment (e.g., designing rooms to reduce spread of infection and patient falls), and even macro-level factors external to the institution (e.g., evidence base for safe practices, public awareness of patient safety concerns). 103 There were 10 studies that assessed the association of human factors with MAEs. Four major themes emerged in the review: fatigue, cognitive abilities, experience, and skills.
Effects of fatigue and sleep loss
Five studies assessed the association between fatigue and sleep loss with MAE errors. The first specifically investigated the effects of fatigue and sleep loss on errors using a national sample of nurses over a 2-week period. In this study, the rate of errors increased after working 12.5 hours. 99 A subpopulation of critical care nurses reported forgetfulness, heavy workload, distractions, and high patient acuity as causes for their medication errors or near errors. 84 Fatigue and sleep loss was also a factor in a subpopulation of ICU nurses, who reported errors with high-alert medications (e.g., morphine, chemotherapeautic agents). 85 The other two studies assessed fatigue along with other variables associated with medication errors. In one of these, a survey of 57 nurses, respondents reported that the majority of medication errors were attributable to fatigue. 70 The other study, a survey of 25 nurses in one hospital, found that one of the most frequently perceived causes of medication errors for nurses was being tired and exhausted (33.3 percent). 102
The thought processes of nurses during medication administration was assessed in two studies. A semistructured, qualitative interview of 40 hospital nurses prior to implementation of a bar-coding system explored the thinking processes of nurses associated with medication administration. 110 Their thought processes involved analyzing situations and seeking validation or a solution when communicating about patients; using knowledge, experience, and understanding of patients’ responses to anticipate problems; integrating their knowledge of lab values and patterns of pathophysiological responses to determine possible need to change dosage or administration timing; checking orders for validity and correctness; assessing patients’ responses for possible side effects and effectiveness of the drug; using cues from patients or family members about need for explanations about drugs; bypassing protocols or procedures, some taking a risk, to get drugs to patients or use time more efficiently; anticipating needs for future problem solving; and applying professional knowledge during drug administration. The other study of nurses, using direct observation in a medical and surgical unit in Australia, found that participants used hypotheticodeductive reasoning to manage patient problems. 111 Graduate nurses used pattern recognition of patient characteristics and medications during decisionmaking. Intuition and tacit knowledge was used in relation to changes in patients’ vital signs and to objectively monitor patients.
Thought process can also be distorted by distractions and interruptions. One study employed direct observation of medication administration to determine the effects of human factors on MAEs. 24 The investigators found that slips and memory lapses were associated with 46.7 percent of MAEs. During both the prescribing and administration of medications, the causes of errors were attributable to slips and memory lapses (23.1 percent during prescribing vs. 46.7 percent during administration), lack of drug knowledge (46.2 percent during prescribing vs. 13.3 percent during administration), and rule violations (30.8 percent during prescribing vs. 13.3 percent during administration). Another study using direct observation found causes associated with MAEs to include slips and memory lapses (40 percent), rule violations (26 percent), infusion pump problems (12 percent), and lack of drug knowledge (10 percent). 45
Experience and skills also impact thought processes. In one study of 40 student nurses and 6 nurses using a computerized program to assess the impact of dyslexia found that the greater the tendency towards dyslexia, the poorer the potential cognitive ability to effectively provide the skills associated with effective drug administration. 112 Similarly, in two reviews of the literature, a number of medications errors were found to be caused by poor mathematical skills, 30 especially if mathematical skills were needed to properly administer drugs. 39
Lack of medication knowledge is a constant problem, and there is a need to continually gain more knowledge about current and new medications. 30 Nurses with more education and experience may have greater knowledge of medications. 39 However, experience has not been found to mitigate the effect of poor mathematical skills nor frequency of MAEs. 30 Those new to a unit or profession may be at risk for errors. 39 In a survey of nurses working in three hospitals in Taiwan, nurses reported causes of MAEs as new staff (37.5 percent), unfamiliarity with medication (31.9 percent), unfamiliarity with patient’s condition (22.2 percent), and insufficient training (15.3 percent). 93 Inexperience may also contribute to performance (human) deficit, willingness to follow a procedure/protocol, and knowledge deficit. Of these reported contributing factors, 78 percent were due to the inexperience of staff. 44 Blegen, Vaughn, and Goode 113 found that medication errors rates were inversely related to the proportion of nurses on a unit with greater experience, but were not related to the educational level of the staff on the unit.
Evidence Table 2
Working Conditions Associated With Medication Administration Errors and Adverse Drug Events
Strategies To Improve Medication Administration Safety
Strategies to improve medication safety focused on acute care settings. Twenty-six studies and descriptions of quality improvement projects were identified. Strategies used included recommendations from a nationwide voluntary organization to improve safety, education of nurses and other providers in safe practices, and system change and technology.
Nationwide voluntary efforts
Lucian Leape and colleagues 116 reported on a 15-month Institute for Healthcare Improvement Breakthrough Series Collaborative intended to reduce ADEs. Eight types of strategies were successfully used, including documentation of allergies, nonpunitive reporting, and standardizing medication administration times. Effective leadership and appropriateness of intervention were associated with successful change implementation. The converse was associated with failure, as were unclear aims, poorly designed interventions, lack of focus on underlying system failures, unclear measures, too much focus on data collection, involvement from only some stakeholders, opposition from physicians and nurses, and conflicting time demands for team members. The findings were limited by the lack of an analysis of the relationship between established safety policies and practices and the success of implementing new strategies, as well as the relationship between the implementation and the occurrence of ADEs.
A survey of 148 hospitals about the characteristics and barriers associated with adoption of the National Quality Forums’ 30 safe practices was done by Rask and colleagues. 117 These practices included unit dosing, adopting computerized physician order entry (CPOE), and having a culture of safety. Of the recommended practices, there was high adoption of standardized labeling and storage of medications (90.5 percent), identification of high-alert medications (81 percent), and use of unit doses (81 percent). For-profit hospitals were more likely than not-for-profit hospitals to have unit-dose medication distribution systems (93.1 percent vs. 78.2 percent) and policies on reading back verbal orders (83.1 percent vs. 58.4 percent). There were greater distractions affecting medication administration in large hospitals. Hospitals with 100–299 beds were more likely to report using pharmacists to review and approve nonemergency orders prior to dispensing; and, 69.4 percent of all hospitals used data analysis to drive patient safety quality improvement efforts.
Nurses’ education and training
Educational strategies aimed to improve medication safety and avert unnecessary medication errors. One randomized controlled study used an interactive CD-ROM education program to improve the use of safe medication practices and decrease the rate of MAEs. 118 Direct observation of medication administration was used to assess the impact. After the training, nurses’ use of safe administration practices increased, but preparation errors did not decrease. There were too few actual medication errors to analyze pre-post differences. Another approach used an 11 module Web-based educational strategy to improve drug safety with a small sample of nurses. 119 Direct observation of medication administration was used to determine the outcome. After using these modules, rates of nonintravenous MAEs decreased from 6.1 percent to 4.1 percent. Rates of errors in intravenous drug administration did not decline as expected. Dennison 120 reported the results of a medication safety training program for nurses. Knowledge scores improved in this pre-post test study, but there was no significant change in safety climate scores, labeling of intravenous infusion setups, or the number of self-reported errors.
Attempts to improve basic and continuing education in medication safety have been reported, but they have not assessed the impact on actual error rates. In a small pilot study, a problem-based learning approach was found to enable students to use findings from topic-specific research to develop and apply solutions for clinical problems. Papastrat and Wallace 121 proposed using problem-based learning and a systems approach to teach students how to prevent medication errors and suggested content, but their approach was not compared to other teaching methods. Another proposed educational strategy for practicing nurses was to use simulation of medication administration and errors in a controlled setting to improve medication safety, “duplicate the complexity of the nurse-patient interaction and related cognitive thought” 122 (p. 249). Simulations could be used to prepare nurses to recognize and manage medication errors when and if they occur.
System change
Several attempts to change the system have been tested. Some of the strategies addressed the thoroughness of error reporting, some the processes and events surrounding medication administration, and some focused directly on reducing errors. Using a hospitalwide performance improvement project that emphasized system factors, not individual blame, error reporting increased from a rate of 14.3 percent to 72.5 percent. 123 To address intravenous infusion problems, a medication safety education program and medication calculation worksheets were introduced, followed by ongoing Plan-Do-Study-Act cycles. 124 Multiple system changes were also used to improve safety of intravenous drug infusion. These included removing 90 to 95 percent of potassium chloride ampoules from the bedside; developing preprinted labels for five common drug infusions; removing four-channel infusion pumps the unit and replacing them with double-channel infusion pumps with a simple interface design; standardizing administration of drugs given by bolus dose using a syringe pump; decreasing missed doses of immunosupression drugs for transplant patients from 25 percent to 9 percent by incorporating them into the main drug chart; implementing standardized prefilter and heparin-lock central venous catheters and heparin infusions into ICU protocol; redesigning drug infusion administration practices throughout the hospital; eliminating burettes for IV drug infusion; preparing standardized drug infusions for 36 drugs; and providing Intranet-based up-to-date drug information.
A time study and focus groups were used to compare nurse efficiency during medication administration using either medication carts with unit doses or a locked wall-mounted cupboard in each patient room. 125 After 12 weeks, the wall-mounted units were found to have decreased medication administration time for nurses an average 23 minutes per 12-hour shift. Time saved by not having to search for missing medications saved 0.38 full-time equivalent (FTE) annually. Pharmacists spent an additional 0.05 FTE in stocking room cupboards. Nurses reported more contact time with patients when using room cupboards and fewer interruptions by colleagues during medication preparation and administration. Two small experimental studies attempted to reduce distractions that frequently interrupt nurses during medication administration and thereby introduce the potential for error. 126 , 127 In both studies a standardized protocol for safe administration of medications was introduced to the nursing staff in the experimental group and signage was used to remind others (physicians, patients, other staff) to not interrupt. The signage in the first study was a vest that the nurse administering medication wore; in the second it was a sign above the preparation area. Direct observation of the number and types of distractions provided the outcome measures in the first study; a questionnaire completed by each nurse administering medications provided the measure of distractions for the second. In both studies, the number of distractions was significantly reduced. Medication error rates were not captured.
One randomized controlled trial compared the use of a dedicated nurse for medication administration to nurses providing comprehensive care, including administering medications, to their patients in two hospitals. 128 MAEs were then assessed using direct observation. The investigators found the error rates to be 15.7 percent at the intervention hospital and 14.9 percent in the control hospital. The rate of MAEs was not significantly different between control and experimental groups.
Involving patients in the administration of medications while in the hospital is another system strategy that has been assessed. With this intervention, hospitalized patients have the responsibility for administering their own medication under the supervision of nursing staff. A literature review reported on 12 studies that described and evaluated a patient self-administration program. 129 This review found that the patients’ knowledge about their medications and the prescribed dosing increased, but knowledge about the potential side effects of their medications did not. Given the body of the reviewed literature, it appeared as though patients and families make as many or more MAEs than do health care providers.
System change with technology
Another rapid-cycle implementation project over 6 months used continuous quality improvement data before and after implementing a modular, computerized, integrated infusion system. 130 Most infusion error warnings occurred between 3 p.m. and 9 p.m., peaking at 6 p.m. Nurses responded to 12 percent of the infusion error warnings by altering the setting and averting errors. The nature of the 88 percent of warnings not responded to was not discussed. Risk scores associated with heparin infusion rates decreased almost fourfold. Almost all nurses used the new software correctly.
Two studies focused on documentation of medication administration. One study introduced a charting system with decision support and used a quasi-experimental design to determine the effects. 131 Researchers collected medication charting data for 8 weeks in both the control and study units. Staff in the study unit received an educational intervention about error avoidance through real-time bedside charting, followed by 12 weeks of monitoring and performance feedback. After the 12 weeks, medication charting rates increased from 59 percent to 72 percent in the intervention group. The second study used a computer-based “unreported meds followup” to remind nurse staff about scheduled medications omitted or not documented. 132 After charts were prospectively reviewed, a mandatory medication error prevention seminar was given to nurses, and a medication review report was created for nurses. Reported medication errors and documentation of medication administration were reviewed, medication administration policies were developed, and focus changed to the potential causes of errors. Documentation errors decreased over the 3 years of the study, and reported error rates increased by 0.5 percent each year.
Bar-coded medication administration (BCMA) is promoted as the most effective way to reduce administration errors and is being implemented widely. Conceptually this technology should catch nearly all errors, but rigorous evaluation of the impact of technology on error rates has lagged behind implementation. The biggest challenge to determining the effectiveness of BCMA or other interventions is the lack of valid measures of MAEs. Data from voluntary self-reported medication errors are known to capture only a small portion (5 percent to 50 percent) of actual errors, and the BCMA system itself greatly alters nurses’ awareness of errors, thereby systematically affecting reported error rates. Many studies reporting analysis of the impact of BCMA have used data collected by the system only after implementation. 133–136 From these we learn the types of errors intercepted by the system. Three other studies of the impact of BCMA on administration errors reported very large reductions: 59–70 percent decrease, 137 71 percent and 79 percent drops. 138 However, the sources of the data for determining these decreases are not known.
Direct observation of medication administration, a resource- and time-intensive approach to data collection, is the only way to gather unbiased data to evaluate the impact of BCMA on medication administration errors. Three studies have used direct observation; however, each evaluated the implementation of a different set of technology. Franklin and colleagues 139 reported a decline in MAE rates from 8.6 percent to 4.4 percent when a new system was implemented in a teaching hospital in England. The system included BCMA, computerized order entry, automated dispensing, and electronic medication administration record. Prescription errors also declined from 3.8 to 2 percent. It is noteworthy that the rate of both administration and prescribing errors by direct observation was much lower than other direct observation studies have reported. Paoletti and colleagues 140 used direct observation to determine the impact of BCMA and an electronic medication record in a hospital in the United States. They reported that the rate of MAEs declined from 13.5 percent to 3 percent. Finally, the implementation of only the electronic medication administration record led to a decline in MAEs from 10.5 percent to 6.1 percent using direct observation. 141 Health-related technology designed to increase medication safety has great promise, but more study using valid outcome measures and controlled interventions needs to be done to demonstrate the potential benefits.
Evidence Table 3
Strategies To Reduce Medication Administration Errors
- Evidence-Based Practice Implications
Medication safety is a significant issue in hospitals and throughout health care. Great improvements are needed, and hospitals are engaged in many efforts to reduce errors and increase this aspect of patient safety. Unfortunately, there is little evidence on which to base interventions. Based on the research literature, we can have confidence in only two aspects of our knowledge. First, data from voluntary self-reports of medication errors is neither reliable nor valid. Yet, this is the evidence most available for evaluating quality improvement. Interventions to improve the quality of voluntary self-report data include changing the culture to focus on system issues rather than individual deficiencies and having explicit and visible quality management system responses to these data. Staff who do not fear the response to an error report and see that the reports are used to improve quality are much more likely to take the time to report.
The second area about which there is some consensus in the literature is the rate and types of medication administration errors that commonly occur. Using the more reliable and valid data from direct observation studies, we see that the proportion of doses in error is between 20 and 27 percent counting wrong-time errors and between 7 and 18 percent without the wrong-time errors. MAEs are most likely to be wrong time, omissions, and wrong dose (wrong or extra dose). Because the nurse is often the last health care provider in the medication-use process, no one, except the patient, is in a position to intercept those errors. Given the number of medication doses administered each day in U.S. hospitals, the probable number of errors is truly staggering. If hospital patients get 10 doses of medication each day, at least 1 and possibly 3 of those will be wrong.
While the research base for practice interventions is growing, it is still weak for most of the strategies currently recommended to improve medication safety. System-focused strategies include increasing nurse staffing levels, otherwise decreasing workloads, improving the safety climate, and instituting policy and procedures such as RN independent double-checks. There are few research studies describing nurses’ perceptions of the impact of these system features and even fewer assessing the actual impact, and none that have implemented and rigorously evaluated the effects of system strategies. Instituting new technological systems is most highly recommended. Given the emphasis, there have been surprisingly few studies actually assessing the impact on error rates of bar-coded medication administration and other medication safety technologies.
Process-focused factors include minimizing distractions and interruptions during medication administration, using equipment correctly, and assessing and monitoring the patients’ responses to the medications. Again, a few small, single-site studies have assessed the effects of implementing protocols addressing these issues; but overall, the evidence is weak.
The human factors of knowledge and skills (e.g., mathematical) have been studied for decades, and changes in basic education and nurses’ orientation and continuing education have been instituted. Studies linking these strategies to outcomes such as the rate of medication errors have not been completed. The impact of fatigue on MAEs is currently of great interest. But with only one descriptive study available and no interventions tested, it is difficult to know how to approach this issue.
Based on this review of the literature, it is clear that medication errors are an immense problem. When implementing interventions to improve medication safety, use the most reliable and valid data available, and share the results through publications to make the knowledge available to all.
- Research Implications
The implications for research follow directly on the discussion of practice implications. Research in this area is constrained by the need to carry out these projects “in the field.” Secondary analysis of existing data sets cannot be used for most of the pertinent questions in this area. Laboratory studies are equally impossible. The situations at the heart of medication safety are complex, multifaceted, and multidisciplinary; knowledge about them must be produced with studies conducted within that complex environment. This requires health care institutions to simultaneously attempt to implement changes that will reduce the problem and evaluate the impact. Essentially, this is quality improvement (QI) work.
The question is, should the results of QI projects be considered evidence and used as part of the knowledge foundation for future evidence-based practice projects? 142 QI is a set of activities intended to improve some aspect of health care processes, 143 a dynamic and changing package of interventions, 144 and identification of ways to implement effective change. 145 For the most part, definitions of QI do not include assessing the effectiveness of these activities or producing knowledge. And yet, reports of QI projects are increasingly used as evidence for practice and organizational change.
Health care institutions are responding to the crisis in quality and safety with frenetic activities designed to bring about improvement. They desperately want evidence that will assist them in knowing which of these activities to focus on. Massive amounts of money are being invested in organizational changes to improve quality and safety with mostly expert advice and hunches to go on. There is little doubt that these projects are well intentioned; many of them suggest changes that are intuitive or reflect common sense. To move beyond the current state of multiple projects targeting similar changes, the industry needs evidence of the effects of specific changes: the direct and indirect effects, the intended and unintended effects, and the cost effectiveness.
By their nature, QI efforts are local, attempt to minimize disruption to the organization, and try to constrain costs of implementation. To justify the organization’s investment in the project, there is a desire to show that the project had the intended effect. Further, the directors of the project often want to capitalize on the QI activities by reporting the results publicly, preferably through respected journals or presentations at professional meetings. As a result of these multiple goals, the project usually has only low-cost, superficial evaluation efforts that are then reported as evidence with an emphasis on outcomes supporting the intervention and omission of those that did not. Many current QI studies have significant bias and can cause harm by disseminating results that lead health care institutions to invest in activities that may not improve quality, while ignoring others that could. 146 But, there is no consensus on standards that can be applied to improve this situation. As Mosser and Kane 147 asked recently, What level of proof should we require to conclude that improvement has been achieved? What level of proof is there that the intervention was the cause of improvement?
The problem of bias inherent in local efforts to improve quality is crucial. When organizations make decisions to invest large amounts of money in a QI project, there is understandable reluctance to hear, let alone share, results that show no systematic effects on the outcomes of care. Yet, to produce the science required for future QI efforts, reports of activities that were ineffective and those that resulted in unintended and disruptive side effects must also be shared with others. Most QI activities cannot be tested with rigorous and controlled research, and we therefore need to develop a QI science to enhance the internal and external validity of the results. We cannot accept poorly conducted studies of efforts to improve quality and safety—it is too crucial to the future of health care. At the same time, we must recognize that the complexity of projects taking place in the real world cannot be simplified and that analytic methods must substitute for experimental controls in this work. 148 Both the practitioners’ distrust of research and its accompanying statistics and the researchers’ disdain of the messiness of QI activities must be tempered with a better understanding.
Despite concerns about the rigor of QI, it is crucial that these activities be reported to promote learning about implementation methods that worked and those that did not, and the types of projects that produced desired results and those that did not. To maximize learning, these reports must be thorough and include both the intended and unintended outcomes, descriptions of the intervention and implementation must be candid, the robustness of the measures must be clear, and the description of the organizational context must be adequate. Recent guidelines for the publication of QI projects may assist in achieving this thoroughness and transparency. 149 Collaboration between the principals involved in the QI project and health systems researchers would maximize the potential for producing evidence from these field studies. It is unlikely that science will ever develop methods to study implementation and evaluation of QI projects in their natural setting with a level of rigor similar to experiments or clinical trials, and that makes the results of QI projects even more valuable. It is crucial that we learn which QI activities work in which settings and which outcomes can most likely be improved with organizational changes.
The specific issues most in need of research (QI activities) at this time are as follows:
- Bar-coding and other medication safety technology—widely recommended but little or no valid research using before-and-after designs.
- Independent RN double-checks—logical and widely recommended, but no research has been done describing, let alone testing, the effects of this policy.
- Relationship between nurse staffing and medication errors—a few descriptive studies and studies asking RN perceptions of the problem suggest that staffing and workload are major factors, but there are no research studies using valid and reliable data.
- Techniques to reduce distractions, interruptions, other risk factors for medication error need to be tested.
- Methods of effective education in medication safety for nurses and all providers.
- Effectiveness of implementing new checklists, policies, and procedures.
- Understanding work-arounds.
- Methods and techniques for successful implementation of system and process change.
Despite the national emphasis on patient safety and quality care, very little is known about effective medication safety strategies for nurses. The recent IOM report on medication safety 2 identified several areas needing future research, including the following:
- What are the most effective mechanisms to improve communication between patients and clinicians regarding the safe use of medications?
- What are the most effective mechanisms to improve patient education about the safe use of medications?
- Which self-management support strategies are effective in improving patient outcomes?
- How can information about specific medications be effectively used by patients? What is the impact of that information on patients’ adherence and communication with clinicians?
- How can patient-centered approaches to medication safety decrease errors associated with medications and improve patient outcomes?
- How can medication-related competencies become a core competency among the current workforce?
- What is the impact of free samples on patient adherence and health outcomes?
There is a large and growing body of research addressing medication safety in health care. This literature covers the extent of the problem of medication errors and adverse drug events, the phases of the medication-use process vulnerable to error, and the threats all of this poses for patients. As this body of literature is evaluated, the fact that there are crucial areas about which we know little becomes apparent. Nurses are most involved at the medication administration phase, although they provide a vital function in detecting and preventing errors that occurred in the prescribing, transcribing, and dispensing stages. Administration errors comprise a significant proportion of all errors and yet, beyond that fact, there isn’t much known about the causes or about the effectiveness of proposed solutions. Research addressing the complex process of medication use in hospitals is badly needed and requires a new approach to produce valid knowledge from studies done in the field with few controls of confounding factors.
- Search Strategy
A search of the literature was conducted using PubMed ® and CINAL ® . The key words employed in the search included “adverse drug events,” “drug administration,” “medication administration,” “medication administration errors,” “medication error reporting,” “medication safety,” “nursing,” “patient safety,” and “work(ing) conditions.” This resulted in 1,400 abstracts, which were narrowed as follows. Literature that addressed topics covered in this book on health information technology, specifically computerized provider order entry with clinical decision-support systems (for nurses and/or physicians) and bar-code medication administration systems, children, and medication reconciliation were excluded from this review, as were studies with only physicians and pharmacists as study subjects, those in home health care settings, and those related only to prescribing medications or patient compliance. Additional exclusion criteria included research not differentiating the nursing role in medication administration, administration of medications to reverse adverse drug reactions (e.g., naloxone for opioid overdose), prescribing and dispensing process of medications, and unique specifications regarding specific medications. Reviewed articles were searched for references that we did not already have, and PubMed ® links were checked as additional articles were found. The final review also excluded editorials, newsletters, single-case studies, medication safety outside institutional settings (if dealing with patient self-management or adherence), and studies with critically flawed methodology and inadequate reporting. The literature was then also limited to reports written in English and research published in 1997 or later. A total of 70 articles were identified as having met the inclusion criteria as evidence and were discussed in this chapter.
- Cite this Page Hughes RG, Blegen MA. Medication Administration Safety. In: Hughes RG, editor. Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Rockville (MD): Agency for Healthcare Research and Quality (US); 2008 Apr. Chapter 37.
- PDF version of this page (350K)
In this Page
- Research Evidence—Medication Administration by Nurses
Other titles in this collection
- Advances in Patient Safety
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Review The extent of medication errors and adverse drug reactions throughout the patient journey in acute care in Australia. [Int J Evid Based Healthc. 2016] Review The extent of medication errors and adverse drug reactions throughout the patient journey in acute care in Australia. Roughead EE, Semple SJ, Rosenfeld E. Int J Evid Based Healthc. 2016 Sep; 14(3):113-22.
- Strategies to reduce medication errors with reference to older adults. [Int J Evid Based Healthc. 2006] Strategies to reduce medication errors with reference to older adults. Hodgkinson B, Koch S, Nay R, Nichols K. Int J Evid Based Healthc. 2006 Mar; 4(1):2-41.
- Review Electronically Generated Medication Administration and Electronic Medication Administration Records for the Prevention of Medication Transcription Errors: Review of Clinical Effectiveness and Safety [ 2016] Review Electronically Generated Medication Administration and Electronic Medication Administration Records for the Prevention of Medication Transcription Errors: Review of Clinical Effectiveness and Safety . 2016 Dec 8
- Incidence of adverse drug events and medication errors in intensive care units: a prospective multicenter study. [J Patient Saf. 2009] Incidence of adverse drug events and medication errors in intensive care units: a prospective multicenter study. Benkirane RR, Abouqal R, Haimeur CC, S Ech Cherif El Kettani SS, Azzouzi AA, Mdaghri Alaoui AA, Thimou AA, Nejmi MM, Maazouzi WW, Madani NN, et al. J Patient Saf. 2009 Mar; 5(1):16-22.
- Identification of prescribing errors by pre-registration student nurses: a cross-sectional observational study utilising a prescription medication quiz. [Nurse Educ Today. 2014] Identification of prescribing errors by pre-registration student nurses: a cross-sectional observational study utilising a prescription medication quiz. Whitehair L, Provost S, Hurley J. Nurse Educ Today. 2014 Feb; 34(2):225-32. Epub 2013 Jan 30.
Recent Activity
- Medication Administration Safety - Patient Safety and Quality Medication Administration Safety - Patient Safety and Quality
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
- Fact sheets
- Facts in pictures
- Publications
- Questions and answers
- Tools and toolkits
- Endometriosis
- Excessive heat
- Mental disorders
- Polycystic ovary syndrome
- All countries
- Eastern Mediterranean
- South-East Asia
- Western Pacific
- Data by country
- Country presence
- Country strengthening
- Country cooperation strategies
- News releases
- Feature stories
- Press conferences
- Commentaries
- Photo library
- Afghanistan
- Cholera
- Coronavirus disease (COVID-19)
- Greater Horn of Africa
- Israel and occupied Palestinian territory
- Disease Outbreak News
- Situation reports
- Weekly Epidemiological Record
- Surveillance
- Health emergency appeal
- International Health Regulations
- Independent Oversight and Advisory Committee
- Classifications
- Data collections
- Global Health Estimates
- Mortality Database
- Sustainable Development Goals
- Health Inequality Monitor
- Global Progress
- World Health Statistics
- Partnerships
- Committees and advisory groups
- Collaborating centres
- Technical teams
- Organizational structure
- Initiatives
- General Programme of Work
- WHO Academy
- Investment in WHO
- WHO Foundation
- External audit
- Financial statements
- Internal audit and investigations
- Programme Budget
- Results reports
- Governing bodies
- World Health Assembly
- Executive Board
- Member States Portal
- Publications /
5 moments for medication safety: Infographics

The 5 Moments for Medication Safety patient engagement tool focuses on 5 key moments where action by the patient or caregiver can reduce the risk of harm associated with the use of medication/s. This tool aims to engage and empower patients to be involved in their own care. It should be used in collaboration with health professionals, but should always remain with the patients, their families or caregivers.

Taysha Gene Therapies Announces Poster Presentation on TSHA-102 in Rett Syndrome at Upcoming British Paediatric Neurology Association 2024 Annual Conference
Taysha gene therapies, inc. today announced that it will present clinical data on its tsha-102 program in evaluation for rett syndrome during an oral poster presentation at the upcoming british paediatric neurology association (bpna) 2024 annual conference..
DALLAS, Jan. 22, 2024 (GLOBE NEWSWIRE) -- Taysha Gene Therapies , Inc. (Nasdaq: TSHA), a clinical-stage gene therapy company focused on developing and commercializing AAV-based gene therapies for the treatment of monogenic diseases of the central nervous system (CNS), today announced that it will present clinical data on its TSHA-102 program in evaluation for Rett syndrome during an oral poster presentation at the upcoming British Paediatric Neurology Association (BPNA) 2024 Annual Conference, taking place in Bristol, England from January 24-26, 2024.
The presentation will include previously disclosed clinical data from the first two adult patients with stage four Rett syndrome dosed with TSHA-102 in the REVEAL Phase 1/2 adolescent and adult trial in Canada. The Company expects to provide further updates on available clinical data from cohort one (low dose) in the REVEAL adolescent and adult trial in the first quarter of 2024.
Oral poster presentation details are as follows:
Abstract Title: Early safety and efficacy observations following the first use of TSHA-102 gene therapy in patients with Rett Syndrome
Presenter: Meredith Schultz, M.D., M.S., Senior Vice President of Clinical Development and Medical Affairs at Taysha Gene Therapies
Oral Presentation Session Date/Time: Thursday, January 25 at 12:05-12:40 PM GMT
Location: Screen C - Wallace Suite
Poster Number: 056
Additional details on the meeting can be found at the BPNA 2024 Annual Congress website .
About TSHA-102 TSHA-102 is a self-complementary intrathecally delivered AAV9 investigational gene transfer therapy in clinical evaluation for Rett syndrome. TSHA-102 utilizes a novel miRNA-Responsive Auto-Regulatory Element (miRARE) technology designed to mediate levels of MECP2 in the CNS on a cell-by-cell basis without risk of overexpression. TSHA-102 has received Fast Track designation and Orphan Drug and Rare Pediatric Disease designations from the FDA and has been granted Orphan Drug designation from the European Commission.
About Rett Syndrome Rett syndrome is a rare neurodevelopmental disorder caused by mutations in the X-linked MECP2 gene, which is a gene that’s essential for neuronal and synaptic function in the brain. The disorder is characterized by intellectual disabilities, loss of communication, seizures, slowing and/or regression of development, motor and respiratory impairment, and shortened life expectancy. Rett syndrome primarily occurs in females and is one of the most common genetic causes of severe intellectual disability. Currently, there are no approved disease-modifying therapies that treat the genetic root cause of the disease. Rett syndrome caused by a pathogenic/likely pathogenic MECP2 mutation is estimated to affect between 15,000 and 20,000 patients in the U.S., EU and U.K.
About Taysha Gene Therapies Taysha Gene Therapies (Nasdaq: TSHA) is on a mission to eradicate monogenic CNS disease. With a singular focus on developing curative medicines, we aim to rapidly translate our treatments from bench to bedside. We have combined our team’s proven experience in gene therapy drug development and commercialization with the world-class UT Southwestern Gene Therapy Program. Together, we leverage our fully integrated platform with a goal of dramatically improving patients’ lives. More information is available at www.tayshagtx.com .
Company Contact: Hayleigh Collins Director, Head of Corporate Communications and Investor Relations Taysha Gene Therapies, Inc. [email protected]
Media Contact: Carolyn Hawley Canale Communications [email protected]

IMAGES
VIDEO
COMMENTS
Acknowledge that medication safety is a topic and an understanding of the area will affect how you perform the following tasks: Use generic names where appropriate. Tailor your prescribing for each patient. Learn and practise thorough medication history taking. Know which medications are high-risk and take precautions.
Resources to support medication safety. Resources to support medication safety. Skip directly to site content Skip directly to search. ... 8.5"x14" Spoons are for Soup poster. Feb. 7, 2024. Soups Are For Soup Poster. 11"x17" Spoons are for Soup poster. Feb. 7, 2024. Images. Spoons Are For Soup Button 285.
1 Basics of Medication Safety. This is a sample PowerPoint from "Learn to be Safe - Medication Safety. A Guide for Pharmacists". It is for conducting a presentation on medication safety to the public - your patients and families. To prepare for presentations, review the purpose of the guide, how to use the guide, key topics and messages ...
The 5 Moments for Medication Safety is a patient engagement tool developed to support the implementation of the third WHO Global Patient Safety Challenge: Medication Without Harm. The tool focuses on 5 key moments where action by the patient or caregiver can reduce the risk of harm associated with the use of medication/s. This tool aims to ...
Medication safety poster. Summary. This poster, published by the World Health Organization (WHO) in 2017, summarises in a visual way the '5 Moments for Medication Safety', which are the key moments where action by the patient or caregiver can greatly reduce the risk of harm associated with the use of their medication/s.
Discover a valuable resource on this website that focuses on safe storage and disposal of medications. Access a comprehensive poster that provides essential guidelines for keeping medications secure and out of reach of children, as well as proper disposal methods to prevent misuse and environmental harm. Learn about the importance of medication safety and how to promote responsible medication ...
Activity 1: "Medication Safety for Teens" Presentation . An interactive PowerPoint presentation that teaches teens how to safely use medication. "Medication Safety for Teens" Activity ... or posters, wallpaper or stickers; relevant posts from NIDA's Sara Bellum Blog; and fact sheets. ...
The 5 Moments for Medication Safety patient engagement tool focuses on 5 key moments where action by the patient or caregiver can reduce the risk of harm associated with the use of medication/s. This tool aims to engage and empower patients to be involved in their own care. It should be used in collaboration with health professionals, but ...
ion Without Harm.It is intended to engage patients in their own care in a more active way, to encourage their curiosity about the medications they are taking, and to empower them to communicate openly with their hea. th professionals.This tool is intended for use by patients, their families and caregivers, with the help of health professionals ...
This poster comes in nine languages and conveys four key medication safety messages: Keep medication up high, out of reach of children. Talk to your doctor before giving medication to your child. Only use the measuring tool that came with your child's medication. Keep the poison center number in your phone: 1-800-222-1222.
Medicines are safe when used as prescribed or as directed on the label. There are risks in taking any medicine, vitamin or other supplement. An adverse drug event (ADE) is when a medication causes harm to someone. ADEs include allergic reactions, side effects, overmedication and medication errors.
Posters are developed in collaboration with the Medication Safety Network and provide to hospitals by WA Health. Below are the posters that have been printed for previous years. Clinician focused posters. Acceptable prescribing terms and abbreviations- lanyard card (PDF 186KB) Acceptable prescribing terms and abbreviations - poster (PDF 874KB)
Medication Safety. Medication Safety. The Good Hospital Practice Training Series 2009 The Medical City. In this presentation…. The roles of the Medical City staff in ensuring the safe use of medications Prescription writing Verbal and phone orders High risk medication monitoring Medication reconciliation. 6.29k views • 43 slides
Rotation Desscription. The medicattion safety rrotation willl help studen nts become familiar wiith the key p principles uttilized in h ospitals and d health systtems to imprrove medica ation safety. The rotatio on is designe ed to expose e students t o medicatio on safety no omenclature, , key princiiples, tools and availab ble resources s.
A recent Australian study reported that interruptions occurred in 53% of medication administrations and that the risk and severity of medication errors double when the number of interruptions increasing from 0 to 4. This video can be used to highlight the issues associated with medication interruptions and how to prevent and manage them.
Department of Pharmacy , R. P. Shaha University , Narayanganj-1400, Bangladesh. [email protected] ; Mobile - 01845510817. Abstract : Medication safety is a critical component of ...
Use of posters. The posters group labels according to intended route of administration and are available in PDF and Word formats. They may be altered to reflect the mix of labels needed in specific clinical areas. Poster resources. Posters are available for the following routes.
There is a large and growing body of research addressing medication safety in health care. This literature covers the extent of the problem of medication errors and adverse drug events, the phases of the medication-use process vulnerable to error, and the threats all of this poses for patients. As this body of literature is evaluated, the fact that there are crucial areas about which we know ...
Medication Safety. Nine out of every 10 poisonings for children ages 12 and younger involve medication errors or unsupervised children taking medicine on their own. With nearly all of these incidents occurring in the home, storing, using, and disposing of over-the-counter and prescription medication is an essential safety check for every parent.
The 5 Moments for Medication Safety patient engagement tool focuses on 5 key moments where action by the patient or caregiver can reduce the risk of harm associated with the use of medication/s. This tool aims to engage and empower patients to be involved in their own care. It should be used in collaboration with health professionals, but ...
Oral poster presentation details are as follows: Abstract Title: Early safety and efficacy observations following the first use of TSHA-102 gene therapy in patients with Rett Syndrome Presenter: Meredith Schultz, M.D., M.S., Senior Vice President of Clinical Development and Medical Affairs at Taysha Gene Therapies
Registration is now open for the 32nd Annual Nutrient Management Conference, hosted by CDFA's Fertilizer Research and Education Program (FREP) and Western Plant Health (WPH).This year's conference will be held October 29-30 at the Embassy Suites by Hilton Monterey Bay, Seaside, CA, and includes a pre-conference tour of McFadden Woodchip Bioreactor in Salinas 2-4 p.m. October 28.