
- Upload Ppt Presentation
- Upload Pdf Presentation
- Upload Infographics
- User Presentation
- Related Presentations


Cardiac MRI
By: drdwayn Views: 3856

Basic life support
By: drdwayn Views: 2178

General Pharmacodynamics
By: drdwayn Views: 1431

Cardiac catheters
By: drdwayn Views: 1826

Physiotherapy
By: drdwayn Views: 1340

By: manouchfada Views: 1939

Impact of Covid-19
By: sdgsgsgsd Views: 1200

Kojic Acid Esters As Skin Whitening Agents
By: asadasfassdd Views: 2077

Allergy An Introduction
By: KhushbuSG Views: 4739

All About Allergies
By: sherry Views: 4907

- About : I am Dr. Dwayne Faulk
- Occupation : Medical Professional
- Specialty : Other Health Professionals
- Country : United States of America
HEALTH A TO Z
- Eye Disease
- Heart Attack
- Medications

- My presentations
Auth with social network:
Download presentation
We think you have liked this presentation. If you wish to download it, please recommend it to your friends in any social system. Share buttons are a little bit lower. Thank you!
Presentation is loading. Please wait.
NURSING MANAGEMENT OF COPD. Physiology Respiratory System Upper Tract & Lower Tract Goal is to transfer oxygen and carbon dioxide.
Published by Phillip Welch Modified over 8 years ago
Similar presentations
Presentation on theme: "NURSING MANAGEMENT OF COPD. Physiology Respiratory System Upper Tract & Lower Tract Goal is to transfer oxygen and carbon dioxide."— Presentation transcript:

Arterial Blood Gases Reflect oxygenation, gas exchange, and acid-base balance PaO2 is the partial pressure of oxygen dissolved in arterial blood SaO2 is.
Pre-Hospital Treatment Using the Respironics Whisperflow
Michael W. Nash, MD Family Medicine Clinton County Rural Health Clinic Understanding COPD.
OXYGENATION Normal respiratory functioning depends on: The ability of the airway system A properly functioning alveolar system A properly functioning.
Prehospital Treatment of Dyspnea with CPAP Mark Marchetta, BS, RN, NREMT-P Director, EMS Education Aultman Health Foundation Canton, Ohio.

Chronic obstructive pulmonary disease (COPD) Dr. Walaa Nasr Lecturer of Adult Nursing Second year.
Copyright © 2010 Delmar, Cengage Learning. ALL RIGHTS RESERVED. Chapter 13 Resistance-Training Strategies for Individuals with Chronic Obstructive Pulmonary.
ABG Interpretation.
Copyright 2003 by Mosby, Inc. All rights reserved. CHAPTER 12 RESPIRATORY SYSTEM.
Dr. Maha Al-Sedik. Why do we study respiratory emergency? Respiratory Calls are some of the most Common calls you will see. Respiratory care is.
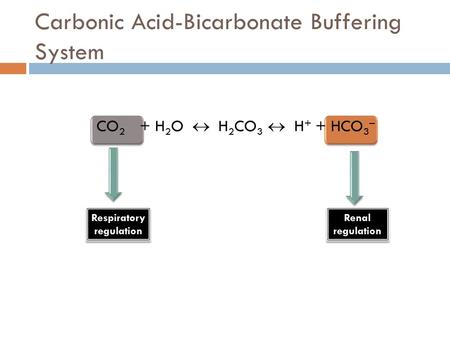
Carbonic Acid-Bicarbonate Buffering System CO 2 + H 2 O H 2 CO 3 H + + HCO 3 – Respiratory regulation Respiratory regulation Renal regulation Renal.
Respiratory Failure 215a.
Chronic Obstructive Pulmonary Disease
Management of Patients With Chronic Pulmonary Disease.
Pathophysiology of Respiratory Failure Fern White & Annabel Fothergill.
Copyright © 2007, 2004, 2000, Mosby, Inc., an affiliate of Elsevier Inc. All Rights Reserved. Focus on Respiratory Failure (Relates to Chapter 68, “Nursing.
Respiratory System.
Arterial blood gas By Maha Subih.
Diseases of the Lower Respiratory System Nursing II Valencia Community College.
Essentials of Anatomy and Physiology Fifth edition Seeley, Stephens and Tate Slide 2.1 Copyright © 2003 Pearson Education, Inc. publishing as Benjamin.
About project
© 2024 SlidePlayer.com Inc. All rights reserved.
It seems you are using an outdated browser. Please upgrade to a modern browser to improve your experience on this website.
COPD Foundation Educational Materials
Thank you for your interest in the copd foundation’s educational library. we have a variety of useful booklets, flyers, and tools to help you learn more about living and thriving with copd – everything from the basics of lung conditions to specific topics such as exercise and exacerbations (flare-ups)., the following are available to download to your computer, tablet, or smartphone. hard copies are available to purchase through our online store ., if you are a health care professional, would you please take a minute to register for our copd360social community, guides for better living, the basics of copd, copd 101/201, all about bronchiectasis, oxygen therapy basics.
- COPD Pocket Consultant Guide
Disaster Preparedness Plan (DPP)
Covid-19 defenses: what you need to know, the impact of smoking, my copd action plan, tips for living well with copd, staying healthy and avoiding pneumonia, staying safe with copd: protecting against shingles, medication and immunization wallet card.
Back to Top
The NEW! COPD Foundation Guides for Better Living are comprehensive educational booklets for use by individuals with COPD and their families, pulmonary rehabilitation programs, COPD support groups, and health care facilities. Each of the nine Guides for Better Living focuses on one important aspect of life with COPD. Many in this series of 12- to 20-page easy-to-read booklets feature interactive portions for patients and caregivers to discuss together. The Guides are available for purchase individually or in a set in our online catalogue.
English plus

Click to View All Languages plus
COPD 101: Understanding the Basics of COPD, covers introductory information about COPD and includes a screening tool and symptom tracker.
COPD 201: Beyond the Basics, will be of particular interest to those looking for more advanced information and covers topics such as medication, treatments, smoking cessation, nutrition, and co-existing conditions. It also includes a copy of My COPD Action Plan.
All About Bronchiectasis contains helpful information for people with bronchiectasis. This booklet covers many important topics, such as how bronchiectasis is diagnosed, treatment options, tips for living well and reducing exacerbations, and how to find support for living with bronchiectasis. This booklet may also be beneficial to caregivers as well.
All About Bronchiectasis plus
Oxygen Therapy Basics is intended to support individuals who are new to (or curious about) supplemental oxygen therapy. This guide covers the goals of oxygen therapy, oxygen equipment, safety, travel, and more.
Oxygen Therapy Basics plus
Copd pocket consultant guide (pcg).
The app. The COPD Pocket Consultant Guide (PCG) app is built to support patients with COPD and their family members in self-management and to assist health care professionals in providing optimal care. The patient and caregiver track contains several helpful tools, including an interactive My COPD Action Plan and activity tracking calendar; inhaler, nebulizer and exercise videos; and a wallet card to track important information such as medications and immunizations. In the health care provider view, users can access the CAT and mMRC Breathlessness Scale; an evidence-based therapy flowchart; COPD medications lists; inhaler and nebulizer education videos; and much more. To download the free app, please visit the App Store or Google Play . You can read more about the PCG tracks for patients and caregivers and for health care professionals .
The tri-fold card. For health care professionals, hard copies of the COPD Pocket Consultant Guide, including the treatment decision tree, seven COPD severity domains, the CAT, the mMRC Breathlessness Scale, and listings of brand or generic medications are available for download below. In addition, laminated versions are available through our online catalogue .
The COPD Pocket Consultant Guide was supported by Astra Zeneca and GSK.
COPD Pocket Consultant Guide plus
The COPD Foundation Disaster Preparedness Plan (DPP) is a comprehensive resource for individuals and families impacted by chronic lung diseases, including COPD. This booklet will help you plan for emergencies and stay safe during a disaster event. You’ll also find an interactive removable insert containing helpful forms, lists, and charts for making a disaster preparedness plan that is specific to your own needs. The DPP can also be found in the COPD Pocket Consultant Guide (PCG) app, available on the Apple App Store or Google Play .

Español (Spanish) plus
Testing positive for COVID-19 can be scary and overwhelming, and people with COPD are at higher risk for severe symptoms. While you should always discuss treatments with your health care provider, this poster covers currently-approved treatment options.
COVID-19 Defenses: What You Need to Know plus
This flyer highlights the benefits and importance of quitting smoking at any age. Learn about tools to help you quit smoking as well as risk factors for COPD in this double-sided flyer.
It can be very helpful to have an action plan to follow when managing your COPD. This plan guides you when you’re feeling well and when an exacerbation (flare-up) is starting. The COPD Foundation's My COPD Action Plan should be filled out the first time as part of a discussion with your health care provider, and then used daily or as often as you can. Remember to update it at least every six months. Download your copy here or use the interactive My COPD Action Plan in the COPD Pocket Consultant Guide (PCG) app (free for download in the App Store and Google Play ).
When you visit your doctor, complete the activity list before you arrive for the appointment. This will help them understand your current activities and limitations. It is also important to bring a complete list of the medications you are currently taking (you can write these down or enter them into the Wallet Card in the PCG app). Ask your doctor to help you complete the special medications section of your My COPD Action Plan for Yellow days and Red days.
The Report Early Warning Signs of Exacerbation is another great tool that you should have. Be sure to share both with your family and caregivers so everyone knows what to do and who to call when you are having a COPD flare-up.
It’s important for individuals with COPD to stay healthy and enjoy their favorite activities. In the Tips for Living Well with COPD flyer, you will learn about tools, techniques, and resources to help you on your journey with COPD. You will also learn useful health and safety tips for managing your COPD.
Tips for Living Well with COPD plus
This one-page fact sheet focuses on preventing pneumonia in individuals with COPD. This flyer will give you helpful tips and tools for staying healthy, avoiding illness, and recognizing early warning signs of an infection or flare-up.
Staying Healthy and Avoiding Pneumonia plus
This one-page flyer focuses on preventing the symptoms and complications of shingles for people with COPD. While discussing treatment options with your health care provider is important, this flyer can help you make well-informed choices about the best available care.
Staying Safe with COPD: Protecting Against Shingles plus
It is important to keep a list of your medications and immunizations handy. Fill out this wallet card and carry it with you. Be sure to update it periodically.
For details on copyrights and use of COPD Foundation content, please see our Disclaimer .
Questions contact us at [email protected] ., join us on copd360social.
Join the Conversation
Already a Member?
This page was reviewed on May 14, 2024 by the COPD Foundation Content Review and Evaluation Committee .
- Management and Treatment of COPD
There is no cure for COPD, however, lifestyle changes and treatments can help you feel better, stay more active, and slow disease progression.
The goals of COPD treatment are to relieve symptoms, slow the progression of disease, improve exercise tolerance, prevent and manage complications such as “flare-ups”, and improve overall health.
Patients should become informed about COPD by speaking with their doctor. Sometimes a referral to a pulmonologist, or lung doctor, may be required. Patients who are informed about their COPD are likely to have better health outcomes.
Lifestyle changes are important. Quitting smoking is vitally important, and your doctor and support groups can help you quit. COPD risk increases with smoking, and ranges from 35% to as high as 50%.
Avoiding second hand smoke and other lung irritants like air pollution (dust and chemical fumes) is also very important.
Getting regular exercise may also greatly benefit persons with COPD.
Medical treatment of COPD may consist of inhaled medications and oral medications.
The most important medicines used to treat COPD include inhaled bronchodilators, which patients breathe in to the lungs to open up (or dilate) the airways (or bronchi); thus these medicines are called bronchodilators.
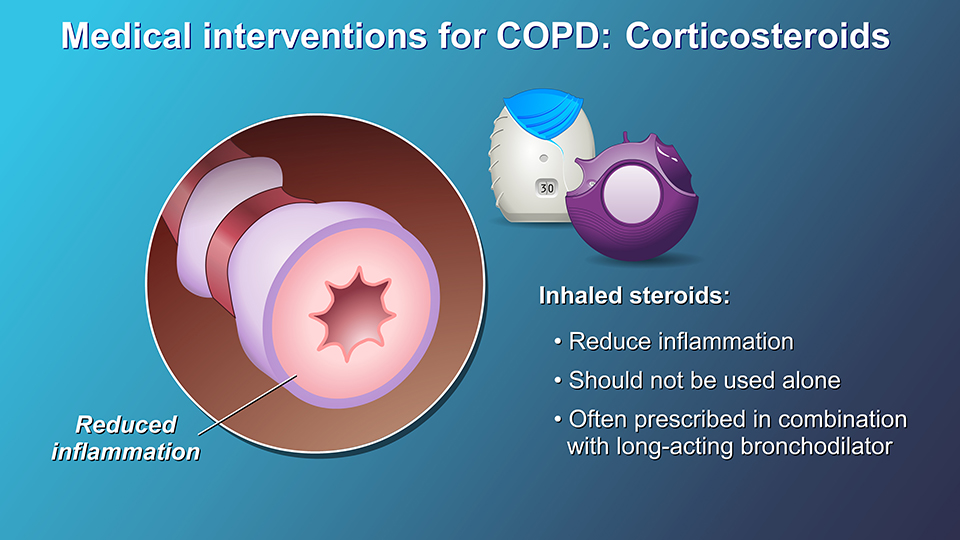
Other medicines can be used with the bronchodilators in special situations and include inhaled corticosteroids, oral methylxanthines (such as theophylline), or oral phosphodiesterase-4 inhibitors.
Inhaled corticosteroids are also used for the treatment of COPD. Inhaled steroids may help to reduce inflammation in the lungs. If your COPD becomes more severe, or if your symptoms flare up often, your doctor may prescribe a combination of a bronchodilator and an inhaled steroid.
Inhaled steroids should not be used alone, without also using a long-acting bronchodilator for COPD. Your doctor may want you to try this combination to see whether the addition of an inhaled steroid to a long-acting bronchodilator helps to relieve your symptoms and/or reduces your chances of having flare-ups (or exacerbations of COPD).
Another medical treatment for COPD is a class of drugs known as phosphodiesterase-4 inhibitors (or PDE-4 inhibitors).
If you don’t have relief of symptoms, or if your COPD exacerbations continue, your doctor may decide to prescribe a PDE-4 inhibitor to lower your chances of having more COPD exacerbations and improve your quality of life.
Antibiotics are also used to control bacterial lung infections in COPD, especially during acute flare-ups. These drugs treat sudden infections that may arise from time to time in the course of COPD.
Oral corticosteroids should only be used during acute flare-ups, or acute exacerbations of COPD, and should not be used on a routine basis. These medicines, when used during an acute exacerbation of COPD, help you get over the flare-up faster, reduce your chance of relapsing, and lower your chance of having to be admitted to the hospital.
Pulmonary rehabilitation is recommended for most people with COPD.
Rehabilitation may include an exercise program, disease management training, as well as nutritional and psychological counselling.
The goal is to help persons with COPD to stay healthy, carry on with daily activities, follow healthy eating habits, sleep well, and better manage exacerbations of their illness.
In rare cases, surgical intervention may be recommended for persons with COPD who have severe symptoms that have not improved with medical therapy.
Lung-volume reduction (or LVR ) surgery is the removal of damaged tissue from the lungs, helping to improve breathing and quality of life, but only helps a few, select people with COPD.
Lung transplantation involves replacing a damaged lung with a healthy lung from a donor. This surgery can improve your lung function and quality of life, but has many risks such as infections or rejection of the transplanted lung. Your doctor can discuss the benefits and risks of this surgical option with you.
Slide Show - Management and Treatment of COPD
- Share with family and friends:
Click here to take our SURVEY Your feedback is important to us! We will use your feedback to develop future areas of content about COPD which will help other patients, caregivers, and families.
Other Modules:
Understanding COPD
Diagnosis and Evaluation of COPD
Jointly provided by the Annenberg Center for Health Sciences at Eisenhower and Prime Medic Inc., in collaboration with Postgraduate Institute for Medicine and Mechanisms in Medicine Inc.
This activity is supported by an educational grant from Boehringer Ingelheim
This website is part of the Animated Patient ™ series developed by Mechanisms in Medicine Inc., to provide highly visual formats of learning for patients to improve their understanding, make informed decisions, and partner with their healthcare professionals for optimal outcomes.
- Terms of Use
- Technical Requirements
- © Mechanisms in Medicine Inc.
Chronic Obstructive Pulmonary Disease (COPD)
Learn about the nursing care management of patients with chronic obstructive pulmonary disease in this study guide .
Table of Contents
- What is Chronic Obstructive Pulmonary Disease?
Chronic Bronchitis
Pathophysiology, epidemiology, clinical manifestations, complications, assessment and diagnostic findings, pharmacologic therapy, management of exacerbations, surgical management, nursing assessment, planning & goals, nursing priorities, nursing interventions, discharge and home care guidelines, documentation guidelines, what is chronic obstructive pulmonary disease.
Nurses care for patients with COPD across the spectrum of care, from outpatient to home care to emergency department, critical care, and hospice settings.
- Chronic Obstructive Pulmonary Disease (COPD) is a condition of chronic dyspnea with expiratory airflow limitation that does not significantly fluctuate.
- Chronic Obstructive Pulmonary Disease has been defined by The Global Initiative for Chronic Obstructive Lung Disease as “a preventable and treatable disease with some significant extrapulmonary effects that may contribute to the severity in individual patients.”
- This updated definition is a broad description of COPD and its signs and symptoms.
Classification
There are two classifications of COPD: chronic bronchitis and emphysema. These two types of COPD can be sometimes confusing because there are patients who have overlapping signs and symptoms of these two distinct disease processes.
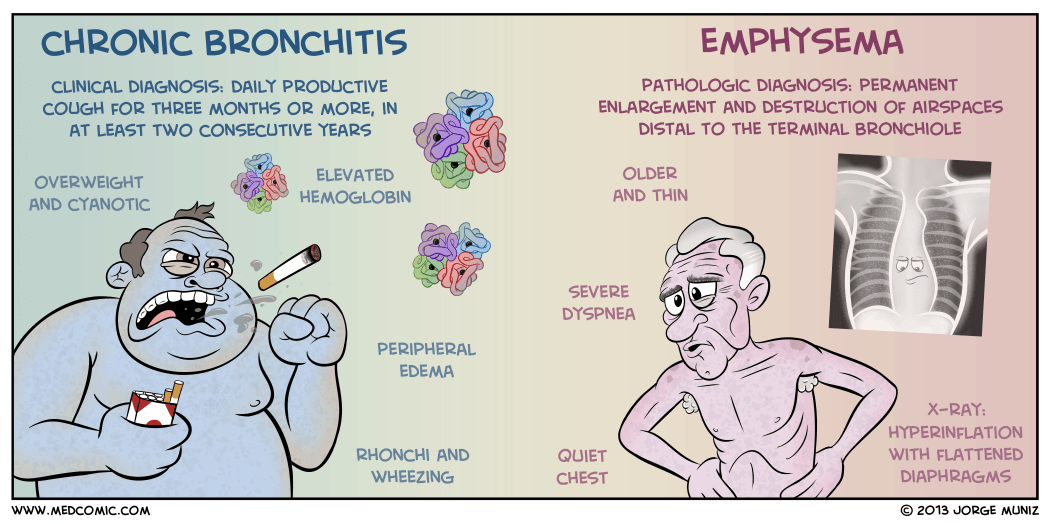
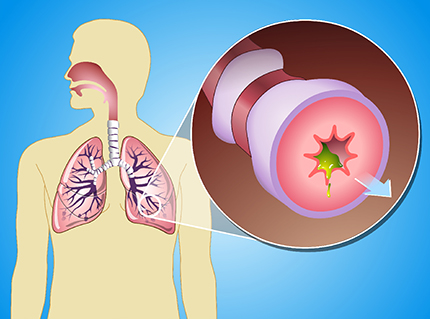
- Chronic bronchitis is a disease of the airways and is defined as the presence of cough and sputum production for at least 3 months in each of 2 consecutive years .
- Chronic bronchitis is also termed as “blue bloaters” .
- Pollutants or allergens irritate the airways and leads to the production of sputum by the mucus-secreting glands and goblet cells.
- A wide range of viral, bacterial, and mycoplasmal infections can produce acute episodes of bronchitis.
- Pulmonary Emphysema is a pathologic term that describes an abnormal distention of airspaces beyond the terminal bronchioles and destruction of the walls of the alveoli.
- People with emphysema are also called “pink puffers”.
- There is impaired carbon dioxide and oxygen exchange, and the exchange results from the destruction of the walls of overdistended alveoli.
- In panlobular , there is destruction of the respiratory bronchiole, alveolar duct, and alveolus.
- All spaces in the lobule are enlarged.
- In centrilobular , pathologic changes occur mainly in the center of the secondary lobule.
In COPD, the airflow limitation is both progressive and associated with an abnormal inflammatory response of the lungs to noxious gases or particles.
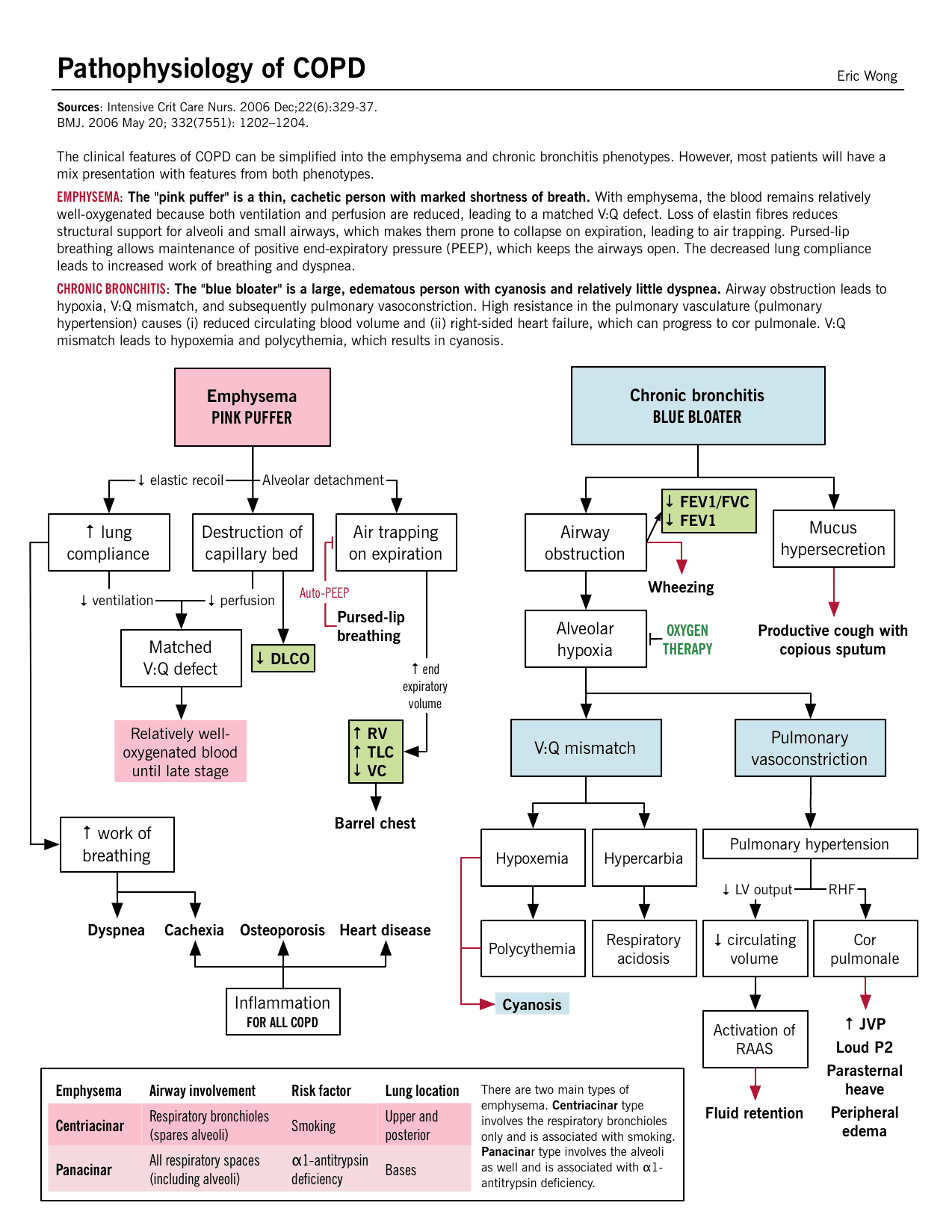
- An inflammatory response occurs throughout the proximal and peripheral airways, lung parenchyma, and pulmonary vasculature.
- Due to the chronic inflammation, changes and narrowing occur in the airways.
- There is an increase in the number of goblet cells and enlarged submucosal glands leading to hypersecretion of mucus.
- Scar formation. This can cause scar formation in the long term and narrowing of the airway lumen.
- Wall destruction . Alveolar wall destruction leads to loss of alveolar attachments and a decrease in elastic recoil.
- The chronic inflammatory process affects the pulmonary vasculature and causes thickening of the vessel lining and hypertrophy of smooth muscle .
Mortality for COPD has been increasing ever since while other diseases have decreasing mortalities.
- COPD is the fourth leading cause of death in the United States.
- COPD also account for the death of 125, 000 Americans every year.
- Mortality from COPD among women has increased, and in 2005, more women than men died of COPD.
- Approximately 12 million Americans live with a diagnosis of COPD.
- An additional 2 million may have COPD but remain undiagnosed.
- The annual cost of COPD is approximately $42.6 billion with overall healthcare expenditures of $26.7 billion.
Causes of COPD includes environmental factors and host factors. These includes:
- Smoking depresses the activity of scavenger cells and affects the respiratory tract’s ciliary cleansing mechanism.
- Occupational exposure. Prolonged and intense exposure to occupational dust and chemicals, indoor air pollution, and outdoor air pollution all contribute to the development of COPD.
- Genetic abnormalities . The well-documented genetic risk factor is a deficiency of alpha1- antitrypsin, an enzyme inhibitor that protects the lung parenchyma from injury .
The natural history of COPD is variable but is a generally progressive disease.
- Chronic cough . Chronic cough is one of the primary symptoms of COPD.
- Sputum production . There is a hyperstimulation of the goblet cells and the mucus-secreting gland leading to overproduction of sputum.
- Dyspnea on exertion . Dyspnea is usually progressive, persistent, and worsens with exercise.
- Dyspnea at rest . As COPD progress, dyspnea at rest may occur.
- Weight loss . Dyspnea interferes with eating and the work of breathing is energy depleting.
- Barrel chest . In patients with emphysema, barrel chest thorax configuration results from a more fixed position of the ribs in the inspiratory position and from loss of elasticity.
Prevention of COPD is never impossible. Discipline and consistency are the keys to achieving freedom from chronic pulmonary diseases.
- Smoking cessation . This is the single most cost-effective intervention to reduce the risk of developing COPD and to stop its progression.
- Healthcare providers should promote cessation by explaining the risks of smoking and personalizing the “at-risk” message to the patient.
There are two major life-threatening complications of COPD: respiratory insufficiency and failure.
- Respiratory failure . The acuity and the onset of respiratory failure depend on baseline pulmonary function, pulse oximetry or arterial blood gas values, comorbid conditions, and the severity of other complications of COPD.
- Respiratory insufficiency . This can be acute or chronic, and may necessitate ventilator support until other acute complications can be treated.
Diagnosis and assessment of COPD must be done carefully since the three main symptoms are common among chronic pulmonary disorders.
- Health history . The nurse should obtain a thorough health history from patients with known or potential COPD.
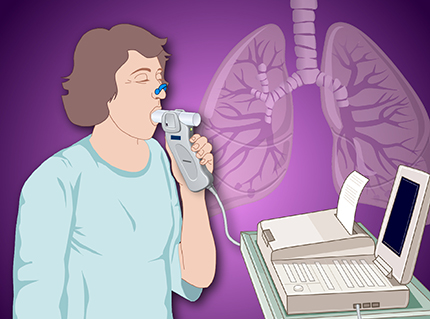
- Pulmonary function studies . Pulmonary function studies are used to help confirm the diagnosis of COPD, determine disease severity, and monitor disease progression.
- Spirometry . Spirometry is used to evaluate airway obstruction , which is determined by the ratio of FEV1 to forced vital capacity.
- ABG . Arterial blood gas measurement is used to assess baseline oxygenation and gas exchange and is especially important in advanced COPD.
- Chest x-ray . A chest x-ray may be obtained to exclude alternative diagnoses.
- CT scan . Computed tomography chest scan may help in the differential diagnosis.
- Screening for alpha1-antitrypsin deficiency . Screening can be performed for patients younger than 45 years old and for those with a strong family history of COPD.
- Chest x-ray: May reveal hyperinflation of lungs, flattened diaphragm , increased retrosternal air space, decreased vascular markings/bullae (emphysema), increased bronchovascular markings (bronchitis), normal findings during periods of remission ( asthma ).
- Pulmonary function tests: Done to determine cause of dyspnea, whether functional abnormality is obstructive or restrictive, to estimate degree of dysfunction and to evaluate effects of therapy, e.g., bronchodilators . Exercise pulmonary function studies may also be done to evaluate activity tolerance in those with known pulmonary impairment/progression of disease.
- The forced expiratory volume over 1 second (FEV 1 ): Reduced FEV 1 not only is the standard way of assessing the clinical course and degree of reversibility in response to therapy, but also is an important predictor of prognosis.
- Total lung capacity (TLC), functional residual capacity (FRC), and residual volume (RV): May be increased, indicating air-trapping. In obstructive lung disease, the RV will make up the greater portion of the TLC.
- Arterial blood gases ( ABGs ): Determines degree and severity of disease process, e.g., most often Pao 2 is decreased, and Paco 2 is normal or increased in chronic bronchitis and emphysema , but is often decreased in asthma ; pH normal or acidotic, mild respiratory alkalosis secondary to hyperventilation (moderate emphysema or asthma ).
- D L CO test: Assesses diffusion in lungs. Carbon monoxide is used to measure gas diffusion across the alveocapillary membrane. Because carbon monoxide combines with hemoglobin 200 times more easily than oxygen, it easily affects the alveoli and small airways where gas exchange occurs. Emphysema is the only obstructive disease that causes diffusion dysfunction.
- Bronchogram: Can show cylindrical dilation of bronchi on inspiration; bronchial collapse on forced expiration ( emphysema ); enlarged mucous ducts (bronchitis).
- Lung scan: Perfusion/ ventilation studies may be done to differentiate between the various pulmonary diseases. COPD is characterized by a mismatch of perfusion and ventilation (i.e., areas of abnormal ventilation in area of perfusion defect).
- Complete blood count (CBC) and differential: Increased hemoglobin (advanced emphysema ), increased eosinophils (asthma).
- Blood chemistry: alpha 1 -antitrypsin is measured to verify deficiency and diagnosis of primary emphysema .
- Sputum culture: Determines presence of infection , identifies pathogen.
- Cytologic examination: Rules out underlying malignancy or allergic disorder.
- Electrocardiogram ( ECG ): Right axis deviation, peaked P waves (severe asthma); atrial dysrhythmias (bronchitis), tall, peaked P waves in leads II, III, AVF (bronchitis, emphysema ); vertical QRS axis (emphysema).
- Exercise ECG , stress test: Helps in assessing degree of pulmonary dysfunction, evaluating effectiveness of bronchodilator therapy, planning /evaluating exercise program.

Medical Management
Healthcare providers perform medical management by considering the assessment data first and matching the appropriate intervention to the existing manifestation.
- Bronchodilators . Bronchodilators relieve bronchospasm by altering the smooth muscle tone and reduce airway obstruction by allowing increased oxygen distribution throughout the lungs and improving alveolar ventilation.
- Corticosteroids . A short trial course of oral corticosteroids may be prescribed for patients to determine whether pulmonary function improves and symptoms decrease.
- Other medications . Other pharmacologic treatments that may be used in COPD include alpha1-antitrypsin augmentation therapy, antibiotic agents, mucolytic agents, antitussive agents, vasodilators , and narcotics .
- Optimization of bronchodilator medications is first-line therapy and involves identifying the best medications or combinations of medications taken on a regular schedule for a specific patient.
- Hospitalization . Indications for hospitalization for acute exacerbation of COPD include severe dyspnea that does not respond to initial therapy, confusion or lethargy , respiratory muscle fatigue , paradoxical chest wall movement , and peripheral edema .
- Oxygen therapy . Upon arrival of the patient in the emergency room, supplemental oxygen therapy is administered and rapid assessment is performed to determine if the exacerbation is life-threatening.
- Antibiotics . Antibiotics have been shown to be of some benefit to patients with increased dyspnea, increased sputum production, and increased sputum purulence.
Patients with COPD also have options for surgery to improve their condition.
- Bullectomy . Bullectomy is a surgical option for select patients with bullous emphysema and can help reduce dyspnea and improve lung function.
- Lung Volume Reduction Surgery . Lung volume reduction surgery is a palliative surgery in patients with homogenous disease or disease that is focused in one area and not widespread throughout the lungs.
- Lung Transplantation . Lung transplantation is a viable option for definitive surgical treatment of end-stage emphysema.
Nursing Management
Management of patients with COPD should be incorporated with teaching and improving the respiratory status of the patient. Learn about the nursing care management of patients with Chronic Obstructive Pulmonary Disease using the nursing process in this guide.
SEE ALSO: 8 Chronic Obstructive Pulmonary Disease (COPD) Nursing Care Plans for a comprehensive nursing care plan and management guide
Assessment of the respiratory system should be done rapidly yet accurately.
- Assess patient’s exposure to risk factors.
- Assess the patient’s past and present medical history .
- Assess the signs and symptoms of COPD and their severity.
- Assess the patient’s knowledge of the disease.
- Assess the patient’s vital signs.
- Assess breath sounds and pattern.
Diagnosis of COPD would mainly depend on the assessment data gathered by the healthcare team members.
- Impaired gas exchange due to chronic inhalation of toxins.
- Ineffective airway clearance related to bronchoconstriction, increased mucus production, ineffective cough, and other complications.
- Ineffective breathing pattern related to shortness of breath , mucus, bronchoconstriction, and airway irritants.
- Self-care deficit related to fatigue .
- Activity intolerance related to hypoxemia and ineffective breathing patterns.
Goals to achieve in patients with COPD include:
- Improvement in gas exchange.
- Achievement of airway clearance.
- Improvement in breathing pattern.
- Independence in self-care activities.
- Improvement in activity intolerance .
- Ventilation/ oxygenation adequate to meet self-care needs.
- Nutritional intake meeting caloric needs.
- Infection treated/prevented.
- Disease process/prognosis and therapeutic regimen understood.
- Plan in place to meet needs after discharge.
- Maintain airway patency .
- Assist with measures to facilitate gas exchange.
- Enhance nutritional intake.
- Prevent complications, slow progression of condition.
- Provide information about disease process/prognosis and treatment regimen.
Patient and family teaching is an important nursing intervention to enhance self-management in patients with any chronic pulmonary disorder.
To achieve airway clearance:
- The nurse must appropriately administer bronchodilators and corticosteroids and become alert for potential side effects.
- Direct or controlled coughing . The nurse instructs the patient in direct or controlled coughing, which is more effective and reduces fatigue associated with undirected forceful coughing.
To improve breathing pattern:
- Inspiratory muscle training . This may help improve the breathing pattern.
- Diaphragmatic breathing . Diaphragmatic breathing reduces respiratory rate, increases alveolar ventilation, and sometimes helps expel as much air as possible during expiration.
- Pursed lip breathing . Pursed lip breathing helps slow expiration, prevents collapse of small airways, and control the rate and depth of respiration.
To improve activity intolerance :
- Manage daily activities . Daily activities must be paced throughout the day and support devices can be also used to decrease energy expenditure.
- Exercise training . Exercise training can help strengthen muscles of the upper and lower extremities and improve exercise tolerance and endurance.
- Walking aids . Use of walking aids may be recommended to improve activity levels and ambulation .
To monitor and manage potential complications:
- Monitor cognitive changes . The nurse should monitor for cognitive changes such as personality and behavior changes and memory impairment .
- Monitor pulse oximetry values . Pulse oximetry values are used to assess the patient’s need for oxygen and administer supplemental oxygen as prescribed.
- Prevent infection . The nurse should encourage the patient to be immunized against influenza and S. pneumonia because the patient is prone to respiratory infection.
During evaluation , the effectiveness of the care plan would be measured if goals were achieved in the end and the patient:
- Identifies the hazards of cigarette smoking.
- Identifies resources for smoking cessation.
- Enrolls in smoking cessation program.
- Minimizes or eliminates exposures.
- Verbalizes the need for fluids.
- Is free of infection.
- Practices breathing techniques.
- Performs activities with less shortness of breath .
It is important for the nurse to assess the knowledge of patient and family members about self-care and the therapeutic regimen .
- Setting goals. If the COPD is mild, the objectives of the treatment are to increase exercise tolerance and prevent further loss of pulmonary function, while if COPD is severe, these objectives are to preserve current pulmonary function and relieve symptoms as much as possible.
- Temperature control. The nurse should instruct the patient to avoid extremes of heat and cold because heat increases the temperature and thereby raising oxygen requirements and high altitudes increase hypoxemia .
- Activity moderation. The patient should adapt a lifestyle of moderate activity and should avoid emotional disturbances and stressful situations that might trigger a coughing episode.
- Breathing retraining. The home care nurse must provide the education and breathing retraining necessary to optimize the patient’s functional status.
Documentation is an essential part of the patient’s chart because the interventions and medications given and done are reflected on this part.
- Document assessment findings including respiratory rate, character of breath sounds; frequency, amount and appearance of secretions laboratory findings and mentation level.
- Document conditions that interfere with oxygen supply.
- Document plan of care and specific interventions.
- Document liters of supplemental oxygen.
- Document client’s responses to treatment, teaching, and actions performed.
- Document teaching plan.
- Document modifications to plan of care.
- Document attainment or progress towards goals.
See also: Respiratory System NCLEX Practice Questions and Reviewer (220 Questions)
6 thoughts on “Chronic Obstructive Pulmonary Disease (COPD)”
This article is very helpful with nursing plans with first semester nursing students. Thank you.
VERY HELPFUL WITH NURSING CARE PLAN. THANK YOU
Full care plan send sir
VERY INFORMATIVE…
Hey Suzanne, Thanks a lot! 😊 Glad you found it helpful.
Very helpful for work use and outside of work use
Leave a Comment Cancel reply
COPD: Epidemiology, Pathogenesis, & Pathophysiology
Jan 03, 2020
510 likes | 556 Views
COPD: Epidemiology, Pathogenesis, & Pathophysiology. Wyatt E. Rousseau, MD May 11, 2006. COPD Definition.
Share Presentation
- chronic bronchitis
- lung function
- transferase p1
- early onset copd
- copd exacerbations pathogenic bacteria

Presentation Transcript
COPD: Epidemiology, Pathogenesis, & Pathophysiology Wyatt E. Rousseau, MD May 11, 2006
COPD Definition Chronic obstructive pulmonary disease (COPD) is a preventable and treatable disease state characterized by airflow limitation that is not fully reversible. The airflow limitation is usually progressive and is associated with an abnormal inflammatory response of the lungs to noxious particles or gases, primarily caused by cigarette smoking. Although COPD affects the lungs, it also produces significant systemic consequences.
COPD Definitions/Terms • Simple chronic bronchitis • Asthmatic bronchitis/Chronic asthmatic bronchitis • Chronic obstructive bronchitis – “small airways disease • Pulmonary emphysema
Simple chronic bronchitis Exposure to irritants without hyperreactive airways. Characterized by mucoid sputum production, decreased ciliary activity, and impaired resistance to infection.
Chronic asthmatic bronchitis or COPD with asthma Exposure to irritants in individuals with reactive or twitchy airways. Bronchospasm is frequently accompanied by excessive mucous production and edema of bronchial walls. Episodic worsening of airway obstruction often called asthma, but there is persisting obstruction, and often productive cough, with the episodic bronchospasm.
Obstructive Chronic Bronchitis Irreversible narrowing of airways, usually bronchioles or bronchi smaller than 2 mm., associated with increased resistance to airflow, hypoxemia, hypercapnea.
Pulmonary Emphysema Permanent, abnormal distension of the air spaces distal to the terminal bronchiole with destruction of alveolar septae, with or without fibrosis. Reduces lung elastic recoil causing airway collapse and irreversible airway obstruction.
Pathology – Chronic Bronchitis • Hypertrophy of mucous glands in submucosa of airways. Reid index (submucosa to bronchial wall). • Small airways obstruction esp. with goblet cell hyperplasia, mucosal and submucosal inflammatory cells, edema, peribronchial fibrosis, mucous plugs, and increased smooth muscles. • Alveolar epithelium is the target and the initiator of inflammation in CB, with neutrophils, macrophages, and CD8 lymphocytes causing epithelial cell release of IL-8 and other chemotactic and proinflammatory cytokines, and colony stimulating factors released in response to toxic, infectious, or inflammatory stimuli.
More CB Pathology • Injured epithelium may release reduced amounts of regulatory products such as ACE or neutral peptidase. • Sputum production is stimulated by increased exocytosis from secretory cells, lipid mediators, and inflammatory cell products. • Mucin gene expression is amplified by TNF-alpha, and secretory cell hyperplasia by the neutrophil enzymes elastase and cathepsin G.
Pathology - Emphysema • Classified by pattern of involvement of the acini distal to terminal bronchiole. • Centriacinar or Centrilobular – limited to respiratory bronchioles primarily with little change in acinus. Normal aging is associated with this. • Panacinar or Panlobular – involves both central and peripheral portions of the acinus.
Epidemiology • Background - Lung function over time • Cigarette smoking • Airway responsiveness and Allergy • Air Pollution • Occupational exposure to environmental dust and organic antigens • Infection • Antioxidant deficiency • Molecular/Genetic risk factors
Cigarette Smoking • Responsible for 80% of risk of Chronic Bronchitis • Doubles or triples rate of FEV1 decline • Responsible for 2-20 fold increase in death from COPD • Never smokers account for 23% of COPD • Only 15% of white and 5% Asian smokers develop COPD
Cigarette Smoking • Impairs ciliary movement • Inhibits alveolar macrophages • Leads to hypertrophy and hyperplasia of mucus-secreting glands • Probably inhibits antiprotease • Acutely increases vagally mediated smooth-muscle constriction
Airway Responsiveness-Dutch Hypothesis • Increased airways responsiveness and allergy are clinical phenotypes that predict increased susceptibility to cigarette smoke. • Methacholine and histamine responsiveness precedes and predicts accelerated decline in lung function, thus a risk factor for COPD.* • Increased airways responsiveness noted among 1st degree relatives of patients with early onset COPD.@ *Silva, GE et al. Asthma as a risk factor for COPD in a longitudinal study. Chest 2004; 126:59. @Celedon JC et al. Bronchodilator responsiveness and serum total IgE levels in families of probands with severe early-onset COPD. Eur Respir J 1999; 14:1009.
Air Pollution • Increased incidence and higher mortality rates of COPD in industrialized urban areas. • Exacerbations of CB clearly related to periods of heavy sulfur dioxide pollution and particulates. • Nitrogen dioxide NOT implicated in human airways obstruction.
Occupational Exposures • Environmental dusts – gold and coal miners • Organic antigens – COPD is most common respiratory syndrome in agricultural workers, and there is a 10% prevalence of COPD among farm workers • Accelerated decline in lung function among plastics workers exposed to toluene diisocyanate and in carding room workers in cotton mills
Infection • Severe viral pneumonia in childhood may lead to small airways obstruction (SAO). • Mortality, morbidity, and frequency of ARI are higher in patients with chronic bronchitis. • The Rhinovirus is found more often during COPD exacerbations…pathogenic bacteria, other viruses, & mycoplasmas found as often between as during exacerbations. However there is increased chance of detecting bacteria if sputum purulent*, and isolating new strain of bacteria may be associated with exacerbations.@ *Stockley RA et al. Relationship of sputum color to nature and outpatient management of acute exacerbation of COPD. Chest 2000; 117: 1638. @Sethi S et al. New strains of bacteria and exacerbations of COPD. N Engl J Med 2002; 347: 465.
Antioxidant Deficiency • Oxidizing radicals derive from cigarette smoke or may be released by phagocytes in the lung. Deficiencies of antioxidants vitamins may impair host defenses against oxidative radicals and permit tissue destruction leading to COPD. • Sanguinetti, CM. Oxidant/antioxidant imbalance: role in the pathogenesis of COPD. Respiration 1992; 59 Suppl 1:20.
Molecular/Genetic Risk Factors • Protease/antiprotease • TNF-a gene polymorphisms • Microsomal epoxide hydrolase* • Glutathione S-transferase P1 • Transforming growth factor beta 1* • Metalloproteinase dysregulation • Hersh, CP et al. Genetic association analysis offunctional impairment in chronic obstructive pulmonary disease. Am JRespir Crit Care Med 2006; 173: 977-984.
Protease/Antiprotease • Alpha –1- antitrypsin/elastase imbalance. • Alveolar macrophages from COPD patients express more matrix metalloproteinase (MMP)-9 than normals. Elevated MMP-9 is associated with an increase in degradation of elastin. • Russell RE et al. Release and activity of matrix metalloproteinase-9 and tissue inhibitor of metalloproteinase-1 by alveolar macrophages from patients with chronic obstructive pulmonary disease. Am J Respir Cell Mol Biol. 2002;283:L867-L873.
TNF – alpha gene polymorphisms • May influence host immune responses, increase inflammatory tissue damage, and favor the development of chronic bronchitis- a specific TNF-a polymorphism found in 19% CB vs. 5% schoolchildren vs. 2% of controls • Huang SL et al. Tumor necrosis factor-alpha gene polymorphism in chronic bronchitis. Am J Respir Crit Care Med 1997; 156:1436
Microsomal epoxide hydrolase • Microsomal epoxide hydrolase (MEH) reduces highly reactive epoxide intermediates generated by smoking. The genotypes associated with decreased activity of MEH were found in 19 and 22 per cent of COPD patients vs. 6% controls • Smith CAD, Harrison DJ. Association between polymorphism in gene for microsomal epoxide hydrolase and susceptibility to emphysema. Lancet 1997; 350:630.
Glutathione S-transferase P1 • Glutathione S-transferase P1 aids in the detoxification of substances in cigarette smoke, and COPD may occur more frequently among persons with decreased activity of this enzyme by virtue of genetic polymorphisms. • Ishii, T et al. Glutathione S-transferase P1 polymorphism in patients with chronic obstructive pulmonary disease. Thorax 1999; 54:693.
Transforming growth factor beta 1 • Transforming growth factor beta 1 is a member of a large family of polypeptides involved in cellular growth, differentiation, and activation. Specific, single nucleotide polymorphisms of the gene encoding transforming growth factor beta 1 have been associated with the development of COPD in smokers. • Wu, L et al. Transforming growth factor beta1 genotype and susceptibility to chronic obstructive pulmonary disease. Thorax 2004; 59:126.
Systemic Inflammation in Pathogenesis of COPD • COPD is a systemic disease. • Cytokines and other inflammatory markers are a response to cigarette smoke. • They circulate and may impact other diseases and symptoms, e.g. cardiac disease and cachexia. • Reduced lung function associated with increased levels of systemic inflammatory markers, including CRP, fibrinogen, WBC’s, and TNF-alpha.* • Gan WQ et al. Association between chronic obstructive pulmonary disease and systemic inflammation: a systematic review and meta-analysis. Thorax 2004; 59:574.
Elastic Recoil Pressure of the Lung • Provides radial support. • Major determinant of maximal expiratory flow. • Static recoil pressure of the lung is alveolar pressure minus pleural pressure. • Maximum expiratory flow rates represent a complex and dynamic interplay between airways caliber, elastic recoil pressures, and collapsibility of the airways.
Lung Volumes and Capacities in COPD • RV increased • FRC is the volume at which inward recoil of lung = outward recoil of chest wall…loss of elastic recoil will increase FRC • TLC increased due to loss of elastic recoil • VC may be normal to decreased
Time Constants • Prolonged in all obstructive diseases due to increased airways resistance and/or increased compliance. • If sufficiently prolonged, there is insufficient time for expiration, progressively increasing lung volume, moving tidal breathing to a higher, less compliant portion of the P/V curve, increasing work of breathing. • The increased elastic recoil pressure associated with the higher end-tidal volume is termed auto-PEEP or intrinsic PEEP, and this represents and additional threshold load that must be overcome.
Vd/Vt • Areas of wasted ventilation and wasted blood flow in COPD • Some maintain increased minute volume, with normal to low pCO2, and relatively high pO2 • Others may have less dyspnea, accepting higher pCO2 and a depressed pO2 • Difference debated – ventilatory drive related to peripheral or central chemoreceptor sensitivity or through other afferent pathways
Pulmonary Circulation Malfunctions • Regional maldistribution of blood flow • Abnormal pressure-flow relationships • Pulmonary hypertension often present • Reduced cross-sectional area due to anatomic changes and destruction of alveolar septae • Vessel constriction due to alveolar hypoxemia • Erythrocytosis also due to chronic hypoxemia
Clinical Correlates • Dyspnea and work capacity impairment • Emphysema usually greater impairment with less airways obstruction than chronic bronchitis • Usually dyspnea when FEV1<50% • Dyspnea at rest when FEV1<25% • CO2 retention and cor pulmonale often when FEV1<25% • Survival: 20-30% live >5years with CO2 retention
TORCH Towards a Revolution in COPD Health* *The TORCH Study Group. EurRespir J2004; 24: 2006-210.
TORCH • Multicenter, randomised, double-blind, parallel-group, placebo-controlled • 6200 patients, mod-severe COPD • Salmeterol/fluticasone 500/50 vs. Salmeterol 50 vs. Fluticasone 500 vs. placebo
TORCH preliminary results- to be published late 2006 • 17% relative reduction in mortality over 3 years cf. placebo. • Reduced exacerbations of COPD by 25% cf. placebo. • Improved QOL by St. George’s Respiratory Questionnaire. • Despite reduced rate of excerbations overall, there was increased reporting of adverse events classified as LRI cf. placebo.
- More by User
CTD objectives
CTD objectives. Know why CTDs are considered autoimmune diseases Know what the epidemiology of CTDs implies about their pathophysiology Understand the concept of disease criteria Know the criteria for SLE and SSc Consider the role of immune pathways in autoimmune disease pathogenesis
614 views • 32 slides
COPD. Chronic obstructive pulmonary disease. Juliana Tambellini University of Pittsburgh. COPD. C hronic O bstructive P ulmonary D isease A progressive disease that affects the lungs, making it difficult to breathe. COPD: an umbrella term.
1.43k views • 19 slides
Cigarettes in the pathogenesis of asthma and COPD
Cigarettes in the pathogenesis of asthma and COPD. John Jay Shannon, M.D. Divisions of Pulmonary and Critical Care Medicine John H. Stroger, Jr. Hospital of Cook County. John Jay Shannon, M.D. Disclosure of Conflict of Interest Information I have no existing conflict
556 views • 32 slides
COPD Tintinalli Chapter 69
2. Epidemiology. 4th most common killer in US3rd most common cause of hospitalization in the USOnly leading cause of death increasing in prevalence10% prevalence in 55-85 yrs Rare < 40 years old. 3. Epidemiology. Men > WomenPrevalence in women doubled in the past few decades Increased female smokingPrevalence highest in countries with most cigarette useMortality of hospitalized is 5-14%ICU mortality is 24%If age > 65, one year mortality post ICU discharge is 59%.
839 views • 60 slides
Anaesthesia for Patients with COPD
Anaesthesia for Patients with COPD. Dr Sajith Damodaran. University College of Medical Sciences & GTB Hospital, Delhi. COPD: Pathophysiology, Diagnosis, Treatment. Chronic Obstructive Pulmonary Disease. Definition:
4.07k views • 76 slides

Syphilis , Chlamydia and Gonorrhea : Bacteriology, Epidemiology, Pathogenesis, Clinical Manifestations, Diagnosis and Treatment. Group B6. Epidemiology - Syphilis. Epidemiology - Syphilis. Epidemiology - Syphilis. Epidemiology - Syphilis. Epidemiology - Syphilis. Epidemiology - Syphilis.
1.41k views • 56 slides
COPD update
COPD update. By Prof. Ramadan Nafae Professor and Head of Chest Diseases Department Faculty of Medicine Zagazig University. COPD update. Definition and Overview Diagnosis and Assessment Therapeutic Options Manage Stable COPD Manage Exacerbations Manage Comorbidities.
1.74k views • 87 slides
Viral Pathogenesis
Viral Pathogenesis. Viral Pathogenesis. Viral pathogenesis is the process by which a viral infection leads to disease. Viral pathogenesis is an abnormal situation of no value to the virus.
1.06k views • 32 slides
INSULINOMA. Epidemiology Pathophysiology & Symptoms Dignosis & Locallization Management Anaesthetic considerations. www.anaesthesia.co.in [email protected]. Epidemiology. First described by Harris in JAMA 1924 Commonest hormone producing NET of GIT 99% of pancreatic origin
4.69k views • 16 slides
病理生理学 Pathophysiology 山东大学医学院病理生理学教研室
病理生理学 Pathophysiology 山东大学医学院病理生理学教研室. Introduction Pathophysiology: The ology is to study the mechanisms of the occurrence, development and outcome of the diseases Pathological anatomy Pathology Pathophysiology
580 views • 16 slides
Tracheobronchomalacia
Tracheobronchomalacia. The ugly, but treatable step-cousin of the COPD family. Colin McKnight, MSIII, 2007. Presentation Outline. Brief review of “COPD†definition, epidemiology and economic costs Tracheobronchomalacia Definition Pathophysiology Known epidemiology and natural history
775 views • 48 slides
DIABETUS MELLITUS: ETIOLOGY, PATHOGENESIS, CLASSIFICATION, DIAGNOSTIC CRITERIA
DIABETUS MELLITUS: ETIOLOGY, PATHOGENESIS, CLASSIFICATION, DIAGNOSTIC CRITERIA. Martynyuk L.P. Epidemiology. About 2 to 4 % of the world population is affected with DM The disease is more common: in persons after age 45 in obese individuals in certain ethnic groups
869 views • 59 slides
Mechanical Ventilation in COPD patients
Mechanical Ventilation in COPD patients. Theodoros Vassilakopoulos Critical Care Department University of Athens Medical School Athens, Greece. Outline. Pathophysiology Non invasive ventilation during exacerbations to avoid intubation Controlled mechanical ventilation
2.57k views • 86 slides
COPD Health Education
COPD Health Education. Caregiving for People with COPD. COPD77722CONS SAR00341. Funding for this program provided by Boehringer Ingelheim Pharmaceuticals, Inc. and Pfizer Inc. What is a COPD Caregiver?. COPD Caregivers are people who take care of those with COPD. This may include:
650 views • 10 slides
COPD. All you wanted to know about COPD but were afraid to ask…. What to expect:. Definition Epidemiology Risk Factors History/Physical Findings Diagnostic Studies Overview of Current Treatment Options Treatment of exacerbations. What is COPD?.
712 views • 23 slides
CELIAC DISEASE
CELIAC DISEASE. A Lifetime Without Beer. Kyle Mulligan Northwestern Ontario Medical Program. Outline. Epidemiology Pathogenesis Clinical Features Associated Conditions Diagnosis Treatment. Epidemiology. True prevalence unknown Variable symptoms Slight female preponderance
984 views • 31 slides
COPD. Alison Boland StR Respiratory medicine. Aims & Objectives. Overview of COPD Recap basic knowledge Update on COPD Know when to use nebulisers and home oxygen therapy The role of NIV in palliative setting / end stage COPD Gain patient, carer and personal view about COPD.
1.47k views • 39 slides
COPD/asthma
COPD/asthma. Written by Mick Svoboda D.O. Presented by Dr Moosally D.O. COPD definition. COPD is characterized by airflow limitation that is not fully reversible. Airflow obstruction is progressive and associated with an abnormal inflammatory response to noxious particles or gases.
498 views • 23 slides
COPD. Tintinalli Chapter 73. COPD definition. Airflow limitation that is progressive and not fully reversible Abnormal inflammatory response to noxious particles or gases. Only major cause of death that is ↑ 85% chronic bronchitis Productive cough for >3 months x 2 yrs 15% emphysema
295 views • 12 slides
Pathogenesis of Stroke: Ischemia & Hemorrhage
Pathophysiology of Stroke Sid M. Shah, MD Assistant Residency Director Assistant Clinical Professor Department of Emergency Medicine Michigan State University East Lansing, MI. Pathogenesis of Stroke: Ischemia & Hemorrhage.
744 views • 22 slides
Got any suggestions?
We want to hear from you! Send us a message and help improve Slidesgo
Top searches
Trending searches
49 templates

44 templates

61 templates
american history
85 templates

el salvador
34 templates

63 templates
Chronic Obstructive Pulmonary Disease (COPD)
It seems that you like this template, chronic obstructive pulmonary disease (copd) presentation, free google slides theme, powerpoint template, and canva presentation template.
Chronic obstructive pulmonary disease, also known as COPD, encompasses a group of diseases that cause problems with breathing. In the United States alone it affects about 16 million people. If you are preparing a presentation about it you can use this Slidesgo proposal. It has a simple style, with a white background and light blue waves and lines, which convey elegance and serenity. In addition, we have included a multitude of resources that you can edit to convey your information, such as graphics, map, infographics, etc.
Features of this template
- 100% editable and easy to modify
- 26 different slides to impress your audience
- Contains easy-to-edit graphics such as graphs, maps, tables, timelines and mockups
- Includes 500+ icons and Flaticon’s extension for customizing your slides
- Designed to be used in Google Slides, Canva, and Microsoft PowerPoint
- 16:9 widescreen format suitable for all types of screens
- Includes information about fonts, colors, and credits of the free resources used
How can I use the template?
Am I free to use the templates?
How to attribute?
Attribution required If you are a free user, you must attribute Slidesgo by keeping the slide where the credits appear. How to attribute?
Register for free and start downloading now
Related posts on our blog.

How to Add, Duplicate, Move, Delete or Hide Slides in Google Slides

How to Change Layouts in PowerPoint

How to Change the Slide Size in Google Slides
Related presentations.
Create your presentation Create personalized presentation content
Writing tone, number of slides.

Premium template
Unlock this template and gain unlimited access

Register for free and start editing online

IMAGES
COMMENTS
COPD 101 is a presentation for healthcare providers on COPD, including risk factors, epidemiology, screening, diagnostics, and treatment. It is available in Basic, Enhanced, and Full PowerPoint formats for download.
COPD Digital Resource Toolkit for Health Professionals. Use the COPD resources below to help patients and their families and caregivers learn more about COPD including risk factors, signs and symptoms, treatment options, and more. Healthcare providers play an important role in the diagnosis and management of COPD.
Bronchodilators - inhaled medications that help to open up the airways within the lungs by relaxing the muscle around them. helps to relieve shortness of breath and coughing. long-acting and short-acting forms. with more severe disease, a long-acting and a short-acting bronchodilator may be used in combination.
COPD Foundation | Learn More, Take Action and Breathe Better
COPD National Action Plan Goals. Empower people with COPD, their families, and caregivers to recognize and reduce the burden of COPD. Improve the prevention, diagnosis, treatment, and management of COPD by improving the quality of care delivered across the health care continuum. Collect, analyze, report, and disseminate COPD-related public ...
Learn about COPD diagnosis, management and prevention with the updated GOLD teaching slide set for 2023. Download the PowerPoint file here.
Transcript. Slide 1-. Chronic Obstructive Pulmonary Disease (COPD) Slide 2-. COPD Description Characterized by presence of airflow obstruction Caused by emphysema or chronic bronchitis Generally progressive May be accompanied by airway hyperreactivity May be partially reversible. Slide 3-.
Similar presentations . More. Presentation on theme: "NURSING MANAGEMENT OF COPD. Physiology Respiratory System Upper Tract & Lower Tract Goal is to transfer oxygen and carbon dioxide."— Presentation transcript: 1 NURSING MANAGEMENT OF COPD 2 Physiology ...
COPD 101: Understanding the Basics of COPD, covers introductory information about COPD and includes a screening tool and symptom tracker. COPD 201: Beyond the Basics, will be of particular interest to those looking for more advanced information and covers topics such as medication, treatments, smoking cessation, nutrition, and co-existing ...
COPD is a long-term disease that often gets worse over time and is characterized by inflammation and severe limitation of air flow in and out of the lungs. COPD is an umbrella term used to describe a group of breathing conditions, the most common being chronic bronchitis and emphysema. Many people living with COPD may have both emphysema and ...
Whether you're presenting research findings, educating colleagues, or delivering a medical lecture, this template provides a visually appealing and informative slideshow. Engage your audience with captivating visuals and concise content. Take your presentations to the next level and make an impact with our COPD presentation template.
The goals of COPD treatment are to relieve symptoms, slow the progression of disease, improve exercise tolerance, prevent and manage complications such as "flare-ups", and improve overall health. Patients should become informed about COPD by speaking with their doctor. Sometimes a referral to a pulmonologist, or lung doctor, may be required.
Patient and family teaching is an important nursing intervention to enhance self-management in patients with any chronic pulmonary disorder. To achieve airway clearance: The nurse must appropriately administer bronchodilators and corticosteroids and become alert for potential side effects. Direct or controlled coughing.
PK !!¡ú*· NS [Content_Types].xml ¢ ( ÌœÛnÚ@ †ï+õ ,ßV`¯Ï®BrÑÃU ''>ÀÖ^À +ï& oßµ!© '@b¬ n ¶wfÿ ðy€ù÷ìâ®*[Ѫ¢© 6›»¶%ê¬É‹zµ° \ ž%¶¥4¯s^6µXØ ¡ì‹ó·oή7R(ËD×ja¯µ-ï GekQq5o¤¨Í•eÓV\›ÃvåHžýæ+áx® 9YSkQë™îrØçg Å'ß"ÚútgNo•Èze[ ¶ãº© vQuñÝygoÄ/)ö‡ô öÇ´¢T b¸"e'qm®;·uþh-³Ý ...
COPD: Epidemiology, Pathogenesis, & Pathophysiology Wyatt E. Rousseau, MD May 11, 2006. COPD Definition Chronic obstructive pulmonary disease (COPD) is a preventable and treatable disease state characterized by airflow limitation that is not fully reversible. The airflow limitation is usually progressive and is associated with an abnormal inflammatory response of the lungs to noxious particles ...
Average cost of hospital stay for ten days = $10,000. Total cost of COPD hospitalizations per year = $1.5 billion. Potential effects of hospitalization include: • Decreased quality of life. • Risk of acquiring nosocomial infections. • Weakness. • Close monitoring of condition. • Exposure to health teaching.
Free Google Slides theme, PowerPoint template, and Canva presentation template. Chronic obstructive pulmonary disease, also known as COPD, encompasses a group of diseases that cause problems with breathing. In the United States alone it affects about 16 million people. If you are preparing a presentation about it you can use this Slidesgo proposal.
PK !GÒ~Dé ppt/presentation.xmlì—ÝnÛ Çï'í ,ßN©ƒ¿ Å©šuž&uRÔ´ @mÒXÅ` IÓN{÷ ˆ" ¸šú¾ ð?çpø 0gz½k¨³%BÖœå.º » a%¯jöœ» Å(u ©0«0åŒäî 'îõìë—i;i '„)¬ÀÕ 0LNpj'ž'Ë5i°¼â-a ¸h°‚®xö* _!|C= Ž½ ×ÌíüÅgüùjU—ä-—› ¦ß „šäºnå!Zû™hö*ÎS'xK-›'ITÁ™'@Ç Á²%~c©ˆøUÝIu1âÔUîú(LÂ4ˆC ...