

Nursing Case Study Examples and Solutions
- Premium Academia
- August 17, 2023
- Nursing Essay Examples
NursingStudy.org is your ultimate resource for nursing case study examples and solutions. Whether you’re a nursing student, a seasoned nurse looking to enhance your skills, or a healthcare professional seeking in-depth case studies, our comprehensive collection has got you covered. Explore our extensive category of nursing case study examples and solutions to gain valuable insights, improve your critical thinking abilities, and enhance your overall clinical knowledge.
Comprehensive Nursing Case Studies
Discover a wide range of comprehensive nursing case study examples and solutions that cover various medical specialties and scenarios. These meticulously crafted case studies offer real-life patient scenarios, providing you with a deeper understanding of nursing practices and clinical decision-making processes. Each case study presents a unique set of challenges and opportunities for learning, making them an invaluable resource for nursing education and professional development.
- Nursing Case Study Analysis [10 Examples & How-To Guides] What is a case study analysis? A case study analysis is a detailed examination of a specific real-world situation or event. It is typically used in business or nursing school to help students learn how to analyze complex problems and make decisions based on limited information.
- State three nursing diagnoses using taxonomy of North American Nursing Diagnosis Association (NANDA) that are appropriate, formatted correctly, prioritized, and are based on the case study. NUR 403 Week 2 Individual Assignment Case Study comprises: Resources: The case study found on p. 131 in Nursing Theory and the Case Study Grid on the Materials page of the student website Complete the Case Study Grid. List five factors of patient history that demonstrates nursing needs.
- Neuro Case Study
- Endocrine Case Study
- Anxiety & Depression Case Study
- Ethical dilemma
- A Puerto Rican Woman With Comorbid Addiction
- Tina Jones Comprehensive SOAP Note
- Insomnia 31 year old Male
- Chest Pain Assessment
Pediatric Nursing Case Studies

In this section, delve into the world of pediatric nursing through our engaging and informative case studies. Gain valuable insights into caring for infants, children, and adolescents, as you explore the complexities of pediatric healthcare. Our pediatric nursing case studies highlight common pediatric conditions, ethical dilemmas, and evidence-based interventions, enabling you to enhance your pediatric nursing skills and deliver optimal care to young patients.
- Case on Pediatrics : Part 1& 2 Solutions
- Pediatric Infant Reflux : History and Physical – Assignment 1 Solution
- Otitis Media Pediatrics Toddler – NSG 5441 Reflection Assignment/Discussion – Solution
- Pediatric Patient With Strep – NSG 5441 Reflection Assignment/Discussion
- Pediatric Urinary Tract infections (UTI) -NSG 5441 Reflection Assignment/Discussion – Solution
- Week 3 discussion-Practical Application in critical care/pediatrics
- Cough Assessmen t
Mental Health Nursing Case Study Examples
Mental health nursing plays a crucial role in promoting emotional well-being and providing care for individuals with mental health conditions. Immerse yourself in our mental health nursing case studies, which encompass a wide range of psychiatric disorders, therapeutic approaches, and psychosocial interventions. These case studies offer a holistic view of mental health nursing, equipping you with the knowledge and skills to support individuals on their journey to recovery.
- Psychiatric Nursing: Roles and Importance in Providing Mental Health Care
- Mental Health Access and Gun Violence Prevention
- Fundamentals of neurotransmission as it relates to prescribing psychotropic medications for clients with acute and chronic mental health conditions – Unit 8 Discussion – Reflection
- Unit 7 Discussion- Complementary and Alternative Medicine in Mental Health Care – Solution
- Ethical and Legal Foundations of PMHNP Care Across the Lifespan Assignment – Analyze salient ethical and legal issues in psychiatric-mental health practice | Solution
- Pathways Mental Health Case Study – Review evaluation and management documentation for a patient and perform a crosswalk of codes – Solution
- Analyze salient ethical and legal issues in psychiatric-mental health practice
- SOAP notes for Mental Health Examples
- compare and contrast two mental health theories
- Environmental Factors and Health Promotion Presentation: Accident Prevention and Safety Promotion for Parents and Caregivers of Infants
Geriatric Nursing Case Studies
As the population ages, the demand for geriatric nursing expertise continues to rise. Our geriatric nursing case studies focus on the unique challenges faced by older adults, such as chronic illnesses, cognitive impairments, and end-of-life care. By exploring these case studies, you’ll develop a deeper understanding of geriatric nursing principles, evidence-based gerontological interventions, and strategies for promoting optimal health and well-being in older adults.
- M5 Assignment: Elderly Driver
- HE003: Delivery of Services – Emmanuel is 55-year-old man Case – With Solution The Extent of Evidence-Based Data for Proposed Interventions – Sample Assignment 1 Solution
- Planning Model for Population Health Management Veterans Diagnosed with Non cancerous chronic pain – Part 1 & 2 Solutions
- PHI 413 Case Study Fetal Abnormality Essay
- Insomnia Response and Insomnia
- Analysis of a Pertinent Healthcare Issue: Short Staffing
- Paraphrenia as a Side of the Schizophrenia – Week 4 Solution
- Module 6 Pharm Assignment: Special Populations
- Public Health Nursing Roles and Responsibilities in Disaster Response – Assignment 2 Solution
- Theory Guided Practice – Assignment 2 Solution
- How can healthcare facilities establish a culture of safety – Solution
- Discuss the types of consideration a nurse must be mindful of while performing a health assessment on a geriatric patient as compared to a middle-aged adult – Solution
- Promoting And Protecting Vulnerable Populations – Describe what is meant by vulnerable populations and explain strategies you, as the public health nurse, could use to best facilitate the achievement of healthful outcomes in this population?
Community Health Nursing Case Studies
Community health nursing plays a vital role in promoting health, preventing diseases, and advocating for underserved populations. Dive into our collection of community health nursing case studies, which explore diverse community settings, public health issues, and population-specific challenges. Through these case studies, you’ll gain insights into the role of community health nurses, interdisciplinary collaboration, health promotion strategies, and disease prevention initiatives.
- Community and Target Aggregate: Residents of the community health center, particularly those aged 65 and above Topic: Secondary Prevention/Screenings for a Vulnerable Population
- Tools For Community Health Nursing Practice2
- 5 Theories in Community Health Nursing: A Complete Guide
- Role of community health nursing and community partnerships as they apply to the participating family’s community – Assignment 1 Solution
- Community/Public Health Nursing DQ2
- CSU-Community healthcare Presentation – Assignment 1 Solution
- Community Healthcare Presentation – Domestic Violence And Level Of Prevention – Solution
Critical Care Nursing Case Study Examples
Critical care nursing demands swift decision-making, advanced technical skills, and the ability to provide intensive care to acutely ill patients. Our critical care nursing case studies encompass a range of high-acuity scenarios, including trauma, cardiac emergencies, and respiratory distress. These case studies simulate the fast-paced critical care environment, enabling you to sharpen your critical thinking skills, enhance your clinical judgment, and deliver exceptional care to critically ill patients.
- Nursing Case Study Parkinsons Disease
- Nursing Case Study: Patient with Drug and Alcohol Induced Paranoid Schizophrenia
- Neonatal Hypothermia and Neonatal Sepsis: Nursing Case Study
- Chronic Obstructive Pulmonary Disease Nursing Case Study
Maternal and Child Health Nursing Case Study Examples
The field of maternal and child health nursing requires specialized knowledge and skills to support the health and well-being of women and children throughout their lifespan. Explore our collection of maternal and child health nursing case studies, which encompass prenatal care, labor and delivery, postpartum care, and pediatric nursing. These case studies provide a comprehensive view of maternal and child health, allowing you to develop expertise in this essential area of nursing practice.
You can also check out Patient Safety in High-Tech Settings PICOT Questions Examples
Surgical Nursing Case Studies
Surgical nursing involves caring for patients before, during, and after surgical procedures. Our surgical nursing case studies cover a wide range of surgical specialties, including orthopedics, cardiovascular, and gastrointestinal surgeries. Delve into these case studies to gain insights into preoperative assessment, perioperative management, and postoperative care. By examining real-life surgical scenarios, you’ll develop a comprehensive understanding of surgical nursing principles and refine your skills in providing exceptional care to surgical patients.
- Discuss DI in relation to a postoperative neurosurgical patient – Week 2, 3, 4 Solution
- DISCUSSION WK 3
- Career Planning & Professional Identity Paper
- N ursing Case Analysis
- Ethical Dilemma on Robotic Surgery and ACS Codes of Ethics – Post 2
- NURS – 6521C Advanced Pharmacology
- Essay on Alterations in Neurological and Endocrine Functions
- Clinical Preparation Tool – Child and Adolescent Symptom Inventory – Unit
- Initial Psychiatric Interview/SOAP Note – Assignment 1 Solution
- Current Trends in Nursing Practice: Electronic Prescriptions for Opioids – Week 4 Solution
- Nurse-Sensitive Indicators -Week 3 Solution
- Theory–Practice Gap in Jean Watson Theory of Human Caring – Assignment 1 Solution
- Bowel Obstruction Case Video Presentation – Week 4 Solution
- Appendicitis SOAP Note – Sample SOAP Solution 1
- Week 4: GERD SOAP Note Assignment Solution
Obstetric Nursing Case Study
Obstetric nursing focuses on providing care to women during pregnancy, childbirth, and the postpartum period. Our obstetric nursing case studies explore various aspects of prenatal care, labor and delivery, and postpartum recovery. Gain valuable knowledge about common obstetric complications, evidence-based interventions, and strategies for promoting maternal and fetal well-being. These case studies will enhance your obstetric nursing skills and prepare you to deliver compassionate and competent care to expectant mothers.
- Capstone Proposal: Postpartum Hemorrhage Education To Nursing Students
- Progress Evaluation Telecommunication: Teleconference on Post-Partum Hemorrhage
- Case Study 5.2 the Moral and Ethical Questions of Aborting an Anencephalic Baby
- Holistic intervention plan design to improve the quality of outcomes – Problem Statement (PICOT)
- ADV HEALTH ASSESSMENT: TJ a 32-year-old pregnant lesbian, is being seen for an annual physical exam and has been having vaginal discharge – Solution
- Facilitative Communication and Helping Skills in Nursing & Decision Making Assignment Solution
- Benchmark – Evidence-Based Practice Proposal Paper Example
- Three nursing diagnoses for this client based on the health history and screening (one actual nursing diagnosis, one wellness nursing diagnosis, and one “risk for” nursing diagnosis)
- Identify two or more issues with the existing system
- Differences between inpatient and outpatient coding
Nursing Ethics Case Study
Ethical dilemmas are an inherent part of nursing practice. Our nursing ethics case studies shed light on complex ethical issues that nurses encounter in their daily work. Explore thought-provoking scenarios involving patient autonomy, confidentiality, end-of-life decisions, and resource allocation. By examining these case studies, you’ll develop a deeper understanding of ethical principles, ethical decision-making frameworks, and strategies for navigating ethical challenges in nursing practice.
- Ethics in Complementary Therapies
- Ethics Case Study Analysis
- Ethics in Practice
- Ethical Dilemma on Robotic Surgery and ACS Codes of Ethics – Post 1
- Case Study on Biomedical Ethics in the Christian Narrative
- Academic Success and Professional Development Plan Part 2: Strategies to Promote Academic Integrity and Professional Ethics
- Week 9 Assignment 9.1: Mercy Killing Ethics – Using one theory that you have studied that you agree with and one theory that you disagree with, describe how Officer Jones would act in each case – Solution
- Deliverable 4 – Code of Ethics Intake Packet
- Ethics in the Workplace
- code of ethics for nurses
- Applying the ANA Code of Ethics
Health Promotion Case Study
Community health promotion plays a crucial role in improving the health and well-being of populations. Our community health promotion case studies highlight successful initiatives aimed at preventing diseases, promoting healthy lifestyles, and addressing social determinants of health. Explore strategies for community engagement, health education, and collaborative interventions that make a positive impact on the well-being of individuals and communities.
- Health Promotion in Minority Populations
- Environmental Factors and Health Promotion Presentation: Accident Prevention and Safety Promotion for Parents and Caregivers of Infants
- Health Education And Current Challenges For Family-Centered Health Promotion
- Cultural Competence And Nutrition In Health Promotion
- Why is the concept of family health important? Consider the various strategies for health promotion.
- levels of health promotion
- Integrate evidence from research and theory into discussions of practice competencies, health promotion and disease prevention strategies, quality improvement, and safety standards.
- Discuss various theories of health promotion, including Pender’s Health Promotion Model, the Health Belief Model, the Transtheoretical Theory, and the Theory of Reasoned Action.
- What strategies, besides the use of learning styles, can a nurse educator consider when developing tailored individual care plans, or for educational programs in health promotion?
- Describe health promotion for Pregnant women
- Identify a health problem or need for health promotion for a particular stage in the life span of a population from a specific culture in your area. Choose one of the Leading Health Indicators (LHI) priorities from Healthy People 2020: https://www.healthypeople.gov/2020/Leading-Health-Indicators
- A description of a borrowed theory (expectancy-value theory and social cognitive theory) that could be applied to improve health promotion patient education in primary care clinic. Is this borrowed theory appropriate?
- How has health promotion changed over time
- Primary Prevention/Health Promotion
- Health Risk Assessment and Health Promotion Contract
Nursing Leadership Case Studies
Nursing leadership is essential for driving positive change and ensuring high-quality patient care. Our nursing leadership case studies examine effective leadership strategies, change management initiatives, and interprofessional collaboration in healthcare settings. Gain insights into the qualities of successful nurse leaders, explore innovative approaches to leadership, and learn how to inspire and motivate your team to achieve excellence in nursing practice.
- Part 3: Nursing Leadership – Childbearing after menopause – Assignment Solution
- Capstone Project Ideas for Nursing Leadership
- The purpose of this assignment is to examine the impact of contemporary challenges in care delivery facing nursing leadership. Select and research a major issue in the delivery of care facing nurse leaders today and write a 1,250-1,500 word paper addressing the following:
- One nursing theory will be presented as a framework to resolve a problem occurring within one of the professional areas of leadership, education, informatics, healthcare policy or advance clinical practice. The same nursing theory selected in Assignment One may be used to resolve the identified problem.
- Module 6: Change and Leadership in Nursing Education – Professional Development
- Module 6: Change and Leadership in Nursing Education – Critical Thinking
- Module 6: Change and Leadership in Nursing Education – Discussion
- Analyze one of the following concepts: “Advanced Practice Nursing,” “Leadership in Nursing Practice” or “Holistic Nursing Practice”
- Nursing Administration Function: A Comprehensive Guide for Nursing Students
- Theory and Leadership
- NUR-514: Organizational Leadership and Informatics
- Leadership: Workplace Environment Assessment
- Professional Development in Nursing – Topic 3 Assignment Solution
- Leadership Change Framework – Week 8 Assignment Solution
At NursingStudy.org, we strive to provide you with a comprehensive collection of nursing case study examples and solutions that align with the best practices recommended by YOAST and RankMath. By exploring these diverse case studies, you’ll enhance your clinical knowledge, critical thinking abilities, and overall understanding of nursing practice. Take advantage of this valuable resource and elevate your nursing skills to new heights.
Remember, success in nursing begins with knowledge and continues with lifelong learning. Explore our nursing case study examples and solutions today and embark on a journey of professional growth and excellence.
Working On an Assignment With Similar Concepts Or Instructions?
A Page will cost you $12, however, this varies with your deadline.
We have a team of expert nursing writers ready to help with your nursing assignments. They will save you time, and improve your grades.
Whatever your goals are, expect plagiarism-free works, on-time delivery, and 24/7 support from us.
Here is your 15% off to get started. Simply:
- Place your order ( Place Order )
- Click on Enter Promo Code after adding your instructions
- Insert your code – Get20
All the Best,
Have a subject expert Write for You Now
Have a subject expert finish your paper for you, edit my paper for me, have an expert write your dissertation's chapter, what you'll learn.
- Nursing Paper Examples
Related Posts
- Personal Philosophy Statement Example for a PMHNP
- Leadership Strategies for Success-Nursing Paper Examples
- Applying the Scientific Method-Nursing Paper Examples
Important Links
Knowledge base, paper examples, nursing writing services.
Nursingstudy.org helps students cope with college assignments and write papers on various topics. We deal with academic writing, creative writing, and non-word assignments.
All the materials from our website should be used with proper references. All the work should be used per the appropriate policies and applicable laws.
Our samples and other types of content are meant for research and reference purposes only. We are strongly against plagiarism and academic dishonesty.
Phone: +1 628 261 0844
Mail: [email protected]

We Accept:

@2015-2024, Nursingstudy.org

June 15, 2024 . By Kepher
Nursing Case Study on Mental Health: The Ultimate Guide for Learners and Professionals

Table of Contents
In the realm of nursing, the ability to analyze and synthesize complex patient situations is paramount. This is particularly true in the field of mental health, where understanding the intricacies of human experience and behavior is crucial for effective care. Nursing case studies on mental health provide a unique opportunity to delve into the nuances of patient experiences, explore the multifaceted nature of mental illness, and apply nursing knowledge to real-world scenarios.
This article serves as a comprehensive guide for crafting impactful nursing case studies on mental health. Whether you’re a student honing your clinical reasoning skills or a seasoned professional seeking to deepen your understanding, this resource will equip you with the tools necessary to create compelling, insightful narratives.
The Core Principles of a Nursing Case Study on Mental Health

A nursing case study on mental health is not merely a retelling of a patient’s story. It’s a structured, analytical exploration that demonstrates your understanding of:
- The patient’s unique mental health condition: This includes accurate diagnosis, symptomatology, and potential contributing factors.
- The nursing process: The case study should showcase your application of assessment, diagnosis, planning, implementation, and evaluation within the context of mental health care.
- Evidence-based practice: Incorporating current research, clinical guidelines, and best practices demonstrates your commitment to providing informed care.
- Ethical considerations: Mental health care presents unique ethical dilemmas. The case study should address these thoughtfully and demonstrate an understanding of patient autonomy, confidentiality, and professional boundaries.
How to Craft a Compelling Case Study on Mental Health
1. Choosing the Right Subject for Your Nursing Case Study
A nursing case study on mental health should focus on a specific patient scenario. When selecting a subject, consider the following factors:
- Complexity: Choose a case that allows for exploration of multiple dimensions, such as the interplay between biological, psychological, and social factors influencing the patient’s mental health.
- Relevance: Select a case that reflects current trends in mental health care, such as the increasing focus on integrated care, stigma reduction, or the impact of social determinants of health.
- Ethical considerations: Ensure the case study adheres to ethical guidelines, respecting patient confidentiality and avoiding potentially harmful generalizations.

2. Gathering Data for Your Nursing Case Study on Mental Health
Thorough data collection is the cornerstone of any effective nursing case study on mental health. Here’s a comprehensive approach:
- Patient interview: Engage in a comprehensive interview with the patient, allowing them to share their experiences, perspectives, and goals.
- Medical records review: Thoroughly review the patient’s medical history, including diagnoses, medications, and previous treatments.
- Observations: Document your direct observations of the patient’s behavior, appearance, and interactions with others.
- Family and support system interviews: Gather information from family members, friends, or other support systems, gaining insights into the patient’s home environment and coping mechanisms.
- Literature review: Conduct a thorough review of relevant research and clinical guidelines to provide context and evidence-based support for your analysis.
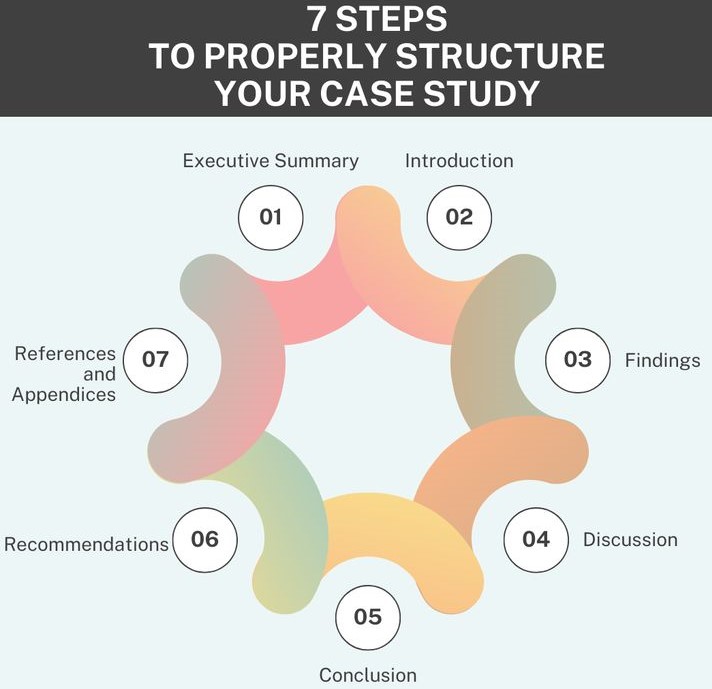
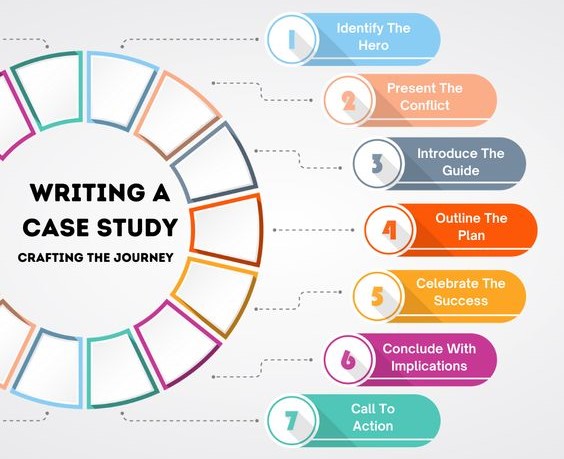
3. Organizing and Structuring Your Nursing Case Study
A well-structured nursing case study on mental health ensures clarity and logical progression of information. Here’s a suggested framework:
Introduction:
- Briefly introduce the patient and their presenting problem.
- State the case study’s purpose and objectives.
Background Information:
- Provide demographic information about the patient, including age, gender, race, ethnicity, and socioeconomic status.
- Briefly summarize the patient’s medical history, including any relevant physical health conditions or past mental health diagnoses.
- Outline the patient’s social history, including family dynamics, support systems, education, and employment.
Assessment:
- Summarize the patient’s physical and mental health status.
- Include relevant assessment data gathered through interviews, observations, and medical records.
- Analyze the patient’s current mental state, including their mood, thought processes, and behaviors.
- Identify any potential contributing factors to their mental health condition.
- Discuss the patient’s current mental health diagnosis, providing a rationale for the chosen diagnosis based on assessment findings.
- Briefly explain the symptoms associated with the diagnosis.
- Identify any co-occurring disorders or underlying conditions that may be contributing to the patient’s overall presentation.
- Develop a comprehensive plan of care for the patient.
- Identify specific nursing interventions aimed at addressing the patient’s needs, including medication administration, therapeutic interventions, and support services.
- Set realistic and measurable goals for the patient, considering their individual needs and preferences.
Implementation:
- Document the implementation of the nursing interventions chosen for the patient.
- Describe how these interventions were carried out, including any challenges or modifications encountered.
- Include any patient education provided, such as information about their diagnosis, medication, or coping strategies.
Evaluation:
- Assess the effectiveness of the nursing interventions implemented.
- Evaluate the patient’s progress towards achieving the established goals.
- Analyze any changes in the patient’s mental state, behaviors, or coping mechanisms.
- Identify any factors that may have influenced the patient’s response to treatment.
Conclusion:
- Summarize the key findings of the nursing case study on mental health.
- Reflect on the patient’s journey and the impact of nursing interventions.
- Discuss any lessons learned or areas for further improvement in future practice.
4. Incorporating Ethical Considerations into Your Nursing Case Study
Mental health care often presents ethical challenges. In your nursing case study on mental health, it’s essential to address these thoughtfully:
- Confidentiality: Ensure that all patient information is treated with strict confidentiality. Avoid disclosing details that could compromise the patient’s identity or privacy.
- Informed consent: Discuss the importance of informed consent in mental health care, including the patient’s right to refuse treatment or participate in research.
- Patient autonomy: Emphasize the patient’s right to make decisions about their own care, even if those decisions differ from professional recommendations.
- Professional boundaries: Maintain professional boundaries in all interactions with the patient, avoiding dual relationships or inappropriate disclosure.
5. Using Evidence-Based Practice in Your Nursing Case Study on Mental Health
A nursing case study on mental health should not rely solely on anecdotal evidence. It’s crucial to integrate evidence-based practice:
- Literature review: Conduct a thorough literature review to support your analysis and interventions. Scholarly articles and papers from reputable academic platforms such as Google Scholar and PhD Nurse Writer can be quite useful in the research.
- Clinical guidelines: Refer to relevant clinical guidelines to ensure your approach aligns with best practices.
- Research findings: Incorporate findings from relevant research studies to provide a scientific basis for your conclusions.
6. Writing Style and Format for an Engaging Mental Health Nursing Case Study
- Clarity and conciseness: Write in a clear and concise style, avoiding jargon or overly technical language.
- Objectivity: Present information in an objective manner, avoiding personal opinions or biases.
- APA style: Follow the guidelines of the American Psychological Association (APA) for formatting, citations, and references.
- Word count: Adhere to any specified word count limits for the assignment.
Topic Examples for Your Nursing Case Study on Mental Health
To ignite your creativity, here are some compelling topics for your nursing case study on mental health:
- The impact of trauma on mental health: Explore the effects of traumatic experiences on a patient’s emotional well-being, coping mechanisms, and treatment needs.
- The role of culture and ethnicity in mental health: Analyze how cultural beliefs and societal factors influence a patient’s understanding of their mental health condition and their access to care.
- Addressing stigma and discrimination in mental health: Examine the societal stigma surrounding mental illness and its impact on a patient’s willingness to seek help, their self-esteem, and their overall quality of life.
- The integration of physical and mental health care: Illustrate how a holistic approach to healthcare can benefit patients with mental health conditions, addressing both their physical and mental well-being.
- The impact of social determinants of health on mental health: Investigate how poverty, housing insecurity, lack of access to education, and other social factors contribute to mental health challenges.
- The use of technology in mental health care: Explore the role of technology in providing mental health services, including teletherapy, mobile apps, and online support groups.
Tips for Success in Writing Mental Health Case Studies
- Start early: Begin working on your case study well in advance of the deadline to allow for thorough research and analysis.
- Seek guidance from faculty or mentors: Don’t hesitate to ask for feedback and guidance from your instructors or other experienced nurses.
- Practice critical thinking skills: Develop your ability to analyze complex patient situations and make sound clinical judgments.
- Stay current with evidence-based practices: Keep abreast of the latest research and clinical guidelines in mental health care.
- Emphasize patient-centered care: Prioritize the patient’s perspective and needs throughout the case study.
The Value of Writing a Nursing Case Study on Mental Health
Crafting a nursing case study on mental health offers a multitude of benefits:
- Deepening knowledge and skills: The process of developing a case study strengthens your understanding of mental health conditions, nursing interventions, and ethical considerations.
- Improving critical thinking abilities: Case studies challenge you to analyze complex situations, apply your knowledge, and make informed decisions.
- Enhancing communication skills: Writing a case study refines your ability to communicate complex ideas clearly and concisely.
- Developing a professional portfolio: Case studies can be valuable additions to your portfolio, showcasing your clinical skills and expertise.
Writing a nursing case study on mental health is a rewarding and enriching experience. By following these guidelines and approaching the process with dedication, you’ll create a compelling and informative narrative that highlights the complexities of mental health care and the vital role of nursing in promoting patient well-being. Remember, your case study is not just an academic exercise; it’s an opportunity to make a tangible contribution to the field of mental health nursing by sharing your knowledge, insights, and commitment to providing compassionate care.
Professional Help with a Nursing Case Study on Mental Health
At PhD Nurse Writer , we are the academic writing experts that you should engage when seeking professional help with a nursing case study on mental health. We offer the best nursing assignment help , with a guarantee of original, engaging and plagiarism free case studies.
- nursing case study on mental health ,
- Article Reviews (2)
- Case Studies (9)
- Dissertations (13)
- Nursing essays (27)
- Nursing Thesis (6)
- Research papers (22)
- Uncategorized (28)
Recent News
Nursing Dissertation Outline: A Definitive Writing Guide
Dissertation writing pitfalls: the top 10 mistakes to avoid for success, nursing essay topic: top 20 topics for compelling nursing essays, struggling with your essay.
Top-class writers are here!

Our Products/Tools
- Plagiarism Checker
- Paraphrasing Tool
- Thesis statement generator
- Words to pages converter
- Free college GPA calculator
- Citation Generator
- Plagiarism Checker Reddit
Legal & Policies
- Terms & Conditions
- Refund policy
- Privacy policy
- Cookies policy
Customer Services
- Code of conduct
+1-917-810-5386
© 2024 PHD Nurse Writer. All rights reserved.
Academic Support for Nursing Students
No notifications.
Disclaimer: This case study has been written by a student and not our expert nursing writers. View professional sample case studys here.
View full disclaimer
Any opinions, findings, conclusions, or recommendations expressed in this case study are those of the author and do not necessarily reflect the views of NursingAnswers.net. This case study should not be treated as an authoritative source of information when forming medical opinions as information may be inaccurate or out-of-date.
Mental Health - Definition and Case Study
Info: 1058 words (4 pages) Nursing Case Study Published: 29th Mar 2021
Reference this
Tagged: gibbs reflective cycle mental health
If you need assistance with writing your nursing case study, our professional nursing case study writing service is here to help!
BIBLIOGRAPHY
Cite this work.
To export a reference to this article please select a referencing stye below:
Related Services

- Case Study Service

- Nursing Essay Writing Service

- Reflective Writing Service
Related Content
Content relating to: "mental health"
Everyone experiences emotional ups and downs from time to time caused by certain events in our lives. Mental health related conditions go beyond these emotional reactions to specific situations. They are medical conditions that cause changes in how we think and feel and within our mood.
Related Articles

A Human Rights Based Approach to Mental Health Care
Human rights within adult mental health are enshrined in the 2006, Convention on the Rights of People with Disabilities (CRPD). Ireland signed the Convention in 2007 and further to its ratification in March 2018. ...
Integrated Treatment for Substance Use and Depression
Mental Health: Simone Case Scenario Dual diagnosis, co morbidity and co-occurring disorders are terms often used interchangeably to describe mental ill health and substance abuse (drugs and/or alcohol...
Recovery-Oriented Practice in Mental Health
What is the difference between ‘clinical recovery’ and ‘personal recovery’ for people with lived experience of mental illness? ...
DMCA / Removal Request
If you are the original writer of this case study and no longer wish to have your work published on the NursingAnswers.net website then please:
Our academic writing and marking services can help you!
- Marking Service
- Samples of our Work
- Full Service Portfolio
Related Lectures
Study for free with our range of nursing lectures!
- Drug Classification
- Emergency Care
- Health Observation
- Palliative Care
- Professional Values

Write for Us
Do you have a 2:1 degree or higher in nursing or healthcare?
Study Resources
Free resources to assist you with your nursing studies!
- APA Citation Tool
- Example Nursing Essays
- Example Nursing Assignments
- Example Nursing Case Studies
- Reflective Nursing Essays
- Nursing Literature Reviews
- Free Resources
- Reflective Model Guides
- Nursing and Healthcare Pay 2021
Mental Health Nursing
At a glance, grahame smith.
- Your Feedback
- Become a reviewer
- More student books
- Student Apps
- Join an e-mail list

Buy now/find out more
Case Studies
Case 5: denise.
Denise, a 19-year-old woman, has been admitted informally to an acute mental health ward; this is Denise's first admission. Denise was being treated for depression by her GP; prior to her admission Denise attempted to kill herself by cutting her wrists. Subsequently a short admission was arranged with the aim of devising a comprehensive care package.
After speaking about the circumstances leading up to her suicide attempt Denise became increasingly tearful and distressed, and started demanding to see a doctor. After being told that the doctor was on their way and would arrive in about 10 minutes, Denise became angry demanding medication to calm her down; she then proceeded to run towards the ward's doors shouting that she wanted to go home. At that moment the doctor arrived on the ward and Denise also immediately calmed down.
During the assessment process Denise disclosed that being angry if she did not get her way was not unusual for her. She also mentioned that she felt awful after these bouts of anger. She described herself as a "terrible person who was out of control" and she just wanted to die. After assessing Denise the nurse started to formulate a plan of care.
(a) What type of psychological interventions would the nurse consider implementing?
Show Answer
- Build a collaborative and therapeutic relationship based on a person-centred approach.
- Normalise an individual's experiences of mental distress.
- Take a "strengths approach".
- Maintain safety and effectively manage challenging behaviours.
- Explore the individual's capacity to change.
- Modify thought processes – identify, challenge and replace negative thoughts.
- Focus on the individual controlling and regulating their behaviour – promoting and enhancing healthy ways of coping.
- Prevent social isolation and promote social functioning.
- Focus on relapse prevention – early warning signs and self-monitoring of symptoms.
- Signpost to self-help and relevant support groups.
- Therapeutically support recovery.
(b) Currently Denise has been admitted informally to the ward. Due to Denise's impulse control difficulties this may change. On this basis what does the nurse professionally need to know when managing Denise's legal status?
- Understand and apply current legislation in a way that protects Denise.
- Act in accordance with the law, relevant ethical and regulatory frameworks, and also take into account local protocols/policies.
- Respect and uphold Denise's rights
- Know when to actively share personal information with others when the interests of safety and protection override the need for confidentiality.
(c) Denise is subsequently diagnosed with a "borderline personality disorder". What other types of personality disorders are there?
- Cluster A – paranoid, schizoid and schizotypal.
- Cluster B – antisocial (type: dissocial), borderline (type: emotionally unstable), histrionic, and narcissistic (not included in types).
- Cluster C – avoidant (type: anxious), dependent, obsessive-compulsive (type: anankastic).
- paranoid – suspicious and excessively sensitive;
- schizoid – emotional coldness, little interest in other people;
- schizotypal – odd beliefs and unusual appearance;
- borderline – instability of mood, impulsive;
- histrionic – excessive attention seeking;
- narcissistic – grandiose and arrogant;
- antisocial – disregard of self and others;
- avoidant – feelings of inadequacy;
- dependent – submissive behaviour;
- 0bsessive-compulsive – a preoccupation with orderliness.
(d) What specific psychological interventions would the nurse deliver?
- boundary setting;
- promoting healthy ways of coping;
- motivational interviewing and pre-therapy work;
- delivering specific therapeutic approaches/therapies.
(e) How could the nurse learn from their experiences of working with Denise?
- identifying and describing the experiences;
- examining the experiences in depth and teasing out the key issues;
- critically processing the issues;
- learning from the experiences by implementing future actions that improve the nurse's practice.
Denise has now been on the ward for over 6 months. Each time discharge has been arranged Denise self-harms or threatens suicide. Denise has now agreed to go to a therapeutic community, a place has been secured and Denise is now engaging in pre-therapy work.
(a) What other treatments besides a therapeutic community are recommended for individuals diagnosed with a borderline personality disorder?
- cognitive behaviour therapy – group and individual;
- behavioural approaches;
- mentalisation-based approaches;
- dialectic behaviour therapy.
(b) While working with Denise the primary nurse has found the relationship at times to be quite stressful. What are the signs of stress?
- sleep problems;
- loss of appetite;
- difficulty concentrating;
- constantly feeling anxious;
- feeling irritable and/or angry;
- having repeating thoughts;
- avoiding certain situations and/or people;
- an increased use of alcohol;
- muscle tension.
(c) What strategies could the nurse use to manage their stress?
- engage in physical activity;
- engage in something that makes them laugh;
- learn relaxation and/or deep breathing techniques;
- take control of the situation;
- seek support and talk;
- problem solve;
- eat a healthily diet;
- drink plenty of water;
- be mindful.
(d) What process should be utilised as a way to support the primary nurse to improve their practice?
Correct answer: A common method of systematically reflecting on practice is through the clinical supervision, which is a formal activity where a clinical supervisor facilitates the nurse to reflect upon their practice and identify strategies that focus on improving their practice.
Consider Chapters 20, 34 and 37.
Print Answers | « Previous Case
Mental Health and Psychiatric Nursing
The field of mental health often seems a little unfamiliar or mysterious, making it hard to imagine what the experience will be like or what nurses do in this area. This is an overview of the history of mental illness, advances in treatment, current issues in mental health, and the role of the psychiatric nurse .
Table of Contents
Mental health, mental illness, diagnostic and statistical manual of mental disorders, ancient times, period of enlightenment and creation of mental institutions, sigmund freud and treatment of mental disorders, development of psychopharmacology, mental illness in the 21st century, psychiatric nursing practice, mental health and mental illness.
Mental health and mental illness are difficult to define precisely. The culture of any society strongly influences its beliefs and values, and this in turn affects how that society defines health and illness.
No single universal definition of mental health exists. Generally, a person’s behavior can provide clues to his or her mental health.
- In most cases, mental health is a state of emotional, psychological, and social wellness evidenced by satisfying interpersonal relationships , effective behavior and coping, positive self-concept, and emotional stability.
- Factors influencing a person’s mental health can be categorized as individual, interpersonal, and social/cultural.
- Individual , or personal, factors include a person’s biologic make up, autonomy and independence, self-esteem , capacity for growth, vitality, ability to find meaning in life, emotional resilience or hardiness, sense of belonging, reality orientation, and coping or stress management abilities.
- Interpersonal , or relationship, factors include effective communication , ability to help others, intimacy, and a balance of separateness and connectedness.
- Social/cultural , or environmental, factors include a sense of community, access to adequate resources, intolerance of violence, support of diversity among people, mastery of the environment, and a positive, yet realistic, view of one’s world.
The American Psychiatric Association (APA, 2000) defines a mental disorder as “a clinically significant behavioral or psychological syndrome or pattern that occurs in an individual and is associated with present distress or with a significantly increased risk of suffering death , pain , disability, or an important loss of freedom.
- General criteria to diagnose mental disorders include dissatisfaction with one’s characteristics, abilities, and accomplishments; ineffective or unsatisfying relationships; dissatisfaction with one’s place in the world; ineffective coping with life events; and lack of personal growth.
- Factors contributing to mental illness also can be viewed within individual, interpersonal, and social/cultural categories.
- Individual factors include biologic make up, intolerable or unrealistic worries or fears, inability to distinguish reality from fantasy, intolerance of life’s uncertainties, a sense of disharmony in life, and a loss of meaning in one’s life.
- Interpersonal factors include ineffective communication , excessive dependency on or withdrawal from relationships, no sense of belonging, inadequate social support, and loss of emotional control.
- Social/cultural factors include lack of resources, violence, homelessness, poverty, an unwarranted negative view of the world, and discrimination.
The Diagnostic and Statistical Manual of Mental Disorders, 4th edition, Text Revision (DSM-IV-TR) is a taxonomy published by the APA.
- The DSM-IV-TR describes all mental disorders, outlining specific diagnostic criteria for each based on clinical experience and research.
- The DSM-IV-TR has three purposes:
- To provide a standardized nomenclature and language for all mental health professionals.
- To present defining characteristics or symptoms that differentiate specific diagnoses.
- To assist in identifying the underlying causes of disorders.
- The multiaxial classification system that involves assessment on several axes, or domains of information, allows the practitioner to identify all the factors that relate to a person’s condition.
- Axis I is for identifying all major psychiatric disorders except mental retardation and personality disorders .
- Axis II is for reporting mental retardation and personality disorders as well as prominent maladaptive personality features and defense mechanisms .
- Axis III is for reporting current medical conditions that are potentially relevant to understanding or managing the person’s mental disorder as well as medical conditions that might contribute to understanding the person.
- Axis IV for reporting psychosocial and environmental problems that may affect the diagnosis, treatment, and prognosis of mental disorders.
- Axis V presents a Global Assessment of Functioning, which rates the person’s overall psychological functioning on a scale of 0 to 100; this represents the clinician’s assessment of the person’s current level of functioning.
Historical Perspectives of the Treatment of Mental Illness
- People of ancient times believed that any sickness indicated displeasure of the gods and in fact was punishment for sins and wrongdoing.
- Those with mental disorders were viewed as either divine or demonic, depending on their behavior.
- Later, Aristotle attempted to relate mental disorders to physical disorders and developed his theory that the amounts of blood , water, and yellow and black bile in the body controlled the emotions.
- These four substances, or humors, corresponded with happiness, calmness, anger, and sadness; imbalances of the four humors were believed to cause mental disorders, so treatment was aimed at restoring balance through bloodletting, starving, and purging.
- In early Christian times, all diseases were again blamed on demons, and the mentally ill were viewed as possessed; priests perform exorcism to to rid evil spirits.
- During the Renaissance, people with mental illness were distinguished from criminals in England; those considered harmless were allowed to wander the countryside and or live in rural communities, but the more “dangerous lunatics” were thrown in prison, chained, and starved.
- In 1547, the Hospital of St. Mary of Bethlehem was officially declared a hospital for the insane, the first of its kind; by 1775, visitors at the institution were charged a fee for the privilege of viewing and ridiculing the intimates, who were seen as animals, less than human.
- In the 1790s, a period of enlightenment concerning persons with mental illness began.
- Phillipe Pinel in France and William Tukes in England formulated the concept of asylum as a safe refuge or haven offering protection at institutions where people had been whipped, beaten, or starved just because they were mentally ill (Gollaher, 1995).
- In the United States, Dorothea Dix (1802-1887) began a crusade to reform the treatment of mental illness after a visit to Tukes’ institution in England; she was instrumental in opening 32 state hospitals that offered asylum to the suffering.
- The period of scientific study and treatment of mental disorders began with Sigmund Freud (1856-1939) and others, such as Emil Kraeplin (1856-1926) and Eugene Bleuler (1857-1939).
- With these men, the study of psychiatry and the diagnosis and treatment of mental illness started in earnest.
- Freud challenged society to view human beings objectively; he studied the mind, its disorders, and their treatment as no one had before.
- Kraeplin began classifying mental disorders according to their symptoms, and Bleuler coined the term schizophrenia .
- A great leap in the treatment of mental illness began in about 1950 with the development of psychotropic drugs, or drugs used to treat mental illness.
- Chlorpromazine ( Thorazine ) an antipsychotic drug, and lithium, an antimanic agent, were the first drugs to be developed.
- Over the following 10 years, monoamine oxidase inhibitor antidepressants , haloperidol ( Haldol ), an antipsychotic; tricyclic antidepressants ; and antianxiety agents, called benzodiazepines , were introduced.
The National Institute of Mental Health (NIMH) estimates that more than 26% of Americans aged 18 years and older have a diagnosable mental disorder- approximately 57.7 million persons each year (2006).
- Furthermore, mental illness or serious emotional disturbances impair daily activities for an estimated 10 million adults and 4 million children and adolescents.
- Mental disorders are the leading cause of disability in the United States and Canada for persons 15 to 44 years of age.
- Homelessness is a major problem in the United States today; the National Resource and Training Center on Homelessness and Mental Illness (2006) estimates that one-third of adult homeless persons have a serious mental illness and that more than one half also have substance abuse problems.
- In 1993, the federal government created and funded Access to Community Care and Effective Services and Support (ACCESS) to begin to address the needs of people with mental illness who were homeless either all or part of the time.
- In 1873, Linda Richards graduated from the New England Hospital for Women and Children in Boston; she went on to improve nursing care in psychiatric hospitals and organized educational programs in state mental hospitals in Illinois.
- Richards is called the first American psychiatric nurse; she believed that “the mentally sick should be at least as well cared for as the physically sick” (Doona, 1984).
- The first training of nurses to work with persons with mental illness was in 1882 at McLean Hospital in Belmont, Massachusetts.
- The care was primarily custodial and focused on nutrition , hygiene , and activity.
- The role of psychiatric nurses expanded as somatic therapies for the treatment of mental disorders were developed.
- Treatments such as insulin shock therapy (1935), psychosurgery (1936), and electroconvulsive therapy (1937) required nurses to use their medical- surgical skills more extensively.
- The first psychiatric nursing textbook, Nursing Mental Diseases by Harriet Bailey was published in 1920; in 1913, John Hopkins was the first school of nursing to include a course in psychiatric nursing in its curriculum.
- In 1973, the division of psychiatric and mental health practice of the American Nurses Association (ANA) developed standards of care, which it revised in 1982, 1994, and 2000.
- Standards of care are authoritative statements by professional organizations that describe the responsibilities for which nurses are accountable.
- The goal of self-awareness is to know oneself so that ones’ values, attitudes, and beliefs are not projected to the client, interfering with nursing care; self-awareness does not mean having to change one’s values and beliefs unless one desires to do so.
1 thought on “Mental Health and Psychiatric Nursing”
Such a useful information in brief, really appreciate the efforts of writer Marianne
Leave a Comment Cancel reply
1234 North Avenue South Bandung, IND 36001

+1 (567) 269-1073
Mon-Sun:8.00-18.00.

Mental Health Case Studies

Student Response
This Knowledge Check reviews the topics in Module 6 and is formative in nature. It is worth 20 points where each question is worth 1 point. You are required to submit a sufficient response of at least 2-4 sentences in length for each question.
Scenario 1: Schizophrenia
A 21-year-old male college student was brought to Student Health Services by his girlfriend who was concerned about changes in her boyfriend’s behaviors. The girlfriend says that recently he began hearing voices and believes everyone is out to get him. The student says he is unable to finish school because the voices told him he was not smart enough. The girlfriend relates episodes of unexpected rage and crying. Past medical history noncontributory but family history positive for a first cousin who “had mental problems”. Denies current drug abuse but states he smoked marijuana every day during his junior and senior years of high school. He admits to drinking heavily on weekends at various fraternity houses. Physical exam reveals thin, anxious disheveled male who, during conversations, stops talking, cocks his head and appears to be listening to something. There is poor eye contact and conversation is rambling.
Based on the observed behaviors and information from girlfriend, the APRN believes the student has schizophrenia.
Question 1 of 4:
Describe the positive symptoms of schizophrenia and relate those symptoms to the case study patient.
Schizophrenia often changes how individuals think, feel, and behave and vary from person to person. The symptoms can appear and disappear suddenly. No individual has all the symptoms at a time. Positive symptoms of schizophrenia include the highly exaggerated ideologies, perceptions, or actions that show that an individual cannot tell what is real and what is not. Positive symptom include hallucinations, in which the individual sees, hears, smells, or feels things that no one else does; delusion, which implies the beliefs that seem strange to most people and are easy to prove wrong. However, the individual affected might think that some other person is trying to control their brain through things such as TV or the belief that some is out to get them; confused thoughts and disorganized speech; trouble in concentrating, movement disorders. For instance, in this scenario, the patient believes that someone is out to get him, when that is not true. Besides, the patient changed his behaviors and begun to drink heavily on weekends.
Question 2 of 4:
Explain the genetics of schizophrenia.
Also Read : Nursing Assignment Help
The exact cause of schizophrenia is unknown but a combination of genetics, environment, and altered brain chemistry and structure may play a significant role in its development. Besides, the inheritance pattern is not known. However, the risk of developing schizophrenia is higher among individuals with family member who has schizophrenia compared to the general population. Most individuals with a close relative with schizophrenia will, however not develop the disorder themselves. Genetically, schizophrenia and bipolar disorders have some similarities in that the two share similar risk genes. A predisposition to schizophrenia can run in families. However, in the general population, only one percent o individuals develop it over their lifetime, but if one of the parents had schizophrenia, the children have a 10 percent chance o developing schizophrenia. In the case scenario, the patient has a family history positive for a first cousin who “had mental problems”, implying that he is also at high risk for schizophrenia.
Question 3 of 4:
The APRN reviews recent literature and reads that neurotransmitters are involved in the development of schizophrenia. What roles do neurotransmitters play in the development of schizophrenia?
There are about 100 neurotransmitters in the brain charged with carrying messages from the end of one nerve branch to the cell body of another. In the brain of a person with schizophrenia, something goes wrong with this system of communication. Notably, two neurotransmitters play a substantial role in the development of schizophrenia. They include DOPAMINE and SEROTONIN. An increase in dopamine in certain areas of the brain results in overstimulation and excess sensory information that causes difficulty with concentration, thought process, reality orientation, feelings and behaviors besides, any abnormalities in serotonin activities results in a sensitive brain, to appear as if the nerve cells were sandpapered, thus leading to schizophrenia. The action of dopamine and serotonin explains why the patient in this case scenario experiences episodes of unexpected rage and crying.
Question 4 of 4:
The APRN reviews recent literature and reads that structural problems in the brain may be involved in the development of schizophrenia. Explain what structural abnormalities are seen in people with schizophrenia.
Structural problems in the brain such as complications brought about by other diseases may cause structural damage to the brain, which may develop into schizophrenia in later years. During older ages, structural changes result in alterations or abnormalities of both the white and gray mater. These changes lead to brain abnormalities and start prior to the onset of clinical symptoms of schizophrenia, especially those that concern language processing. The other abnormalities include neu roanatomical abnormalities before and after the onset of psychosis, leading to schizophrenia.
Scenario 2: Bipolar Disorder
A 34-year-old female was brought to the Urgent Care Center by her husband who is very concerned about the changes he has seen in his wife for the past 3 months. He states that his wife has had been depressed and irritable, has complaints of extreme fatigue, has lost 10 pounds and has had insomnia. He has come home from work to find his wife sitting in front of the TV and not moving for hours. In the past few days, she suddenly has become very hyperactive, has been talking incessantly, has been easily distracted and seems to “flit from one thing to another . ”. She hasn’t slept in 3 days. The wife went on an excessive shopping spree for new clothes that resulted in their credit card being denied for exceeding the line of credit. The wife is unable to sit in the exam room and is currently pacing the hallway muttering to herself and is reluctant to talk with or be examined the ARNP. Physical observation shows agitated movements, rapid fire speech, and hyperactivity. Based on the history and observable symptoms, the APRN suspects that the patient has bipolar type 2 disorder. The APRN refers the patient and husband to the Psychiatric Mental Health Nurse Practitioner for evaluation and treatment.
Question 1 of 6 :
Discuss the role genetics plays in the development of bipolar 2 disorders.
Bipolar 2 disorder is not only caused by one single gene, but by multiple genes, with each gene contributing only a small percentage of vulnerability, though acting together with other environmental factors like stress, lifestyle, habits and sleep to cause bipolar 2 disorder. The genes involved in bipolar disorder include G72/DAOA, DISC1, NRG1, TPH2, BDNF, 5-HTT, and DAT1. Therefore, genetics play a significant role in the development of bipolar disorder even though the exact inheritance pattern is not clear, but variations in many genes likely combine to increase an individual’s chance of developing bipolar 2 disorders. This combination results in mood swings, ranging from depressive lows to manic highs, as witnessed in this patient. The patient went n a spree o shopping until they run out of credit.
Question 2 of 6 :
Explain how the hypothalamic-pituitary-adrenal (HPA) system may be associated with bipolar type 2 disease.
Hypothalamic-pituitary-adrenal (HPA) system is associated with bipolar 2 disorders because it is central to the pathogenesis of depressive symptoms and cognitive deficits, which may further lead to neurocytotoxic effects of raised cortisol levels. Dysregulation o the hypothalamic-pituitary-adrenal (HPA) axis leads to manic episodes experienced by individuals with bipolar 2 disorders may be preceded by an increased in ACTH and cortisol levels, resulting in cognitive problems and functional impairments. For instance, the patient in this scenario had irritable behavior and depressed, indicating a compromised HPA system.
Question 3 of 6 :
Discuss the role inflammatory cytokines play in the development and exacerbation of bipolar type 2 symptoms
Inflammatory cytokines play some role in the development and exacerbation of bipolar type 2 symptoms. Cytokines are proteins involved in the regulation and orchestration of the immune response. Cytokines can directly affect neuronal activity, thus inducing neuronal excitability and plastic changes in the mood regulating areas of the brain and neuroprogression of the bipolar diathesis. Besides, inflammatory cytokines influence the symptoms and exacerbation of type 2 bipolar by influencing the HPA through effects on HPA axis as it increases the levels of cortisol hormone.
Question 4 of 6 :
Discuss the role of the amygdala in bipolar disorder.
Amygdale plays the role of mediating in not only physiologic but also behavioral arousal in response to environmental stimuli. In bipolar disorder, amygdale plays a role in emotion-related brain function. Any damage to amygdale leads to changes in the mood states such as facial expression and social withdrawal, as noted in the patient in this scenario. The patient has suddenly become very hyperactive and has been talking incessantly, indicating changes in behavioral arousal and changes in emotions.
Question 5 of 6 :
How does neurochemical dysregulation contribute to bipolar disorders?
Bipolar 2 disorders occur as a result of chemical imbalance in the brain. Therefore, neurochemical dysregulation means that the neurotransmitters, the chemical responsible for controlling the functions of the brain such as noradrenaline, serotonin and dopamine are not balanced. Any faulty in homoeostasis between noradrenaline, serotonin and dopamine transporter and receptors lead to depressive and manic phases of bipolar disorders.
Question 6 of 6 :
What is the current status of the use of nutraceuticals in management of depression?
Currently, nutraceuticals are increasingly being used in the management and treatment of depression due to limited prescription options. However, research indicates that patients with long-standing depression are not likely candidates for nutraceutricals, which tend to be more effective in patients with milder forms of depressive illnesses. Therefore, physicians are encouraged to always monitor the side effects and possible drug-drug interactions, and utilize their critical judgment in deciding if he agents are making any difference.
Scenario 3: Panic Disorders and Attacks
A 27-year-old female presents to the Emergency Room , with a chief complaint of palpitations, rapid heart rate, sweating, tremors, and inability to catch her breath. The symptoms started about 10 hour ago and have gotten worse. She states she has some chest pain that remains constant no matter what. She also has numbness and tingling around her mouth and lips. She says she knows something “terrible is going to happen”. She denies having any similar episode in the past. Past medical history noncontributory. Social history significant for recent stressor of applying for medical school and taking the Medical College Admission Test (MCAT). She had not received the results prior to the episode but is sure that the failed the test. Says she doesn’t know if anyone else in her family has had similar episodes. Physical exam reveals a thin, anxious appearing female who is profusely sweating despite cool ambient air temperature. BP 176/88, Pulse 136, and respirations 26. Electrocardiogram negative for evidence of myocardial infarction and all lab data within normal limits except for mild respiratory alkalosis. The patient’s symptoms are subsiding and the patient states she is feeling better. The APRN suspects the patient has just experienced a panic attack.
Question 1 of 2 :
What are panicogens and how do they contribute to the development of panic attack symptoms?
Panicogens are substances that cause panic or anxiety. They include sever stress, Yohimbine, CCK tetrapeptide (CCK-4), caffeine, m -chlorophenylpiperazine, and benzodiazepine partial inverse agonist FG 7142. These agents cause panic attack by increasing anxiety, nervousness, fear, nausea, palpitations, restlessness, and tremors. For instance, the patient in this scenario had chief complaint of palpitations, rapid heart rate, sweating, and tremors, which re all triggered by the panicogenic agents.
Question 2 of 2 :
How does the GABA-benzodiazepine (BZ) receptor systems contribute to panic attacks/disorders?
The GABA-benzodiazepine (BZ) receptor systems contribute to panic attacks because their blockage with antagonists results in severe anxiety that eventually leads to panic attack. However, increasing GABA receptor function with antagonists reduces anxiety and changes of panic disorders.
Scenario 4: Social Anxiety Disorder (SAD)
A 21-year-old female college junior makes an appointment to see the APRN in the Student Health Clinic. The student tells the APRN that it has gotten harder and harder for her to attend classes, especially her history class where the class is preparing for the semester’s end presentations. She says she is terrified to speak to the class and is considering dropping the class so she will not have to present. She has a significant impairment in social activities and has resigned from her sorority. She is unable to go to the library to study as she feels everyone is looking at her and mocking her. She admits to having some of these symptoms in high school, but the guidance counselor was able to work with her to decrease some of her symptoms. Past medical history noncontributory except for the milder symptoms exhibited in high school. Family history noncontributory. Social history positive for anxiety related to social situations that has had a negative impact on both her scholarly and social endeavors. The APRN diagnoses the student with social anxiety disorder (SAD).
Describe the areas of the brain that are associated with social anxiety disorder.
The areas of the brain that are mostly associated with social anxiety include brain stem, prefrontal cortex, and amygdale, which play a key role in modulating fear and anxiety. Prefrontal cortex is responsible for pathological anxiety responses related to negative emotions caused by amygdala, while brain stem controls the rate of breathing and any fault may result in social anxiety. In these cases, the patient’s social anxiety possibly originated from the prefrontal cortex which concerns negative emotions. The patient has a significant impairment in social activities and has resigned from her sorority and is also unable to go to the library to study as she feels everyone is looking at her and mocking her, which are all negative social emotions.
How is oxytocin associated with SAD?
Oxytocin hormone is associated with SAD as it is known to promote positive social interactions such as feelings of love, social bonding, and well-being. The hormone act by reducing the impact of SAD on and individual and enhance emotional health.
Scenario 5: Generalized Anxiety Disorder (GAD)
A 36-year-old female comes to see the APRN in clinic with a chief complaint of “I’m so and I feel all keyed up all the time”. She states she feels restless, keyed up, and on edge most of the time. She fatigues easily and has difficulty concentrating and says her mind goes blank. She admits to being irritable and snapping at her coworkers which she worries will affect her job. She says the symptoms have been present for about 8 or 9 months. and Increased muscle tension. She has had difficulty falling asleep or stay sleeping. Further questioning revealed that prior to her symptoms, her parents got divorced which has been a great stressor for her. Past medical history noncontributory. Social history positive for a case of “nerves” when she was in high school that seemed to resolve after she graduated from college. No drug or alcohol history. The APRN believes the patient has generalized anxiety disorder (GAD).
Discuss the role of neurotransmitters in the expression of GAD.
Several neurotransmitters are involved in GAD such as serotonin , glutamate, gamma-amino butyric acid, Cholecystokinnin, Adenosine and many others. However, some of these neurotransmitters are inhibitory while others are excitatory. Therefore, these neurotransmitters play a key role in up-regulation or down-regulation of GAD. Neurotransmitters in the brain modulate the neural circuitry involved in anxiety. For instance, the dysregulation of GABA, an inhibitory neurotransmitter, especially the GABA A variant, tend to elevate the amygdala activity in the brain, thus causing GAD.
Explain the structural brain changes that occur in people with GAD.
In people with GAD, brain structural changes occurs a result of alterations of the gray and white matter. The structural changes in gray matter include macrostructural changes such as decreased cortical thickness and volume, as well as through microstructural changes such as increased gray matter mean diffusivity. On the other hand, structural changes in white matter include changes in macrostructural lesions measured by the total white matter hyper-intensity (WMH) burden and through microstructural damage in the white matter tracts.
Scenario 6: Post-Traumatic Stress Disorder (PTSD)
A 27-year-old man comes to the Veteran’s Administration Hospital at the insistence of his fiancée who accompanies him to the appointment. She tells the APRN that her fiancée has not “been the same” since he returned from his second tour in Iraq. He was an infantryman with a local Marine Reserve unit and served 2 tours and was honorably discharged. Since his return, he has had difficulty sleeping, and says he “sleeps with one eye open” and fears sleep. Deep sleep brings vivid nightmares. He grudgingly admits to having experienced several traumatic events during his second tour of duty. He is unwilling to discuss them and will not reveal specific details. He is short tempered and irritable and is afraid to be around people as he doesn’t want to snap at people and alienate them. He startles easily at loud noises, especially the sounds of cars backfiring. He admits to thinking there are threats everywhere and spends an excessive amount of time searching for them but never finding any. He has intrusive memories almost every day and says he really isn’t interested in doing much of anything. He is very worried that these symptoms are irreparably hurting his relationship with his fiancée who he loves very much. The APRN diagnoses him with post-traumatic stress disorder (PTSD).
Describe the changes seen in the brain structure in patients with PTSD.
Changes in the brain structure in patients with PTSD emanates from severe emotional trauma that causes lasting alterations in the ventromedial prefrontal cortex region of the brain. Prefrontal cortex is responsible for the regulation of responses triggered by amygdale. PTSD patients show a marked decrease in the volume of the ventromedial prefrontal cortex and the functional ability of this region. For instance, the patient in this scenario grudgingly admits to having experienced several traumatic events during his second tour of duty, indicating alterations in the ventromedial prefrontal cortex region of the brain.
Briefly discuss the role glucocorticoids may have on the development of PTSD
Glucocorticoids play an important role in the development of PTSD. Notably, moderate secretion of glucocorticoids enhances a patients’ coping mechanism by helping them to process information is a way that reduces the retrieval of fear-evoking memories. However, when there is inadequate production of glucocorticoids such as cortisol, which is a stress hormone, the individuals may have problems to emotionally adapt following a traumatic event as seen in the patient in this scenario.
Scenario 7: Obsessive-Compulsive Disorder (OCD)
A 17-year-old male high school junior comes to the clinic to establish care. He recently moved from a relatively urban area to a very rural area and has just started his junior year in a new school. The mother states that she has noticed that her son has been frequently washing his hands and avoids contact with any dirty or soiled object. He uses paper towels or napkins over the knob on a door when opening it. According to the mother, this behavior has just appeared since moving. The patient, upon close questioning, admits that he is “grossed out” by some of the boys in the boys’ room since they use the toilet and do not wash their hand afterwards. He is worried about all the germs the boys are carrying around. Past medical history is noncontributory. Social history -lives with parents and 2 siblings in a house in a new town. Is an honors student. Based on these behaviors, The APRN thinks the patient has obsessive-compulsive disorder (OCD).
Question 1 of 2:
What is primary pathophysiology of OCD?
Obsessive-compulsive disorder (OCD) is a mental disorder that is characterized by absurd, recurrent, and uncontrollable thoughts that lead to anxiety, followed by repetitive behaviors aimed at reducing anxiety. The primary pathophysiology of OCD is overly persistent and uncontrolled neural activity in SMS, possibly as a result of dopamine-serotonin imbalance. For instance, in the case scenario, the patient admits that he is “grossed out” by some of the boys in the boys’ room since they use the toilet and do not wash their hand afterwards. He is also worried about all the germs the boys are carrying around; indicating that he is has anxiety from the thought that other boys’ hands may be contaminated with germs.
Question 2 of 2:
Describe the role the dorsal anterior cingulate cortex (dACC) has in reinforcement of obsessive behaviors.
In patients with OCD, the dACC acts as a hub that processes negative emotional and reinforcing information and then uses the information to direct motivated behavior. Therefore, it is likely that OCD processes such as anxiety and depression can be reinforced by dACC modulation.
Get a top-grade nursing assignment today!
- NICE Guidance
- Conditions and diseases
- Mental health, behavioural and neurodevelopmental conditions
Common mental health problems: identification and pathways to care
Clinical guideline [CG123] Published: 25 May 2011
This guideline has been stood down. All of the recommendations are now covered in other NICE guidelines, or are out of date and no longer relevant to clinical practice.
For guidance on common mental health problems, see our guidelines on:
- Depression in adults
- Depression in adults with a chronic physical health problem
- Depression in children and young people
- Generalised anxiety disorder and panic disorder in adults
- Obsessive-compulsive disorder and body dysmorphic disorder
- Social anxiety disorder
Arms Control Wonk
Abuse of Psychiatry for Political Purposes in the USSR: A Case-Study and Personal Account of the Efforts to Bring Them to an End
- First Online: 01 January 2010
Cite this chapter

- Robert Van Voren 3
Part of the book series: International Library of Ethics, Law, and the New Medicine ((LIME,volume 45))
1310 Accesses
3 Citations
The issue of political abuse of psychiatry has dominated the agenda of world psychiatry for more than 40 years. The consequential discussions have had a profound impact on the conceptual debates with regard to medical ethics and the professional responsibilities of physicians. These have led to the development of a range of international documents and declarations outlining the boundaries between acceptable and inadmissible behavior within the psychiatric profession. Discussions as to what exactly constitutes political abuse of psychiatry are still ongoing. In this chapter, political abuse of psychiatry refers to the misuse of psychiatric diagnosis, treatment and detention for the purposes of obstructing the fundamental human rights of certain individuals and groups in a given society. The case of political abuse of psychiatry in the Soviet Union is used as an important example of how the abuse evolved and eventually was brought to an end.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
Subscribe and save.
- Get 10 units per month
- Download Article/Chapter or eBook
- 1 Unit = 1 Article or 1 Chapter
- Cancel anytime
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
- Durable hardcover edition
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Similar content being viewed by others

Stemming the Tide of Anti-Semitism: The Roles of Psychiatrists and Psychiatry

Psychiatry, Law, and Revolution: A View from Egypt

Beyond ideological platitudes: socialism and psychiatry in Eastern Europe
The author has been involved in the struggle against the political abuse of psychiatry since the late 1970s and was one of the founding members of the International Association on the Political Use of Psychiatry. This organization was later renamed in Geneva Initiative on Psychiatry and since 2005 it is called Global Initiative on Psychiatry. Van Vorens memoirs On Dissidents and Madness were published by Rodopi, Amsterdam/New York, in 2009 . A book on the issue of Soviet psychiatric abuse and the WPA in 1983–1989, titled Cold War in Psychiatry , will appear with the same publisher in 2010
See Psychiatry under Tyranny, An Assessment of the Political Abuse of Romanian Psychiatry During the Ceaucescu Years , Amsterdam, IAPUP, 1998.
Article 62 of the Soviet Constitution (1977) stated: ‘Each citizen is obliged to protect the interests of the Soviet State and to contribute to its power and authority’ (Helmchen 1986 ).
Speech published by Pravda on May 24, 1959 .
and private conversations of the author with Dr. Korotenko. Other former Soviet psychiatrists confirmed this dilemma, see Van Voren, R., On Dissidents and Madness , Rodopi, 2009 , pp. 168–171.
The same bibliographical dictionary of A. Koppers lists over 150 institutions where these abuses took place.
American Journal of Psychiatry, 1970, vol 126, pp. 1327–1328; vol. 127, pp. 842–843; 1971, vol. 127, pp. 1575–1576, and 1974, vol. 131, p. 474.
Kaznimye sumasshestviem , Frankfurt, Possev, 1971, p. 479.
Vladimir Bukovsky was eventually exchanged for the Chilean Communist Party leader Luis Corvalan at Zürich airport on December 18, 1976.
Report of the Secretary-General, 1983 . WPA, Vienna July 1983. Following the Soviet resignation, several other Eastern European societies withdrew from the WPA, as well as the Cuban Association.
This book is based on extensive investigation of Stasi archives and shows how Prof. Juhasz was put under maximum pressure by the Hungarian authorities until his untimely death on February 27, 1984. It also explains how Prof. Jochen Neumann was proposed as successor by the East German authorities and managed to get himself elected by the WPA Executive Committee. The author has extenssively interviewed Jochen Neumann and former Hungarian colleagues of Pal Juhasz on the matter in preparation of the book Cold War in Psychiatry .
data based on examination of both WPA Executive Committee minutes and Stasi archives.
Blazhenny Izgnannye (Beatified Exilees) ( 1989 ). The film was eventually broadcasted in many countries, including the USSR, and remains a powerful document of the political abuse of psychiatry in the Soviet Union.
The US State Department visit was not the only attempt to assess the state of affairs in Soviet psychiatry and whether Soviet psychiatric abuse was indeed coming to an end. Also organizations such as the International Academy of Law and Mental Health (IALMH) sent teams to the USSR to meet with Soviet authorities and psychiatrists, yet the reports were mostly conflicting and showed an intransigence on the part of the Soviet psychiatric leadership to adjust to the new political situation in the country.
Information from Dr. Yuri Yudin, member of the Soviet delegation.
Dr.Koryagin would remain in Switzerland for a few more years and then returned to Russia. He now lives in a small town east of Moscow.
The Independent Psychiatric Association was founded in Moscow in March 1989 and was the first challenge to the monopoly over Soviet psychiatry of the AUSPN.
For instance, from the book by Sonja Süss it becomes clear that the main actor against the political abuse of psychiatry in the USSR, the International Association on the Political Use of Psychiatry, was unknowingly infiltrated by the Stasi. The available reports run until 1983; the files of a later date seem to have been destroyed when Eastern German totalitarian rule disintegrated.
The negotiations in Athens were led by Yuri Reshetov of the Soviet Ministry of Foreign Affairs, with direct and constant communication with the Soviet leadership in Moscow.
Abbreviations
All Union Society of Psychiatrists and Neuropathologists (of the USSR)
Diagnostic and Statistic Manual (of Mental Disorders), 4th Revision (American Psychiatric Association)
International Academy of Law and Mental Health
International Association on the Political Use of Psychiatry
International Classification of Diseases (World Health Organisation)
Komitet Gosudarstvennoi Besopasnosti
Royal College of Psychiatrists
Ministerium für Staatssicherheit”, i.e. Secret Service of the German Democratic Republic
Union of Soviet Socialist Republics
BlazhennyIzgnannye (Beatified Exilees) (1989).
Google Scholar
Bloch S, Reddaway P (1977) Russia’s political hospitals, Gollancz, London
Bloch S, Reddaway P (1984) Soviet psychiatric abuse, Gollancz, London
Bloch S (1989) Soviet psychiatry and Snezhnevskyism. In: Van Voren R (ed) Soviet psychiatric abuse in the Gorbachev era. IAPUP, Amsterdam
Brown CA, Lago A (1991) The politics of psychiatry in revolutionary Cuba. Transaction Publishers, New York, NY
Bukovsky V (1978) To build a castle, my life as a dissenter. André Deutsch Publishers, London
Dmitrieva D (2001) Alyans Prava i Miloserdiya. Nauka, Moscow
Helmchen H (1986) Ethische Fragen in der Psychiatrie. In: Kisker KP, Lauter H, Meyer JE, Müller C, Strömgren E (eds) Psychiatrie der Gegenwart. Bd 2 Krisenintervention, Suizid, Konsiliarpsychiatrie. Springer, Berlin, Heidelberg, New York, NY, pp 310–368
Kaznimye sumasshestviem (1971)
Komsomolskaya Pravda (15 July 1987)
Komsomolskaya Pravda (18 Nov 1987)
Koppers A (1990) A biographical dictionary on the political abuse of psychiatry in the USSR. IAPUP, Amsterdam
Korotenko A, Alkina N (2002) Sovietskaya Psikhiatriya – Zabluzhdeniya I Umysl. Sphera, Kiev
Koryagin A (1987) Unwilling patients. In: Van Voren R (ed) Koryagin: a man struggling for human dignity. IAPUP, Amsterdam
Mexico City News (13 Nov 1971)
Nijeboer A (2006) Een man tegen de Staat. Papieren Tijger, Breda
Pisarev S (1970) Soviet mental prisons. Survey, London
Pravda (24 May 1959)
Psychiatric News (1 Oct 1976)
Reuter report, Mexico City (2 Dec 1971)
Royal College of Psychiatrists (Nov 1976) News and notes
Schizophrenia Bulletin (1989) Supplement to 15(4):
Shaw C (1989) The world psychiatric association and Soviet psychiatry. In: Van Voren R (ed) Soviet psychiatric abuse in the Gorbachev era. IAPUP, Amsterdam
Süss S (1998) Politisch Missbraucht? Psychiatrie und Staatssicherheit in der DDR, Ch. Linke, Berlin
The Times (16 Nov 1971)
Van Voren R (ed) (1987) Koryagin: a man struggling for human dignity. IAPUP, Amsterdam
Van Voren R (ed) (1989) Soviet psychiatric abuse in the Gorbachev era, IAPUP, Amsterdam
Van Voren R (2009) On dissidents and madness. Rodopi, Amsterdam, New York, NY
WPA (Nov 28 1971) Minutes of the committee meeting
WPA Newsletter (31 Oct 1975)
Download references
Author information
Authors and affiliations.
Global Initiative on Psychiatry, 1282, BG, Hilversum, The Netherlands
Robert Van Voren
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Robert Van Voren .
Editor information
Editors and affiliations.
Charité Campus Benjamin Franklin, Klinik für Psychiatrie/ Psychotherapie, Universitätsklinikum Berlin, Eschenallee 3, Berlin, 14050, Germany
Hanfried Helmchen
chemin Colladon 14, Geneve, 1209, Switzerland
Norman Sartorius
Rights and permissions
Reprints and permissions
Copyright information
© 2010 Springer Science+Business Media B.V.
About this chapter
Van Voren, R. (2010). Abuse of Psychiatry for Political Purposes in the USSR: A Case-Study and Personal Account of the Efforts to Bring Them to an End. In: Helmchen, H., Sartorius, N. (eds) Ethics in Psychiatry. International Library of Ethics, Law, and the New Medicine, vol 45. Springer, Dordrecht. https://doi.org/10.1007/978-90-481-8721-8_29
Download citation
DOI : https://doi.org/10.1007/978-90-481-8721-8_29
Published : 16 July 2010
Publisher Name : Springer, Dordrecht
Print ISBN : 978-90-481-8720-1
Online ISBN : 978-90-481-8721-8
eBook Packages : Medicine Medicine (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research

IMAGES
COMMENTS
mental health case study with psychosis unfolding reasoning jenna taylor, 18 years old primary concept mood and affect interrelated concepts (in order of ... Alcoholic Anonymous Assignment for lecture; Case Study Schizophrenia; Case Study #1 Mental Health Depresson; Related Studylists m. ... Mental Health Nursing (NUR-355) 113 Documents ...
Case Study: Mental Health Problems. 3997 words (16 pages) Essay in Nursing The purpose of this assignment is to select a client with the diagnosis of enduring mental illness and carry out an assessment based on the presenting problem of the chosen patient and the psychosocial intervention during his treatment.
Case Study Schizophrenia Keith RN unfolding clinical reasoning case study history of present problem: jeremy brown is caucasian male who was brought to the ... Mental Health Nursing (NUR-355) 113 Documents. Students shared 113 documents in this course. University California Baptist University. Academic year: 2021/2022. Uploaded by:
The purpose of this assignment is to select a client with the diagnosis of enduring mental illness and carry out an assessment based on the presenting problem of the chosen patient and the psychosocia ... Case Study: Mental Health Problems. Info: 4264 words (17 pages) Nursing Case Study ... Psychiatric and Mental Health Nursing: The Craft of ...
NUR 403 Week 2 Individual Assignment Case Study comprises: Resources: The case study found on p. 131 in Nursing Theory and the Case Study Grid on the Materials page of the student website Complete the Case Study Grid. ... Mental Health Nursing Case Study Examples . Mental health nursing plays a crucial role in promoting emotional well-being and ...
At PhD Nurse Writer, we are the academic writing experts that you should engage when seeking professional help with a nursing case study on mental health. We offer the best nursing assignment help , with a guarantee of original, engaging and plagiarism free case studies.
This assignment is going to explore about what mental health is and make a distinction between mental disorders and mental illnesses. A case study of a patient suffering with depression is going t. ... the Art and Science of Mental Health Nursing, Second Edition, Open University Press BIBLIOGRAPHY. Andrews, G and Jenkins, R (Eds) 1999 ...
Perfect for exam preparation, our reviewers and sample nursing test bank questions are designed to enhance your understanding and proficiency in mental health nursing. Key topics include: Mental Health and Psychiatric Nursing Overview. Nursing Care Management for Mental Health Conditions. Personality Disorders and Their Treatment.
NCMHCE Sample Case Study. You are a licensed mental health counselor working in a community agency. Your client self-referred for services because "my mother won't stop bugging me for staying in bed all day. I can't help it. I am in a rut and cannot find a way out.".
Case 5: Denise. Denise, a 19-year-old woman, has been admitted informally to an acute mental health ward; this is Denise's first admission. Denise was being treated for depression by her GP; prior to her admission Denise attempted to kill herself by cutting her wrists. Subsequently a short admission was arranged with the aim of devising a ...
Module 8 Case Study: Anxiety Disorder/Obsessive Compulsive Disorder. Nicole Visneski NUR 2459: Mental and Behavioral Health Nursing Ebony Wilhelm Rasmussen University August 29th, 2021. Describe at least three clinical signs of Anxiety observed in the videos.
Mental Health and Psychiatric Nursing. The field of mental health often seems a little unfamiliar or mysterious, making it hard to imagine what the experience will be like or what nurses do in this area. This is an overview of the history of mental illness, advances in treatment, current issues in mental health, and the role of the psychiatric ...
You are required to submit a sufficient response of at least 2-4 sentences in length for each question. Scenario 1: Schizophrenia. A 21-year-old male college student was brought to Student Health Services by his girlfriend who was concerned about changes in her boyfriend's behaviors. The girlfriend says that recently he began hearing voices ...
For guidance on common mental health problems, see our guidelines on: Depression in adults. Depression in adults with a chronic physical health problem. Depression in children and young people. Generalised anxiety disorder and panic disorder in adults. Obsessive-compulsive disorder and body dysmorphic disorder. Social anxiety disorder.
Case Study: Mental Health Problems. The purpose of this assignment is to select a client with the diagnosis of enduring mental illness and carry out an assessment based on the presenting problem of the chosen patient and the psychosocial intervention during his treatment. From the assessment process, the problem identified will be considered ...
However, the imminent deployment of Iskander missiles in Kaliningrad raises two concerns. First, Russian officials have repeatedly emphasized the role that the 500 km-range, nuclear-capable Iskander system would play in targeting US missile defense assets in Polan d. The United States and Poland held a ground-breaking for the US missile defense ...
To help with this assignment: • Review information about Anxiety in your ATI Content Mastery Series textbook PN Mental Health Nursing • Read the posted PowerPoints (with slide notes) for information about Bipolar disorders • Refer to the handout titled 'Psychiatric and Psychological Definitions' found under course documents.
In the case of South Africa severe abuses were the result of the policy of Apartheid, which resulted in very different conditions in mental health services for the white ruling class and the black majority of the population. Claims that psychiatry was abused as a means of political or religious repression were never confirmed.