Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.
This case study presents a 68-year old “right-handed” African-American man named Randall Swanson. He has a history of hypertension, hyperlipidemia and a history of smoking one pack per day for the last 20 years. He is prescribed Atenolol for his HTN, and Simvastatin for Hyperlipidemia (but he has a history of not always taking his meds). His father had a history of hypertension and passed away from cancer 10 years ago. His mother has a history of diabetes and is still alive.
Randall was gardening with his wife on a relaxing Sunday afternoon. Out of nowhere, Randall fell to the ground. When his wife rushed to his side and asked how he was doing, he answered with garbled and incoherent speech. It was then that his wife noticed his face was drooping on the right side. His wife immediately called 911 and paramedics arrived within 6 minutes. Upon initial assessment, the paramedics reported that Randall appeared to be experiencing a stroke as he presented with right-sided facial droop and weakness and numbness on the right side of his body. Fortunately, Randall lived nearby a stroke center so he was transported to St. John’s Regional Medical Center within 17 minutes of paramedics arriving to his home.
Initial Managment
Upon arrival to the Emergency Department, the healthcare team was ready to work together to diagnose Randall. He was placed in bed with the HOB elevated to 30 degrees to decrease intracranial pressure and reduce any risks for aspiration. Randall’s wife remained at his side and provided the care team with his brief medical history which as previously mentioned, consists of hypertension, hyperlipidemia and smoking one pack per day for the last 20 years. He had no recent head trauma, never had a stroke, no prior surgeries, and no use of anticoagulation medications.
Physical Assessment
Upon first impression, Nurse Laura recognized that Randall was calm but looked apprehensive. When asked to state his name and date of birth, his speech sounded garbled at times and was very slow, but he could still be understood. He could not recall the month he was born in but he was alert and oriented to person, time, and situation. When asked to state where he was, he could not recall the word hospital. He simply pointed around the room while repeating “here.”
Further assessment revealed that his pupils were equal and reactive to light and that he presented with right-sided facial paralysis. Randall was able to follow commands but when asked to move his extremities, he could not lift his right arm and leg. He also reported that he could not feel the nurse touch his right arm and leg. Nurse Laura gathered the initial vital signs as follows: BP: 176/82, HR: 93, RR: 20, T:99.4, O2: 92% RA and a headache with pain of 3/10.
Doctor’s Orders
The doctor orders were quickly noted and included:
-2L O2 (to keep O2 >93%)
– 500 mL Bolus NS
– VS Q2h for the first 8 hrs.
-Draw labs for: CBC, INR, PT/INR, PTT, and Troponin
-Get an EKG
-Chest X ray
-Glucose check
-Obtain patient weight
-Perform a National Institute of Health Stroke Scale (also known as NIHSS) Q12h for the first 24 hours, then Q24h until he is discharged
-Notify pharmacy of potential t-PA preparation.
Nursing Actions
Nurse Laura started an 18 gauge IV in Randall’s left AC and started him on a bolus of 500 mL of NS. A blood sample was collected and quickly sent to the lab. Nurse Laura called the Emergency Department Tech to obtain a 12 lead EKG.
Pertinent Lab Results for Randall
The physician and the nurse review the labs:
WBC 7.3 x 10^9/L
RBC 4.6 x 10^12/L
Plt 200 x 10^9/L
LDL 179 mg/dL
HDL 43 mg/dL
Troponin <0.01 ng/mL
EKG and Chest X Ray Results
The EKG results and monitor revealed Randall was in normal sinus rhythm; CXR was negative for pulmonary or cardiac pathology
CT Scan and NIHSS Results
The NIH Stroke Scale was completed and demonstrated that Randall had significant neurological deficits with a score of 13. Within 20 minutes of arrival to the hospital, Randall had a CT-scan completed. Within 40 minutes of arrival to the hospital, the radiologist notified the ED physician that the CT-scan was negative for any active bleeding, ruling our hemorrhagic stroke.
The doctors consulted and diagnosed Randall with a thrombotic ischemic stroke and determined that that plan would include administering t-PA. Since Randall’s CT scan was negative for a bleed and since he met all of the inclusion criteria he was a candidate for t-PA. ( Some of the inclusion criteria includes that the last time the patient is seen normal must be within 3 hours, the CT scan has to be negative for bleeding, the patient must be 18 years or older, the doctor must make the diagnosis of an acute ischemic stroke, and the patient must continue to present with neurological deficits.)
Since the neurologist has recommended IV t-PA, the physicians went into Randall’s room and discussed what they found with him and his wife. Nurse Laura answered and addressed any remaining concerns or questions.
Administration
Randall and his wife decided to proceed with t-PA therapy as ordered, therefore Nurse Laura initiated the hospital’s t-PA protocol. A bolus of 6.73 mg of tPA was administered for 1 minute followed by an infusion of 60.59 mg over the course of 1 hour. ( This was determined by his weight of 74.8 kg). After the infusion was complete, Randall was transferred to the ICU for close observation. Upon reassessment of the patient, Randall still appeared to be displaying neurological deficits and his right-sided paralysis had not improved. His vital signs were assessed and noted as follows: BP: 149/79 HR: 90 RR: 18 T:98.9 O2: 97% 2L NC Pain: 2/10.
Randall’s wife was crying and he appeared very scared, so Nurse John tried to provide as much emotional support to them as possible. Nurse John paid close attention to Randall’s blood pressure since he could be at risk for hemorrhaging due to the medication. Randall was also continually assessed for any changes in neurological status and allergic reactions to the t-PA. Nurse John made sure that Stroke Core Measures were followed in order to enhance Randall’s outcome.
In the ICU, Randall’s neurological status improved greatly. Nurse Jan noted that while he still garbled speech and right-sided facial droop, he was now able to recall information such as his birthday and he could identify objects when asked. Randall was able to move his right arm and leg off the bed but he reported that he was still experiencing decreased sensation, right-sided weakness and he demonstrated drift in both extremities.
The nurse monitored Randall’s blood pressure and noted that it was higher than normal at 151/83. She realized this was an expected finding for a patient during a stroke but systolic pressure should be maintained at less than 185 to lower the risk of hemorrhage. His vitals remained stable and his NIHSS score decreased to an 8. Labs were drawn and were WNL with the exception of his LDL and HDL levels. His vital signs were noted as follows: BP 151/80 HR 92 RR 18 T 98.8 O2 97% RA Pain 0/10
The Doctor ordered Physical, Speech, and Occupational therapy, as well as a swallow test.
Swallowing Screen
Randall remained NPO since his arrival due to the risks associated with swallowing after a stroke. Nurse Jan performed a swallow test by giving Randall 3 ounces of water. On the first sip, Randall coughed and subsequently did not pass. Nurse Jan kept him NPO until the speech pathologist arrived to further evaluate Randall. Ultimately, the speech pathologist determined that with due caution, Randall could be put on a dysphagia diet that featured thickened liquids
Physical Therapy & Occupational Therapy
A physical therapist worked with Randall and helped him to carry out passive range of motion exercises. An occupational therapist also worked with Randall to evaluate how well he could perform tasks such as writing, getting dressed and bathing. It was important for these therapy measures to begin as soon as possible to increase the functional outcomes for Randall. Rehabilitation is an ongoing process that begins in the acute setting.
Day 3- third person
During Day 3, Randall’s last day in the ICU, Nurse Jessica performed his assessment. His vital signs remained stable and WNL as follows: BP: 135/79 HR: 90 RR: 18 T: 98.9 O2: 97% on RA, and Pain 0/10. His NIHSS dramatically decreased to a 2. Randall began showing signs of improved neurological status; he was able to follow commands appropriately and was alert and oriented x 4. The strength in his right arm and leg markedly improved. he was able to lift both his right arm and leg well and while he still reported feeling a little weakness and sensory loss, the drift in both extremities was absent.
Rehabilitation Therapies
Physical, speech, and occupational therapists continued to work with Randall. He was able to call for assistance and ambulate with a walker to the bathroom and back. He was able to clean his face with a washcloth, dress with minimal assistance, brush his teeth, and more. Randall continued to talk with slurred speech but he was able to enunciate with effort.
On day 4, Randall was transferred to the med-surg floor to continue progression. He continued to work with physical and occupational therapy and was able to perform most of his ADLs with little assistance. Randall could also ambulate 20 feet down the hall with the use of a walker.
Long-Term Rehabilitation and Ongoing Care
On day 5, Randall was discharged to a rehabilitation facility and continued to display daily improvement. The dysphagia that he previously was experiencing resolved and he was discharged home 1.5 weeks later. Luckily for Randall, his wife was there to witness his last known well time and she was able to notify first responders. They arrived quickly and he was able to receive t-PA in a timely manner. With the help of the interdisciplinary team consisting of nurses, therapists, doctors, and other personnel, Randall was put on the path to not only recover from the stroke but also to quickly regain function and quality of life very near to pre-stroke levels. It is now important that Randall continues to follow up with his primary doctor and his neurologist and that he adheres to his medication and physical therapy regimen.
Case Management
During Randall’s stay, Mary the case manager played a crucial role in Randall’s path to recovery. She determined that primary areas of concern included his history of medical noncompliance and unhealthy lifestyle. The case manager consulted with Dietary and requested that they provide Randall with education on a healthy diet regimen. She also provided him with smoking cessation information. Since Randall has been noncompliant with his medications, Mary determined that social services should consult with him to figure out what the reasons were behind his noncompliance. Social Services reported back to Mary that Randall stated that he didn’t really understand why he needed to take the medication. It was apparent that he had not been properly educated. Mary also needed to work with Randall’s insurance to ensure that he could go to the rehab facility as she knew this would greatly impact his ultimate outcome. Lastly, throughout his stay, the case manager provided Randall and his wife with resources on stroke educational materials. With the collaboration of nurses, education on the benefits of smoking cessation, medication adherence, lifestyle modifications, and stroke recognition was reiterated to the couple. After discharge, the case manager also checked up with Randall to make sure that he complied with his follow up appointments with the neurologist and physical and speech therapists,
- What risk factors contributed to Randall’s stroke?
- What types of contraindications could have prevented Randall from receiving t-PA?
- What factors attributed to Randall’s overall favorable outcome?
Nursing Case Studies by and for Student Nurses Copyright © by jaimehannans is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License , except where otherwise noted.

Share This Book
- Remote Access
- Save figures into PowerPoint
- Download tables as PDFs

Chapter 7: 10 Real Cases on Transient Ischemic Attack and Stroke: Diagnosis, Management, and Follow-Up
Jeirym Miranda; Fareeha S. Alavi; Muhammad Saad
- Download Chapter PDF
Disclaimer: These citations have been automatically generated based on the information we have and it may not be 100% accurate. Please consult the latest official manual style if you have any questions regarding the format accuracy.
Download citation file:
- Search Book
Jump to a Section
Case review, case discussion, clinical symptoms.
- Radiologic Findings
- Full Chapter
- Supplementary Content
Case 1: Management of Acute Thrombotic Cerebrovascular Accident Post Recombinant Tissue Plasminogen Activator Therapy
A 59-year-old Hispanic man presented with right upper and lower extremity weakness, associated with facial drop and slurred speech starting 2 hours before the presentation. He denied visual disturbance, headache, chest pain, palpitations, dyspnea, dysphagia, fever, dizziness, loss of consciousness, bowel or urinary incontinence, or trauma. His medical history was significant for uncontrolled type 2 diabetes mellitus, hypertension, hyperlipidemia, and benign prostatic hypertrophy. Social history included cigarette smoking (1 pack per day for 20 years) and alcohol intake of 3 to 4 beers daily. Family history was not significant, and he did not remember his medications. In the emergency department, his vital signs were stable. His physical examination was remarkable for right-sided facial droop, dysarthria, and right-sided hemiplegia. The rest of the examination findings were insignificant. His National Institutes of Health Stroke Scale (NIHSS) score was calculated as 7. Initial CT angiogram of head and neck reported no acute intracranial findings. The neurology team was consulted, and intravenous recombinant tissue plasminogen activator (t-PA) was administered along with high-intensity statin therapy. The patient was admitted to the intensive care unit where his hemodynamics were monitored for 24 hours and later transferred to the telemetry unit. MRI of the head revealed an acute 1.7-cm infarct of the left periventricular white matter and posterior left basal ganglia. How would you manage this case?
This case scenario presents a patient with acute ischemic cerebrovascular accident (CVA) requiring intravenous t-PA. Diagnosis was based on clinical neurologic symptoms and an NIHSS score of 7 and was later confirmed by neuroimaging. He had multiple comorbidities, including hypertension, diabetes, dyslipidemia, and smoking history, which put him at a higher risk for developing cardiovascular disease. Because his symptoms started within 4.5 hours of presentation, he was deemed to be a candidate for thrombolytics. The eligibility time line is estimated either by self-report or last witness of baseline status.
Ischemic strokes are caused by an obstruction of a blood vessel, which irrigates the brain mainly secondary to the development of atherosclerotic changes, leading to cerebral thrombosis and embolism. Diagnosis is made based on presenting symptoms and CT/MRI of the head, and the treatment is focused on cerebral reperfusion based on eligibility criteria and timing of presentation.
Symptoms include alteration of sensorium, numbness, decreased motor strength, facial drop, dysarthria, ataxia, visual disturbance, dizziness, and headache.
Get Free Access Through Your Institution
Pop-up div successfully displayed.
This div only appears when the trigger link is hovered over. Otherwise it is hidden from view.
Please Wait
Explore prestigious scientific journals and award and funding opportunities to advance your research.
Access practice-improvement tools, including guidelines, measures, and practice management resources.
Learn to effectively advocate on behalf of neurologists and their patients, and access AAN position and policy statements.
Loading... please wait
We’re experiencing unusually high levels of traffic. Thank you for your patience.
Inpatient Stroke Case Studies
Inpatient e/m case studies.
Case study of a stroke patient at varying visit levels to better understand code selection for inpatient encounters under the revised guidelines for 2024.
67-year-old Female with Stroke
Total time* for Inpatient E/M in 2023
Refer to the following tables for correct code selection when billing based on time for inpatient E/M Services:
| CPT Code | Time (Minutes) | |
| 99221 99222 99223 | 40 55 75 | |
| 99231 99232 99233 | 25 35 50 | |
| 99291 99292 | First 30-74 Each additional 30 |
*Total time includes non face-to-face time on the date of service
Day 1: Critical Care (99291)
A 67-year-old woman with hypertension and diabetes presents to the emergency department with abrupt onset of left hemiparesis 45 minutes ago.
Pre-evaluation : Discussed presentation and vital signs with ED provider (3 mins).
Face-to-face evaluation : Performed medically appropriate history and exam. She has a dense left hemiparesis and an NIH Stroke Scale score of 8. Thrombolysis safety criteria reviewed (7 mins).
Post-evaluation : Non-contrast head CT, CTA of head and neck, and lab results reviewed in the ED. Case discussed with ED provider and thrombolysis recommended. Consultation documented in the ED (25 mins).
Total time : 35 minutes.
| Problems Addressed | Data Reviewed | Patient Management Risk of Complications |
| Acute impairment of a vital organ system with high risk of deterioration | Independent hisotry, review of vitals and lab data, review of head CT and other imaging | Recommendation for thrombolysis |
| High/Critical | High/Critical | High/Critical |
Critical Care Coding
According to the 2024 CPT code set, a provider may bill for critical care when the following requirements are met:
- A critical condition: one that acutely impairs a vital organ system with a high probability of imminent or life-threatening deterioration. This includes, for example, central nervous system failure.
- Direct delivery of critical care: high complexity decision-making to assess, manipulate, and support vital systems to treat organ system failure or prevent further life-threatening deterioration.
- At least 30 minutes of time spent solely in the care of the patient. It does not need to be continuous, and it includes both time at the bedside and time spent on the same floor or unit engaged in work directly related to the patient’s care (e.g., documenting critical care, reviewing test results, discussing care with other providers, obtaining history, or discussing treatments or treatment limitations with surrogates when the patient lacks the capacity to do so).
Specific critical care credentials are not required to bill critical care. Critical care is usually provided in a critical care area such as an intensive care unit or emergency department, but this is not always the case (for example, critical care provided to a deteriorating patient in a non-critical care unit).
Other examples of critical care might include:
- Evaluating a patient with status epilepticus and prescribing anti-epileptic drugs or sedative infusions,
- Evaluating a patient with acute respiratory failure from neuromuscular disease and prescribing plasmapheresis,
- Evaluating a patient with coma after cardiac arrest and discussing prognosis, treatment, and goals of care with surrogates (documenting the patient’s lack of capacity to participate)
| Condition | Treatment | Time |
| Acute ischemic stroke | Thrombolysis | 35 minutes |
Critical care, 30-74 minutes CPT 99291 is justified based on the above documentation, although E&M codes (e.g., 99223) associated with fewer wRVUs and lower reimbursement could be used as well.
Day 2: Subsequent Hospital Inpatient Care
Pre-rounds : Reviewed vitals, labs, and studies (LDL, Hemoglobin A1c, EKG, TTE). Review and document independent interpretation of MRI (8 mins).
On Rounds : Performed medically appropriate history and exam. The patient’s symptoms and findings improved somewhat overnight. Patient counseled about stroke evaluation and secondary prevention (10 mins).
Post-rounds : Order atorvastatin, order diabetes consult for management of diabetes. Document discussion with case management possible need for acute inpatient rehabilitation. Documentation completed (10 mins).
Total time : 28 minutes
| Problems Addressed | Data Reviewed | Patient Management Risk of Complications |
| One acute illness that poses a threat to life or bodily function | Review of test results Independent interpretation of tests Discussion of management | Prescription drug management |
| High | High | Moderate |
| Time | MDM |
| Total time of visit (includes all time on pre-rounds, on round, and post-rounds): Subsequent encounter, level 1: ≥ 25 minutes
| Problems addressed: Data reviewed: Risk of complications: Level 3:
|
In this situation, billing according to MDM would be associated with higher reimbursement.
Day 3: Discharge Day Management (By Primary Service)
Pre-rounds : Reviewed vitals, daily CBC and BMP, nursing notes and PT/OT notes (5 mins).
On Rounds : Performed medically appropriate history and exam. The patient reports continued slight improvement in symptoms and requests counseling on how complementary and alternative medicine might help manage her chronic conditions (15 mins).
Post-rounds : Prescribe antiplatelet agent, antidiabetic medications, and antihypertensives. Prepare discharge paperwork and document discharge summary (15 mins).
Total time : 35 minutes
| Problems Addressed | Data Reviewed | Patient Management Risk of Complications |
| One acute illness that poses a threat to life or bodily function | Limited | Prescription drug management |
| High | Low | Moderate |
Discharge Day Management Coding (Inpatient or Observation)
Discharge CPTs are selected based on total (face-to-face and non-face-to-face) time, not MDM:
- 99238: 30 minutes or less
- 99239: 31 minutes or more
Discharge CPTs would be used by the primary attending service (e.g., a Neurohospitalist service). Consulting services would continue to choose Subsequent Day codes based on time or MDM.
Discharge Day Management, 31 minutes or more CPT 99239
Disclaimer: The billing and coding information provided by the American Academy of Neurology and its affiliates (collectively, “Academy”) are assessments of clinical information provided as an educational service. The information (1) is not clinical advice; (2) does not account for how private payers cover and reimburse procedures or services*; (3) is not continually updated and may not reflect the most current clinical information (new clinical information may emerge between the time information is developed and when it is published or read); and (4) is not a substitute for the independent professional judgment of the treating provider, who is responsible for correctly coding procedures and services.
Using this information is voluntary. The Academy is providing the information on an “as is” basis and makes no warranty, expressed or implied, regarding the information. The Academy specifically disclaims any warranties of merchantability or fitness for a particular use or purpose. The Academy assumes no responsibility for any injury or damage to persons or property arising out of or related to any use of this information or for any errors or omissions.
*The Academy recommends always checking private payer policies before rendering procedures or services
Case Presentation
Statement of ethics, conflict of interest statement, funding sources, author contributions, ischemic stroke in a 29-year-old patient with covid-19: a case report.
- Split-Screen
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- Open the PDF for in another window
- Get Permissions
- Cite Icon Cite
- Search Site
Christian Avvantaggiato , Loredana Amoruso , Maria Pia Lo Muzio , Maria Assunta Mimmo , Michelina Delli Bergoli , Nicoletta Cinone , Luigi Santoro , Lucia Stuppiello , Antonio Turitto , Chiara Ciritella , Pietro Fiore , Andrea Santamato; Ischemic Stroke in a 29-Year-Old Patient with COVID-19: A Case Report. Case Rep Neurol 2 September 2021; 13 (2): 334–340. https://doi.org/10.1159/000515457
Download citation file:
- Ris (Zotero)
- Reference Manager
Increasing evidence reports a greater incidence of stroke among patients with Coronavirus disease 2019 (COVID-19) than the non-COVID-19 population and suggests that SARS-CoV-2 infection represents a risk factor for thromboembolic and acute ischemic stroke. Elderly people have higher risk factors associated with acute ischemic stroke or embolization vascular events, and advanced age is strongly associated with severe COVID-19 and death. We reported, instead, a case of an ischemic stroke in a young woman during her hospitalization for COVID-19-related pneumonia. A 29-year-old woman presented to the emergency department of our institution with progressive respiratory distress associated with a 2-day history of fever, nausea, and vomiting. The patient was transferred to the intensive care unit (ICU) where she underwent a tracheostomy for mechanical ventilation due to her severe clinical condition and her very low arterial partial pressure of oxygen. The nasopharyngeal swab test confirmed SARS-CoV-2 infection. Laboratory tests showed neutrophilic leucocytosis, a prolonged prothrombin time, and elevated D-dimer and fibrinogen levels. After 18 days, during her stay in the ICU after suspension of the medications used for sedation, left hemiplegia was reported. Central facial palsy on the left side, dysarthria, and facial drop were present, with complete paralysis of the ipsilateral upper and lower limbs. Computed tomography (CT) of the head and magnetic resonance imaging of the brain confirmed the presence of lesions in the right hemisphere affecting the territories of the anterior and middle cerebral arteries, consistent with ischemic stroke. Pulmonary and splenic infarcts were also found after CT of the chest. The age of the patient and the absence of serious concomitant cardiovascular diseases place the emphasis on the capacity of SARS-CoV-2 infection to be an independent cerebrovascular risk factor. Increased levels of D-dimer and positivity to β2-glycoprotein antibodies could confirm the theory of endothelial activation and hypercoagulability, but other mechanisms – still under discussion – should not be excluded.
Coronavirus disease 2019 (COVID-19), caused by the novel coronavirus SARS-CoV-2, is characterized by a wide range of symptoms, most of which cause acute respiratory distress syndrome [1, 2], associated with intensive care unit (ICU) admission and high mortality [3]. On March 11, 2020, the large global outbreak of the disease led the World Health Organization (WHO) to declare COVID-19 a pandemic, with 11,874,226 confirmed cases and 545,481 deaths worldwide (July 9, 2020) [4]. In many cases, the clinical manifestations of COVID-19 are characteristic of a mild disease that may, however, worsen to a critical lower respiratory infection [2]. At the onset of the disease, the most frequent symptoms are fever, dry cough, fatigue, and shortness of breath as the infection progresses may appear signs and symptoms of respiratory failure that require ICU admission [5, 6]. Although acute respiratory distress syndrome is the most important cause of ICU admission for COVID-19 patients, several studies have underlined the presence of neurological symptoms such as confusion, dizziness, impaired consciousness, ataxia, seizure, anosmia, ageusia, vision impairment, and stroke [7, 8]. In particular, the state of hypercoagulability in patients affected by COVID-19 favors the formation of small and/or large blood clots in multiple organs, including the brain, potentially leading to cerebrovascular disease (ischemic stroke but also intracranial hemorrhage) [9, 10 ].
We found an interesting case of stroke following a SARS-CoV-2 infection in a young patient. A 29-year-old woman, during her ICU hospitalization for COVID-19-related pneumonia, was diagnosed with ischemic stroke of the right hemisphere, without other cardiac/cerebrovascular risk factors except hypertension. The young age of the patient and the absence of higher cerebrovascular risk factors make the present case very interesting as it can help demonstrate that COVID-19 is an independent risk factor for acute ischemic stroke. In a case series of 214 patients with COVID-19 (mean [SD] age, 52.7 [15.5] years), neurologic symptoms were more common in patients with severe infection who were older than the others [ 11 ]. New-onset CVD was more common in COVID-19 patients who had underlying cerebrovascular risk factors, such as older age (>65 years) [ 12 ], and very few cases of stroke in patients younger than 50 years have been reported [ 12, 13 ]. Our case seems to be the only one younger than 30 years.
On the night between March 19 and 20, 2020, a 29-year-old woman was referred to our hospital “Policlinico Riuniti di Foggia” due to a progressive respiratory distress associated with a 2-day history of fever, nausea, and vomiting. At presentation, the heart rate was 128 bpm, the blood oxygen saturation measured by means of the pulse oximeter was 27%, the respiratory rate was 27 breaths per minute, and the blood pressure was 116/77 mm Hg. The arterial blood gas test showed a pH of 7.52, pO 2 20 mm Hg, and pCO 2 34 mm Hg. The patient was immediately transferred to the ICU where she underwent tracheostomy and endotracheal intubation for mechanical ventilation due to her severe clinical condition and deteriorated pulmonary gas exchange. The diagnosis of COVID-19 was confirmed by PCR on a nasopharyngeal swab.
The family medical history was normal, and the only known pre-existing medical conditions were polycystic ovary syndrome (diagnosed 3 years earlier), conversion disorder, and hypertension (both diagnosed 2 years earlier). Ramipril and nebivolol were prescribed for the high blood pressure treatment, and sertraline was prescribed for the conversion disorder treatment. Drug therapy adherence was inconstant. The patient had no history of diabetes, cardiac pathologies, strokes, transient ischemic attacks, thromboembolic, or other vascular pathologies.
Laboratory tests showed neutrophilic leukocytosis (white blood cell count 14.79 × 10 3 , neutrophil percentage 89.8%, and neutrophil count 13.29 × 10 3 ), a prolonged prothrombin time (15.3 s) with a slightly elevated international normalized ratio (1.38), and elevated D-dimer (6,912 ng/mL) and fibrinogen levels (766 mg/dL). Other findings are shown in Table 1 .
Laboratory test

This pharmacological therapy was set as follows: enoxaparin 6,000 U.I. once a day, piperacillin 4 g/tazobactam 0.5 g twice a day; Kaletra, a combination of lopinavir and ritonavir indicated for human immunodeficiency virus (HIV) infection treatment, 2 tablets twice a day; hydroxychloroquine 200 mg once a day; and furosemide 250 mg, calcium gluconate, and aminophylline 240 mg 3 times a day. No adverse events were reported.
On April 7, 2020, during her stay in the ICU and after suspension of the medications used for sedation, left hemiplegia was reported. The same day, the patient underwent a computed tomography examination of the head, which showed areas of hypodensity in the right hemisphere due to recent cerebral ischemia.
On April 16, 2020, the patient was oriented to time, place, and person. Central facial palsy on the left side, dysarthria, and facial drop were present, with complete paralysis of the ipsilateral upper and lower limbs. The power of all the muscles of the left limbs was grade 0 according to the Medical Research Council (MRC) scale. Deep tendon reflexes were reduced on the left upper limb but hyperactive on the ipsilateral lower limb, with a slight increase in the muscle tonus. The senses of touch, vibration, and pain were reduced on the left side of the face and body.
On the same day, the patient underwent magnetic resonance imaging (MRI) of the brain (Fig. 1 a), showing lesions on the right hemisphere affecting the territories of the anterior and middle cerebral arteries. On May 5, 2020, magnetic resonance angiography showed an early duplication of the sphenoidal segment of the right middle cerebral artery, the branches of which are irregular with rosary bead-like aspects (Fig. 1 d, e); on the same day, the second MRI (Fig. 1 b) confirmed the lesions. Computed tomography of the chest (Fig. 1 c) and abdomen (Fig. 1 f), performed 5 days after the MRI of the brain, showed not only multifocal bilateral ground-glass opacities but also a basal subpleural area of increased density within the left lung (4 × 4 × 3 cm), consistent with a pulmonary infarction. In addition, a vascular lesion, consistent with a splenic infarct, was found in the inferior pole of the spleen. Doppler echocardiography of the hearth showed regular right chambers and left atrium and a slightly hypertrophic left ventricle with normal size and kinetics (ejection fraction: 55%). The age of the patient and the absence of serious concomitant cardiovascular diseases place the emphasis on the capacity of SARS-CoV-2 infection to be an independent cerebrovascular risk factor.

Imaging. a April 16, 2020; MRI of the brain: lesions in the right hemisphere affecting the territories of the anterior and the middle cerebral arteries. b May 5, 2020; MRI of the brain: same lesions in the right hemisphere shown in the previous image. d , e May 5, 2020; MRA showed an early duplication of the sphenoidal segment of the right middle cerebral artery, the branches of which are irregular with rosary bead-like aspect and reduction of blood flow in the middle cerebral artery. c April 20, 2020; CT of the abdomen: vascular lesion, consistent with a splenic infarct, found in the inferior pole of the spleen. f April 20, 2020; CT of the chest: basal subpleural area of increased density within the left lung (4 × 4 × 3 cm), consistent with a pulmonary infarction. MRA, magnetic resonance angiography; CT, computed tomography; MRI, magnetic resonance imaging.
The pandemic outbreak of novel SARS-CoV-2 infection has caused great concern among the services and authorities responsible for public health due to not only the mortality rate but also the danger of filling up hospital capacities in terms of ICU beds and acute non-ICU beds. In this regard, the nonrespiratory complications of COVID-19 should also be taken into great consideration, especially those that threaten patients’ lives and extend hospitalization times. Stroke is one of these complications, since a greater incidence of stroke among patients with COVID-19 than the non-COVID-19 population has been reported, and a preliminary case-control study demonstrated that SARS-CoV-2 infection represents a risk factor for acute ischemic stroke [ 14 ].
We found that the reported case is extremely interesting, since the woman is only 29 years old and considering how stroke in a young patient without other known risk factors is uncommon. Not only elderly people have higher risk factors associated with acute ischemic stroke or embolization vascular events [ 15 ], but it is also true that advanced age is strongly associated with severe COVID-19 and death. The severity of the disease is directly linked to immune dysregulation, cytokine storm, and acute inflammation state, which in turn are more common in patients who present immunosenescence [6].
Inflammation plays an important role in the occurrence of cardiovascular and cerebrovascular diseases since it favors atherosclerosis and affects plaque stability [ 16 ]. The ischemic stroke of the 29-year-old woman does not appear to be imputable to emboli originating a pre-existing atheromatous plaque, both for the age of the patient and for the absence of plaques at the Doppler ultrasound study of the supra-aortic trunks.
Most likely, COVID-19-associated hypercoagulability and endothelial dysfunction are the causes of ischemic stroke, as suggested by other studies and case reports [ 10, 13, 17 ]. Although the mechanisms by which SARS-CoV-2 infection leads to hypercoagulability are still being studied, current knowledge suggests that cross talk between inflammation and thrombosis has a crucial role [ 18 ]. The release of inflammatory cytokines leads to the activation of epithelial cells, monocytes, and macrophages. Direct infection of endothelial cells through the ACE2 receptor also leads to endothelial activation and dysfunction, expression of tissue factor, and platelet activation and increased levels of VWF and FVIII, all of which contribute to thrombin generation and fibrin clot formation [ 17 ]. The 29-year-old patient showed an increased level of D-dimer, which is a degradation product of cross-linked fibrin, indicating a global activation of hemostasis and fibrinolysis and conforming to the hypothesis of COVID-19-associated hypercoagulability. Endothelial activation and hypercoagulability are also confirmed by positivity to β2 glycoprotein antibodies. Anticardiolipin antibody and/or β2 glycoprotein antibody positivity has been reported in a few studies [ 17, 19, 20 ]. In addition, widespread thrombosis in SARS-CoV-2 infection could also be caused by neutrophil extracellular traps (NETs). Neutrophilia [ 21 ] and an elevated neutrophil-lymphocyte ratio [ 22 ] have been reported by numerous studies as predictive of worse disease outcomes, and recently, the contribution of NETs in the pathophysiology of COVID-19 was reported [ 23 ]. Thrombogenic involvement of NETs has been described in various settings of thrombosis, including stroke, myocardial infarction, and deep vein thrombosis [ 24 ]. The high neutrophil count found in our case does not exclude the hypothesis that NETs are involved in the pathogenesis of ischemic stroke.
Ischemic stroke in young patients without pre-existing cerebrovascular risk factors is very unusual. In this regard, our case of an ischemic stroke, reported in a 29-year-old woman, is very interesting. Although it is not possible to determine precisely when the thromboembolic event occurred, our case of stroke during COVID-19-related pneumonia seems to confirm that COVID-19 is an independent risk factor for acute ischemic stroke. The mechanisms by which coronavirus disease leads to stroke are still under study, but it is clear that hypercoagulability and endothelial activation play a key role. Testing for SARS-CoV-2 infection should be considered for patients who develop neurologic symptoms, but it is equally important to monitor COVID-19 patients during their hospitalization to find any neurological sign or symptom in a timely manner. Our case suggests that discovering neurological deficits in sedated patients promptly can be very difficult; for this reason, sedation in mechanically ventilated patients has to be considered only if strictly necessary. Performing serial laboratory testing and waking up the patient as soon as clinical conditions allow are strategies that should be taken into account.
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the editor-in-chief of this journal.
The authors certify that there is no conflict of interest with any financial organization regarding the material discussed in the manuscript.
No funding was received for the publication of this case report.
All authors agree with the contents of the manuscript and were fully involved in the study and preparation of the manuscript. All authors read and approved the final version of the manuscript. M.A. Mimmo, M.P. Lo Muzio, M. Delli Bergoli, and L. Amoruso collected the data. C. Avvantaggiato wrote the manuscript with support of N. Cinone, L. Santoro, and C. Ciritella. C. Avvantaggiato, A. Turitto, and L. Stuppiello researched and discussed the neurophysiological principles of this study. P. Fiore and A. Santamato supervised the project.

Email alerts
Citing articles via, suggested reading.
- Online ISSN 1662-680X
INFORMATION
- Contact & Support
- Information & Downloads
- Rights & Permissions
- Terms & Conditions
- Catalogue & Pricing
- Policies & Information
- People & Organization
- Stay Up-to-Date
- Regional Offices
- Community Voice
SERVICES FOR
- Researchers
- Healthcare Professionals
- Patients & Supporters
- Health Sciences Industry
- Medical Societies
- Agents & Booksellers
Karger International
- S. Karger AG
- P.O Box, CH-4009 Basel (Switzerland)
- Allschwilerstrasse 10, CH-4055 Basel
- Tel: +41 61 306 11 11
- Fax: +41 61 306 12 34
- Contact: Front Office
- Experience Blog
- Privacy Policy
- Terms of Use
This Feature Is Available To Subscribers Only
Sign In or Create an Account
Our systems are now restored following recent technical disruption, and we’re working hard to catch up on publishing. We apologise for the inconvenience caused. Find out more: https://www.cambridge.org/universitypress/about-us/news-and-blogs/cambridge-university-press-publishing-update-following-technical-disruption
We use cookies to distinguish you from other users and to provide you with a better experience on our websites. Close this message to accept cookies or find out how to manage your cookie settings .
Login Alert
- < Back to search results
- Case Studies in Stroke
Case Studies in Stroke
Common and uncommon presentations.
- Get access Buy a print copy Check if you have access via personal or institutional login Log in Register

This Book has been cited by the following publications. This list is generated based on data provided by Crossref .
- Google Scholar
- Michael G. Hennerici , Universität Mannheim, Germany , Michael Daffertshofer , Universität Mannheim, Germany , Louis R. Caplan , Harvard University, Massachusetts , Kristina Szabo , Universität Mannheim, Germany
- 124.00 (USD) Digital access for individuals (PDF download and/or read online) Add to cart Added to cart Digital access for individuals (PDF download and/or read online) View cart
- Export citation
- Buy a print copy
Book description
Neurologists learn from their patients, and this selection of 60 stroke cases will inform and challenge clinicians at all stages in their careers. Including both common and unusual cases, the aim is to reinforce diagnostic skills through careful analysis of individual presenting patterns, and to guide treatment decisions. Each case consists of a clinical history, examination findings and special investigations, usually involving imaging before a diagnosis is given. There then follows for each case a discussion of the clinical issues raised by the case, in which the main teaching points are emphasized. Selected references, frequently including the first description, are provided at the conclusion of each case. Drawing on the expertise of leading teachers and practitioners, and liberally illustrated, these case studies and the discussions that accompany them are an essential guide to learning the complexity of stroke diagnosis.
- Aa Reduce text
- Aa Enlarge text
Refine List
Actions for selected content:.
- View selected items
- Save to my bookmarks
- Export citations
- Download PDF (zip)
- Save to Kindle
- Save to Dropbox
- Save to Google Drive
Save content to
To save content items to your account, please confirm that you agree to abide by our usage policies. If this is the first time you use this feature, you will be asked to authorise Cambridge Core to connect with your account. Find out more about saving content to .
To save content items to your Kindle, first ensure [email protected] is added to your Approved Personal Document E-mail List under your Personal Document Settings on the Manage Your Content and Devices page of your Amazon account. Then enter the ‘name’ part of your Kindle email address below. Find out more about saving to your Kindle .
Note you can select to save to either the @free.kindle.com or @kindle.com variations. ‘@free.kindle.com’ emails are free but can only be saved to your device when it is connected to wi-fi. ‘@kindle.com’ emails can be delivered even when you are not connected to wi-fi, but note that service fees apply.
Find out more about the Kindle Personal Document Service .
Save Search
You can save your searches here and later view and run them again in "My saved searches".
Page 1 of 3
- « Prev
- Next »
Frontmatter pp i-vi
- Get access Check if you have access via personal or institutional login Log in Register
Contents pp vii-ix
The following cases described herein have been published previously pp x-x, list of contributors pp xi-xi, list of abbreviations pp xii-xiv, preface pp xv-xviii, introduction pp 1-12, part i - common cases of stroke pp 13-14, case 1 - dysarthria and clumsy hand syndrome pp 15-18, case 2 - sudden numbness of the right extremities pp 19-22, case 3 - a 52-year-old woman with sudden hemiparesis pp 23-26, case 4 - sudden difficulty reading the left side of the morning paper pp 27-30, case 5 - an 85-year-old man with difficulty expressing himself on the telephone pp 31-34, case 6 - transient loss of vision pp 35-38, case 7 - massive intracerebral hemorrhage pp 39-43, case 8 - tinnitus during cycling in an orthopedic surgeon pp 44-46, case 9 - headache after an exhausting tennis match pp 47-51, case 10 - anticoagulation-associated hemorrhage pp 52-55, case 11 - worst headache of his life pp 56-59, case 12 - drooping eyelid and gait problems pp 60-64, part ii - uncommon cases of stroke pp 65-66, case 13 - similar infarction – different outcome: the importance of the brain network pp 67-70, case 14 - an 80-year-old woman with sudden paresis and normal motor latencies pp 71-74, case 15 - lower limb weakness after surgery pp 75-78, case 16 - a young engineer with suspected ms pp 79-81, case 17 - vertigo after lifting a heavy suitcase pp 82-85, case 18 - a 79-year-old man with a typical mca-stroke pp 86-89, case 19 - a man with slowly progressive weakness of the left hand pp 90-93, case 20 - sudden weakness after holidays in kenya pp 94-97, case 21 - recurrent spells of right-sided weakness pp 98-101, full text views.
Full text views reflects the number of PDF downloads, PDFs sent to Google Drive, Dropbox and Kindle and HTML full text views for chapters in this book.
Book summary page views
Book summary views reflect the number of visits to the book and chapter landing pages.
* Views captured on Cambridge Core between #date#. This data will be updated every 24 hours.
Usage data cannot currently be displayed.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
The PMC website is updating on October 15, 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.10(7); 2018 Jul

A Case Report in Hemorrhagic Stroke: A Complex Disease Process and Requirement for a Multimodal Treatment Approach
Brain d sindelar.
1 Neurosurgery, University of Florida, Gainesville, USA
Vimal Patel
2 NorthShore Neurological Institute, NorthShore University Health System/University of Chicago Pritzker School of Medicine, Chicago, USA
Shakeel Chowdhry
3 Neurosurgery, NorthShore University Health System/University of Chicago Pritzker School of Medicine, Chicago, USA
Julian E Bailes
Intracerebral hemorrhage (ICH) with or without intraventricular hemorrhage (IVH) is a highly morbid disease process due to the mass effect and secondary injury that occurs upon the surrounding brain. Historically, surgical evacuation has failed to demonstrate improved outcomes in comparison to standard medical therapy likely due to the significant brain trauma when accessing the clot. Recent minimally invasive techniques have proposed a way to improve outcomes by reducing this injury. We report here a 62-year-old male with ICH and IVH with acute neurological deterioration due to hydrocephalus was found to have no improvement following external ventricular drainage. A repeat non-contrasted computed tomography (CT) head was obtained which demonstrated the worsening mass effect from peri-hematoma edema. Surgical intervention was employed that uses a variety of techniques (endoscopic and exoscopic visualization, stereotactic trans-sulcal approach and side cutting aspiration, and intraventricular thrombolytic therapy) to reduce cerebral trauma while effectively removing both ICH and IVH. The surgical intervention reduces the mass effect and associated secondary injury, lessens the likelihood of shunt placement and length of stay, and improves long-term morbidity. We conclude that the effectiveness of surgical management of ICH could potentially be improved by employing a multifaceted approach to address the different characteristics of the hemorrhagic stroke.
Introduction
Minimally invasive surgical interventions for evacuation of intracerebral hemorrhage (ICH) and/or intraventricular hemorrhage (IVH) (in order to remove mass effect, prevent secondary injury, and potentially reduce morbidity/mortality) have demonstrated a range of published clinical outcomes, and therefore the use of one specific or any surgical modality is greatly contested. Here, we will present our management of a particular case of significant ICH with IVH with the purpose of transitioning the dialogue away from choosing a single medical or specific surgical approach to suggesting a multifaceted treatment tactic of ICH in order to reduce this devastating affliction.
Case presentation
A 62-year-old male with a history of gastroesophageal reflux and deep vein thrombosis/pulmonary embolism, developed sudden onset headache prior to his scheduled Nissen fundoplication. The patient presented to an outside hospital neurologically intact, but due to intractable symptoms, a non-contrasted head computed tomography (CT) was ordered which was significant for a right-sided caudate ICH with ventricular extension but without hydrocephalus (Figure (Figure1A) 1A ) (ICH score 1). Of note, the patient’s coagulation labs were within normal range.

A) Right caudate intracerebral hemorrhage (ICH) (17 cm 3 ) (black arrow) with ventricular extension (red arrow) but without hydrocephalus. B) Repeat CT head significant for slight increased size of ICH (21 cm 3 ) (black arrow) with greater intraventricular hemorrhage (red arrow), casting of the right lateral and third ventricles, and hydrocephalus (blue arrow).
En route to our hospital, the patient declined dramatically requiring intubation upon arrival. Repeat imaging was significant for expansion of the ICH with worsening of the IVH and associated hydrocephalus (Figure (Figure1B). The 1B ). The patient was localizing on the right upper extremity and withdrawing in the left upper extremity and bilateral lower extremities to noxious stimuli (GCS 7t, ICH score 2). An external ventricular drain (EVD) was placed and the patient was admitted to the intensive care unit (ICU). Vascular imaging was negative for underlying malformations. A repeat CT head six hours post EVD placement demonstrated a collapsed ventricle secondary to cerebrospinal fluid (CSF) drainage, but the progression of perihematoma edema and midline shift (Figure (Figure2). With 2 ). With increasing mass effect and failure of neurological improvement with CSF drainage, it was decided to take the patient to the operating room for ICH evacuation.

Increased size of the intracerebral hemorrhage (23 cm 3 ), a collapsed left lateral ventricle (red arrow) secondary to cerebrospinal fluid drainage, entrapment of the left temporal horn, and peri-hematoma edema with 6.5 mm of midline shift.
Following anesthetization, a 5 cm curvilinear right frontal incision was made behind the hairline. A 4 cm craniotomy was performed followed by identification of the posterior aspect of the right frontal superior sulcus, and then stereotactic trans-sulcal introduction of a 75 mm sheath and obturator (BrainPath, NICO Corp, Indianapolis, Indiana). Under exoscope magnification, the inferior depth of the hematoma was evacuated with gentle irrigation and suction. A small opening into the right lateral ventricle was identified, and a straight rigid endoscope was used to atraumatically enter the ventricle for further ventricular clot evacuation and irrigation. The endoscope was removed and the trans-sulcal port was slightly retracted in successive fashion to deliver more of the frontal ICH into view. With the use of suction, irrigation, and a side cutting resection device (Myriad, NICO Corp, Indianapolis, Indiana), the remainder of parenchymal hematoma was extracted. A post-operative head CT showed near complete removal of the ICH and IVH from the right lateral ventricle but with residual hematoma predominantly within the left lateral and third ventricles (Figure (Figure3 3 ).

Almost complete removal of the intracerebral hemorrhage and intraventricular hemorrhage from the right lateral ventricle but with persistent clot within the left lateral and third ventricles.
Due to the persistence of third ventricle IVH, the patient received intrathecal tPA post-operative day two (two doses, 1 mg each, nine hours apart) followed by successful weaning and removal of the ventricular drain. After three days, the patient was discharged to a long-term acute care hospital. At the three-month follow-up visit, the patient had transitioned to a skilled nursing facility. At the five-month follow-up visit, the patient was living at home, neurologically intact except for a slight facial droop and mild gait imbalance with a goal to return to work in the coming month. At each follow-up, head CT at each outpatient visit was negative for hydrocephalus.
It has been long hypothesized and studied in pre-clinical models that surgical evacuation of an intracerebral hemorrhage aids in removing both the mass effect of the primary injury along with the reduction in the secondary injury associated with clot-induced blood-brain barrier breakdown, the release of inflammatory cytokines, and the development of perihematomal edema. But, two randomized clinical trials, STITCH and STITCH 2, failed to prove this theory due to their inability to strongly demonstrate a statistically significant difference in those offered surgical evacuation through a standard craniotomy compared with medical management, even in those with superficially located lesions [ 1 ]. Lack of clinical efficacy has been suggested to be due to the overall morbidity associated with large craniotomies and the cerebral trauma required to access deep-seeded lesions.
For this reason, minimally invasive techniques have been suggested in order to reduce the morbidity associated with a craniotomy, specifically the cerebral injury when retrieving the hematoma. These approaches can be subdivided into those that use thrombolytic agents or those that use mechanical methods for ICH/IVH evacuation. The most popularized approach to targeting intracerebral hemorrhage through thrombolytic means is by stereotactically aspirating the hematoma followed by infusion of either alteplase or urokinase. A phase two clinical trial for this method called “Minimally invasive surgery plus alteplase in intracerebral hemorrhage evacuation”, MISTIE, demonstrated efficacy in reducing clot burden and perihematomal edema and a correlation between outcomes and volume of clot removed [ 2 ]. The phase three trial has completed subject enrollment but study results are pending collection of final patient follow-up assessments. A thrombolytic therapy to address IVH has been studied in the “Clot lysis evaluating accelerated resolution,” or CLEAR. This study administered 1 mg of tPA through a ventricular drain every eight hours. This technique reduced overall clot burden but showed no difference in overall outcomes in comparison to control (saline ventricular injection) [ 3 ].
Variations in mechanical means to remove deep-seeded clots vary by the type of optics used (endoscope vs exoscope), ways to gain access to the clot, and also various devices to mechanically remove the clot. Case series and retrospective reviews have demonstrated efficacy in clot removal through endoscopic means, but there is only limited evidence demonstrating superior means to standard therapy (medical management). A newer technology published, “minimally invasive subcortical parafascicular access for clot evacuation” or MISPACE, uses an imaged guided placement of a trans-sulcal port with the use of a side cutting aspirator [ 4 ]. This approach allows a small craniotomy, practically atraumatic trans-sulcal access to the clot, minimal retraction to surrounding brain, and elimination of pulling that occurs with standard suction. There is currently a randomized multicenter trial (ENRICH: Early Minimally-Invasive Removal of ICH) evaluating the effectiveness of this method but results are still pending [ 5 ].
These techniques all bring great promise to possibly improving the standard of care, but due to limited trials directly comparing each to the other and medical management, there is great controversy to their role in ICH management. Due to the multidimensional presentations (size/location of ICH, presence or absence of IVH, etc.) of those with hemorrhagic stroke, we presented this case study in order to pose that a single surgical approach may not be the answer to improving outcomes in comparison to medical management but actually a transition to a multimodal manner that combines the various mechanical and thrombolytic methods to improve visualization, intracerebral and intraventricular clot retrieval, and weaning from ventricular drainage. It appears disadvantageous to not use our arsenal of techniques to provide individualized care to the heterogeneous nature of hemorrhagic stroke. Also, as this case report emphasizes, the standard heterogeneous clinical presentation and management is far different than the homogenous subject pool with two-arm treatment approach standard in clinical trials potentially influencing and explaining the limited benefit demonstrated in previous trials.
Conclusions
The presentation of a hemorrhagic stroke is multidimensional due to the size, location, and extent of secondary pathological processes (peri-hematomal edema, ventricular hemorrhage, hydrocephalus, etc.). This case report demonstrates the typical clinical presentation of an ICH and demonstrates a multimodal approach that involves not only the standard medical therapy of intracerebral hemorrhage, but also a combination of the various minimally invasive surgical, mechanical and thrombolytic methods in order to safely access and visualize both intracerebral and intraventricular clot to improve removal with the ultimate goal to potentially improve long-term functional outcomes and reduce the requirement of shunting. Though we understand the inherent limitations to an anecdotal case report, we hope that this brings contemplation and consideration in future clinical trials.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained by all participants in this study
This presents an analysis of a case of Ischemic stroke in terms of possible etiology, pathophysiology, drug analysis and nursing care
New? Questions? Start Here!
- Information Hub
- Important Notices
- Need Access to Evidence
- Communities & Collections
- Publication Date
- Posting Date
- Subject(CINAHL)
- Item Format
- Level of Evidence
- Research Approach
- Sigma Chapters
- Author Affiliations
- Review Type
- Create an Account
Ischemic stroke: A case study
View file(s).
Author Information
- Martinez, Rudolf Cymorr Kirby P. ;
- Sigma Affiliation
Item Information
Item link - use this link for citations and online mentions..
Clinical Focus: Adult Medical/Surgical
Repository Posting Date
Type information.
| Type | | |
Category Information
| Evidence Level | ; ; |
Original Publication Info
| 2017-12-07 |
Conference Information
| Name |

Rights Holder
All rights reserved by the author(s) and/or publisher(s) listed in this item record unless relinquished in whole or part by a rights notation or a Creative Commons License present in this item record.
All permission requests should be directed accordingly and not to the Sigma Repository.
All submitting authors or publishers have affirmed that when using material in their work where they do not own copyright, they have obtained permission of the copyright holder prior to submission and the rights holder has been acknowledged as necessary.
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Global health
- BMJ Journals
You are here
- Volume 13, Issue 8
- Clinical course of a 66-year-old man with an acute ischaemic stroke in the setting of a COVID-19 infection
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0002-7441-6952 Saajan Basi 1 , 2 ,
- Mohammad Hamdan 1 and
- Shuja Punekar 1
- 1 Department of Stroke and Acute Medicine , King's Mill Hospital , Sutton-in-Ashfield , UK
- 2 Department of Acute Medicine , University Hospitals of Derby and Burton , Derby , UK
- Correspondence to Dr Saajan Basi; saajan.basi{at}nhs.net
A 66-year-old man was admitted to hospital with a right frontal cerebral infarct producing left-sided weakness and a deterioration in his speech pattern. The cerebral infarct was confirmed with CT imaging. The only evidence of respiratory symptoms on admission was a 2 L oxygen requirement, maintaining oxygen saturations between 88% and 92%. In a matter of hours this patient developed a greater oxygen requirement, alongside reduced levels of consciousness. A positive COVID-19 throat swab, in addition to bilateral pneumonia on chest X-ray and lymphopaenia in his blood tests, confirmed a diagnosis of COVID-19 pneumonia. A proactive decision was made involving the patients’ family, ward and intensive care healthcare staff, to not escalate care above a ward-based ceiling of care. The patient died 5 days following admission under the palliative care provided by the medical team.
- respiratory medicine
- infectious diseases
- global health
This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
https://doi.org/10.1136/bcr-2020-235920
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
SARS-CoV-2 (Severe Acute Respiratory Syndrome Coronavirus 2) is a new strain of coronavirus that is thought to have originated in December 2019 in Wuhan, China. In a matter of months, it has erupted from non-existence to perhaps the greatest challenge to healthcare in modern times, grinding most societies globally to a sudden halt. Consequently, the study and research into SARS-CoV-2 is invaluable. Although coronaviruses are common, SARS-CoV-2 appears to be considerably more contagious. The WHO figures into the 2003 SARS-CoV-1 outbreak, from November 2002 to July 2003, indicate a total of 8439 confirmed cases globally. 1 In comparison, during a period of 4 months from December 2019 to July 2020, the number of global cases of COVID-19 reached 10 357 662, increasing exponentially, illustrating how much more contagious SARS-CoV-2 has been. 2
Previous literature has indicated infections, and influenza-like illness have been associated with an overall increase in the odds of stroke development. 3 There appears to be a growing correlation between COVID-19 positive patients presenting to hospital with ischaemic stroke; however, studies investigating this are in progress, with new data emerging daily. This patient report comments on and further characterises the link between COVID-19 pneumonia and the development of ischaemic stroke. At the time of this patients’ admission, there were 95 positive cases from 604 COVID-19 tests conducted in the local community, with a predicted population of 108 000. 4 Only 4 days later, when this patient died, the figure increased to 172 positive cases (81% increase), illustrating the rapid escalation towards the peak of the pandemic, and widespread transmission within the local community ( figure 1 ). As more cases of ischaemic stroke in COVID-19 pneumonia patients arise, the recognition and understanding of its presentation and aetiology can be deciphered. Considering the virulence of SARS-CoV-2 it is crucial as a global healthcare community, we develop this understanding, in order to intervene and reduce significant morbidity and mortality in stroke patients.
- Download figure
- Open in new tab
- Download powerpoint
A graph showing the number of patients with COVID-19 in the hospital and in the community over time.
Case presentation
A 66-year-old man presented to the hospital with signs of left-sided weakness. The patient had a background of chronic obstructive pulmonary disease (COPD), atrial fibrillation and had one previous ischaemic stroke, producing left-sided haemiparesis, which had completely resolved. He was a non-smoker and lived in a house. The patient was found slumped over on the sofa at home on 1 April 2020, by a relative at approximately 01:00, having been seen to have no acute medical illness at 22:00. The patients’ relative initially described disorientation and agitation with weakness noted in the left upper limb and dysarthria. At the time of presentation, neither the patient nor his relative identified any history of fever, cough, shortness of breath, loss of taste, smell or any other symptoms; however, the patient did have a prior admission 9 days earlier with shortness of breath.
The vague nature of symptoms, entwined with considerable concern over approaching the hospital, due to the risk of contracting COVID-19, created a delay in the patients’ attendance to the accident and emergency department. His primary survey conducted at 09:20 on 1 April 2020 demonstrated a patent airway, with spontaneous breathing and good perfusion. His Glasgow Coma Scale (GCS) score was 15 (a score of 15 is the highest level of consciousness), his blood glucose was 7.2, and he did not exhibit any signs of trauma. His abbreviated mental test score was 7 out of 10, indicating a degree of altered cognition. An ECG demonstrated atrial fibrillation with a normal heart rate. His admission weight measured 107 kg. At 09:57 the patient required 2 L of nasal cannula oxygen to maintain his oxygen saturations between 88% and 92%. He started to develop agitation associated with an increased respiratory rate at 36 breaths per minute. On auscultation of his chest, he demonstrated widespread coarse crepitation and bilateral wheeze. Throughout he was haemodynamically stable, with a systolic blood pressure between 143 mm Hg and 144 mm Hg and heart rate between 86 beats/min and 95 beats/min. From a neurological standpoint, he had a mild left facial droop, 2/5 power in both lower limbs, 2/5 power in his left upper limb and 5/5 power in his right upper limb. Tone in his left upper limb had increased. This patient was suspected of having COVID-19 pneumonia alongside an ischaemic stroke.
Investigations
A CT of his brain conducted at 11:38 on 1 April 2020 ( figure 2 ) illustrated an ill-defined hypodensity in the right frontal lobe medially, with sulcal effacement and loss of grey-white matter. This was highly likely to represent acute anterior cerebral artery territory infarction. Furthermore an oval low-density area in the right cerebellar hemisphere, that was also suspicious of an acute infarction. These vascular territories did not entirely correlate with his clinical picture, as limb weakness is not as prominent in anterior cerebral artery territory ischaemia. Therefore this left-sided weakness may have been an amalgamation of residual weakness from his previous stroke, in addition to his acute cerebral infarction. An erect AP chest X-ray with portable equipment ( figure 3 ) conducted on the same day demonstrated patchy peripheral consolidation bilaterally, with no evidence of significant pleural effusion. The pattern of lung involvement raised suspicion of COVID-19 infection, which at this stage was thought to have provoked the acute cerebral infarct. Clinically significant blood results from 1 April 2020 demonstrated a raised C-reactive protein (CRP) at 215 mg/L (normal 0–5 mg/L) and lymphopaenia at 0.5×10 9 (normal 1×10 9 to 3×10 9 ). Other routine blood results are provided in table 1 .
CT imaging of this patients’ brain demonstrating a wedge-shaped infarction of the anterior cerebral artery territory.
Chest X-ray demonstrating the bilateral COVID-19 pneumonia of this patient on admission.
- View inline
Clinical biochemistry and haematology blood results of the patient
Interestingly the patient, in this case, was clinically assessed in the accident and emergency department on 23 March 2020, 9 days prior to admission, with symptoms of shortness of breath. His blood results from this day showed a CRP of 22 mg/L and a greater lymphopaenia at 0.3×10 9 . He had a chest X-ray ( figure 4 ), which indicated mild radiopacification in the left mid zone. He was initially treated with intravenous co-amoxiclav and ciprofloxacin. The following day he had minimal symptoms (CURB 65 score 1 for being over 65 years). Given improving blood results (declining CRP), he was discharged home with a course of oral amoxicillin and clarithromycin. As national governmental restrictions due to COVID-19 had not been formally announced until 23 March 2020, and inconsistencies regarding personal protective equipment training and usage existed during the earlier stages of this rapidly evolving pandemic, it is possible that this patient contracted COVID-19 within the local community, or during his prior hospital admission. It could be argued that the patient had early COVID-19 signs and symptoms, having presented with shortness of breath, lymphopaenia, and having had subtle infective chest X-ray changes. The patient explained he developed a stagnant productive cough, which began 5 days prior to his attendance to hospital on 23 March 2020. He responded to antibiotics, making a full recovery following 7 days of treatment. This information does not assimilate with the typical features of a COVID-19 infection. A diagnosis of community-acquired pneumonia or infective exacerbation of COPD seem more likely. However, given the high incidence of COVID-19 infections during this patients’ illness, an exposure and early COVID-19 illness, prior to the 23 March 2020, cannot be completely ruled out.
Chest X-ray conducted on prior admission illustrating mild radiopacification in the left mid zone.
On the current admission, this patient was managed with nasal cannula oxygen at 2 L. By the end of the day, this had progressed to a venturi mask, requiring 8 L of oxygen to maintain oxygen saturation. He had also become increasingly drowsy and confused, his GCS declined from 15 to 12. However, the patient was still haemodynamically stable, as he had been in the morning. An arterial blood gas demonstrated a respiratory alkalosis (pH 7.55, pCO 2 3.1, pO 2 6.7 and HCO 3 24.9, lactate 1.8, base excess 0.5). He was commenced on intravenous co-amoxiclav and ciprofloxacin, to treat a potential exacerbation of COPD. This patient had a COVID-19 throat swab on 1 April 2020. Before the result of this swab, an early discussion was held with the intensive care unit staff, who decided at 17:00 on 1 April 2020 that given the patients presentation, rapid deterioration, comorbidities and likely COVID-19 diagnosis he would not be for escalation to the intensive care unit, and if he were to deteriorate further the end of life pathway would be most appropriate. The discussion was reiterated to the patients’ family, who were in agreement with this. Although he had evidence of an ischaemic stroke on CT of his brain, it was agreed by all clinicians that intervention for this was not as much of a priority as providing optimal palliative care, therefore, a minimally invasive method of treatment was advocated by the stroke team. The patient was given 300 mg of aspirin and was not a candidate for fibrinolysis.
Outcome and follow-up
The following day, before the throat swab result, had appeared the patient deteriorated further, requiring 15 L of oxygen through a non-rebreather face mask at 60% FiO 2 to maintain his oxygen saturation, at a maximum of 88% overnight. At this point, he was unresponsive to voice, with a GCS of 5. Although, he was still haemodynamically stable, with a blood pressure of 126/74 mm Hg and a heart rate of 98 beats/min. His respiratory rate was 30 breaths/min. His worsening respiratory condition, combined with his declining level of consciousness made it impossible to clinically assess progression of the neurological deficit generated by his cerebral infarction. Moreover, the patient was declining sharply while receiving the maximal ward-based treatment available. The senior respiratory physician overseeing the patients’ care decided that a palliative approach was in this his best interest, which was agreed on by all parties. The respiratory team completed the ‘recognising dying’ documentation, which signified that priorities of care had shifted from curative treatment to palliative care. Although the palliative team was not formally involved in the care of the patient, the patient received comfort measures without further attempts at supporting oxygenation, or conduction of regular clinical observations. The COVID-19 throat swab confirmed a positive result on 2 April 2020. The patient was treated by the medical team under jurisdiction of the hospital palliative care team. This included the prescribing of anticipatory medications and a syringe driver, which was established on 3 April 2020. His antibiotic treatment, non-essential medication and intravenous fluid treatment were discontinued. His comatose condition persisted throughout the admission. Once the patients’ GCS was 5, it did not improve. The patient was pronounced dead by doctors at 08:40 on 5 April 2020.
SARS-CoV-2 is a type of coronavirus that was first reported to have caused pneumonia-like infection in humans on 3 December 2019. 5 As a group, coronaviruses are a common cause of upper and lower respiratory tract infections (especially in children) and have been researched extensively since they were first characterised in the 1960s. 6 To date, there are seven coronaviruses that are known to cause infection in humans, including SARS-CoV-1, the first known zoonotic coronavirus outbreak in November 2002. 7 Coronavirus infections pass through communities during the winter months, causing small outbreaks in local communities, that do not cause significant mortality or morbidity.
SARS-CoV-2 strain of coronavirus is classed as a zoonotic coronavirus, meaning the virus pathogen is transmitted from non-humans to cause disease in humans. However the rapid spread of SARS-CoV-2 indicates human to human transmission is present. From previous research on the transmission of coronaviruses and that of SARS-CoV-2 it can be inferred that SARS-CoV-2 spreads via respiratory droplets, either from direct inhalation, or indirectly touching surfaces with the virus and exposing the eyes, nose or mouth. 8 Common signs and symptoms of the COVID-19 infection identified in patients include high fevers, severe fatigue, dry cough, acute breathing difficulties, bilateral pneumonia on radiological imaging and lymphopaenia. 9 Most of these features were identified in this case study. The significance of COVID-19 is illustrated by the speed of its global spread and the potential to cause severe clinical presentations, which as of April 2020 can only be treated symptomatically. In Italy, as of mid-March 2020, it was reported that 12% of the entire COVID-19 positive population and 16% of all hospitalised patients had an admission to the intensive care unit. 10
The patient, in this case, illustrates the clinical relevance of understanding COVID-19, as he presented with an ischaemic stroke underlined by minimal respiratory symptoms, which progressed expeditiously, resulting in acute respiratory distress syndrome and subsequent death.
Our case is an example of a new and ever-evolving clinical correlation, between patients who present with a radiological confirmed ischaemic stroke and severe COVID-19 pneumonia. As of April 2020, no comprehensive data of the relationship between ischaemic stroke and COVID-19 has been published, however early retrospective case series from three hospitals in Wuhan, China have indicated that up to 36% of COVID-19 patients had neurological manifestations, including stroke. 11 These studies have not yet undergone peer review, but they tell us a great deal about the relationship between COVID-19 and ischaemic stroke, and have been used to influence the American Heart Associations ‘Temporary Emergency Guidance to US Stroke Centres During the COVID-19 Pandemic’. 12
The relationship between similar coronaviruses and other viruses, such as influenza in the development of ischaemic stroke has previously been researched and provide a basis for further investigation, into the prominence of COVID-19 and its relation to ischaemic stroke. 3 Studies of SARS-CoV-2 indicate its receptor-binding region for entry into the host cell is the same as ACE2, which is present on endothelial cells throughout the body. It may be the case that SARS-CoV-2 alters the conventional ability of ACE2 to protect endothelial function in blood vessels, promoting atherosclerotic plaque displacement by producing an inflammatory response, thus increasing the risk of ischaemic stroke development. 13
Other hypothesised reasons for stroke development in COVID-19 patients are the development of hypercoagulability, as a result of critical illness or new onset of arrhythmias, caused by severe infection. Some case studies in Wuhan described immense inflammatory responses to COVID-19, including elevated acute phase reactants, such as CRP and D-dimer. Raised D-dimers are a non-specific marker of a prothrombotic state and have been associated with greater morbidity and mortality relating to stroke and other neurological features. 14
Arrhythmias such as atrial fibrillation had been identified in 17% of 138 COVID-19 patients, in a study conducted in Wuhan, China. 15 In this report, the patient was known to have atrial fibrillation and was treated with rivaroxaban. The acute inflammatory state COVID-19 is known to produce had the potential to create a prothrombotic environment, culminating in an ischaemic stroke.
Some early case studies produced in Wuhan describe patients in the sixth decade of life that had not been previously noted to have antiphospholipid antibodies, contain the antibodies in blood results. They are antibodies signify antiphospholipid syndrome; a prothrombotic condition. 16 This raises the hypothesis concerning the ability of COVID-19 to evoke the creation of these antibodies and potentiate thrombotic events, such as ischaemic stroke.
No peer-reviewed studies on the effects of COVID-19 and mechanism of stroke are published as of April 2020; therefore, it is difficult to evidence a specific reason as to why COVID-19 patients are developing neurological signs. It is suspected that a mixture of the factors mentioned above influence the development of ischaemic stroke.
If we delve further into this patients’ comorbid state exclusive to COVID-19 infection, it can be argued that this patient was already at a relatively higher risk of stroke development compared with the general population. The fact this patient had previously had an ischaemic stroke illustrates a prior susceptibility. This patient had a known background of hypertension and atrial fibrillation, which as mentioned previously, can influence blood clot or plaque propagation in the development of an acute ischaemic event. 15 Although the patient was prescribed rivaroxaban as an anticoagulant, true consistent compliance to rivaroxaban or other medications such as amlodipine, clopidogrel, candesartan and atorvastatin cannot be confirmed; all of which can contribute to the reduction of influential factors in the development of ischaemic stroke. Furthermore, the fear of contracting COVID-19, in addition to his vague symptoms, unlike his prior ischaemic stroke, which demonstrated dense left-sided haemiparesis, led to a delay in presentation to hospital. This made treatment options like fibrinolysis unachievable, although it can be argued that if he was already infected with COVID-19, he would have still developed life-threatening COVID-19 pneumonia, regardless of whether he underwent fibrinolysis. It is therefore important to consider that if this patient did not contract COVID-19 pneumonia, he still had many risk factors that made him prone to ischaemic stroke formation. Thus, we must consider whether similar patients would suffer from ischaemic stroke, regardless of COVID-19 infection and whether COVID-19 impacts on the severity of the stroke as an entity.
Having said this, the management of these patients is dependent on the likelihood of a positive outcome from the COVID-19 infection. Establishing the ceiling of care is crucial, as it prevents incredibly unwell or unfit patients’ from going through futile treatments, ensuring respect and dignity in death, if this is the likely outcome. It also allows for the provision of limited or intensive resources, such as intensive care beds or endotracheal intubation during the COVID-19 pandemic, to those who are assessed by the multidisciplinary team to benefit the most from their use. The way to establish this ceiling of care is through an early multidisciplinary discussion. In this case, the patient did not convey his wishes regarding his care to the medical team or his family; therefore it was decided among intensive care specialists, respiratory physicians, stroke physicians and the patients’ relatives. The patient was discussed with the intensive care team, who decided that as the patient sustained two acute life-threatening illnesses simultaneously and had rapidly deteriorated, ward-based care with a view to palliate if the further deterioration was in the patients’ best interests. These decisions were not easy to make, especially as it was on the first day of presentation. This decision was made in the context of the patients’ comorbidities, including COPD, the patients’ age, and the availability of intensive care beds during the steep rise in intensive care admissions, in the midst of the COVID-19 pandemic ( figure 1 ). Furthermore, the patients’ rapid and permanent decline in GCS, entwined with the severe stroke on CT imaging of the brain made it more unlikely that significant and permanent recovery could be achieved from mechanical intubation, especially as the damage caused by the stroke could not be significantly reversed. As hospitals manage patients with COVID-19 in many parts of the world, there may be tension between the need to provide higher levels of care for an individual patient and the need to preserve finite resources to maximise the benefits for most patients. This patient presented during a steep rise in intensive care admissions, which may have influenced the early decision not to treat the patient in an intensive care setting. Retrospective studies from Wuhan investigating mortality in patients with multiple organ failure, in the setting of COVID-19, requiring intubation have demonstrated mortality can be up to 61.5%. 17 The mortality risk is even higher in those over 65 years of age with respiratory comorbidities, indicating why this patient was unlikely to survive an admission to the intensive care unit. 18
Regularly updating the patients’ family ensured cooperation, empathy and sympathy. The patients’ stroke was not seen as a priority given the severity of his COVID-19 pneumonia, therefore the least invasive, but most appropriate treatment was provided for his stroke. The British Association of Stroke Physicians advocate this approach and also request the notification to their organisation of COVID-19-related stroke cases, in the UK. 19
Learning points
SARS-CoV-2 (Severe Acute Respiratory Syndrome Coronavirus 2) is one of seven known coronaviruses that commonly cause upper and lower respiratory tract infections. It is the cause of the 2019–2020 global coronavirus pandemic.
The significance of COVID-19 is illustrated by the rapid speed of its spread globally and the potential to cause severe clinical presentations, such as ischaemic stroke.
Early retrospective data has indicated that up to 36% of COVID-19 patients had neurological manifestations, including stroke.
Potential mechanisms behind stroke in COVID-19 patients include a plethora of hypercoagulability secondary to critical illness and systemic inflammation, the development of arrhythmia, alteration to the vascular endothelium resulting in atherosclerotic plaque displacement and dehydration.
It is vital that effective, open communication between the multidisciplinary team, patient and patients relatives is conducted early in order to firmly establish the most appropriate ceiling of care for the patient.
- Cannine M , et al
- Wunderink RG
- van Doremalen N ,
- Bushmaker T ,
- Morris DH , et al
- Wang X-G , et al
- Grasselli G ,
- Pesenti A ,
- Wang M , et al
- American Stroke Assocation, 2020
- Zhang Y-H ,
- Zhang Y-huan ,
- Dong X-F , et al
- Li X , et al
- Hu C , et al
- Zhang S , et al
- Jiang B , et al
- Xu J , et al
- British Association of Stroke Physicians
Contributors SB was involved in the collecting of information for the case, the initial written draft of the case and researching existing data on acute stroke and COVID-19. He also edited drafts of the report. MH was involved in reviewing and editing drafts of the report and contributing new data. SP oversaw the conduction of the project and contributed addition research papers.
Funding The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests None declared.
Patient consent for publication Next of kin consent obtained.
Provenance and peer review Not commissioned; externally peer reviewed.
Read the full text or download the PDF:
Ohio State nav bar
The Ohio State University
- BuckeyeLink
- Find People
- Search Ohio State
Pathophysiology and clinical presentation
(DiGiovanna, A. G; 1999)
Cerebrovascular accidents, also known as strokes, happen when the blood supply becomes occluded in part of the brain. They can be classified as either ischemic, hemorrhagic, or cryptogenic. In ischemic strokes blood supply can be occluded for three different reasons, a vascular occlusion by either an embolus or thrombi, a gradual vessel occlusion, or a stenosed vessel (McCance & Huether, 2019). In ischemic strokes or cerebral infarctions, the arterial blood flow that leads to the brain is obstructed and can be classified as ischemic infarcts or hemorrhagic infarcts. This can be from transient ischemic attacks, thrombotic strokes, embolic strokes, lacunar strokes or hemodynamic strokes. In an ischemic infarct, the area that is affected becomes pale, soft, and swollen. This eventually leads to necrosis of the brain tissue which creates a cavity that is surrounded by glial scarring (McCance & Huether, 2019). If an occlusion of a cerebral artery occurs, branches of connecting arteries can partially maintain blood supply to prevent cell death (McCance & Huether, 2019). In hemorrhagic infarcts leaking vessels create a bleed when fragments from an emboli resolve and reperfusion starts (McCance & Huether, 2019).
There are many different types of ischemic strokes that can occur in the human body. Transient ischemic attacks are dysfunctions in the brain that cause ischemia for about one hour. Transient ischemic attacks can eventually lead to a stroke within 90 days if not fixed. Individuals experiencing a TIA may have weakness, numbness, loss of vision or balance, a severe headache, or confusion (McCance & Huether, 2019). In thrombotic strokes a thrombus is formed inside the vessels that feed the brain or intracranial vessels and a part of that clot detaches, travels up to the brain, occludes blood flow, and causes ischemia (McCance & Huether, 2019). Embolic strokes start in the outside of the brain, either in the heart, aorta, or common carotid artery where a thrombus is formed. Parts of that thrombus breaks off and causes an obstruction usually in small brain vessels causing ischemia (McCance & Huether, 2019). In embolic strokes the embolus can completely occlude the vessels or have pieces that remain in vessels which can lead to a second stroke because the embolus is still there (McCance & Huether, 2019). In lacunar strokes there is edema or inflammation to the wall of an artery and leads to ischemia. They mostly occur in the basal ganglia, internal capsules or the pons. Lastly, in hemodynamic strokes there is inadequate blood supply to the brain caused by either cardiac failure, pulmonary embolism or bleeding (McCance & Huether, 2019).
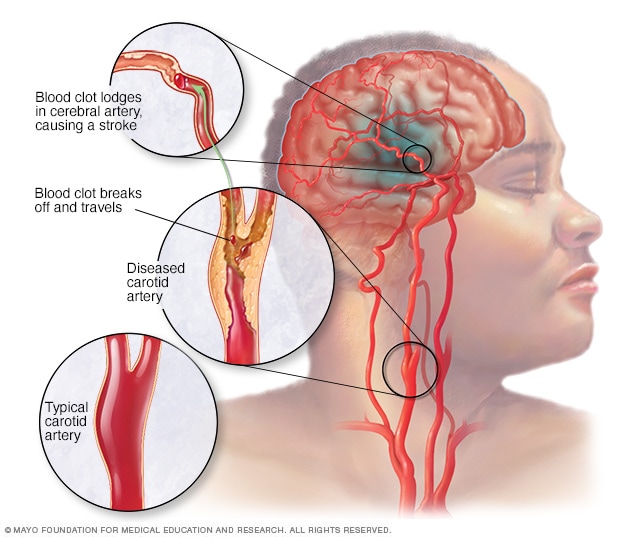
(https://www.mayoclinic.org/diseases-conditions/stroke/symptoms-causes/syc-20350113)
In a hemorrhagic stroke or spontaneous intracranial hemorrhage, bleeding happens in the brain tissue causing a mass of blood due to leaky vessels or bursting aneurysm (McCance & Huether, 2019). In both ischemic and hemorrhagic strokes, the decrease in blood supply causes ischemia which can eventually cause death of the tissue or infarction. There are two types of hemorrhages that can occur from a hemorrhagic stroke, subarachnoid hemorrhage and intracerebral hemorrhage. Subarachnoid is a bleed that occurs between the brain and the dura while an intercerebral bleed occurs actually in the brain parenchyma. Brain tissue that is near the bleed can start to become compressed and can be displaced causing ischemia, edema, increased intracranial pressure, and necrosis (McCance & Huether, 2019). Hemorrhagic strokes can range in all different sizes which can determine how much edema and necrosis there will be. They can be classified as massive, small, slit, or petechial (McCance & Huether, 2019). In a massive cerebral hemorrhage, there will be a significant amount of edema which can lead to death.
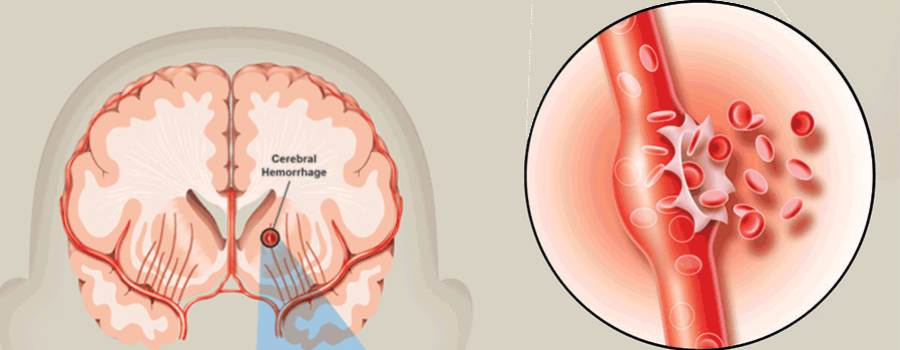
Symptoms of a stroke happen fast and can range from mild to severe depending on how large the stroke is and what kind of stroke the person is experiencing. In a thrombotic or embolic ischemic stroke, the symptoms a person may experience varies depending on what artery in the vein is involved (McCance & Huether, 2019). A person may loose sensory and motor function on the opposite side of where the stroke happened in the brain making it contralateral or on the same side as the stroke making it ipsilateral. In a hemorrhagic stroke a person may experience a horrible headache that leads to unresponsiveness, a headache but a person remains conscious or a person can immediately become unconscious. They can also have numbness and tingling, speech issues, weakness or paralysis. In some cases, if the hemorrhage is just in the subarachnoid space, a person may not experience any symptoms at all (McCance & Huether, 2019).
Upon observations of possible symptoms or clinical manifestations of a stroke, as detailed throughout this website, imaging tests are used to identify and diagnose. The key criteria for diagnosis are a CT of the head and MRI of the brain. These tests can confirm if there is a stroke, and determine what type of stroke so the practitioner can appropriately treat the individual (McCance & Huether, 2019).
- Systematic Review
- Open access
- Published: 18 September 2024
Systematic review and meta-analysis of stroke and thromboembolism risk in atrial fibrillation with preserved vs. reduced ejection fraction heart failure
- Meijuan Zhang 1 &
- Jie Zhou 1
BMC Cardiovascular Disorders volume 24 , Article number: 495 ( 2024 ) Cite this article
Metrics details
Stroke and thromboembolism (TE) are significant complications in patients with atrial fibrillation (AF) and heart failure (HF). The impact of ejection fraction status on these risks remains unclear. This study aims to compare the risk of stroke and TE in patients with AF and HF with preserved (HFpEF) or reduced (HFrEF) ejection fraction.
Literature search of PubMed, Embase, and Scopus databases was done for studies in adult (20 years or more) population of AF patients. Included studies had reported on the incidences of stroke and/or TE in patients with AF and associated HF with reduced ejection fraction (HFrEF) and preserved ejection fraction (HFpEF). Cohort (prospective and retrospective), case-control studies, and studies that were based on secondary analysis of data from a trial were eligible for inclusion. Methodological quality was assessed using the Newcastle Ottawa Scale (NOS). Pooled hazard ratio (HR) with 95% confidence intervals (CI) were reported. Exploratory analysis was conducted based on the different cut-offs used to define HFrEF and HFpEF.
Twenty studies were analyzed. In the overall analysis, HFrEF in AF patients was associated with a significantly reduced risk of stroke and systemic TE (HR 0.88, 95% CI: 0.81, 0.96; n = 20, I2 = 86.6%), compared to HFpEF. However, most studies showed comparable risk of stroke among the two groups of patients except for two studies that had documented significantly reduced risk. Upon doing the sensitivity analysis by excluding these two studies, we found similar risk among the two group of subjects and with no heterogeneity (HR 1.01, 95% CI: 0.99, 1.03; n = 18, I2 = 0.0%). Exploratory analysis also showed that the risk of stroke and systemic thromboembolism was similar between those with HFpEF and HFrEF.
The findings suggest that there is no significantly different risk of stroke and systemic thromboembolism in cases of AF with associated HFpEF or HFrEF. The finding does not support integration of left ventricular ejection fraction into stroke risk assessments.
Peer Review reports
Introduction
Atrial fibrillation (AF) is connected to a higher incidence of stroke and systemic thromboembolism (TE) [ 1 , 2 ]. This risk is particularly significant if accompanied by heart failure (HF) [ 3 , 4 ], which is recognized as a risk factor for stroke and systemic TE [ 5 , 6 ]. Echocardiographic parameters allow to stratify HF into two distinct categories based on left ventricular ejection fraction (LVEF): HF with preserved and reduced ejection fraction (HFpEF and HFrEF, respectively) [ 7 , 8 ]. HFrEF is characterized by impaired pumping capability of the heart, which exacerbates blood stasis, and increases the risk of thrombus formation [ 9 ]. HFpEF is defined as HF despite preserved LVEF(≥ 50%), with elevated natriuretic peptides, and impaired blood flow dynamics [ 10 ]. Given the increasing prevalence of AF and HF and their intricate relationship, it becomes imperative to understand nuanced aspects of their association with the risk of stroke and TE [ 11 ].
A prior systematic review that was published in 2015 and included seven studies, investigated cardiovascular outcomes among patients with AF and HFrEF, as opposed to HFpEF [ 12 ], and revealed that HFrEF correlated with a marked increase in all-cause mortality (Risk ratio, RR 1.24; N = 10). However, there were no differences in the rates of stroke. During the following half-decade, additional studies have been conducted on this particular aspect, but no recent comprehensive updated meta-analysis attempted to summarize most current data.
This meta-analysis aims to bridge this gap by systematically reviewing and quantitatively synthesizing the available literature to compare the risk of stroke and thromboembolism in AF patients with HFpEF or HFrEF.
Materials and methods
Study protocol.
The protocol of the review was preregistered in PROSPERO ( https://www.crd.york.ac.uk/prospero/ ) under the registration number (CRD42024505106). The meta-analysis followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [ 13 ].
Literature search
Electronic searched were done in PubMed, Embase, and Scopus databases to identify relevant studies, published until 31st December 2023 using a combination of key terms: (Atrial fibrillation OR atrial flutter OR tachycardia) AND (heart failure OR cardiac failure OR cardiac disease) AND (preserved ejection fraction OR reduced ejection fraction OR ejection fraction OR cardiac output) AND (complications OR thromboembolism OR stroke OR cerebrovascular accident). Manual search of reference lists and review articles was also conducted.
We understand that including “atrial flutter” as a keyword was not strictly necessary. We decided to incorporate it to broaden our search and increase the number of potential studies identified. Our goal was to ensure a comprehensive review and reduce the risk of overlooking important studies that could contribute valuable data. Additionally, while not a primary reason, some studies might include results for combined cohorts of atrial fibrillation and atrial flutter patients, and we thought that this keyword may help us identify such studies as well.
Eligibility criteria
This meta-analysis included studies that involved adult populations (aged 20 years or more) diagnosed with AF and concurrent HF where ejection fraction data (preserved or reduced) was documented. We included cohort studies (both prospective and retrospective), case-control studies, and studies that were based on secondary analysis of trial records. The primary outcomes of interest were risk of stroke and systemic thromboembolism in AF patients with associated HF, with a specific focus on the stratification of outcomes by ejection fraction status (HFpEF or HFrEF). Peer-reviewed English-language articles published until 31st December 2023 were considered. We excluded studies involving paediatric patients or patients without a clear diagnosis of AF and/or HR. Review articles, editorials, letters, commentaries, and studies lacking original data, such as case reports, were also excluded. Additionally, non-peer-reviewed sources, such as conference posters, as well as studies with unclear reporting of outcomes or insufficient data were excluded.
Selection of studies for inclusion
Data deduplication was done for the studies identified through the preliminary literature search. Two study authors comprehensively screened titles and abstracts of remaining studies. Full texts of studies that met the initial criteria underwent a detailed evaluation to determine eligibility for inclusion. All discrepancies or disagreements were resolved by discussions.
Quality assessment of the studies
The Newcastle-Ottawa Scale (NOS) was employed for the standardized quality assessment of the selected studies [ 14 ]. The assessment is made based on study groups selection, intergroup comparability, and ascertainment of outcomes, with a maximum achievable value of 9. Higher scores indicate better quality [ 14 ].
Data extraction
Relevant data were extracted and included study authors, publication year, study location, design, subject characteristics, duration of follow-up, type of AF in the included patients, cut-off for ejection fraction used to define HFpEF and HFrEF, sample size, and key findings. Any disagreements were resolved by discussions.
Statistical analysis
Pooled effect sizes were reported as hazard ratios (HR) with 95% confidence intervals (CI). For all the statistical comparisons, HFpEF served as the reference. Subgroup analyses were conducted according to study design, type of AF, duration of follow up and sample size. The random-effects model was employed for all analysis to account for differences in participant characteristics and methodological variations among the included studies. The Cochrane I 2 > 40% indicated significant heterogeneity [ 15 ]. Publication bias was assessed by funnel plot and Egger’s test [ 16 ]. A P < 0.05 on Egger’s test indicated presence of publication bias and this was supported by visual inspection of funnel plot. All analysis were conducted using STATA software version 15.0. We evaluated the certainty of the evidence using the standard GRADE approach and GRADE Pro software [ 17 ].
Literature search across databases identified 1714 studies. After deduplication, 1226 distinct studies remained. After subsequent evaluation of titles and abstracts, full texts of 51 relevant articles were screened, and additional 31 studies were eliminated. Finally, a total of 20 studies were included (Fig. 1 ) [ 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 ].

Process of selecting studies for inclusion
As summarized in Table 1 , there were eight studies with a retrospective and seven studies with a prospective cohort design. Remaining five studies were based on secondary analysis of data collected as part of randomized clinical trial. Most studies were conducted in the USA ( n = 7). Three studies were conducted in the Republic of Korea and one study each in Russia, Poland, Japan, Sweden, Canada, and France. Four studies were multicenter. In almost all studies, HFpEF correlated with older age and higher proportion of female gender, compared to HFrEF patients. There were differences in the cut-off values used for defining reduced or preserved ejection fraction (EF) among the included studies. Majority of the studies defined HFrEF as EF < 50% and HFpEF as ≥ 50% ( N = 8) followed by 7 studies that defined HFrEF as EF < 40% and HFpEF as ≥ 50%. This highlights a grey zone for EF between 40 and 50% that should be addressed. Only 11 studies reported on the type of AF. Out of them, eight had predominantly patients with permanent or persistent AF, two had patients with paroxysmal AF and in one study, the equal proportion of patients had either permanent/persistent or paroxysmal AF. We also reported available data from the included studies on CHA2DS2-VASc or CHADS2 score as well as NT-ProBNP or BNP level (Table 1 ). The data suggests that those with reduced ejection fraction had comparatively lower CHA2DS2-VASc/CHADS2 score and higher NT-ProBNP/ BNP level compared to those with preserved ejection fraction.
Most studies had a follow up period of more than one year ( n = 15). The follow up period in these studies ranged from 15 months to 5 years. The included studies contributed to a total of 1,73,876 subjects. The mean NOS quality score of the studies was 7.5. There were 10 studies with a score of 8 and 10 studies with a score of 7 (Supplementary Tables 1 and 2 ). Overall, quality assessment results indicate that the included studies were of acceptable methodological quality.
Risk of stroke and systemic thromboembolism
HFrEF patients had lower risk of stroke and systemic thromboembolism (HR 0.88, 95% CI: 0.81, 0.96; n = 20, I2 = 86.6%) compared to AF patients with HFpEF (Fig. 2 ), with no obvious publication bias (Egger’s p-value = 0.120) (Supplementary Fig. 1 ). However, most studies showed comparable risk of stroke among HFrEF and HFpEF patients except for the publication from Uhm et al. and Chung et al. Upon doing the sensitivity analysis by excluding these two studies, we found similar risk among the two group of subjects and with no heterogeneity (HR 1.01, 95% CI: 0.99, 1.03; n = 18, I2 = 0.0%) (Egger’s p-value = 0.341) (Supplementary Fig. 2 ).

Risk of stroke and systemic thromboembolism among subjects with atrial fibrillation and associated reduced ejection fraction (HFrEF), compared to patients with preserved ejection fraction (HFpEF)
Subgroup analysis showed that the reduced risk of stroke and thromboembolism in HFrEF was only evident in prospective cohort studies (HR 0.74, 95% CI: 0.58, 0.94; n = 7, I2 = 95.4%), studies with longer follow up (> 1 year) (HR 0.86, 95% CI: 0.77, 0.95; n = 15, I2 = 90.0%) and studies with larger sample size (≥ 500) (HR 0.85, 95% CI: 0.76, 0.96; n = 17, I2 = 88.3%) (Table 2 , Supplementary Figs. 3 – 9 ). No statistically significant association could be found on analysis based on the type of AF i.e., persistent or permanent AF (HR 0.86, 95% CI: 0.69, 1.07; n = 8, I2 = 86.1%) and paroxysmal AF (HR 0.66, 95% CI: 0.25, 1.77; n = 2, I2 = 98.3%) (Table 2 , Supplementary Figs. 10 and 11 ).
However, when the two studies i.e., Uhm et al. and Chung et al., were excluded from the subgroup analysis, the risk of stroke and thromboembolism was comparable in the two group of subjects (HFrEF and HFpEF) with low to negligible heterogeneity, irrespective of the study design, duration of follow up and sample size (Supplementary Figs. 12 – 14 ). We also conducted an exploratory analysis based on the cut-off used to define reduced and preserved ejection fraction. There were three sets of studies that we identified: first, where EF ≥ 50% indicated HFpEF and EF < 40% indicated HFrEF; second, where EF ≥ 50% indicated HFpEF and EF < 50% indicated HFrEF; and third, where EF ≥ 40% indicated HFpEF and EF < 40% indicated HFrEF. The findings within each of these three strata show that the risk of stroke and systemic thromboembolism is similar between those with HFpEF and HFrEF (Supplementary Fig. 15 ). The overall quality of evidence was judged to be “Low” according to the GRADE assessment criteria (Supplementary Fig. 16 ).
Our overall analysis shows that AF patients with HFrEF may have a lower risk of stroke and systemic thromboembolism than AF patients with HFpEF. However, substantial heterogeneity could affect this interpretation. The sensitivity analysis, after excluding the studies by Uhm et al. and Chung et al., clearly showed a similar risk of stroke and systemic thromboembolism between the two groups, with low heterogeneity. Subgroup analyses, after excluding these two studies, showed comparable risks of stroke and thromboembolism in the HFrEF and HFpEF groups, regardless of study design, duration of follow-up, and sample size. Our findings are consistent with and support those of a previous review that included data from seven studies ( n = 33,773 subjects) and found a comparable risk of stroke in the HFrEF and HFpEF groups [ 12 ].
If we examine the overall findings, the significantly reduced risk of stroke and thromboembolism observed in those with HFrEF, might be attributed to distinct aspects of the underlying pathophysiology. We may speculate that left ventricular (LV) diastolic dysfunction, as seen in HFpEF, contributes to a higher risk, compared to LV systolic dysfunction found in HFrEF [ 38 , 39 ]. Left atrium (LA) to left ventricle (LV) blood flow is delayed in patients with LV diastolic dysfunction, leading to blood stasis in the LA, and subsequent increase in the risk of thromboembolism and stroke [ 40 ]. However, this reason may not be sufficient, as HFrEF is also associated with some degree of diastolic dysfunction [ 41 ]. Previous study reported higher rates of hypertension and high warfarin usage rate in patients with HFpEF, which might also partly contribute to the risk [ 42 ]. Another possible explanation could be the increased age of patients and a higher proportion of female patients with HFpEF in the included studies. The “congestive heart failure, hypertension, age, diabetes mellitus, prior stroke or transient ischemic attack or thromboembolism, vascular disease, age, sex category” (CHA 2 DS 2 -VASc) score serves as a valuable tool for assessing the risk of stroke associated with AF [ 43 ]. It incorporates various clinical risk factors, including age (higher points for older age) and sex (female sex contributing to a higher score). Patients with HFpEF, therefore, may have increased CHA2DS2-VASc score, and, subsequently, higher risk of stroke and thromboembolism. This brings an interesting perspective: there may actually be no significant difference in the risk of stroke and systemic thromboembolism between the two groups. The adjusting covariates differed between the studies included in this meta-analysis. Patients with AF and HFpEF were older and had a higher prevalence of comorbidities, which, if properly adjusted for in the analysis, could have led to a comparable risk. Additionally, there were differences in the definitions of HFrEF and HFpEF among the included studies. Considering these limitations, the reduced risk of stroke in HFrEF patients might not be significant and could be overstated. The sensitivity analysis (after exclusion of Uhm et al. and Chung et al.) also supports the view that there may be no significant risk difference between the two groups. The low quality of evidence, as judged by the GRADE assessment, strongly supports the need for more studies with robust methodology to provide conclusive evidence.
There were some limitations of our review. We found significant heterogeneity in the reported outcomes which could be due to some differences in the definitions of HFpEF and HFrEF, baseline characteristics of the patients, as well as differences in the methodology (study design and follow up period). The included studies were observational in design and therefore, despite efforts to control for confounding variables, there remains a possibility that some of the important confounders may not have been accounted for. This will ultimately influence the robustness of observed associations. The often-limited longitudinal data in many of the included studies may impact the ability to capture the dynamic nature of HF and AF progression. Additionally, the impact of changing treatment modalities over time on the risk of stroke was not assessed in this review. We were also not able to provide mechanistic insights into the risk of stroke.
Conclusion and implications for clinical practice
In conclusion, the “low” quality evidence from this meta-analysis does not provide convincing evidence that there is significantly different risk of stroke and systemic thromboembolism in cases of AF with associated HFpEF or HFrEF. The finding does not support integration of left ventricular ejection fraction into stroke risk assessments.
Nursing staff may potentially play a crucial role in preventing risk of stroke and systemic thromboembolism in patients with HF and AF. They could be instrumental in educating patients about the importance of adherence to anticoagulation therapy and regularly monitoring their health. Nursing professionals could be involved in assessing medication effectiveness, managing potential complications, and collaborating with healthcare teams for necessary treatment adjustments. They can also contribute to risk stratification, developing individualized care plans based on patient characteristics, and ensuring effective communication within multidisciplinary care teams. Considering limitations of our study, further research would need to focus on the underlying mechanisms contributing to the thromboembolic risk.
Data availability
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.
Takabayashi K, Hamatani Y, Yamashita Y, Takagi D, Unoki T, Ishii M, et al. Incidence of stroke or systemic embolism in Paroxysmal Versus Sustained Atrial Fibrillation: the Fushimi Atrial Fibrillation Registry. Stroke. 2015;46:3354–61.
Article PubMed Google Scholar
Jame S, Barnes G. Stroke and thromboembolism prevention in atrial fibrillation. Heart. 2020;106:10–7.
Schumacher K, Kornej J, Shantsila E, Lip GYH. Heart failure and stroke. Curr Heart Fail Rep. 2018;15:287–96.
Article PubMed PubMed Central Google Scholar
Carlisle MA, Fudim M, DeVore AD, Piccini JP. Heart failure and Atrial Fibrillation, like fire and fury. JACC Heart Fail. 2019;7:447–56.
Kim W, Kim EJ. Heart failure as a risk factor for stroke. J Stroke. 2018;20:33–45.
Adelborg K, Szépligeti S, Sundbøll J, Horváth-Puhó E, Henderson VW, Ording A, et al. Risk of stroke in patients with heart failure: a Population-based 30-Year Cohort Study. Stroke. 2017;48:1161–8.
Simmonds SJ, Cuijpers I, Heymans S, Jones EAV. Cellular and Molecular differences between HFpEF and HFrEF: a step ahead in an Improved Pathological understanding. Cells. 2020;9:242.
McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Böhm M, et al. 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021;42:3599–726.
Murphy SP, Ibrahim NE, Januzzi JL. Heart failure with reduced ejection fraction: a review. JAMA. 2020;324:488–504.
Ma C, Luo H, Fan L, Liu X, Gao C. Heart failure with preserved ejection fraction: an update on pathophysiology, diagnosis, treatment, and prognosis. Braz J Med Biol Res. 2020;53:e9646.
Karnik AA, Gopal DM, Ko D, Benjamin EJ, Helm RH. Epidemiology of Atrial Fibrillation and Heart failure: a growing and important problem. Cardiol Clin. 2019;37:119–29.
Kotecha D, Chudasama R, Lane DA, Kirchhof P, Lip GYH. Atrial fibrillation and heart failure due to reduced versus preserved ejection fraction: a systematic review and meta-analysis of death and adverse outcomes. Int J Cardiol. 2016;203:660–6.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;:n71.
Wells G, Shea B, O’Connell D, Peterson J, Welch V, Losos M et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp . Accessed 18 Nov 2023.
Higgins J, Thomas J, Chandler J, Cumpston M, Li T, Page M et al. Cochrane Handbook for Systematic Reviews of Interventions. https://training.cochrane.org/handbook . Accessed 18 Nov 2023.
Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–34.
McMaster University and Evidence Prime. GRADEpro GDT: GRADEpro Guideline Development Tool [Software]. https://www.gradepro.org/ . Accessed 31 Jul 2024.
Budnik M, Gawałko M, Lodziński P, Tymińska A, Ozierański K, Grabowski M, et al. Heart failure in patients with atrial fibrillation: insights from Polish part of the EORP-AF general long-term registry. ESC Heart Fail. 2023;10:637–49.
Inciardi RM, Giugliano RP, Park J-G, Nordio F, Ruff CT, Chen C, et al. Risks of heart failure, stroke, and bleeding in Atrial Fibrillation according to heart failure phenotypes. JACC Clin Electrophysiol. 2023;9:569–80.
Marzouka GR, Rivner HP, Vaz I, Mehta V, Lopez J, Tang F et al. Stroke risk in Atrial Fibrillation patients with Heart failure with preserved Versus reduced ejection fraction. 2022.
Uhm J-S, Kim J, Yu HT, Kim T-H, Lee S-R, Cha M-J, et al. Stroke and systemic embolism in patients with atrial fibrillation and heart failure according to heart failure type. ESC Heart Fail. 2021;8:1582–9.
Zhang P, Chamberlain AM, Hodge DO, Cai C, Xiao PL, Han J, et al. Outcomes of incident atrial fibrillation in heart failure with preserved or reduced ejection fraction: a community-based study. J Cardiovasc Electrophysiol. 2020;31:2275–83.
Son MK, Park JJ, Lim N-K, Kim W-H, Choi D-J. Impact of atrial fibrillation in patients with heart failure and reduced, mid-range or preserved ejection fraction. Heart. 2020;106:1160–8.
Chung S, Kim T-H, Uhm J-S, Cha M-J, Lee J-M, Park J, et al. Stroke and systemic embolism and other adverse outcomes of heart failure with preserved and reduced ejection fraction in patients with Atrial Fibrillation (from the COmparison study of drugs for symptom control and complication prEvention of Atrial Fibrillation [CODE-AF]). Am J Cardiol. 2020;125:68–75.
Zhirov I, Safronova N, Osmolovskaya Y, Alshevskaya A, Moskalev A, Tereshchenko S. Predictors of unfavorable outcomes in patients with Atrial Fibrillation and Concomitant Heart failure with different ejection fractions: RIF-CHF Register one-year Follow-Up. Cardiol Res Pract. 2019;2019:1692104.
Mentias A, Briasoulis A, Shantha G, Alvarez P, Vaughan-Sarrazin M. Impact of heart failure type on thromboembolic and bleeding risk in patients with atrial fibrillation on oral anticoagulation. Am J Cardiol. 2019;123:1649–53.
Sobue Y, Watanabe E, Lip GYH, Koshikawa M, Ichikawa T, Kawai M, et al. Thromboembolisms in atrial fibrillation and heart failure patients with a preserved ejection fraction (HFpEF) compared to those with a reduced ejection fraction (HFrEF). Heart Vessels. 2018;33:403–12.
Siller-Matula JM, Pecen L, Patti G, Lucerna M, Kirchhof P, Lesiak M, et al. Heart failure subtypes and thromboembolic risk in patients with atrial fibrillation: the PREFER in AF - HF substudy. Int J Cardiol. 2018;265:141–7.
Sartipy U, Dahlström U, Fu M, Lund LH. Atrial fibrillation in heart failure with Preserved, mid-range, and reduced ejection fraction. JACC Heart Fail. 2017;5:565–74.
Sandhu RK, Hohnloser SH, Pfeffer MA, Yuan F, Hart RG, Yusuf S, et al. Relationship between degree of left ventricular dysfunction, symptom status, and risk of embolic events in patients with atrial fibrillation and heart failure. Stroke. 2015;46:667–72.
Eapen ZJ, Greiner MA, Fonarow GC, Yuan Z, Mills RM, Hernandez AF, et al. Associations between atrial fibrillation and early outcomes of patients with heart failure and reduced or preserved ejection fraction. Am Heart J. 2014;167:369–e3752.
Khazanie P, Liang L, Qualls LG, Curtis LH, Fonarow GC, Hammill BG, et al. Outcomes of medicare beneficiaries with heart failure and atrial fibrillation. JACC Heart Fail. 2014;2:41–8.
McMurray JJV, Ezekowitz JA, Lewis BS, Gersh BJ, van Diepen S, Amerena J, et al. Left ventricular systolic dysfunction, heart failure, and the risk of stroke and systemic embolism in patients with atrial fibrillation: insights from the ARISTOTLE trial. Circ Heart Fail. 2013;6:451–60.
Banerjee A, Taillandier S, Olesen JB, Lane DA, Lallemand B, Lip GYH, et al. Ejection fraction and outcomes in patients with atrial fibrillation and heart failure: the Loire Valley Atrial Fibrillation Project. Eur J Heart Fail. 2012;14:295–301.
Badheka AO, Rathod A, Kizilbash MA, Bhardwaj A, Ali O, Afonso L, et al. Comparison of mortality and morbidity in patients with atrial fibrillation and heart failure with preserved versus decreased left ventricular ejection fraction. Am J Cardiol. 2011;108:1283–8.
Olsson LG, Swedberg K, Ducharme A, Granger CB, Michelson EL, McMurray JJV, et al. Atrial fibrillation and risk of clinical events in chronic heart failure with and without left ventricular systolic dysfunction: results from the Candesartan in Heart failure-Assessment of reduction in mortality and morbidity (CHARM) program. J Am Coll Cardiol. 2006;47:1997–2004.
Parkash R, Maisel WH, Toca FM, Stevenson WG. Atrial fibrillation in heart failure: high mortality risk even if ventricular function is preserved. Am Heart J. 2005;150:701–6.
Park H-K, Kim BJ, Yoon C-H, Yang MH, Han M-K, Bae H-J. Left ventricular diastolic dysfunction in ischemic stroke: functional and vascular outcomes. J Stroke. 2016;18:195–202.
Bielecka-Dabrowa A, Gasiorek P, Wittczak A, Sakowicz A, Bytyçi I, Banach M. Left ventricular diastolic dysfunction as predictor of unfavorable prognosis after ESUS. J Multidiscip Healthc. 2021;14:617–27.
Kim T-H, Shim CY, Park JH, Nam CM, Uhm J-S, Joung B, et al. Left ventricular diastolic dysfunction is associated with atrial remodeling and risk or presence of stroke in patients with paroxysmal atrial fibrillation. J Cardiol. 2016;68:104–9.
Daubert MA. Diastolic function in heart failure with reduced ejection fraction: the overlooked prognosticator? JACC Heart Fail. 2019;7:818–20.
Aldaas OM, Malladi CL, Hsu JC. Atrial fibrillation in patients with heart failure with preserved ejection fraction. Curr Opin Cardiol. 2020;35:260–70.
Olesen JB, Torp-Pedersen C, Hansen ML, Lip GYH. The value of the CHA2DS2-VASc score for refining stroke risk stratification in patients with atrial fibrillation with a CHADS2 score 0–1: a nationwide cohort study. Thromb Haemost. 2012;107:1172–9.
Download references
Acknowledgements
Not applicable.
Author information
Authors and affiliations.
Department of Critical Care Medicine, Huzhou Third Municipal Hospital, the Affiliated Hospital of Huzhou University, 2088 Tiaoxi East Road, Wuxing District, Huzhou City, Zhejiang Province, China
Meijuan Zhang & Jie Zhou
You can also search for this author in PubMed Google Scholar
Contributions
MZ, JZ: initial concept ideas, protocol planning and drafting, search screening, analyzing, and drafting all manuscript versions. MZ: methods advice, protocol drafting, and approving final draft. MZ, JZ: data extraction, analysis, and drafting final version.
Corresponding author
Correspondence to Jie Zhou .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Supplementary material 2, supplementary material 3, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/ .
Reprints and permissions
About this article
Cite this article.
Zhang, M., Zhou, J. Systematic review and meta-analysis of stroke and thromboembolism risk in atrial fibrillation with preserved vs. reduced ejection fraction heart failure. BMC Cardiovasc Disord 24 , 495 (2024). https://doi.org/10.1186/s12872-024-04133-1
Download citation
Received : 19 March 2024
Accepted : 19 August 2024
Published : 18 September 2024
DOI : https://doi.org/10.1186/s12872-024-04133-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Atrial fibrillation
- Heart failure
- Preserved ejection fraction
- Reduced ejection fraction
- Systemic thromboembolism
- Systematic review
- Meta-analysis
BMC Cardiovascular Disorders
ISSN: 1471-2261
- General enquiries: [email protected]
An Analysis of the Increasing Trend of Digital Transformation of Business in India: Case Study Approach
- Conference paper
- First Online: 16 September 2024
- Cite this conference paper

- Veenus Gehlot 13 ,
- Poonam Rajharia 14 &
- Madhu Bala Kaushik 13
Part of the book series: Lecture Notes in Networks and Systems ((LNNS,volume 1037))
Included in the following conference series:
- International Conference On Emerging Trends In Expert Applications & Security
Digital transformation is the new normal in the field of business in the present times. In India, the number of internet users is growing exponentially and with respect to that the number of businesses going digital and online is also increasing. The aim of the research is to identify the increasing trend of digital transformations of businesses in India be it SMEs or big companies. An in-depth literature review was presented and the concept of digitisation, the technologies used in the business, and its advantages have been discussed in detail. The research is based on interpretivism philosophy, inductive approach, and qualitative case study method of analysis. It is observed that many small and big companies are using the mentioned digital technologies in the research and are transforming from the traditional form of business to the new form of digital business. The system is installed either in the procurement of raw materials, production, and service process, or the after-sale service.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
Subscribe and save.
- Get 10 units per month
- Download Article/Chapter or eBook
- 1 Unit = 1 Article or 1 Chapter
- Cancel anytime
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Bennett A, Elman C (2006) QUALITATIVE RESEARCH: recent developments in case study methods. Annu Rev Polit Sci 9(1):455–476. https://doi.org/10.1146/annurev.polisci.8.082103.104918
Article Google Scholar
Block RN (2003) Case study methodology. Bargaining for competitiveness: law, research, and case studies, pp 75–86. https://doi.org/10.17848/9780585469652.ch4
Business Insider (2021, Sept 25) One in two corporates in India have a digital transformation strategy in place: Report. https://www.thehindubusinessline.com . https://www.thehindubusinessline.com/info-tech/one-in-two-corporates-in-india-have-a-digital-transformation-strategy-in-place-report/article36665667.ece
Business Standard (2022, Dec 6) Digital transformation spending in India to reach $85 bn by 2026: Report. https://www.business-Standard.com . https://www.business-standard.com/article/economy-policy/digital-transformation-spending-in-india-to-reach-85-bn-by-2026-report-122120600471_1.html
Businesswire (2020, Nov 23) Machine Tool Market to Grow by $1.9 Billion in India: COVID-19 Business Continuity Plan|Rising Industrial Automation to Boost Growth|Technavio. https://www.businesswire.com . https://www.businesswire.com/news/home/20201122005063/en/Machine-Tool-Market-to-Grow-by-1.9-Billion-in-India-COVID-19-Business-Continuity-Plan-Rising-Industrial-Automation-to-Boost-Growth-Technavio
Cenamor J, Rönnberg Sjödin D, Parida V (2017) Adopting a platform approach in servitization: leveraging the value of digitalization. Int J Prod Econ 192:54–65. https://doi.org/10.1016/j.ijpe.2016.12.033
Chetty L (2014) Innovative interpretive qualitative case study research method aligned with systems theory for physiotherapy and rehabilitation research: a review of the methodology. Afr J Physiotherapy Rehabil Sci 5(1–2):40. https://doi.org/10.4314/ajprs.v5i1.7
Conner BP, Manogharan GP, Martof AN, Rodomsky LM, Rodomsky CM, Jordan DC, Limperos JW (2014) Making sense of 3-D printing: creating a map of additive manufacturing products and services. Addit Manuf 1:64–76
Google Scholar
Demirkan H, Bess C, Spohrer J, Rayes A, Allen D, Moghaddam Y (2015) Innovations with smart service systems: analytics, big data, cognitive assistance, and the internet of everything. Commun Assoc Inf Syst 37(1):35
Forbes (2022, Aug 22) SAP BrandVoice: digital India: the next phase of a connected nation driven by midsize businesses. Forbes. https://www.forbes.com/sites/sap/2022/08/24/digital-india-the-next-phase-of-a-connected-nation-driven-by-midsize-businesses/?sh=26a6864f3975
Fortune India (2022, Mar 9) Small biz takes digital highway. https://www.fortuneindia.com . https://www.fortuneindia.com/long-reads/small-biz-takes-digital-highway/107371
Liao Y, Deschamps F, Loures EFR, Ramos LFP (2017) Past, present and future of Industry 4.0—a systematic literature review and research agenda proposal. Int J Prod Res 55(12):3609–3629. https://doi.org/10.1080/00207543.2017.1308576
McKinsey Global Institute (2019, Mar 27) Digital India: technology to transform a connected nation | McKinsey. https://www.mckinsey.com . https://www.mckinsey.com/capabilities/mckinsey-digital/our-insights/digital-india-technology-to-transform-a-connected-nation
Perry C (1998) Processes of a case study methodology for postgraduate research in marketing. Eur J Mark 32(9/10):785–802. https://doi.org/10.1108/03090569810232237
Porter ME, Heppelmann JE (2015) How smart, connected products are transforming companies. Harv Bus Rev 93(10):96–114
Qin J, Fu H, Wang Z, Xia L (2021) Financing and carbon emission reduction strategies of capital-constrained manufacturers in E-commerce supply chains. Int J Prod Econ 241:108271. https://doi.org/10.1016/j.ijpe.2021.108271
Rossato C, Castellani P (2020) The contribution of digitalisation to business longevity from a competitiveness perspective. TQM J 32(4). https://doi.org/10.1108/tqm-02-2020-0032
Saunders M, Lewis P, Thornhill A (2016) Research methods for business students (7th ed). Pearson
Sebastian IM, Ross JW, Beath C, Mocker M, Moloney KG, Fonstad NO (2020) How big old companies navigate digital transformation. In: Strategic information management. Routledge, pp 133–150
Sehlin D, Truedsson M, Cronemyr P (2019) A conceptual cooperative model designed for processes, digitalisation and innovation. Int J Qual Serv Sci 11(4):504–522. https://doi.org/10.1108/ijqss-02-2019-0028
Solis B (2014, Sept 9) Digital transformation and the race against digital darwinism—Brian Solis. Brian Solis. https://www.briansolis.com/2014/09/digital-transformation-race-digital-darwinism/
Tight M (2017) Understanding case study research: small-scale research with meaning. In: Google Books. SAGE. https://www.google.co.in/books/edition/Understanding_Case_Study_Research/fCE9DQAAQBAJ?hl=en&gbpv=1&dq=secondary+data+for+case+study+research&pg=PP1&printsec=frontcover
Truant E, Broccardo L, Dana L-P (2021) Digitalisation boosts company performance: an overview of Italian listed companies. Technol Forecast Soc Chang 173:1–8. https://doi.org/10.1016/j.techfore.2021.121173
Visnjic I, Neely A, Jovanovic M (2018) The path to outcome delivery: interplay of service market strategy and open business models. Technovation 72:46–59. https://doi.org/10.1016/j.technovation.2018.02.003
Westerlund M (2020) Digitalization, internationalization and scaling of online SMEs. Technol Innov Manag Rev 10(4)
Download references
Author information
Authors and affiliations.
Manipal University Jaipur, Jaipur, India
Veenus Gehlot & Madhu Bala Kaushik
JECRC University, Jaipur, India
Poonam Rajharia
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Madhu Bala Kaushik .
Editor information
Editors and affiliations.
Department of Computer Science Engineering, Jaipur Engineering College and Research Centre, Jaipur, Rajasthan, India
Vijay Singh Rathore
Department of Computer Science, University of Milan, MILANO, Italy
Vincenzo Piuri
Porto Accounting and Business School, Polytechnic Institute of Porto, Porto, Portugal
Rosalina Babo
Department of Computer Science and Engineering, ABV-Indian Institute of Information Technology & Management (ABV-IIITM), Gwalior, Madhya Pradesh, India
Vivek Tiwari
Rights and permissions
Reprints and permissions
Copyright information
© 2024 The Author(s), under exclusive license to Springer Nature Singapore Pte Ltd.
About this paper
Cite this paper.
Gehlot, V., Rajharia, P., Kaushik, M.B. (2024). An Analysis of the Increasing Trend of Digital Transformation of Business in India: Case Study Approach. In: Rathore, V.S., Piuri, V., Babo, R., Tiwari, V. (eds) Emerging Trends in Expert Applications and Security. ICE-TEAS 2024. Lecture Notes in Networks and Systems, vol 1037. Springer, Singapore. https://doi.org/10.1007/978-981-97-3991-2_20
Download citation
DOI : https://doi.org/10.1007/978-981-97-3991-2_20
Published : 16 September 2024
Publisher Name : Springer, Singapore
Print ISBN : 978-981-97-3990-5
Online ISBN : 978-981-97-3991-2
eBook Packages : Intelligent Technologies and Robotics Intelligent Technologies and Robotics (R0)
Share this paper
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research

IMAGES
VIDEO
COMMENTS
CASE 1. A 20 year old man with no past medical history presented to a primary stroke center with sudden left sided weakness and imbalance followed by decreased level of consciousness. Head CT showed no hemorrhage, no acute ischemic changes, and a hyper-dense basilar artery. CT angiography showed a mid-basilar occlusion.
Other hypothesised reasons for stroke development in COVID-19 patients are the development of hypercoagulability, as a result of critical illness or new onset of arrhythmias, caused by severe infection. Some case studies in Wuhan described immense inflammatory responses to COVID-19, including elevated acute phase reactants, such as CRP and D-dimer.
Nurse Laura started an 18 gauge IV in Randall's left AC and started him on a bolus of 500 mL of NS. A blood sample was collected and quickly sent to the lab. Nurse Laura called the Emergency Department Tech to obtain a 12 lead EKG. Pertinent Lab Results for Randall. The physician and the nurse review the labs: WBC 7.3 x 10^9/L. RBC 4.6 x 10^12/L.
Read chapter 7 of Patient Management in the Telemetry/Cardiac Step-Down Unit: A Case-Based Approach online now, exclusively on AccessMedicine. AccessMedicine is a subscription-based resource from McGraw Hill that features trusted medical content from the best minds in medicine.
Cramer, SC, Rordorf, G, Maki, JH, et al. Increased pelvic vein thrombi in cryptogenic stroke: results of the Paradoxical Emboli from Large Veins in Ischemic Stroke (PELVIS) study. Stroke 2004;35:46-50
Presentation of Case. Dr. Scott B. Silverman: A 68-year-old man was admitted to this hospital because of worsening confusion. The patient had a history of hypertension and coronary artery disease ...
Day 1: Critical Care (99291) A 67-year-old woman with hypertension and diabetes presents to the emergency department with abrupt onset of left hemiparesis 45 minutes ago. Pre-evaluation: Discussed presentation and vital signs with ED provider (3 mins). Face-to-face evaluation: Performed medically appropriate history and exam.
Abstract. Increasing evidence reports a greater incidence of stroke among patients with Coronavirus disease 2019 (COVID-19) than the non-COVID-19 population and suggests that SARS-CoV-2 infection represents a risk factor for thromboembolic and acute ischemic stroke. Elderly people have higher risk factors associated with acute ischemic stroke or embolization vascular events, and advanced age ...
To our knowledge, the adoption of Learning Health System (LHS) concepts or approaches for improving stroke care, patient outcomes, and value have not previously been summarized. This topical review provides a summary of the published evidence about LHSs applied to stroke, and case examples applied to different aspects of stroke care from high and low-to-middle income countries. Our attempt to ...
A PFO has been demonstrated in 10%-26% of healthy adults. 14 In young patients who have had a cryptogenic stroke, however, the prevalence is thought to be much higher, for example, 40% in one study. 15 It is thought that a PFO allows microemboli to pass into the systemic circulation leading to a stroke.
Contents. Neurologists learn from their patients, and this selection of 60 stroke cases will inform and challenge clinicians at all stages in their careers. Including both common and unusual cases, the aim is to reinforce diagnostic skills through careful analysis of individual presenting patterns, and to guide treatment decisions. Each case ...
Due to the multidimensional presentations (size/location of ICH, presence or absence of IVH, etc.) of those with hemorrhagic stroke, we presented this case study in order to pose that a single surgical approach may not be the answer to improving outcomes in comparison to medical management but actually a transition to a multimodal manner that ...
Go to Case Rubric. Kanika is a 38-year-old right-handed woman who was working as a social media coordinator for an international organization when she had a stroke in early June. Prior to the stroke, Kanika lived alone and frequently saw her sister and nieces, who lived in a nearby state. Her apartment is on the second floor, and there is no ...
General Submissions: Presentations (Oral and Poster) Ischemic stroke: A case study. Rudolf Cymorr Kirby P. Martinez, PhD, MA, RN, CAA, LMT, CSTP, FRIN. Item Link - Use this link for citations and online mentions. This presents an analysis of a case of Ischemic stroke in terms of possible etiology, pathophysiology, drug analysis and nursing care.
In this retrospective study, the case records of 1,287 stroke patients admitted to Al-basher Hospital during a three-year period were reviewed. The stroke patient cohort included 60% men and 40% ...
A 66-year-old man was admitted to hospital with a right frontal cerebral infarct producing left-sided weakness and a deterioration in his speech pattern. The cerebral infarct was confirmed with CT imaging. The only evidence of respiratory symptoms on admission was a 2 L oxygen requirement, maintaining oxygen saturations between 88% and 92%. In a matter of hours this patient developed a greater ...
Pathophysiology and clinical presentation. (DiGiovanna, A. G; 1999) Cerebrovascular accidents, also known as strokes, happen when the blood supply becomes occluded in part of the brain. They can be classified as either ischemic, hemorrhagic, or cryptogenic. In ischemic strokes blood supply can be occluded for three different reasons, a vascular ...
Intracerebral hemorrhage (ICH) with or without intraventricular hemorrhage (IVH) is a highly morbid disease process due to the mass effect and secondary injury that occurs upon the surrounding brain.
Background Stroke and thromboembolism (TE) are significant complications in patients with atrial fibrillation (AF) and heart failure (HF). The impact of ejection fraction status on these risks remains unclear. This study aims to compare the risk of stroke and TE in patients with AF and HF with preserved (HFpEF) or reduced (HFrEF) ejection fraction. Methods Literature search of PubMed, Embase ...
The present section in this research describes the fundamentals and methodologies inspired by Saunders et al. [] and are used in the present research to analyse the trend of digital transformation of Indian businesses.This section also presents the philosophies used in the present research and also defines the ethical considerations that are taken into account while performing the present ...